1.
We describe the case of a patient with severe haemophilia A who underwent major orthopaedic surgery managed postoperatively by telemedicine (TM). The case is a splendid example of the implementation of TM and good collaboration between a Comprehensive Hemophilia Treatment Center (CHTC) and a local hospital.
This is a 56‐year‐old patient diagnosed with severe haemophilia A without an inhibitor. The patient's medical background includes HBV infection, HCV (treated and cured) and HIV positive under treatment with highly active antiretroviral therapy (HAART). Due to severe, painful and disabling bilateral knee arthropathy, the patient underwent surgery for a left total knee arthroplasty (TKA) in January 2013, followed by a right TKA in 2015. The left TKA had become painful at the last annual check‐up, and X‐rays showed severe loosening of the prosthetic components. The patient also had a pronounced arthropathy in the elbows and ankles. The patient was being treated with rFVIII tertiary prophylaxis at 40 IU/kg every 48 hours. In January 2020, the first stage of a two‐stage revision arthroplasty of the left TKA was performed with suspected infection (not confirmed) by implanting an articulated spacer. On 9 March, he was admitted for the second stage of revision to the left knee. Although the situation was becoming more complex in our hospital due to the spread of COVID‐19, we decided to perform the surgery given that the patient had already travelled to the hospital. On 10 March, a long‐stem tumoral prosthesis was implanted, and this was because resection of the distal femur was required due to severe osteolysis secondary to prosthetic loosening (Figure 1A). A bolus of rFVIII was administered preoperatively at a dose of 50 IU/kg, followed by continuous infusion. Preinfusion FVIII levels were 1.8%; no inhibitor was detected with a Cmax 181.9% after 20 minutes. Four hours after surgery, the patient presented an FVIII level of 113.5%. Twenty‐four hours after surgery, having assessed the risk/benefit of admission, it was decided to discharge the patient from hospital for safety reasons, due to the high risk of infection with SARS‐CoV‐2. At that moment, given the progression of the pandemic, the Orthopaedic Surgery Department wards would be handed over to care for COVID‐19 patients, at that point 80% occupied by such patients. The patient's blood test from that morning presented Hb 12.7 g/dL and a FVIII level of 92.3%. Physical examination: Surgical wound of good aspect, without signs of bleeding, range of movement on sagittal plane (ROM): complete extension and 30° flexion, quadriceps force 3‐/5 (according to MRC muscle strength scale), transfers of weight using supports. Postoperative X‐ray showed that the prosthesis had been correctly implanted.
Figure 1.
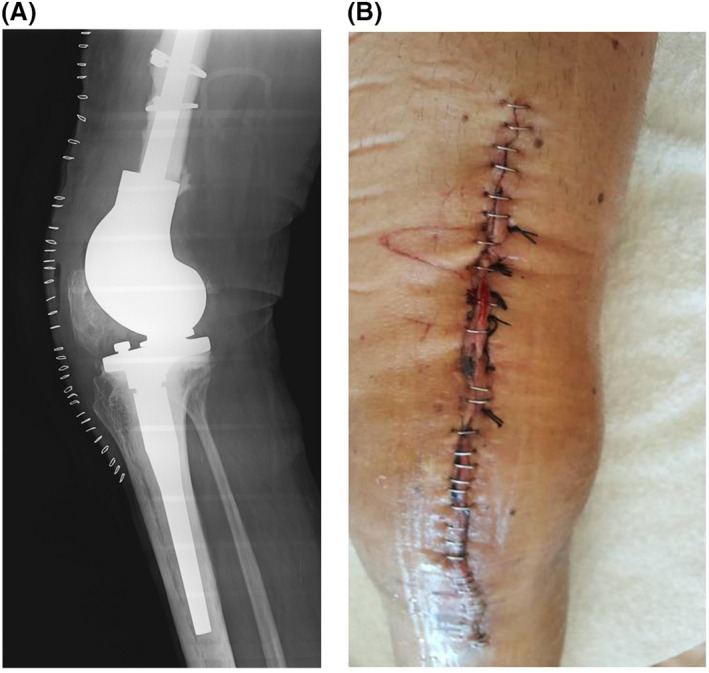
Figure 1, A Lateral radiograph of the long‐stem tumoral prosthesis implanted in the left knee due to severe loosening of the primary prosthesis. B, Left knee on day+3.
Given the impossibility of maintaining continuous infusion during the transfer to his centre, the patient was switched to 40 IU/kg bolus infusions every 8 hours for 2 days until contacting the regional hospital in his home town to adjust treatment depending on FVIII levels, continuing treatment as per Table 1. The patient was transferred by ambulance to his home town, 400 km away from our hospital. On the same day, we contacted the patient upon his arrival to assess bleeding, pain experienced during the trip and to record constants such as BP and temperature. These were checked three times a day for the first 10 days. The patient reported that he had had no bleeding during the journey home and that the pain had been well controlled with metamizole.
