Abstract
The world is facing an explosive COVID‐19 pandemic. Some cases rapidly develop deteriorating lung function, which causes deep hypoxaemia and requires urgent treatment. Many centres have started treating patients in the prone position, and oxygenation has improved considerably in some cases. Questions have been raised regarding the mechanisms behind this. The mini review provides some insights into the role of supine and prone body positions and summarises the latest understanding of the responsible mechanisms. The scope for discussion is outside the neonatal period and entirely based on experimental and clinical experiences related to adults. The human respiratory system is a complex interplay of many different variables. Therefore, this mini review has prioritised previous and ongoing research to find explanations based on three scientific areas: gravity, lung structure and fractal geometry and vascular regulation. It concludes that gravity is one of the variables responsible for ventilation/perfusion matching but in concert with lung structure and fractal geometry, ventilation and regulation of lung vascular tone. Since ventilation distribution does not change between supine and prone positions, the higher expression of nitric oxide in dorsal lung vessels than in ventral vessels is likely to be the most important mechanism behind enhanced oxygenation in the prone position.
Keywords: COVID‐19, fractal geometry, gravity, lung structure, vascular regulation
Abbreviations
- mRNA
messenger ribonucleic acid
- NO
nitric oxide
- NOS
nitric oxide synthase
- SIDS
sudden infant death syndrome
- V/Q
ventilation/perfusion
Key Notes.
Treating COVID‐19 patients in prone positions can increase oxygenation, and key research areas are examined to summarise the latest understanding of the responsible mechanisms.
Gravity is only one variable responsible for ventilation/perfusion matching and is executed in concert with lung structure and fractal geometry, gas distribution and regulation of lung vascular tone.
The most important mechanism is the higher expression of nitric oxide in dorsal lung vessels than in ventral vessels.
1. INTRODUCTION
It may seem a contradiction to write a review about using the prone position for a paediatric journal like Acta Paediatrica. During the 1980s and early 1990s, sudden infant death syndrome (SIDS) was the most frequent cause of death in infants younger than 6 months. In the 1990s, researchers discovered that SIDS was associated with nursing infants prone. Authorities in New Zealand, and later in the United Kingdom, recommended that infants of 6 months and younger must be nursed supine, which has been the routine since then. This simple advice had a dramatic effect and death rates for SIDS in Sweden were reduced by up to 70%. The mechanisms behind this improvement are not entirely known. With their face and head occasionally buried in a pillow and under a blanket, the heat exchange and heat loss necessary to avoid hyperthermia were not efficient enough, particularly since infants younger than 6 months still have active brown adipose tissue. Hyperthermia reduces breathing and infants of this age are vagolytic which may cause bradycardia and, or, asystole.
Hence, the prone position in infants younger than 6 months is not recommended. However, it may be discussed with regard to toddlers, pre‐school and school children who suffer from acute lung insufficiency with deep hypoxaemia to such an extent that it threatens their life. But these age groups are not so well studied. The subject is highly interesting, and it will be a challenge in the future to design investigations that are able to evaluate prone and supine positions in a developing respiratory system.
This paper reviews the use of supine and prone positions in adult patients with severe respiratory insufficiency. It aims to reach a conclusion about the mechanisms that explain the sometimes dramatic improvements in oxygenation when these patients are turned prone. But it has been difficult to demonstrate that the prone position used for these sick patients also improves mortality rates. Such studies are difficult to perform and interpret, as the nature of the disease and the extremely complex intensive care they receive are hard to control. This makes it hard to evaluate comparable patient groups and collect reliable outcome data. This point was well made in a 2019 paper by Gattinoni et al which also highlighted the impact of protective ventilator settings to avoid ventilator‐induced lung injuries. 1 Guérin et al examined a well‐controlled and carefully selected patient population that received intensive care and assessed the mortality rates related to supine and prone positions. The authors concluded that mortality was lower in the group treated prone. 2
The world is currently experiencing an explosive pandemic caused by a new coronavirus, with a clinical presentation of a somewhat different kind. In some cases, patients experience rapidly deteriorating lung function causing deep hypoxaemia and a severely disturbed gas exchange. The COVID‐19 pandemic calls for urgent action in such cases and the prone position has become increasingly used as an early mode of treatment for those who develop this galloping severe hypoxaemia. Many centres have introduced treatment in the prone position early in spontaneously breathing patients even prior to endotracheal intubation and mechanical ventilation. Although the prone position does not improve oxygenation in all patients, there are reports of enhanced oxygenation in many COVID‐19 patients treated prone. Questions regarding mechanistic explanations for the positive effects have been raised. This paper provides some insights into this and, based on the knowledge so far, summarises the latest understanding of the mechanisms responsible.
