Abstract
This essay examines basic functions of crisis decision‐making—cognition, communication, coordination, and control—in response to COVID‐19. This crisis decision‐making framework is applied to cases from South Korea, Italy, and the United States as public officials grapple with how to recognize, respond, and recover from this deadly, invisible threat. The authors acknowledge the harsh trade‐off between the compelling need to limit transmission of the virus to protect public health and the consequent economic losses of halting social interaction. They draw implications from this crisis for better decision‐making and investment in a global information infrastructure system to manage large‐scale, multidisciplinary threats to the health, economy, and sustainability of the world's community of nations. The essay concludes that collective cognition, amplified by timely, valid communication and supported by sound planning, trained personnel, appropriate technology, and bold leadership, enables coordinated action needed to bring a large‐scale global crisis under control.
Evidence for Practice
Invest in information technology to manage systematic data collection, analysis, and modeling.
Provide timely, informed updates on community status to constituents.
Maintain a knowledge base of resources, vulnerabilities, and plans.
In December 2019, a novel coronavirus emerged in China and transmitted illness and death to 210 nations and territories in less than five months, creating a global pandemic. As of May 17, 2020, the World Health Organization (WHO) reported 4,525,497 confirmed cases worldwide, with 307,395 reported deaths corresponding to a case: a fatality ratio of 0.068. Given the initial lack of awareness of the disease, epidemiologists debate the estimated mortality rate, as these figures likely undercount the actual numbers. Delays in recognizing the threat led to an exponential increase in infections and deaths. This rate of increase profoundly challenged government decision makers who are legally responsible for protecting their populations. Although national governments grasped the need for action at varying rates, the rapidity of spread and lethality of the virus severely tested their capacity to manage and control the pandemic. The current risk is cross‐boundary and global.
Central to the challenge of COVID‐19 is the integral relationship between public health and the economy. Without a vaccine, the only known way of stopping the spread of the virus is limiting social interaction through either mitigation or suppression measures (Ferguson et al. 2020). Both are likely to disrupt economic activities significantly, albeit to different degrees. In a global economy with complex transactions and long supply chains, the impact on employment and national debt is enormous. Without robust public health, the economy will falter. If the workforce is sick and consumers are ill, public confidence in production and distribution schedules will drop and economic activity will stall. This cruel trade‐off requires public leaders to search for an elusive balance between reducing the deadly threat to public health and maintaining sustainable economic activity. The complexity of this task compels analysts to reframe this equation on a global scale.
Under the United Nations charter, the WHO has an official role in dealing with global health crises by supporting nations and localities in their crisis response efforts to engage citizens in collective action to reduce risk (WHO 2017). Yet decades of diminished investment by constituent nations and corresponding charges of mismanagement have left the existing international governance mechanisms, such as the WHO, Office for the Coordination of Humanitarian Affairs (OCHA), and Office for Disaster Risk Reduction (UNDRR), without the resources, personnel, monitoring systems or global operational networks necessary to mount an early and effective response. Consequently, the mechanisms for credible search and exchange of valid information to inform decisions and action on multiple scales of operation at the level and speed needed to inform global decision‐making were limited, leaving nations to chart individual courses of action with widely varying results.
Drawing on research from decision‐making in complex, dynamic conditions (Comfort 2007; Hutchins 2000; Kahneman 2011), we examine four basic functions—cognition, communication, coordination, and control—that appear central to government decision processes in all countries as public officials grapple with how to recognize, respond, and recover from this deadly, invisible threat. We follow this discussion with comparative vignettes from three nations as they addressed the threat of COVID‐19, leading to strikingly different outcomes. We conclude with recommendations to invest in a global information infrastructure to enhance cognition as a first step in managing large‐scale, multidisciplinary threats to the health, economy, and sustainability of the world's community of nations.
Decision‐Making in Uncertain Conditions
Public leaders have quintessential responsibility for protecting the lives and livelihoods of their constituents. In routine times, they may follow time‐honored procedures honed over decades of experience, confident that lessons from the past will guide them (Kettl and Fesler 2008). For public leaders facing unknown risks, decision‐making is fraught with uncertainty and becomes an adaptive process that has four distinct components: (1) cognition, (2) communication, (3) coordination, and (4) control (Comfort 2007). Under conditions of COVID‐19, how public leaders exercised these four functions proved critical in different contexts.