Table 1.
Haematological postoperative protocol used in this patient
| Days postsurgery | FVIII levels | Dose guidelines |
|---|---|---|
| +1 | 92.3% | 40 IU/kg/8 h |
| +3 | FVIIIb: 60% Cmax FVIII: 170% | 40 IU/kg/12 h |
| +6 | FVIIIb: 89% Cmax FVIII:159% | 25 IU/kg/12 h |
| +9 | FVIIIb: 55% Cmax FVIII:111% | 25 IU/kg/12 h |
| +13 | FVIIIb: 43% Cmax FVIII:110% | 37 IU/kg/24 h |
| +16 | FVIIIb: 21% Cmax FVIII:139% | 37 IU/kg/48 h |
FVIIIb: level FVIII before infusion, Cmax FVIII 20 min after infusion
Upon discharge of the patient, the Rehabilitation Department set out its guidelines for analgesic and physical therapy to encourage early recovery of the knee. This included assisted mobilizations, progressive muscle strengthening of the quadriceps, proprioception exercises and re‐education of gait using technical aids. After 4‐6 weeks, it was recommended that he start working on stairs and ramp exercises.
During the early postoperative phase, haematologists, physiatrists and orthopaedic surgeons participated in daily videoconferences to communicate with the patient. Physiatrist assessed the progress in joint mobility and haematologists the presence of bleeding. During the late postoperative period, the patient was assessed by emailing the images of his knee and the haematologists adjusted the treatment in coordination with the local haematologist.
The only complications were a subcutaneous haematoma on the lateral side of the left thigh on day + 6; we assessed this using photographs sent by the patient (Figure 1B), with full resolution three days later, bleeding from one of the sutures during a dressing change (day + 14) and an isolated Cutibacterium acnes in periprosthetic skin tissue, which was considered to be contamination, as the patient had no signs of local or systemic infection.
The patient was in daily email contact with our Hematology Department, which in turn kept in close contact with the regional hospital haematologist to adjust treatment as necessary. Samples of blood to track FVIII dosage were taken at the patient's home, and he was later informed of the new treatment guideline by our Hemophilia Unit. Physiotherapy sessions were conducted remotely online with the help of the patient's relatives. On day + 26, the patient was pain free. He had reached 90º flexion, showed good motor control and was walking 2000 steps a day with the help of two canes. Now, the patient is fully recovered by walking 300 metres a day in his home environment due to the current nationwide lockdown. He will soon start exercising with stairs and obstacles. The patient has already returned to working from home.
Telemedicine (TM), defined as the provision of healthcare services remotely, is an expanding discipline, 1 although it is less commonly used in Spanish state‐run hospitals than we would hope. This is mainly due to legal barriers that seek to protect confidentiality and patient data; economic barriers, given the high costs of implementation; and sometimes psychological barriers both for the patient and for the health professionals who tend to prefer face‐to‐face visits.
Since June 2019, our hospital has been working on the implementation of a TM model in the Haemostasis Unit, currently focusing on the most prevalent pathologies such as ITP or venous thromboembolic disease.
Our hospital is one of the largest healthcare centres in the Spanish public network and is therefore one of the hospitals that have treated the most patients with COVID‐19 during the last two months, with an average of 900 patients hospitalized per day.
Early on in the health crisis, we designed a protocol to facilitate TM programmes for patients with congenital coagulopathies. The objective was to keep patients, many of whom were immunocompromised, such as the case in this study, away from the hospital to minimize the risk of infection from SARS‐CoV‐2.
Great progress in TM, such as videoconferencing, audiovisual link and remote patient‐monitoring tools, has always been achieved in times of crisis. Its application in the hospital routine will allow patients to address healthcare issues quickly and offers medical staff a continuous flow of real‐time patient's health data. 2 , 3 So, the healthcare situation caused by COVID‐19 has accelerated the rapid implementation of these services, even for the management of this disease. 4 In this sense, we consider telemedicine to be a good strategy for monitoring patients who, following the recommendations of the World Federation of Haemophilia, should not attend hospital. 5
The above case is a good example of interaction between a CHTC formed by a team of professionals (orthopaedic surgeons, physiotherapists, haematologists and nurses) specializing in the management of patients with congenital coagulopathies and a regional hospital with professionals who attend patients with very diverse pathologies.
There is not much experience in literature regarding the use of TM for haemophilia patients, but the little evidence that there is highlights that it is very useful for patients who live a long distance from the CHTC as in the case with the patient described. 6 , 7 , 8 , 9 However, the global pandemic situation we are experiencing is likely to change the attitude towards remote consultations, both for patients and for professionals alike.
