Editor,
The novel coronavirus disease (COVID‐19) outbreak has been recently declared a pandemic by the World Health Organization (WHO), being Italy and Spain the worst‐hit European countries. Although the main clinical picture consists of fever and respiratory symptoms, an increasing number of studies have reported associated skin manifestations. Herein, we present two patients with urticarial vasculitis arising in the context of COVID‐19 infection.
The first case is an elderly woman who was admitted to the hospital with bilateral pneumonia testing positive for COVID‐19. She had been receiving treatment with hydroxychloroquine, lopinavir/ritonavir and azithromycin for 5 days. The Dermatology Department was consulted for the appearance of painful erythematous patches on her trunk and hips, which left residual purpura when fading (Fig. 1a). A cutaneous biopsy was performed, revealing histologic changes characteristic of small‐vessel vasculitis (Fig. 1b). A sudden worsening of her respiratory condition led to the patient’s death, and therefore, no treatment could be prescribed.
Figure 1.
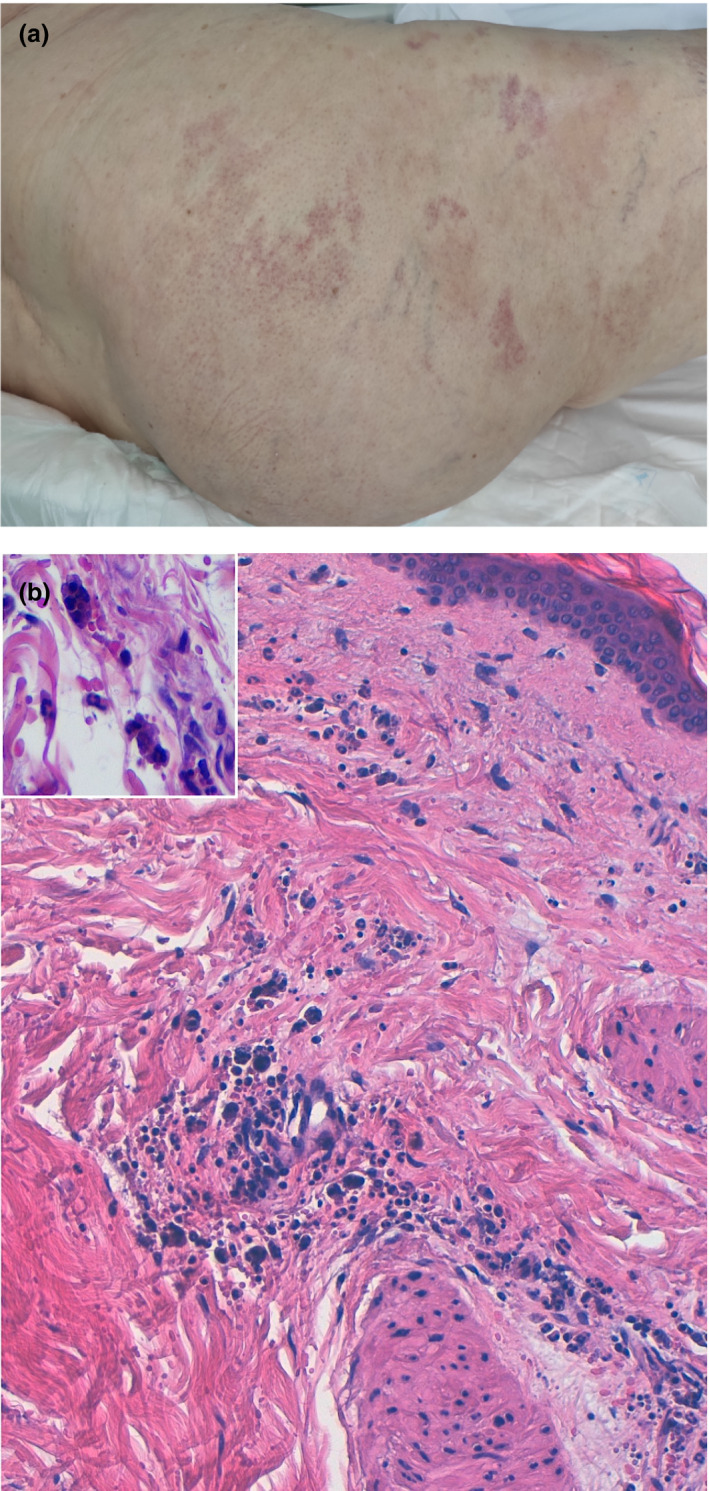
First patient. (a) Clinical lesions on the buttocks and hips. Some erythematous patches are observed, along with other purpuric ones. (b) Histopathological images (H/E × 20) revealing blood extravasation and neutrophilic perivascular inflammation with prominent karyorrhexis. There are some macrophages with a cytoplasm full of nuclear debris (inset: H/E × 40).