Cognition
In crisis management, cognition is the “capacity to recognize the degree of emerging risk to which a community is exposed and to act on that information” (Comfort 2007, 189). Importantly, cognition provides the transition to action. It constitutes not simply the perception of risk to self but also comprehension of the risk to others (Fligstein and McAdam 2012). That is, action taken may help oneself, but action not taken may irretrievably harm others. The fundamental component of empathy in cognition creates a human connection to others who share the risk and spurs collective action for the benefit of the community as a whole.
Public leaders had difficulty recognizing the depth, scale, and lethality of COVID‐19. From the first slow, sobering discovery of the virus as it emerged in Wuhan, China, to the broad determination that ordinary methods of treating the novel coronavirus were ineffective, cognition came late to public leaders in individual countries as they searched unsuccessfully through old models of dealing with contagion. By the time public leaders recognized the lethality of COVID‐19, it was already spreading silently in their communities. While measures to suppress social interaction slowed the spread of the virus, they also created a cruel trade‐off by shutting down schools, travel, commerce, and cultural activities that make societies function.
Communication
Communication is defined as a process that links sender and receiver in shared comprehension of messages (Luhman 1989). In doing so, communication creates shared meaning among actors with different roles. It is the means used to inform partner agencies in the global community as well as the public in different nations about the potential risk and rationale for evidence‐based mitigation measures and the need for collective response. Effective communication to explain COVID‐19 to the public as an invisible, novel, deadly threat requires strong leadership, timely and evidence‐based information, and trust to build broad public consensus to support collective action (Ansell, Boin, and Keller 2010; Kapucu 2006).
Coordination
Coordination is defined by the degree to which organizations align their resources, tasks, and time to engage in interdependent functions to achieve a shared goal (Comfort 2007). In complex environments, coordination requires articulation of shared goals among diverse actors in response to shared risk. Coping with the risk of COVID‐19, each nation faced decisions about how to align the components of their respective national response systems in ways that would slow or stop transmission of the virus, actions that would also contribute to the global goal. Public leaders build trust with their constituents through timely, informed communication, enabling citizens to accept the validity of proposed actions for both self and community and to act, collectively, under the extraordinary constraints of crises.
Control
Control is defined as the capacity to respond to an external threat and still maintain regular operations in the society (Comfort 2007, 2019). In reference to COVID‐19, control means achieving a reasonable balance between mitigating the spread of the infection, building health care capacity, and managing a safe level of economic and social activity. The global crisis generated by COVID‐19 requires coordination not only across jurisdictional boundaries within countries but also across national boundaries to bring this massive pandemic under effective control.
The following section briefly characterizes the policy actions taken by three countries in response to the threat of COVID‐19 but focuses on the function of cognition as the initial step toward building effective communication, coordination, and control of the pandemic.
South Korea
South Korea's previous experience with MERS (Middle East respiratory syndrome) in 2015 significantly increased the level of cognition of COVID‐19 as a severe risk for individuals as well as for government agencies. The MERS experience taught Korean decision makers primary lessons regarding prevention and mitigation of community infection, especially at hospitals; clarification of the command center functions, which became the Korean Center for Disease Control and Prevention (KCDC); and information sharing among ministries, local governments, and citizens using advanced information technology (Moon 2020).
Recognizing early on the risk of community infection from the progress of COVID‐19 in China, the KCDC started to strengthen surveillance for pneumonia cases in health facilities nationwide from January 3, 2020. Moving quickly, the KCDC began to develop analysis and testing methods for COVID‐19 on January 13. Private medical companies such as Seegene also started to develop the test kits on January 21. The KCDC issued emergency use authorization on February 12 within a week after the application for the approval of Seegene. With rapid development of test kits, South Korea reduced the time required for testing for presence of infection from 24 to 6 hours.
Controversies arose when the KCDC reported the first confirmed patient, a Chinese national traveler who resided in Wuhan. Many citizens, as well as opposition parties, called for banning travelers from China and intensive preventive measures. The KCDC scaled the national alert level from blue (level 1) to yellow (level 2) but did not adopt the travel ban policy following the WHO recommendation on January 23. Instead, the Ministry of Foreign Affairs increased the level of travel alert to level 2 and asked for high caution in traveling to Wuhan. Almost two weeks later (February 4), the Korean government banned entry of travelers from Wuhan, but not all of China. The Korean government also checked the health status of entrants from overseas and used information and communications technologies to deliver information and identify contacts.
The second outbreak of COVID‐19 emerged on February 17 as a result of the Shincheonji (religious cult group) community infection in Daegu Province. Well aware of the risk of escalating the infection, the Korean government raised its national alert level to the highest level (level 4) and tested all religious groups in Daegu Province. With the quick development of test kits, the KCDC could test more than 10,000 suspected cases every day and continuously increased the number up to 18,000 tests per day in early March.