The function of the human respiratory system is a complex interplay of different variables, such as the rib cage, the diaphragm, abdominal distension, pleural pressure, body fluids, heart function, pulmonary and systemic circulation, lung parenchyma, the tracheobronchial tree, alveoli and central and peripheral innervation. All of these act in concert to achieve adequate gas exchange for the maintenance of life. Each of them is a theoretical area in its own right, with regard to detailed mechanistic functions. It would not be possible for a review like this to provide a comprehensive overarching presentation of them all.
Therefore, it was necessary to prioritise key scientific areas for this mini review. That is why the finding on mechanisms and explanations will focus on three scientific areas: gravity, lung structure and fractal geometry and vascular regulation.
2. GRAVITY
For many years, pulmonary circulation was defined according to gravity and based on advanced investigations in upright humans. 3 , 4 , 5 According to these studies, pulmonary circulation was described in three zones. This was due to relationships between pulmonary artery pressure, alveolar pressure and pulmonary venous pressure from apical to basal lung regions with increasing pulmonary perfusion down the lung. In addition, a fourth zone was added for basal lung regions, where conditions allow pulmonary interstitial pressure to exceed pulmonary venous and alveolar pressures. These investigations and physiological interpretations have played an important role in developing our understanding of lung function today. This platform created new knowledge which has, step‐by‐step, resulted in advanced treatment of the insufficient lung.
2.1. Clinical and experimental investigations of prone postures
It came as a surprise in 1976 when Piehl and Brown stated that placing patients with respiratory insufficiency in the prone position resulted in better oxygenation. 6 This observation was supported by Douglas et al, in 1977, who agreed with Piehl and Brown. They reported that patients with acute lung insufficiency experienced improved oxygenation when flipped from the supine to prone position. 7 This was later followed up in 1986 by an experimental investigation in dogs by Beck and Rehder. This basic clarifying study stated that vascular conductance was higher in dorsal lung regions than in ventral. 8
During the 1980s, clinical investigations in patients with severe respiratory insufficiency were scarce, apart from a few investigations published in Respiratory Physiology in 1984 9 and in Chest in 1988. 10 However, in the 1990s and early 2000s, several clinical studies were published supporting the beneficial effects of the prone position for patients in intensive care units suffering from acute lung insufficiency and adult respiratory distress syndrome. 9 , 11 , 12 , 13 , 14 , 15
These investigations contributed to the continued discussions about whether gravity was the important factor for gas distribution and lung perfusion. They were also very valuable for stimulating studies to further explain the mechanisms responsible for improved ventilation/perfusion (V/Q) matching in patients in the prone position.
2.2. The continued search for mechanisms
Certainly, gravity is of interest for pulmonary circulation and ventilation and influences V/Q matching along the vertical axis and, more so, at the longer distances down the lung. To extrapolate the importance of gravity for pulmonary circulation, a study was performed using single photon emission tomography in volunteers subjected to hypergravity of three times normal gravity (3 G). A human centrifuge was used with the subjects in the supine position. Interestingly, a paradoxical result was reached, with a shift of dominant perfusion from dependent to independent lung regions when the normal gravitational force (0 G) was changed to 3 G. 16 This paradoxical finding invited to thoughts on lung structure and to the experimental study by Beck and Rehder 8 using microspheres in isolated perfused dog lungs. They concluded that: The distribution of regional vascular conductances were related to the anatomic location and were not related to gravity, nor were they caused by nonuniformities in regional lung expansion or by hypoxic vasoconstriction or edema. That statement is still very central for discussions regarding the explanatory mechanisms responsible for improved oxygenation in the prone position.
The observations above, of lower vascular conductance in dorsal lung regions and the paradoxical shift of lung perfusion during hypergravity, indicate that other factors than gravity are involved in achieving efficient V/Q matching. In a series of experimental investigations during the 1990s, using radioactive microspheres in isolated dog lungs, heterogeneity of lung perfusion within iso‐gravitational fields was demonstrated. 17 , 18 , 19 , 20 These investigations were valuable and very early on a report from 1991 was published using the provocative title that: Gravity is a minor determinant of pulmonary blood flow distribution. 21 Interesting discussions resulted and the brave conclusion from 1991 stood the test of time. Another paper from the same research group appeared in the same journal 8 years later entitled: Gravity is an important but secondary determinant of regional pulmonary blood flow in upright primates. 22
During the time period between these two publications, 1991 to 1999, and into the early years of the 2000s, many scientific investigations were published, as previously discussed. These stated that V/Q matching was more uniform in the prone position and that oxygenation in patients with severe acute lung insufficiency improved in the prone posture. 21 , 22 Hence, there is general agreement today that prone positioning of patients suffering from severe respiratory insufficiency is a successful and important treatment mode in modern intensive care units.