Our second case is a middle‐aged man who presented to the Emergency Department with a 2‐week history of fever, cough and anosmia. Two days before consulting, he had developed a pruritic rash on his buttocks. On examination, the patient had erythematous and oedematous plaques with a purpuric centre (Fig. 2a). A skin biopsy was performed, showing evidence of small‐vessel damage (Fig. 2b). Therapy with hydroxychloroquine and azithromycin was started as treatment for COVID‐19. Additionally, prednisone and antihistamines were administered for his skin condition. Two weeks later, the patient was asymptomatic.
Figure 2.
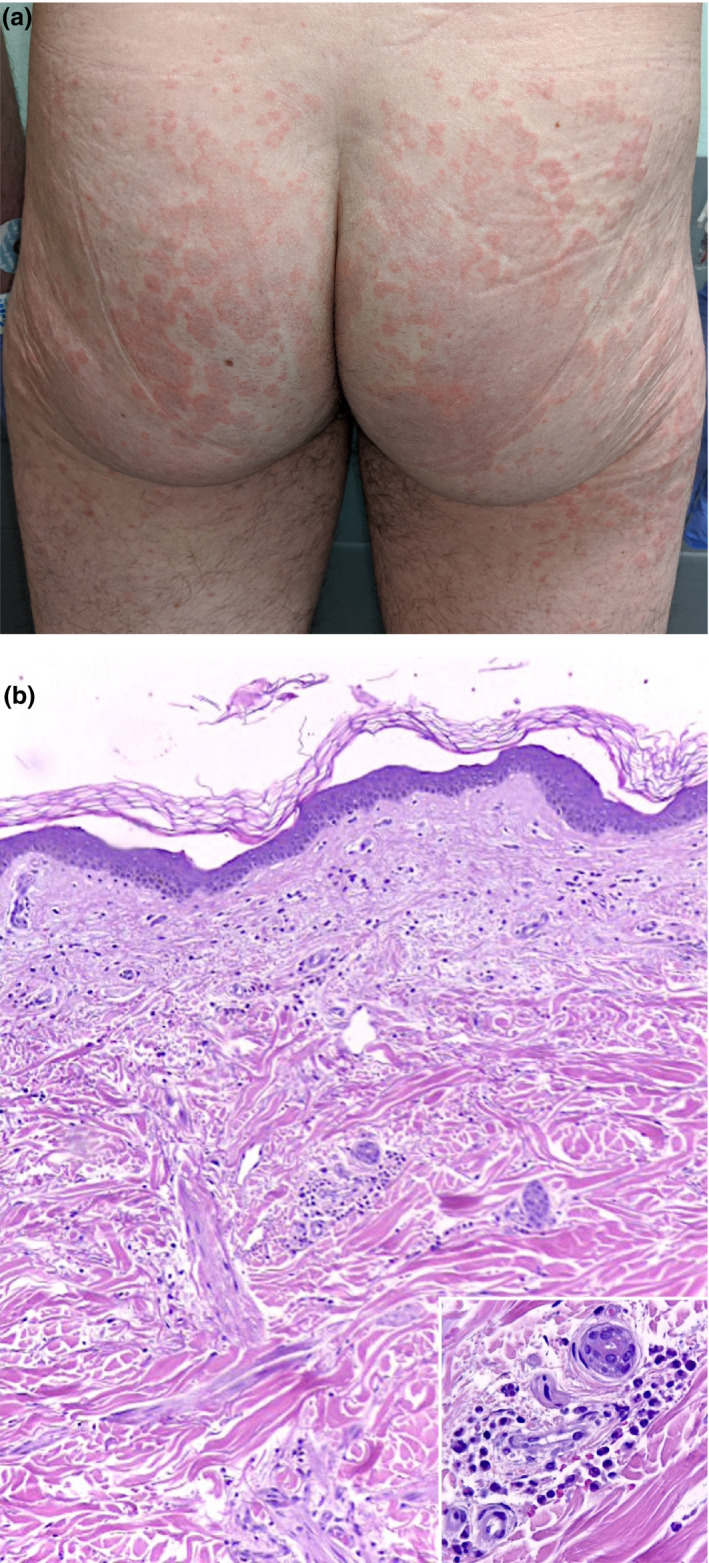
Second patient. (a) Clinical lesions on the buttocks, consisting of erythematous plaques with an active border and a purpuric centre. (b) Histopathological images (H/E × 10) showing preserved epidermis with moderate perivascular neutrophilic inflammation and blood extravasation in the dermis. There is endothelial swelling, necrosis and fibrin deposition (inset: H/E × 40).