At the same time, the Korean government and civil society began to coordinate limited medical resources. While the national health insurance program provides full access to medical services for all people regardless of income, the local government did not have sufficient medical staff and hospital beds. Responding to the immediate challenge, local governments less affected by COVID‐19 took patients from Daegu, and hundreds of doctors and nurses volunteered to take care of patients. Private companies and hospitals provided their facilities as special units for taking light‐symptom patients. More than 180,000 citizens volunteered to help patients and support local communities between January 20 and March 17. Government agencies worked with pharmacies to distribute masks to the public (Government of the ROK 2020b).
Extensive information sharing between local governments and citizens developed and maintained collective cognition of the disease as public risk. Before mid‐February, the KCDC traced contacts of infected people manually. In early February, the Korean government quickly developed the COVID‐19 Smart Management System (SMS), which analyzes data from 28 public as well as private organizations, such as credit card companies and smartphone companies. Using this system, the KCDC could analyze any movement of infected patients within 10 minutes and share that information with citizens through cellphone text messages. The SMS evoked the issue of privacy (Park, Choi, and Ko 2020), but use of the technology was supported by the public and politicians who had experienced the risk of community infection during MERS. This technology supported rapid communication among citizens, enabling collective action to protect both themselves and the larger community to move toward control (Government of the ROK 2020a). Rapid cognition enabled Korean officials to move quickly through communication and coordination to control.
Italy
Cognition of the risk of COVID‐19 came to different groups at different times in Italy. On January 30, 2020, two Chinese tourists were hospitalized for COVID‐19 in Rome after traveling from Malpensa Airport in northern Italy. On January 31, 2020, the prime minister issued a national state of emergency according to Decree 1/2018 and appointed the head of the National Department of Civil Protection to be commissioner in charge of the COVID‐19 response. 1
The first phase of the emergency consisted mainly of coordination between the central government and regional governors and between the Department of Civil Protection and the Ministry of Health. The emergency declaration did not trigger any special change in public life or hospital and health care operations. When a state of emergency was declared, all flights, including cargo, from and to China were banned. However, incoming travelers from China could still enter the country from intermediate destinations in Europe and elsewhere.
On February 19, 2020, the first person from a small town 70 kilometers south of Milan was found to be severely ill from COVID‐19. The Italian government recognized the severity of this discovery, but several problems affected its capacity to translate such understanding into decisions before issuing a total lockdown of the country. The Italian health care system is very stressed and working to near capacity in ordinary conditions. The buffer for emergencies in intensive care units is practically nonexistent (Grasselli, Presenti, and Cecconi 2020) and burdened by poor response capacity of peripheral hospitals and a lack of emergency plans (Villa et al. 2020).
Timely cognition was hampered by the mixed patterns of communication to the public regarding measures to suppress the infection and the chaotic, puzzling debate they generated. Public leaders at all levels issued opposing opinions and statements. Contrasting views and interpretations by experts in virology, epidemiology, and medicine created an environment characterized by mixed feelings of fear and anxiety for many people, distrust and skepticism by others. In this situation, information provided daily by the Department of Civil Protection and the National Institute of Health about COVID‐19 virus diffusion in Italy was crucial. Only a few Italian regions (Piedmont, Umbria, and Molise) implemented specific tools to collect and share COVID‐19 data for all municipalities. Such platforms proved to be useful not only for the public but also for emergency managers and medical staff, as it permitred early detection of potential hot spots of infection and consequent needs for health care both at home and in hospitals.
Difficulties in operationalizing surveillance and preventive measures derived from the lack of coordination between central government and regions. The resulting tension is exacerbated when, as in the present situation, the political parties leading administrative operations at different government levels are on opposite sides. Conflict resulted when the central government wished to impose closure and governors opposed it. When the number of deaths and the crisis in hospitals escalated, the latter issued more restrictive orders than the central government.
Four days after the first Italian COVID‐19 patient was hospitalized on February 23, 10 municipalities south of Milan and one municipality in the Veneto region were quarantined, all commercial activities were closed, and public gatherings were prohibited. Two weekends after the first partial closure measures, the number of infected cases increased exponentially. In 24 hours, on March 8, the government moved from closing the Lombardia region and 14 provinces of the center‐north region of Italy to issuing a national stay‐at‐home order and closure of all gatherings, schools, and nonessential business activities. On March 22, the government extended the closures until May 4. A plateau in the number of patients hospitalized in intensive care units was reached on March 15 in Lombardia and on March 18 in Italy. The Lombardia region proved to be the epicenter of the contagion, with 75,134 cases as of April 29 (Manca 2020).
