Abstract
The study compares empirical results on the coronavirus SARS‐CoV‐2 (causing COVID‐19) fatality risk perception of US adult residents stratified for age, gender, and race in mid‐March 2020 (N1 = 1,182) and mid‐April 2020 (N2 = 953). While the fatality risk perception has increased from March 2020 to April 2020, our findings suggest that many US adult residents severely underestimated their absolute and relative fatality risk (i.e., differentiated for subgroups defined by pre‐existing medical conditions and age) at both time points compared to current epidemiological figures. These results are worrying because risk perception, as our study indicates, relates to actual or intended health‐protective behaviour that can reduce SARS‐CoV‐2 transmission rates.
Keywords: coronavirus SARS‐CoV‐2, COVID‐19, risk perception, health‐protective behaviour, repeated cross‐sectional design
On 31 December 2019, China alerted the World Health Organization (WHO) of several cases of pneumonia induced by an unknown virus in the city of Wuhan. On 11 March 2020, it was declared a pandemic by the WHO (2020a); by mid‐March 2020, the novel coronavirus SARS‐CoV‐2 causing the disease COVID‐19 had already spread to over 140 countries (WHO, 2020b); and by April 2020, the United States had become the country with the highest number of officially confirmed cases of COVID‐19 worldwide according to Johns Hopkins University (2020). In the absence of established pharmaceutical protocols to treat affected individuals or vaccines to halt infections, most countries have implemented containment and mitigation strategies, requiring individuals to dramatically alter their lifestyle limiting personal freedom. The extent to which these measures will be politically acceptable and respected by populations is likely to depend, among other factors, on individuals’ perceived risk of suffering severe consequences following infection (Sheeran, Harris, & Epton, 2014). In fact, not all individuals are at equal risk of dying if infected. In particular, existing data from affected regions suggest that especially individuals with pre‐existing medical conditions and older individuals are at an increased fatality risk if infected (Oke & Heneghan, 2020).
With this study, we aimed to provide time‐critical insights on the SARS‐CoV‐2 fatality risk perception of the US population as a whole as well as for two crucial subgroups defined by pre‐existing medical conditions and age. Further, we aimed to examine risk perception as it relates to protective SARS‐CoV‐2‐related behaviour helping to avoid the virus from spreading. We did so by analysing two different time points in the course of the COVID‐19 crisis in the United States: first, in mid‐March (i.e., 13‐15 March 2020) with 1,663 to 2,951 confirmed COVID‐19 cases in the United States, and, second, in mid‐April (i.e., 10‐12 April 2020) with 466,033 to 529,951 reported cases (Roser, Ritchie, Ortiz‐Ospina, & Hasell, 2020).
Method
We drew on two independent samples of N1 = 1,182 (March) and N2 = 953 (April) US adult residents (i.e., ≥ 20 years, not positively tested for SARS‐CoV‐2) stratified for age, gender, and race (for N1 : 50.4% women, 48.6% men, 1% other; age: M = 45.6 years, SD = 15.72, range = 20 to 83; for N2 : 53.1% women, 46.5% men, 0.4% other; age: M = 41.14 years, SD = 14.87, range = 20 to 78; further demographic characteristics are listed in Table S1 in the supplemental material). Data were collected online on the platform Prolific (prolific.co). Data for the current analyses are made available via the OSF platform (see osf.io/sr4wp). The study was approved by the ethics review panel of the University of Luxembourg; participation was voluntary, and participants were compensated for their participation. In both samples, perceived personal risk of dying from SARS‐CoV‐2 if infected was assessed on a 9‐point scale ranging from Approximately zero (<0.0001%) to Approximately three‐quarters (75%). We used published crude case‐fatality risk estimators (Novel Coronavirus Pneumonia Emergency Response Epidemiology Team, 2020; WHO, 2020c) for the entire population (i.e., around 1%) as well as for the different subgroups defined by pre‐existing medical conditions (i.e., if none present: around 1%; if present: around 10%) and age (i.e., for 20 to 49 years: around 0.1%; for 50 to 69 years: around 1%; for 70 years and older: around 10%; see, for example, for a discussion on COVID‐19 case‐fatality risk estimators: Rajgor, Lee, Archuleta, Bagdasarian, & Quek, 2020). We operationalized pre‐existing medical conditions as a yes or no statement on whether the participant currently or ever experienced a serious medical condition such as heart disease, diabetes, chronic respiratory disease, high blood pressure, or cancer. To examine the effect of perceived fatality risk on behaviour, we assessed protective SARS‐CoV‐2‐related behaviour, which had been identified as key containment measures (Ferguson et al., 2020; WHO, 2020d) by means of an 8‐item scale (e.g., ‘I am planning to/have already started avoiding crowded spaces’; 5‐point rating; for N1 : α = .87, for N2 : α = .83). Additional information on the data collection as well as a full list of employed items can be found in the supplemental material.