Urticarial vasculitis is one of the multiple clinical expressions of leucocytoclastic vasculitis. Drugs, viruses and autoimmune diseases, such as systemic lupus erythematosus, can be found among its most frequent causes. A type III hypersensitivity mechanism with deposit of immunocomplexes is thought to be behind this condition. Clinically, it is characterized by the appearance of urticarial lesions similar to weals, but with individual lesions lasting more than 24 h. Although usually asymptomatic, the lesions can be accompanied by a burning sensation, pain or sometimes even by fever. Laboratory findings can include hypocomplementaemia, especially in cases linked to connective tissue diseases.
COVID‐19 has been associated with a variety of skin manifestations, including varicella‐like exanthemas, dengue‐like petechial rashes 1 , 2 or urticarial eruptions. 3 However, not only have viral rashes been related to COVID‐19, but also other types of skin symptoms that are reminiscent of a vascular disease, such as acro‐ischaemic lesions described by Zhang et al. 4 and chilblain‐like lesions. 5 , 6
Emerging theories claim that this novel coronavirus can produce endothelial activation and possibly microocclusive disease, which could be the cause of acute respiratory distress syndrome. 7 , 8 These aetiopathogenic theories may even explain the neurological manifestations that have been observed in patients with severe disease. 9 Although acro‐ischaemic lesions have been initially attributed to a hypercoagulable state, endothelial activation could play a key role in their development. In both cases, a tendency towards small‐vessel affection by COVID‐19 cannot be denied. Postmortem examinations have not only revealed the presence of hyaline thrombi in small lung vessels, in the presence of virus detectable by PCR, but also in other organs without evidence of coronavirus infection. 10 This suggests the possibility of vascular involvement in remote tissues, producing diverse manifestations. For example, in immunologically predisposed individuals, urticarial vasculitis may appear, as seen in these two patients. Although urticaria‐like rashes have been associated with COVID‐19, urticarial vasculitis has not been described in this population to date. This could be due explained by the lack of skin biopsies performed in patients with COVID‐19, either because lesions are usually mild or because of fear of contagion. We are certain more cases like these could be observed and therefore encourage dermatologists to remain alert to any possible new lesions in these patients. Much is still unknown about this new virus and its effects on the organism, and only our observation and research will allow us to increase this knowledge.
Conflicts of interest
The authors declare that there are no conflicts of interest related to this article. Dr. de Perosanz‐Lobo, Dr Fernandez‐Nieto, Dr. Burgos‐Blasco, Dr. Selda‐Enriquez, Dr. Carretero, Dr. Moreno and Dr. Fernández‐Guarino have nothing to disclose.
Acknowledgement
The patients in this manuscript have given written informed consent to the publication of their case details.
References
- 1. Joob B, Wiwanitkit V. COVID‐19 can present with a rash and be mistaken for dengue. J Am Acad Dermatol 2020; 82: e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Jimenez‐Cauhe J, Ortega‐Quijano D, Prieto‐Barrios M, Moreno‐Arrones OM, Fernandez‐Nieto D. Reply to “COVID‐19 can present with a rash and be mistaken for dengue”: Petechial rash in a patient with COVID‐19 infection. Journal of the American Academy of Dermatology. 2020. 10.1016/j.jaad.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Henry D, Ackerman M, Sancelme E, Finon A, Esteve E. Urticarial eruption in COVID‐19 infection. Journal of the European Academy of Dermatology and Venereology 2020. 10.1111/jdv.16472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhang Y, Cao W, Xiao M et al. Clinical and coagulation characteristics of 7 patients with critical COVID‐2019 pneumonia and acro‐ischemia. Zhonghua Xue Ye Xue Za Zhi Zhonghua Xueyexue Zazhi 2020; 41: E006. [DOI] [PubMed] [Google Scholar]
- 5. Landa N, Mendieta‐Eckert M, Fonda‐Pascual P, Aguirre T. Chilblain‐like lesions on feet and hands during the COVID‐19 Pandemic. Int J Dermatol 2020; 59: 739–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Piccolo V, Neri I, Filippeschi C, et al. Chilblain‐like lesions during COVID‐19 epidemic: a preliminary study on 63 patients. Journal of the European Academy of Dermatology and Venereology 2020. 10.1111/jdv.16526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Escher R, Breakey N, Lämmle B. Severe COVID‐19 infection associated with endothelial activation. Thromb Res 2020; 190: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ciceri F, Beretta L, Scandroglio AM, et al. Microvascular COVID‐19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis. Crit Care Resusc J Australas Acad Crit Care Med 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Asadi‐Pooya AA, Simani L. Central nervous system manifestations of COVID‐19: A systematic review. J Neurol Sci 2020; 413: 116832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yao XH, Li TY, He ZC et al. A pathological report of three COVID‐19 cases by minimally invasive autopsies. Zhonghua Bing Li Xue Za Zhi 2020; 49: E009. [DOI] [PubMed] [Google Scholar]