By mid‐May, the plan for reopening the country mainly consisted of a calendar for gradual reactivation of businesses. Confusion persists regarding the many guidelines circulating within individual organizations and among regions that are not always consistent. Information regarding reopening was provided late, as occurred with all preceding decrees. Decree 33 issued on May 16 provided indications regarding mobility within regions and internationally, but specific norms were not provided for businesses (Dwyer 2020). The report prepared for the Italian government to support the entrance into reopening was not made publicly available, and only partial and fragmented elements of it have been reported by newspapers. Still lacking is a strategy that connects economic rebooting, technical and financial support to enact the many restrictions that will impact business productivity, monitoring and surveillance indicators, and practical tools to be used for tracing new surges and mapping the epidemic through a testing plan.
United States
The U.S. response to COVID‐19 was slow in comparison with other countries. Only in mid‐March 2020 did the federal government and the general public begin to acknowledge the seriousness of the disease and act in accordance. Cognition and the subsequent response were hampered by three interrelated issues. First, the Donald Trump administration downplayed the gravity of the situation. Through both press conferences and conservative media outlets, the early talking points were that the United States had the virus under control and that it posed no more threat than the flu (Leonhardt 2020). Second, the U.S. capacity to identify and respond to global pandemics had been dramatically reduced over the past two years (Sun 2018). The White House National Security Council's Directorate for Global Health Security and Biodefense was disbanded, and a key homeland security adviser focused on biodefense strategies against pandemics was removed (Lopez 2020). These key actors in the pandemic response system have not been replaced. Third, and most critically, the United States lacked the testing capacity needed to understand the extent, and contain the spread, of the virus. Initial concerns of community spread in the United States were confirmed on February 29, when the first known U.S. resident died. Because the individual had not been exposed through travel, health officials feared that community spread was occurring across the country.
Despite these concerns, testing capacity lagged. By mid‐March, U.S. testing capacity ranked last among eight developed nations (Resnick and Scott 2020). Reasons for the lack of testing capacity in the United States were numerous and included the initially faulty tests produced by the Centers for Disease Control and Prevention (CDC) in February. As testing capacity slowly became available, only those who had traveled to China were eligible to be tested. Despite ongoing community transmission, most citizens, even those experiencing symptoms, could not be tested under CDC guidelines. Those guidelines were not updated to facilitate wider testing until March 4 (CDC 2020). At that time, the United States had conducted fewer than 2,000 tests; in comparison, South Korea, a country one‐sixth its size, had conducted 140,000 (Meyer and Madrigal 2020). Without adequate capacity to test, the disease spread relatively undetected and hampered cognition. The artificially low case count provided many public officials with false assurance that COVID‐19 was not a serious threat. On March 25, the WHO indicated that the United States, with roughly 65,000 cases, would become the global epicenter of the pandemic (Quinn 2020). By early April, the country had more than 250,000 confirmed cases and 5,000 deaths.
The initial federal response focused on travel restrictions to and from China and Europe but lacked a broader national coordinated effort to mitigate the spread. In mid‐March, the CDC released guidelines advocating that all events of 50 or more people be canceled, and the president advised people to avoid gatherings of 10 or more. Given the federal structure of the government, and without national stay‐at‐home orders, states varied considerably in the timing and extent of interventions used to combat the spread of COVID‐19 (Science News Staff 2020). By March 13, several states, including Pennsylvania and Michigan, announced plans to close their schools. On March 19, California became the first state to issue a statewide stay‐at‐home order. Several states quickly followed, while others delayed decisions until April. Eight states, all with Republican governors, chose not to issue stay‐at‐home orders for all residents (John 2020). Lack of federal‐level interventions and mixed communication from the Trump administration culminated in a patchwork of policies that varied from state to state and even within states.
Extreme differences in state policy response created confusion and frustration among the public regarding the risk posed by COVID‐19. Protests were held in several states by citizens demanding that stay‐at‐home orders be lifted (Bosman, Tavernise, and Baker 2020). Despite warnings by public health officials, several states decided to reopen their economies by the end of April, much earlier than recommended. Public health officials as well as the WHO warned that reopening the economy and lifting stay‐at‐home orders early would likely escalate infections (Chiu 2020). Lack of federal interventions coupled with an absence of national testing and equipment sourcing strategies pushed states to coordinate response efforts on their own (Science News Staff 2020; Segers, O'Keefe, and Navarro 2020).
