Abstract
COVID‐19 pandemia began in Wuhan, China, in December 2019. A total of 1 878 489 people were infected and 119 044 people were lost because of the disease and its complications by 15 April. Severe morbidity and mortality complications are mostly seen in elderly and patients having comorbidities. Diabetic foot ulcers (DFUs) are one of severe complications of diabetes mellitus and it may require urgent surgical interventions. In this paper, we aimed to create a management algorithm to prevent the unexpected complications that may occur in the patients and health care workers during the evaluation of COVID‐19 in DFU patients who require urgent surgical intervention. We advise the use of thorax computerised tomography for preoperative screening in all DFU patients with severe signs of infection and especially those requiring urgent surgery for both the detection of the possible undiagnosed COVID‐19 in the patient for the need for close follow‐up and protection of the surgical and anaesthesiology team.
Keywords: COVID‐19, diabetic foot, management, ulcer, urgent
1. INTRODUCTION
In December 2019, a novel corona virus strain is identified which is transmitted via droplets and enters human through airway epithelium, which then may cause severe pneumonia and acute respiratory distress and respiratory failure. 1 The outbreak began in Wuhan, China, and the disease is called COVID‐19. On 12 March 2020, it was classified as a pandemic by World Health Organization. A total of 1 878 489 people were infected and 119 044 people were lost because of the disease and its complications by 15 April, since the outbreak of the virus. The course of the disease is very similar to seasonal flu in most of the cases, especially in young and healthy ones, but it has severe morbidity, and some mortality complication is seen in mainly elderly and disadvantaged patients; substantial amounts of them were diabetic and they have also diabetic foot wounds.
Diabetes mellitus (DM) is one of the most common chronic disorders worldwide and affects multiple systems in the body. It may increase the risk to infections through elevated blood glucose levels, microangiopathic complications, and resulting impairment of the immune system. 2 In previous coronavirus outbreaks (such as MERS‐CoV), patients with DM have been shown to have a worse prognosis compared with the population without comorbidities. 3
Diabetic foot ulcer (DFU) is a common complication of DM because of peripheral neuropathy and peripheral angiopathy caused by the disease. DFU is the cause of approximately 20% of DM patients' admissions to the hospital and patients with DM have a 20% risk of developing a foot ulcer in their lifetime. 4 Considering the incidence of DFUs which was reported as 6.1 patients having their first ulceration per 1000 annually in 2018, 5 it is safe to conclude that large number of patients with or without COVID‐19 will require medical services during the pandemic.
In this article, we aimed to create a management algorithm to prevent the unexpected complications that may occur in the patients and health care workers during the evaluation of COVID‐19 in DFU patients who require urgent surgical intervention.
1.1. Evaluation or physical examination
Use of surgical mask at all times (both patient and health care providers).
Keep 6 ft distancing (except physical examination).
Carefully question about for fever, cough, and respiratory distress or whether infected with COVID‐19.
Evaluation of the patient's vital signs (fever, pulse, blood pressure, and breath count).
Evaluation of the wound and degree of infection. 6
1.2. Treatment recommendation: An algorithmic approach
If there is no infection or mild infection in the wound, and there is no fever, local wound care is suffıcient at home and weekly online consultation can be planned by using WhatsApp (WhatsApp Inc., California).
If there is no infection or mild infection in the wound, and a fever is present, local wound care and COVID‐19 investigation should be recommended with nasopharyngeal swab.
If there is moderate infection in the wound, and there is no fever, debridement at outpatient clinic and local wound care are sufficient at home and weekly online consultation can be planned by using WhatsApp (WhatsApp Inc., California).
If there is moderate infection in the wound, and a fever is present, debridement at outpatient clinic and then local wound care are advised and COVID‐19 investigation should be recommended with nasopharyngeal swab.
-
If there are severe infection signs, hospitalisation is needed.
-
If urgent surgical intervention is required:
Thorax computerised tomography (CT) and surgical work‐up prior to surgery.
-
If urgent surgical intervention is not required:
Treatment for DFU infection (such as intravenous antibiotics, fluid replacement, correction of electrolytes imbalance, glucose control, etc.) with investigation of COVID‐19.
-
Single‐stage radical surgery with preferably local or regional block anaesthesia.
Short hospital stay and strict glucose regulation.
Online consultation to decrease the number of hospital visits (Figure 1).
FIGURE 1.