Results
Figure 1 depicts the results. In a first step, we looked at the absolute and relative risk perception (i.e., differentiated for subgroups defined by pre‐existing medical conditions and age) as observed in March 2020 (Figure 1: depicted in darker shade). Looking at the overall sample (Figure 1a), one in five US adults (20%) perceived the absolute risk to die from SARS‐CoV‐2 if infected with the virus to be around 1% matching current epidemiological figures (Novel Coronavirus Pneumonia Emergency Response Epidemiology Team, 2020; WHO, 2020c). Around 14% reported higher perceived risk, whereas the majority of around 67% reported lower perceived risk than the 1% benchmark. As many as one in two US adults (51%) reported that their own odds of dying if infected were approximately one in ten thousand or even lower, thereby severely underestimating fatality risk. Figure 1b,c depicts the relative risk perception across the two subgroups defined by medical condition. Although individuals with pre‐existing medical conditions understood that their own risk of dying from SARS‐CoV‐2 if infected is higher than the average 1%, they still severely underestimated their fatality risk (77% vs. 74% in the no pre‐existing condition group). These results were mirrored by those of the three age subgroups. Figure 1d–f depicts their results. Even though older US adults tended to know that their relative fatality risk is higher than 1%, they unambiguously underestimated their risk (69%). Slightly more than half (58% for both) of the two younger age groups severely underestimated their risk of dying of SARS‐CoV‐2 if infected.
Figure 1.
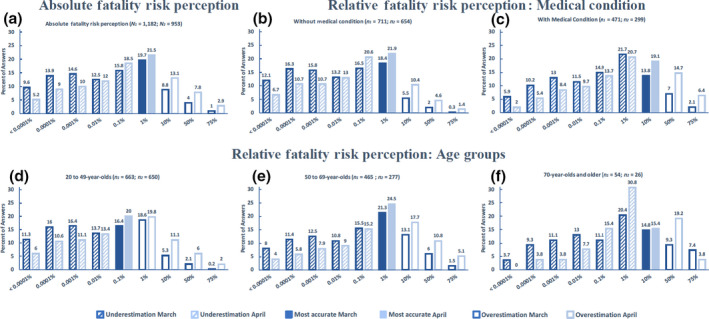
Perceived absolute and relative SARS‐CoV‐2 fatality risk perception in US adult residents for March and April 2020.
In a second step, we tested whether SARS‐CoV‐2 risk perception has changed from March to April 2020. Risk perception as observed in April 2020 is depicted in Figure 1 in lighter shade. A significant Mann–Whitney test indicated that absolute risk perception levels in March (Mdn = 0.01) differed significantly from April (Mdn = 0.1) for the overall sample (U = 453,726, z = −7.82, p < .001, small effect size: r = −.17). US adults thus reported higher risk perception in April compared to March, albeit a considerable number of US adults still severely underestimated their absolute fatality risk (e.g., 36.2% reported that their own fatality risk was approximately one in ten thousand or even lower). The relative risk perception levels for the different subgroups defined by medical conditions and age changed from March to April, too (see Figure 1b–f), indicating overall higher risk perception in April. With the exception for the oldest age group, where statistical power was lacking to detect smaller effect sizes, these observed subgroup differences were statistically significant (ps < .001) with small effects ranging from r = −.18 to r = −.21.