Overall, the impact of the virus on the U.S. economy has been devastating. In the first quarter of 2020, the U.S. stock market experienced one of its worst declines. As the stock market plummeted, so, too, did employment rates. Data from the U.S. Department of Labor indicated that during the five‐week period from March 14 to April 18, more than 26 million unemployment claims were filed. On March 27, the president signed a $2.2 trillion stimulus bill to assist families and companies suffering from the pandemic. By May 17, the number of cases surged to more than 1,474,127 with 88,898 deaths. Slow cognition of the risk led to mixed patterns of communication and lack of coordination at the national level, resulting in devastating losses in lives and economic costs.
Figure 1 shows the rates of increase, days to peak, and decline in the number of infected cases in South Korea, Italy, and the United States. 2 The findings document in stark detail the differences in results from decision‐making patterns among the three countries. The four functions identified in crisis decision‐making emerged in all three countries, but in a massive crisis, the function of cognition set the trajectory for the functions of communication and coordination, leading to control.
Figure 1.
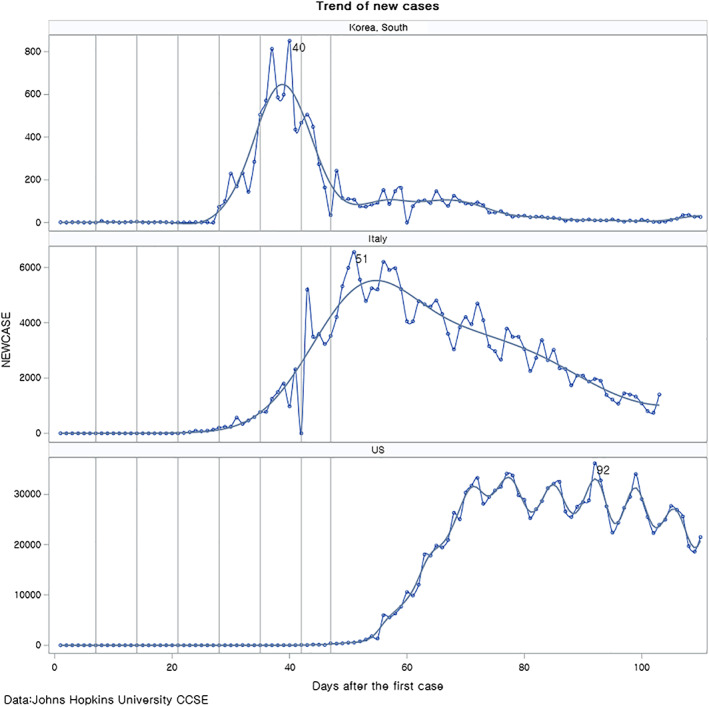
Trend Analyses COVID‐19 Cases
In South Korea, earlier experience with MERS alerted decision makers to the serious risk of a novel coronavirus, and decision makers quickly recognized the risk, communicated it to the public clearly and consistently, and acted decisively to limit the spread of the virus, lessening the number of lives lost and economic damage to the country. In Italy, the first European country to face the pandemic, initially slow cognition hampered clear communication and led to lack of coordination between regions and the central government, delaying the decision for strong suppression measures taken only when the increase in the number of cases exceeded the capacity of the health system in Lombardy. The U.S. case shows dramatically the cost of late cognition, marked by two months of mixed, unclear communication at the federal level, leading to a lack of coordination between federal and state governments in trying to bring the virus under control.
Conclusion
The dilemma between public health and economic functions remains at both the global and national scales. The global pandemic unleashed on the world by COVID‐19 creates a fundamental test of public values for leaders and decision makers both within and between nations. This harsh test reveals the collective responsibility that we share for self and others in uncertain situations of shared risk and the critical role of leadership in decision‐making and mobilizing collective action. It demonstrates the critical role of cognition in precipitating action, as the three countries revealed very different patterns of performance after identifying their first cases of the disease. South Korea already had plans in place after the 2015 MERS threat and quickly devised new programs and policies to strengthen existing capacity in response to COVID‐19. Italy identified the threat of the pandemic early but had several weaknesses in preparedness and health care capacity that did not allow its early recognition to translate into effective practical interventions. The United States faced a critical fragmentation in cognition between scientific experts and political leaders that delayed substantive action at the federal level for over two months, leading to exponential increases in both cases and deaths. These divergent degrees of cognition led to mixed patterns of communication at the federal level and fractured efforts at coordination across a large country, while leadership at state and municipal levels gained the trust and support of their citizens and the large majority, 70 percent of U.S. residents, supported stay‐at‐home policies (Wise 2020).