3. LUNG STRUCTURE AND FRACTAL GEOMETRY
Like all organs, the anatomy and structure of lungs are genetically determined and are important pre‐requisite conditions for function. Embryologic development of the lungs is characterised by dichotomous branching of both the airways and vessels. The branching follows a genetically determined geometric pattern, such as angles related to the common stem from which the dichotomous branching originates. Also, the development of airways and vessels are in parallel and happens synchronously. This structural arrangement will ensure laminar transport of both gas and blood to, and from, alveoli. Altered angulations of the fractal geometry often cause turbulence and increased resistance, which reduces oxygenation and gas exchange (Figure 1).
Figure 1.
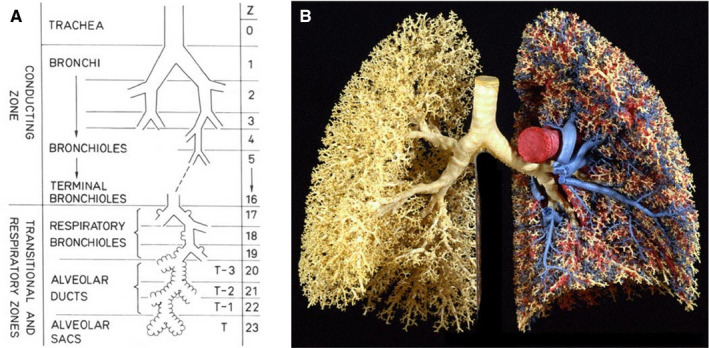
On the left, a schematic presentation of the dichotomous branching of airways. On the right, a presentation of the complex anatomy of airways, venous and arterial vasculature
Fractal geometry of the airways and vessels has, to a large extent, been clarified by findings from the Washington School of Medicine in Seattle. 23 , 24 Investigations using microspheres found that small regions in the lung alternated with regard to V/Q matching, as expressed by measured coefficients of variation. This enabled comparisons between supine and prone positions, which demonstrated improved uniformity in the prone position. 17 , 22 These investigations also illustrated that oxygenation and gas exchange can be reduced by factors such as fluid balance in the lung, pulmonary inflammation and enhanced vascular thrombotisation. All of these variables are likely to disturb the delicate fractal structure and play an important role in lung function.
So, changes in body posture from supine to prone results in more uniform V/Q matching. A study of spontaneously breathing healthy volunteers reported that a change from prone to supine caused a shift in the distribution of lung parenchyma within the rib cage. 25 Such changes are of interest from a fractal point of view. Hence, lung structure is important for lung function, and in addition, the positions of the heart and diaphragm are different in supine and prone postures with the advantage for the prone as far as lung function is concerned. Since V/Q matching is more uniform in the prone position than in the supine, it is of interest to evaluate distributions of ventilation and perfusion separately. This was a focus in a study by Nyrén et al 26 of healthy volunteers during anaesthesia and mechanical ventilation. A single photon emission computed tomography (SPECT) with a dual isotope technique was used. The volunteers were investigated twice, first turning from supine to prone and then from prone to supine. Based on the results of this investigation, it was concluded that: In anesthetized and mechanically ventilated healthy volunteers, regional lung ventilation did not differ with position whereas perfusion was more uniform in the prone position.
There are two important variables for assessing V/Q matching with regard to changes from supine to prone positions and vice versa. The one that was found to change was perfusion, whereas ventilation stayed the same. This finding enhanced the interest for regulation of lung perfusion.
