To the Editor:
We read with interest the correspondence from Montagud-Marrahi et al1 putting forward that solid organ transplant (SOT) recipients are not at higher risk of severe coronavirus disease 2019 (COVID-19) infection despite their immunosuppression and the mild or atypical nature of their symptoms in their Spanish cohort. In the recent literature, this population achieves a mortality rate between 20% and 52% when they become critically ill.2 , 3 (p) Moreover, as innate immunity is altered by the infection, decreased doses of immunosuppressive drugs should be considered.4 , 5
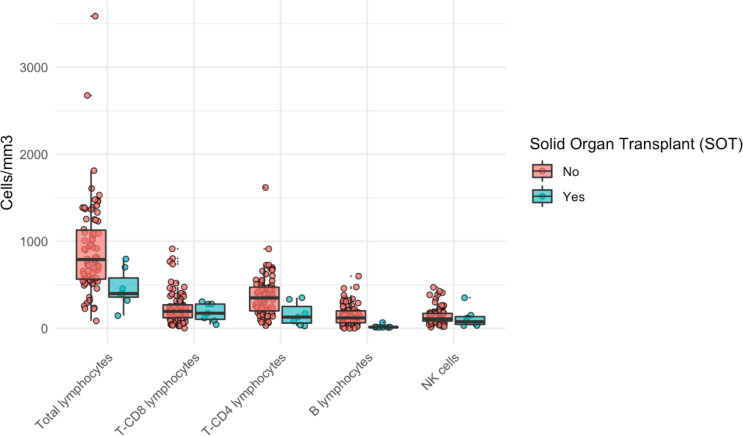
At the Saint-Louis hospital, Paris, among the 106 critically ill COVID patients, we identified 10 consecutive adult SOT recipients (9 kidney and 1 heart, age 57, range, 49-72 years, 70% male) who tested positive for COVID-19 between March 7 and April 10, 2020. Median time from organ transplantation was 50 months (75-80). Main comorbidities included hypertension (100%) and diabetes (50%). All patients were admitted with acute hypoxemic respiratory failure, 90% with asthenia, 70% with fever, and 40% with diarrhea. Mechanical ventilation was needed in six patients, standard oxygen in four, and high flow oxygen in two. Acute kidney injury developed in seven patients of whom three required renal replacement therapy. Laboratory results at admission were marked by elevated D dimers (median 1270 [ranges, 730-2310]), ferritin (1554 [1114-2068]), troponin (33.5 ng/L [29.9-48.6]), elevated procalcitonin (1.08 µg/L [0.47-1.87]), elevated interleukin-6 (IL-6) (46.6 pg/mL [31.9-73.7]) and IL-1β levels (0.54 pg/mL [0.35-0.81]). Levels of ferritin and IL-6 were not different between SOT and non-SOT patients (1230 vs 1554, P = .48 and 46.6 vs 75.4, P = .26, respectively). SOT recipients also presented with more severe lymphopenia than other patients (0.40 G/L [0.36-0.58] vs 0.79 G/L [0.56-1.13], P = .007). This difference concerned mostly B lymphocytes (0.013 [0.011-0.014] vs 0.12 [0.064-0.2] G/L, P < .001), T cells (0.31 [0.21-0.38] vs 0.58 [0.38-0.79] G/L, P = .014), and T-CD4 cells (0.13 [0.06-0.25] vs 0.35 [0.2-0.47] G/L, P = .006). T-CD8 lymphocytes and natural killer (NK) cells were not significantly lower in SOT recipients. The number of HLA-DR molecules on monocytes was not significantly higher in SOT patients (10 010 [6854-12 408] vs 8631 [7013-13 116], P = .89). Lymphocyte immunophenotyping and HLA-DR count on CD14+ monocytes were assessed using flow cytometry (FACS BD Canto II). Differences between SOT and non-SOT patients was assessed using a nonparametric Kruskal-Wallis test. Mycophenolate mofetil was withdrawn in all patients. High-dose steroids were given to eight patients. Viral reactivations were reported in six patients (cytomegalovirus in five and herpes simplex virus in two). Mean length of stay in intensive care unit (ICU) was 10 days (4-15 days). Seven patients were discharged from the ICU and three died. At ICU discharge, six of the seven patients were dialysis free ( Figure 1).
FIGURE 1.
Lymphocyte count in coronavirus disease 2019 (COVID-19) patients. Solid organ transplant recipients with COVID-19 present with lower total lymphocyte count than COVID-19 no solid organ transplant (SOT) patients, and this decrease is related to a reduction in CD4 cells and B cells, but not to a decrease in T-CD8 or natural killer (NK) cells [Color figure can be viewed at wileyonlinelibrary.com]
In conclusion, SOT patients form a specific group of COVID-19 immunocompromised patients with more profound lymphocytopenia, prevalence of acute kidney injury, and need for renal replacement therapy. Despite immunosuppression and high inflammation, survival and renal recovery are substantial for ICU patients3 , 5 but higher than average for COVID-19 patients.4
Acknowledgments
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
REFERENCES
- 1.Montagud-Marrahi E, Cofan F, Torregrosa J-V, et al. Preliminary data on outcomes of SARS-CoV-2 infection in a Spanish single centre cohort of kidney recipients [published online ahead of print 2020]. Am J Transplant. 10.1111/ajt.15970 [DOI] [PMC free article] [PubMed]
- 2.Guinault D, Del Bello A, Lavayssiere L, et al. Outcomes of kidney transplant recipients admitted to the intensive care unit: a retrospective study of 200 patients. BMC Anesthesiol. 2019;19(1):130. doi: 10.1186/s12871-019-0800-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pereira MR, Mohan S, Cohen DJ, et al. COVID-19 in solid organ transplant recipients: Initial report from the US epicenter [published online ahead of print 2020]. Am J Transplant. 10.1111/ajt.15941 [DOI] [PMC free article] [PubMed]
- 4.Coates PT, Wong G, Drueke T, et al. Early experience with COVID-19 in kidney transplantation. Kidney Int. 2020;97(6):1074–1075. doi: 10.1016/j.kint.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akalin E, Azzi Y, Bartash R, et al. Covid-19 and kidney transplantation. N Engl J Med. [published online ahead of print 2020]. 2020. 10.1056/NEJMc2011117 [DOI]