The three cases show that cognition alone does not achieve collective action and control within countries in a global pandemic crisis. Rather, cognition needs to be supported by a rigorous technical capacity and actionable management frameworks for national and international communication and coordination with respect to collecting data, sharing good practices, and monitoring levels of coping capacity. Each nation has a responsibility not only to its own citizens, but also toward other nations in the global community by implementing preparedness plans and making investments to strengthen their health care systems and the system of international organizations.
The COVID‐19 pandemic reveals a rare opportunity to redesign global and national systems for managing deadly risks, using science‐based evidence and information communication technology, to identify, track, search, and share timely, valid data among nations, triggering innovation and collective action to build a resilient international community. Bold redesign of existing international organizations—the WHO, OCHA, and UNDRR—that monitor and compare the status of global risk would reinforce cognition in facilitating effective crisis response across the globe by partnering with nations to work with their local communities.
Enhanced coordination and exchange of good practices among member nations of the global community would save not only hundreds of thousands of lives but forgo trillions of dollars in economic losses, anguish, and pain. It would mean expanding networks of research, collaboration, and knowledge sharing among the world's scientists, scholars, public managers, and students in shared exploration of means for identifying and reducing emerging risks. It would include building and maintaining a global information infrastructure to support continuous learning and adaptation to a changing environment for both professional practitioners and researchers. It would involve designing and implementing plans for a global health infrastructure and training the personnel who would staff and maintain it, with secure funding sustained by responsible international contributions and oversight.
Building a global information infrastructure to support timely, coordinated decision‐making and iterative learning in public health is not an easy task, but the world's nations designed the United Nations, the Marshall Plan, Organisation for Economic Co‐operation and Development, and security alliances after World War II. With insight gained from the precedent‐shattering experience of this pandemic and bold public leadership, nations of the world have a unique policy window for transforming global governance capacity to strengthen and maintain public health and, reciprocally, sustain the global economy.
Biographies
Louise K. Comfort is professor in the Graduate School of Public and International Affairs at the University of Pittsburgh and fellow of the National Academy of Public Administration. Her research interests include decision‐making under conditions of uncertainty and rapid change, sociotechnical systems under stress, and uses of information technology to support public managers operating in urgent conditions. Her most recent book is The Dynamics of Risk: Changing Technologies and Collective Action in Seismic Events (Princeton University Press, 2019).
Email: lkc@pitt.edu
Naim Kapucu is Pegasus Professor of public administration and policy and director of the School of Public Administration at the University of Central Florida. His research interests are emergency and crisis management, decision‐making in complex environments, network governance, and leadership. His work has been published in Public Administration Review, Journal of Public Administration Research and Theory, American Review of Public Administration, and Disasters, among other journals. He teaches network governance, leadership, and methods.
Email: kapucu@ucf.edu
Kilkon Ko is professor in the Graduate School of Public Administration at Seoul National University, Seoul, Korea. He is editor in chief of the Asian Journal of Political Science. His teaching areas include organizational theory, program evaluation in the public sector, public policy theories and application, public administration in Asia, research methods, theories of public administration, the policy‐making process, corruption, and ethics.
Email: kilkon@gmail.com
Scira Menoni is professor at the Politecnico di Milano, Italy, teaching risk assessment and management and related topics; she also teaches a course at Geneva University, Switzerland. She has coordinated European Union–funded projects on postdisaster damage assessment and led a partners' unit in a Horizon 2020 project on culture, cities, and catastrophes. She has worked on projects in Central America and Mexico. She is a consultant for the Italian Ministry of Environment, the Lombardia and Umbria regions, and the Catalunya Civil Protection in Spain.
Email: scira.menoni@polimi.it
Michael D. Siciliano is associate professor of public administration at the University of Illinois at Chicago and codirector of the Networks and Governance Lab. He studies how humans and organizations collaborate to improve society. His work explores the cognitive, social, and institutional factors influencing the formation and performance of networks in the public sector.
Email: sicilian@uic.edu
Notes
Official information regarding both issued decrees, the declaration of a state of emergency, and the overall situation day by day can be found on the website of the National Department of Civil Protection (also available in English): http://www.protezionecivile.gov.it/home.