4. VASCULAR REGULATION
Several questions have been, and still are, asked about the most likely responsible mechanism for improved oxygenation in prone position after the surprising finding, by Piehl and Brown in 1976 6 and the follow‐up study by Douglas et al in 1977. 7 Questions that have enhanced the interest and stimulated not only clinical investigations, but also basic sciences, in order to further elucidate the responsible mechanisms. The finding that vascular conductance in dogs was greater in dorsal than in ventral lung vasculature clearly indicated that there ought to be vasoactive mechanisms in the lungs that were counteracting gravity. 8
Another important observation was in 1996, when Hlastala et al, found that lung perfusion in standing horses was not dominantly governed by gravity. 27 This was a most valuable result on the road to finding a mechanistic explanation for the improved lung perfusion in the prone position. Another important contribution was when Pelletier et al published their findings in horses based on investigations of pulmonary arterial rings in organ bath studies. 28 They concluded that endothelium‐derived relaxation was greater in dorsal, than in ventral, lung vasculature using several substances signalling via the cyclic guanosine monophosphate/nitric oxide (NO) pathway. This was a valuable step as it narrowed down several possibilities that might constitute the most responsible mechanism for improved V/Q matching in the prone position.
A next step was to explore whether NO production in human lung vasculature could be responsible for improved V/Q matching in the prone position. An investigation was designed to challenge the hypothesis that NO plays an important role in the regulation of regional lung perfusion. Nitric oxide synthase (NOS) messenger ribonucleic acid (mRNA) and NOS activity using citrulline assay were analysed in ventral and dorsal lung tissue samples from patients subjected to lung surgery. 29 In addition, the study also assessed regional lung perfusion in volunteers by single photon emission computed tomography before and after NOS inhibition. The hypothesis was supported, and it was found that mRNA expression of endothelial NOS was higher in dorsal than in ventral lung regions. Moreover, it was found that calcium‐dependent NOS activity in citrulline units was higher in dorsal than ventral lung whereas calcium‐independent NOS activity was similar in ventral and dorsal regions (Figure 2A,B).
Figure 2.
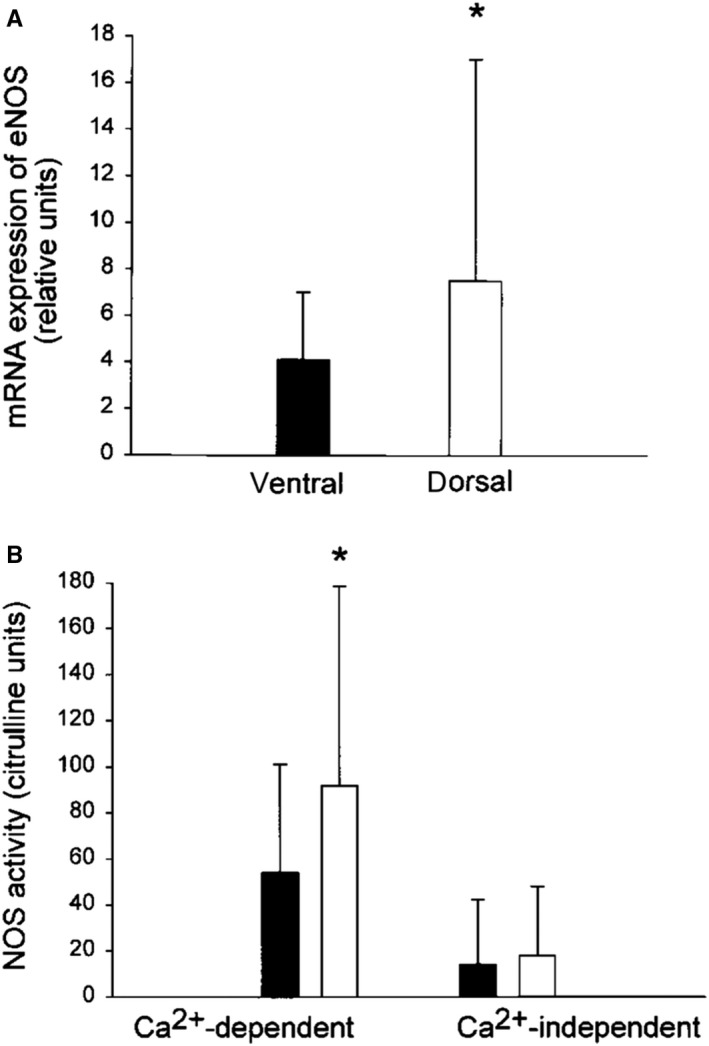
A and B (from Rimeika et al). 29 A, Expression of mRNA for endothelial NOS in ventral and dorsal lung tissue. B, NOS activity determined by citrulline assay in ventral and dorsal human lung tissue
Single photon emission computed tomography studies in volunteers confirmed these results and demonstrated that in supine individuals NOS inhibition, using the NOS inhibitor L‐NMMA, caused a ventral shift of lung perfusion as illustrated by the results from one of the volunteers, 29 (Figure 3).