In a third step, we tested the relation between fatality risk perception and behaviour. A significant Spearman's rho correlation (for March: r = .21, p < .001; for April: r = .14, p < .001) indicated that participants with a lower perceived risk tended to perform less behaviour that can reduce SARS‐CoV‐2 transmission rates (e.g., not shaking hands or avoiding crowded spaces). The observed relation was descriptively lower in April. At the same time, US adults performed or intended to perform higher levels of protective SARS‐CoV‐2‐related behaviour in April (M = 4.41 SE = 0.02) than they did in March (M = 3.93 SE = 0.02). This difference was significant t(2118.087) = −15.658, p < .001, with a medium effect of r = .32.
Discussion
Our results are limited by the use of a repeated cross‐sectional design instead of a longitudinal panel design. Further, we assessed risk perception with nine pre‐defined response categories, which might have induced a response bias (Schwarz, 1999) and, additionally, restricted participants from indicating their fatality risk with greater precision. However, our study provides time‐critical insights into different stages of the unfolding COVID‐19 crisis in the United States aiming at informing health professionals, scholars, and political stakeholders alike. Overall, given the current epidemiological figures (Novel Coronavirus Pneumonia Emergency Response Epidemiology Team, 2020; WHO, 2020c), our findings suggest that many US adult residents severely underestimated their absolute and relative fatality risk if infected with SARS‐CoV‐2 in March 2020. Risk perception changed from March to April towards more accuracy and overestimation albeit still in April, many US adult residents underestimated their fatality risk. These results are worrying because risk perception, as our study suggests, guides behaviour that can reduce transmission rates (see also Sheeran et al., 2014) and thus saves lives. These results confirm previous evidence on the role that risk perceptions play in shaping health‐protective behaviours during pandemics (Bish & Michie, 2010) and highlight the importance of ensuring that policy interventions, regulations, and guidelines as well as communication strategies target the population in general and some demographic groups in particular, to ensure an alignment between the risk they face and the risk they perceive. Suppression and mitigation strategies to halt viral spread during pandemics require drastic behavioural changes that individuals need to implement rapidly and in a sustained way. Our work suggests that ensuring that individuals have an accurate perception of the threat posed by COVID‐19 is an important condition if individuals are to implement such changes. This appears to be especially the case in the early phases of a pandemic, when information and advice is often sparse and contradictory, but was also important in the presence of mandatory requirements later on, thus indicating that individuals are more likely to comply with government advice and regulations if they have a more accurate risk perception. Furthermore, we expect that risk perceptions will continue to play an important role in the long run. In the absence of vaccines and pharmacological treatments, current social distancing and health‐protective behaviour are likely to remain necessary for many months. Because many individuals infected with COVID‐19 are asymptomatic or have only light symptoms (Bai et al., 2020), surges in infections and fatality manifest themselves after a lag from the time people stop washing their hands thoroughly, start shaking hands, visit crowded places, or go out despite feeling sick. The success of public health strategies will therefore continue to depend on the population to develop and maintain accurate risk perceptions in order to show protective behaviour despite personal psychological, physical, and cognitive fatigue.
Conflicts of interest
All authors declare no conflict of interest.
Author contribution
Christoph Niepel (Conceptualization; Formal analysis; Writing – original draft; Writing – review & editing) Dirk Kranz (Formal analysis; Writing – review & editing) Francesca Borgonovi (Formal analysis; Writing – original draft; Writing – review & editing) Valentin Emslander (Formal analysis; Visualization; Writing – review & editing) Samuel Greiff (Conceptualization; Formal analysis; Writing – original draft; Writing – review & editing).