Data are reported to the Johns Hopkins University Coronavirus Resource Center (https://coronavirus.jhu.edu/) from multiple credible sources, including the WHO, and represent the best data available. Yet the data likely include errors and undercount the extent of actual cases and deaths because of inadequate reporting in separate nations and states.
References
- Ansell, Chris , Boin Arjen, and Keller Ann. 2010. Managing Transboundary Crisis: Identifying the Building Blocks of an Effective Response System. Journal of Contingencies and Crisis Management 18(4): 196–207. [Google Scholar]
- Bosman, Julie , Tavernise Sabrina, and Baker Mike. 2020. Why These Protesters Aren't Staying Home for Coronavirus Orders. New York Times, April 23. https://www.nytimes.com/2020/04/23/us/coronavirus‐protesters.html [accessed June 16, 2020].
- Centers for Disease Control and Prevention (CDC) . 2020. Update and Interim Guidance on Outbreak of Coronavirus Disease 2019 (COVID‐19). February 28. https://emergency.cdc.gov/han/2020/HAN00428.asp [accessed June 7, 2020].
- Chiu, Allyson . 2020. Fauci Warns States Rushing to Reopen: “You're Making a Really Significant Risk.” Washington Post, May 1. https://www.washingtonpost.com/nation/2020/05/01/fauci‐open‐states‐coronavirus/ [accessed June 16, 2020].
- Comfort, Louise K. 2007. Crisis Management in Hindsight: Cognition, Communication, Coordination, and Control. Special issue. Public Administration Review 67: 189–97. [Google Scholar]
- Comfort, Louise K . 2019. The Dynamics of Risk: Changing Technologies and Collective Action in Seismic Events. Princeton: Princeton University Press, Studies in Complexity. Princeton, NJ: Princeton University Presss. [Google Scholar]
- Dwyer, Colin . 2020. Italy Plans to Lift Some Travel Restrictions Early Next Month. National Public Radio, May 16. https://www.npr.org/sections/coronavirus‐live‐updates/2020/05/16/857367413/italy‐plans‐to‐lift‐some‐coronavirus‐travel‐restrictions‐early‐next‐month [accessed June 7, 2020].
- Ferguson, Neil , et al. 2020. Report 9: Impact of Non‐pharmaceutical Interventions (NPIs) to Reduce COVID‐19 Mortality and Healthcare Demand. Imperial College COVID‐19 Response Team, March 16. https://www.imperial.ac.uk/mrc‐global‐infectious‐disease‐analysis/covid‐19/report‐9‐impact‐of‐npis‐on‐covid‐19/ [accessed June 16, 2020].
- Fligstein, Neil , and McAdam Doug. 2012. A Theory of Fields. Oxford: Oxford University Press. [Google Scholar]
- Government of the Republic of Korea (ROK) . 2020a. How Korea Responded to a Pandemic Using ICT: Flattening the Curve on COVID‐19. April 15. http://www.moef.go.kr/com/cmm/fms/FileDown.do?atchFileId=ATCH_000000000013739&fileSn=2 [accessed June 7, 2020].
- Government of the Republic of Korea (ROK) . 2020b. Tackling COVID‐19: Health, Quarantine and Economic Measures of South Korea. March 31. https://ecck.eu/wp‐content/uploads/2020/03/Tackling‐COVID‐19‐Health‐Quarantine‐and‐Economic‐Measures‐of‐South‐Korea.pdf [accessed June 7, 2020].
- Grasselli, Giacomo , Pesenti Antonio, and Cecconi Maurizio. 2020. Critical Care Utilization for the COVID‐19 Outbreak in Lombardy, Italy. JAMA 323(16): 1545–6. [DOI] [PubMed] [Google Scholar]
- Hutchins, Edwin . 2000. Cognition in the Wild. Cambridge, MA: MIT Press, 4th Printing. [Google Scholar]
- John, Arit . 2020. These Eight States Haven't Issued Stay‐at‐home Orders to Fight the Coronavirus Outbreak. Los Angeles Times, April 22. https://www.latimes.com/politics/story/2020‐04‐22/states‐without‐coronavirus‐stay‐at‐home‐order [accessed June 7, 2020].