Figure 3.
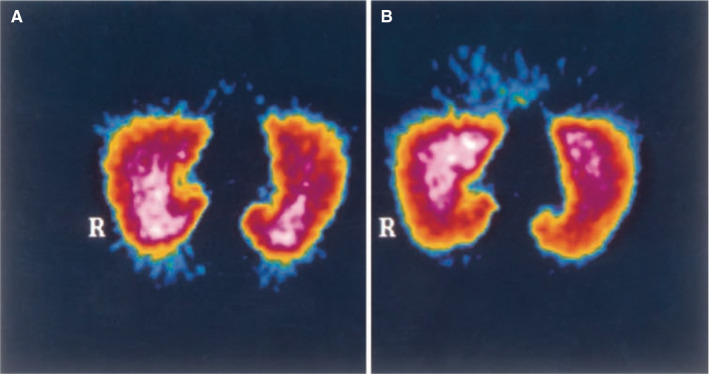
(from Rimeika et al). 29 Single photon emission computed tomography image of pulmonary perfusion in one supine volunteer before (A) and after (B) NOS inhibition using L‐NMMA intravenously. R indicates the right lung
5. CONCLUSION
Based on this review, it is concluded that gravity is one of the variables responsible for V/Q matching, but in concert with lung structure and fractal geometry, gas distribution and regulation of lung vascular tone. This conclusion is based on a long series of investigations published in leading journals and illustrates the essence of science, where brick is laid on brick in a process of continued development.
In view of the unchanged ventilation distribution of prone and supine, it currently seems that the most important mechanism is different regulation of lung vascularity in dorsal and ventral lung regions, due to expression of the potent vasodilator NO. This mechanism is also present in horses and in pigs making it likely that the enhanced NO production in dorsal lung regions is an evolutionary trait preserved from the time when we walked on four legs.
It is very likely that there is more to know, and understand, about the complex lung function which will be further elucidated in future investigations.
Based on the above findings, it appears that using the prone position to combat the fast development of deep hypoxia in some patients with COVID‐19 is a useful tool. This could even be used in spontaneously breathing patients with deep hypoxaemia prior to initiation of mechanical ventilation and extra corporeal oxygenation.
CONFLICTS OF INTEREST
The author has no conflicts of interest to declare.
Lindahl SGE. Using the prone position could help to combat the development of fast hypoxia in some patients with COVID‐19. Acta Paediatr. 2020;109:1539–1544. 10.1111/apa.15382
REFERENCES
- 1. Gattinoni L, Busana M, Giosa L, et al. Prone positioning in acute respiratory distress syndrome. Semin Respir Crit Care Med. 2019;40:94‐100. [DOI] [PubMed] [Google Scholar]
- 2. Guérin C, Reignier J, Richard J‐C, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23):2159‐2168. [DOI] [PubMed] [Google Scholar]
- 3. West J, Dollery C, Naimark A. Distribution of blood flow in isolated lung; relation to vascular and alveolar pressures. J Appl Physiol. 1964;19(4):713‐724. [DOI] [PubMed] [Google Scholar]
- 4. Hughes J, Glazier J, Maloney J, West J. Effect of lung volume on the distribution of pulmonary blood flow in man. Respir Physiol. 1968;4(1):58‐72. [DOI] [PubMed] [Google Scholar]
- 5. Hughes J, Glazier J, Maloney J, West J. Effect of extra‐alveolar vessels on distribution of blood flow in the dog lung. J Appl Physiol. 1968;25(6):701‐712. [DOI] [PubMed] [Google Scholar]
- 6. Piehl MA, Brown RS. Use of extreme position changes in acute respiratory failure. Crit Care Med. 1976;4(1):13‐14. [DOI] [PubMed] [Google Scholar]
- 7. Douglas WW, Rehder K, Beynen FM, Sessler AD, Marsh HM. Improved oxygenation in patients with acute respiratory failure: the prone position. Am Rev Respir Dis. 1977;115(4):559‐566. [DOI] [PubMed] [Google Scholar]
- 8. Beck K, Rehder K. Differences in regional vascular conductances in isolated dog lungs. J Appl Physiol. 1986;61(2):530‐538. [DOI] [PubMed] [Google Scholar]
- 9. Amis T, Jones HA, Hughes J. Effect of posture on inter‐regional distribution of pulmonary ventilation in man. Respir Physiol. 1984;56(2):145‐167. [DOI] [PubMed] [Google Scholar]