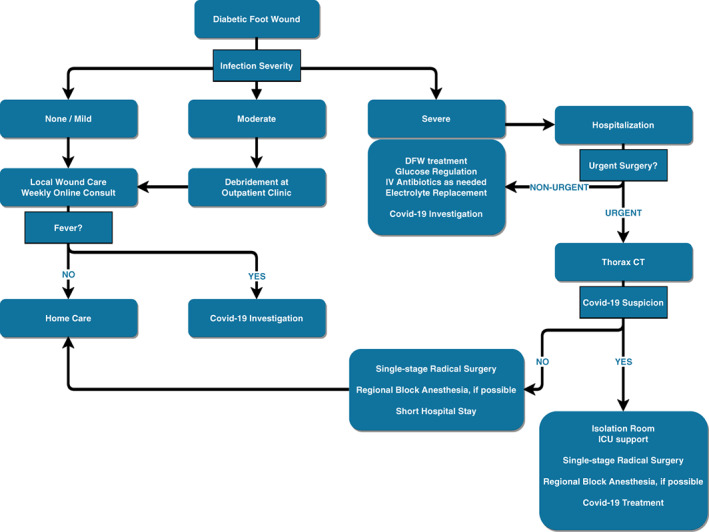
Algorithmic approach for diabetic foot ulcers
2. DISCUSSION
Although DM is an endocrine system disease, it could have systemic effects on different body systems. It has been shown in previous studies that DM increases patient's susceptibility to infection. During COVID‐19 outbreak, it has been shown to be a risk factor for patient mortality. 7 DFU is a complication of the DM, which is the most common reason for DM patients to apply to the hospital. It causes approximately 40% of all non‐traumatic lower extremity amputations. 6 Not all diabetic foot wounds are infected and could often be followed up with local wound care. Recommendations for infection detection, wound care, and treatment are regularly updated by International Working Group on the Diabetic Foot. According to these recommendations, any DFU infection with the presence of two associated systemic manifestations such as temperature >38°C or <36°C, heart rate >90 beats/min, respiratory rate >20 breaths/min or PaCO2 <4.3 kPa (32 mm Hg), white blood cell count >12 000/mm3, or <4000/mm3, or >10% immature forms indicates severe infection (Grade 4). 6
The most common symptoms of COVID‐19 are fever, cough, and dyspnoea. Fever is present in 98% of the patients. In these patients, a decrease in white blood cells and an increase in lymphocytes are shown. The rate of sensitivity of nasopharyngeal swab Reverse Transcriptase Polymerase Chain Reaction (RT‐PCR) in COVID‐19 infection is around 40% to 60%. 8 , 9 The procedure with the highest sensitivity for RT‐PCR is via bronchoalveolar lavage sampling in patients with lung involvement. On the other hand, even if RT‐PCR is negative, the sensitivity of thorax CT is around 97%. 10 , 11 Therefore, a possible false negative result in the RT‐PCR test may not change the COVID‐19 diagnosis.
The prognosis of the disease is similar to seasonal flu in healthy children and adults. But it has severe morbidity, and some mortality complication is seen in mainly elderly having comorbidity such as DM. If there is any suspicion for COVID‐19, routine investigation should be carried out and the patients should be hospitalised if there are any positive signs in investigative studies.
For patients with DFU who have severe infection and systemic findings, especially those requiring urgent surgical intervention, thorax CT screening should be a helpful rule‐out study for COVID‐19 because it has high sensitivity. Besides, it may help delay non‐emergent surgery in those with signs of mild local infection and positive thorax CT. In patients with signs of moderate local infection, detection of COVID‐19 allows monitoring of the patient with a multidisciplinary and cautious approach. Thus, anaesthesiologist's and surgical team's prepared intervention to the patient also minimises the transmission risk of possible COVID‐19 infection to health care workers. Regional block anaesthesia techniques were preferred, radical surgeries should be carried out, and intensive care unit should be prepared.
In DFU patients with severe infection findings and negative thorax CT results, a decision to implement regional block techniques and to perform radical single‐stage surgery instead of staged surgeries can decrease the patient's length of hospital stay, thus decreasing risk of nosocomial infection spreading in DM patients and facilitate usage of currently limited number of patient rooms for other clinics and patients.
3. CONCLUSION
We strongly recommend the use of thorax CT for preoperative screening in all DFU patients with severe signs of infection and especially those requiring urgent surgery for both the detection of the possible undiagnosed COVID‐19 in the patient for the need for close follow‐up and protection of the surgical and anaesthesiology team.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
Kelahmetoglu O, Camlı MF, Kirazoglu A, et al. Recommendations for management of diabetic foot ulcers during COVID‐19 outbreak. Int Wound J. 2020;17:1424–1427. 10.1111/iwj.13416
REFERENCES
- 1. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. The Lancet. 2020;395(10223):507‐513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hodgson K, Morris J, Bridson T, Govan B, Rush C, Ketheesan N. Immunological mechanisms contributing to the double burden of diabetes and intracellular bacterial infections. Immunology. 2015;144(2):171‐185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Badawi A, Ryoo SG. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS‐CoV): a systematic review and meta‐analysis. Int J Infect Dis. 2016;49:129‐133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005;293(2):217‐228. [DOI] [PubMed] [Google Scholar]
- 5. Paisey RB, Abbott A, Paisey CF, Walker D. Diabetic foot ulcer incidence and survival with improved diabetic foot services: an 18‐year study. Diabet Med. 2019;36(11):1424‐1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lipsky BA, Senneville É, Abbas ZG, et al. Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36:e3280. [DOI] [PubMed] [Google Scholar]
- 7. Guo W, Li M, Dong Y, et al. Diabetes is a risk factor for the progression and prognosis of COVID‐19. Diabetes Metab Res Rev. 2020;e3319. 10.1002/dmrr.3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ma SY, Luo YM, Hu TY, et al. Clinical application effect of modified nasopharyngeal swab sampling for 2019 novel coronavirus nucleic acid detection. Zhonghua Shao Shang Za Zhi. 2020;36(0):E009. [DOI] [PubMed] [Google Scholar]
- 9. Kokkinakis I, Selby K, Favrat B, Genton B, Cornuz J. Covid‐19 diagnosis: clinical recommendations and performance of nasopharyngeal swab‐PCR. Rev Med Suisse. 2020;16(689):699‐701. [PubMed] [Google Scholar]
- 10. Long C, Xu H, Shen Q, et al. Diagnosis of the coronavirus disease (COVID‐19): rRT‐PCR or CT? Eur J Radiol. 2020;126:108961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Li D, Wang D, Dong J, et al. False‐negative results of real‐time reverse‐transcriptase polymerase chain reaction for severe acute respiratory syndrome coronavirus 2: role of deep‐learning‐based CT diagnosis and insights from two cases. Korean J Radiol. 2020;21(4):505‐508. [DOI] [PMC free article] [PubMed] [Google Scholar]