According to Valentino et al, in the context of a pandemic, TM has the potential to increase convenience and facilitates access of patients to medical specialists, improves patient safety and allows better budget management, limiting exposures to patients while reducing the burden on healthcare facilities allowing them to deal with the sickest patients 10
In the case presented, it should be noted that telemedicine was useful both in case of the Hematology Service and the Orthopedic and Rehabilitation Departments.
In conclusion, we have presented the case of a 56‐year‐old patient diagnosed with severe haemophilia A that underwent a revision total knee arthroplasty and provided with postoperative follow‐up via TM. The patient was managed by a multidisciplinary team of haematologists, rehabilitation physicians and orthopaedic surgeon and is a magnificent example of the use of TM and good collaboration between a CHTC and a district hospital, at the time of the COVID‐19 pandemic. The first case of COVID‐19 was detected in Spain on 20 February 2020. From that moment on, the number of diagnosed cases increased rapidly, with Spain, and Madrid in particular, being one of the most affected areas in Europe. Our CHTC is a national benchmark for the management of these patients. From the very beginning of the health crisis, our hospital housed a large number of COVID‐19 patients, forcing us to set up TM programmes to manage haemophilia patients safely.
The main disadvantage of TM in this case was the inability to conduct a direct physical examination. But we have learned that in this kind of cases in which surgery cannot be delayed, follow‐up can be performed by TM. If the situation of the pandemic continues, the intervention would be performed in regional hospitals guided by our orthopaedic surgeons through TM.
KEYWORDS
COVID‐19, haemophilia A, orthopaedic, surgery, telemedice
DISCLOSURES
Drs. Álvarez‐Román and Jiménez‐Yuste have participated as speakers, in advisory boards and sponsored symposia with Novo Nordisk, Takeda, Roche, Pfizer, Octapharma, Amgen, Novartis, CSL Behring and Sobi. Drs. De la Corte and Rodriguez‐Merchán have participated as speakers in sponsored symposia with Pfizer and Takeda. García‐Barcenilla has participated as speaker and sponsored symposia by Novo Nordisk, Takeda, Roche, Pfizer, Novartis and Sobi and in advisory boards with Novo Nordisk, Takeda, Roche, Pfizer, CSL Behring and Sobi. The rest of the authors have not conflicts of interest to declare.
AUTHOR CONTRIBUTIONS
MTAR and VJY designed the work. MTAR wrote the letter. HdlC, ECRM, MMS and MIRP were responsible of patient's surgery, treatment and follow‐up. NVB, SGB, PA, TC, EG and EMM were responsible of data management. All authors analysed, revised critically and gave final approval of the manuscript.
REFERENCES
- 1. Organization WH . Telemedicine: opportunities and developments in member states: report on the second global survey on eHealth. In: Organization WH , ed. Global Observatory for eHealth Series. Vol 2. WHO; 2010: 93. [Google Scholar]
- 2. Lurie N, Carr BG. The role of telehealth in the medical response to disasters. JAMA Intern Med. 2018;178(6):745‐746. [DOI] [PubMed] [Google Scholar]
- 3. Moazzami B, Razavi‐Khorasani N, Dooghaie Moghadam A, Farokhi E, Rezaei N. COVID‐19 and telemedicine: Immediate action required for maintaining healthcare providers well‐being. J Clin Virol. 2020;126:104345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid‐19. N Engl J Med. 2020;382(18):1679–1681. [DOI] [PubMed] [Google Scholar]
- 5. https://www.wfh.org. Accessed April 26, 2020.
- 6. Boccalandro EA, Dallari G, Mannucci PM. Telemedicine and telerehabilitation: current and forthcoming applications in haemophilia. Blood Transfus. 2019;17(5):385‐390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Grona SL, Bath B, Busch A, Rotter T, Trask C, Harrison E. Use of videoconferencing for physical therapy in people with musculoskeletal conditions: a systematic review. J Telemed Telecare. 2018;24(5):341‐355. [DOI] [PubMed] [Google Scholar]
- 8. Jacobson K, Hooke MC. Telehealth videoconferencing for children with hemophilia and their families: a clinical project. J Pediatr Oncol Nurs. 2016;33(4):282‐288. [DOI] [PubMed] [Google Scholar]
- 9. Kulkarni R. Use of telehealth in the delivery of comprehensive care for patients with haemophilia and other inherited bleeding disorders. Haemophilia. 2018;24(1):33‐42. [DOI] [PubMed] [Google Scholar]
- 10. Valentino LA, Skinner MW, Pipe S. The role of telemedicine in the delivery of healthcare in the COVID‐19 Pandemic. Haemophilia. 2020. 10.1111/hae.14044 [DOI] [PMC free article] [PubMed] [Google Scholar]
Acknowledgement
This work was supported by FIS‐Fondos FEDER PI19/00631 (VJY) and PI19/00772 (NVB).