- Kahneman, Daniel . 2011. Thinking, Fast and Slow. New York: Farrar, Straus and Giroux. [Google Scholar]
- Kapucu, Naim . 2006. Interagency Communication Networks during Emergencies: Boundary Spanners in Multiagency Coordination. American Review of Public Administration 36(2): 207–25. [Google Scholar]
- Kettl, Donald F , and Fesler James. 2008. The Politics of the Administrative Process, 4th ed. Washington, DC: CQ Press. [Google Scholar]
- Leonhardt, David . 2020. A Complete List of Trump's Attempts to Play Down the Coronavirus. New York Times, March 15. https://www.nytimes.com/2020/03/15/opinion/trump‐coronavirus.html [accessed June 16, 2020].
- Lopez, German . 2020. The Trump Administration's Botched Coronavirus Response, Explained. Vox, April 2. https://www.vox.com/policy‐and‐politics/2020/3/14/21177509/coronavirus‐trump‐covid‐19‐pandemic‐response [accessed June 7, 2020].
- Luhman, Niklas . 1989. Ecological Communication. Chicago: University of Chicago Press. [Google Scholar]
- Manca, Davide . 2020. Dynamics of ICU Patients and Deaths in Italy and Lombardy due to Covid‐19 Analysis Updated to 30‐March, Day #38 Evening. Short Communication. April 1. https://www.esahq.org/esa‐news/dynamics‐of‐icu‐patients‐and‐deaths‐in‐italy‐and‐lombardy‐due‐to‐covid‐19‐analysis‐updated‐to‐30‐march‐day‐38‐evening/ [accessed June 16].
- Meyer, Robinson , and Madrigal Alexis C.. 2020. Exclusive: The Strongest Evidence Yet That America Is Botching Coronavirus Testing. The Atlantic, March 6. https://www.theatlantic.com/health/archive/2020/03/how‐many‐americans‐have‐been‐tested‐coronavirus/607597/ [accessed June 16, 2020].
- Moon, M. Jae. 2020, Fighting COVID‐19 with Agility, Transparency, and Participation: Wicked Policy Problems and New Governance Challenges. Public Administration Review 80(4): 651–656. 10.1111/puar.13214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park, Sangchul , Choi Gina Jeehyun, and Ko Haksoo. 2020. Information Technology–Based Tracing Strategy in Response to COVID‐19 in South Korea—Privacy Controversies. JAMA 323(21): 2129–30. [DOI] [PubMed] [Google Scholar]
- Quinn, Colm . 2020. Is the United States the Cornavirus Pandemic's New Epicenter? Foreign Policy, March 26. https://foreignpolicy.com/2020/03/25/united‐states‐coronavirus‐pandemic‐new‐epicenter/ [accessed June 7, 2020].
- Resnick, Brian , and Dylan Scott 2020. America's Shamefully Slow Coronavirus Testing Threatens All of Us. Vox, March 12. https://www.vox.com/science‐and‐health/2020/3/12/21175034/coronavirus‐covid‐19‐testing‐usa [accessed June 7, 2020].
- Science News Staff . 2020. The United States Leads in Coronavirus Cases, but Not Pandemic Response. Science, April 1. https://www.sciencemag.org/news/2020/04/united‐states‐leads‐coronavirus‐cases‐not‐pandemic‐response [accessed June 7, 2020].
- Segers, Grace , O'Keefe Ed and Aaron Navarro. 2020. States Move Forward with Coordinating Coronavirus Response after Trump Backs Down. CBS News, April 15. https://www.cbsnews.com/news/coronavirus‐states‐coordinating‐response‐reopening‐new‐york‐trump/ [accessed June 7, 2020].
- Sun, Lena H . 2018. Top White House Official in Charge of Pandemic Response Exits Abruptly. Washington Post, May 10. https://www.washingtonpost.com/news/to‐your‐health/wp/2018/05/10/top‐white‐house‐official‐in‐charge‐of‐pandemic‐response‐exits‐abruptly/ [accessed June 16, 2020].
- Villa, Simone , Andrea Lombardi, Davide Mangioni, Giorgio Bozzi, Alessandra Bandera, Andrea Gori, and Mario Raviglione. 2020. The COVID‐19 Pandemic Preparedness or Lack Thereof: From China to Italy. Global Health & Medicine 2(2): 73–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wise, Justin . 2020. Poll: More than 70 Percent of Americans Support Coronavirus Stay‐at‐Home Orders. The Hill, April 21. https://thehill.com/homenews/state‐watch/494028‐poll‐more‐than‐70‐percent‐of‐americans‐support‐stay‐at‐home‐orders [accessed June 16, 2020].
- World Health Organization (WHO) . 2017. Emergency Response Framework, 2nd ed. Geneva: World Health Organization. https://www.who.int/. [Google Scholar]