Supporting information
Table S1. Demographic characteristics for samples N1 (collected from March 13 to 15, 2020) and N2 (collected from April 10 to 12, 2020).
Table S2. List of variables and constituent items.
Acknowledgements
The study was approved by the ethics review panel of the University of Luxembourg (ERP 20‐015 PANIC). Francesca Borgonovi acknowledges support from the British Academy through its Global Professorship programme.
Data availability statement
Data are made available via the OSF platform (see osf.io/sr4wp).
References
- Bai, Y. , Yao, L. , Wei, T. , Tian, F. , Jin, D.‐Y. , Chen, L. , & Wang, M. (2020). Presumed asymptomatic carrier transmission of COVID‐19. JAMA, 323, 1406–7. 10.1001/jama.2020.2565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bish, A. , & Michie, S. (2010). Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. British Journal of Health Psychology, 15, 797–824. 10.1348/135910710X485826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson, N. M. , Laydon, D. , Nedjati‐Gilani, G. , Imai, N. , Ainslie, K. , Baguelin, M. … Ghani, A. C. (2020). Report 9: Impact of non‐pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand. Retrieved from https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf.
- Johns Hopkins University (2020). Coronavirus resource center [Website]. Retrieved from https://coronavirus.jhu.edu.
- Novel Coronavirus Pneumonia Emergency Response Epidemiology Team (2020). Vital surveillances: The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID‐19) — China, 2020. China CDC Weekly, 2, 113–22. [PMC free article] [PubMed] [Google Scholar]
- Oke, J. , & Heneghan, C. (2020). Global Covid‐19 case fatality rates. Retrieved from https://www.cebm.net/covid-19/global-covid-19-case-fatality-rates/. [Google Scholar]
- Rajgor, D. D. , Lee, M. H. , Archuleta, S. , Bagdasarian, N. , & Quek, S. C. (2020). The many estimates of the COVID‐19 case fatality rate. The Lancet Infectious Diseases, 10.1016/S1473-3099(20)30244-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roser, M. , Ritchie, H. , Ortiz‐Ospina, E. , & Hasell, J. (2020). Coronavirus Disease (COVID‐19) – Statistics and Research [Online Resource]. Our World in Data. Retrieved from https://ourworldindata.org/coronavirus.
- Schwarz, N. (1999). Self‐reports: how the questions shape the answers. American Psychologist, 54, 93–105. 10.1037/0003-066X.54.2.93. [DOI] [Google Scholar]
- Sheeran, P. , Harris, P. R. , & Epton, T. (2014). Does heightening risk appraisals change people's intentions and behavior? A meta‐analysis of experimental studies. Psychological Bulletin, 140, 511–43. 10.1037/a0033065 [DOI] [PubMed] [Google Scholar]
- World Health Organization (2020a). Virtual press conference on COVID‐19 – 11 March 2020 [Transcript of press conference]. Retrieved from https://www.who.int/docs/default-source/coronaviruse/transcripts/who-audio-emergencies-coronavirus-press-conference-full-and-final-11mar2020.pdf?sfvrsn=cb432bb3_2.
- World Health Organization (2020b). Coronavirus disease (COVID‐2019) Situation Report 55 [Situation report]. Retrieved from https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200315-sitrep-55-covid-19.pdf?sfvrsn=33daa5cb_6.
- World Health Organization (2020c). Report of the WHO‐China Joint Mission on Coronavirus Disease 2019 (COVID‐19) [Mission report]. Retrieved from https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf.
- World Health Organization (2020d). Coronavirus disease (COVID‐19) advice for the public [Website]. Retrieved from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Demographic characteristics for samples N1 (collected from March 13 to 15, 2020) and N2 (collected from April 10 to 12, 2020).
Table S2. List of variables and constituent items.
Data Availability Statement
Data are made available via the OSF platform (see osf.io/sr4wp).