- 10. Langer M, Mascheroni D, Marcolin R, Gattinoni L. The prone position in ARDS patients: a clinical study. Chest. 1988;94(1):103‐107. [DOI] [PubMed] [Google Scholar]
- 11. Pelosi P, Croci M, Calappi E, et al. The prone positioning during general anesthesia minimally affects respiratory mechanics while improving functional residual capacity and increasing oxygen tension. Anesth Analg. 1995;80(5):955‐960. [DOI] [PubMed] [Google Scholar]
- 12. Pelosi P, Croci M, Calappi E, et al. Prone positioning improves pulmonary function in obese patients during general anesthesia. Anesth Analg. 1996;83(3):578‐583. [DOI] [PubMed] [Google Scholar]
- 13. Mure M, Martling C‐R, Lindahl SG. Dramatic effect on oxygenation in patients with severe acute lung insufficiency treated in the prone position. Crit Care Med. 1997;25(9):1539‐1544. [DOI] [PubMed] [Google Scholar]
- 14. Mure M, Glenny RW, Domino KB, Hlastala MP. Pulmonary gas exchange improves in the prone position with abdominal distension. Am J Respir Crit Care Med. 1998;157(6):1785‐1790. [DOI] [PubMed] [Google Scholar]
- 15. Nyrén S, Mure M, Jacobsson H, Larsson SA, Lindahl SG. Pulmonary perfusion is more uniform in the prone than in the supine position: scintigraphy in healthy humans. J Appl Physiol. 1999;86(4):1135‐1141. [DOI] [PubMed] [Google Scholar]
- 16. Petersson J, Rohdin M, Sánchez‐Crespo A, et al. Paradoxical redistribution of pulmonary blood flow in prone and supine humans exposed to hypergravity. J Appl Physiol. 2006;100(1):240‐248. [DOI] [PubMed] [Google Scholar]
- 17. Glenny RW, Robertson HT. Fractal properties of pulmonary blood flow: characterization of spatial heterogeneity. J Appl Physiol. 1990;69(2):532‐545. [DOI] [PubMed] [Google Scholar]
- 18. Robertson HT, Glenny RW, Stanford D, McInnes LM, Luchtel DL, Covert D. High‐resolution maps of regional ventilation utilizing inhaled fluorescent microspheres. J Appl Physiol. 1997;82(3):943‐953. [DOI] [PubMed] [Google Scholar]
- 19. Walther SM, Domino KB, Glenny RW, Polissar NL, Hlastala MP. Pulmonary blood flow distribution has a hilar‐to‐peripheral gradient in awake, prone sheep. J Appl Physiol. 1997;82(2):678‐685. [DOI] [PubMed] [Google Scholar]
- 20. Altemeier WA, Robertson HT, Glenny RW. Pulmonary gas‐exchange analysis by using simultaneous deposition of aerosolized and injected microspheres. J Appl Physiol. 1998;85(6):2344‐2351. [DOI] [PubMed] [Google Scholar]
- 21. Glenny R, Lamm WJ, Albert RK, Robertson HT. Gravity is a minor determinant of pulmonary blood flow distribution. J Appl Physiol. 1991;71:620‐629. [DOI] [PubMed] [Google Scholar]
- 22. Glenny RW, Bernard S, Robertson HT, Hlastala MP. Gravity is an important but secondary determinant of regional pulmonary blood flow in upright primates. J Appl Physiol. 1999;86(2):623‐632. [DOI] [PubMed] [Google Scholar]
- 23. Glenny RW, Bernard SL, Robertson HT. Pulmonary blood flow remains fractal down to the level of gas exchange. J Appl Physiol. 2000;89(2):742‐748. [DOI] [PubMed] [Google Scholar]
- 24. Mure M, Domino KB, Lindahl SG, Hlastala MP, Altemeier WA, Glenny RW. Regional ventilation‐perfusion distribution is more uniform in the prone position. J Appl Physiol. 2000;88:1076‐1083. [DOI] [PubMed] [Google Scholar]
- 25. Petersson J, Rohdin M, Sánchez‐Crespo A, et al. Posture primarily affects the distribution of lung tissue with minor effect on regional blood flow and ventilation. Respir Physiol Neurobiol. 2007;156:293‐303. [DOI] [PubMed] [Google Scholar]
- 26. Nyrén S, Radell P, Lindahl SGE, et al. Lung ventilation and perfusion in prone and supine postures with reference to anesthetized and mechanically ventilated healthy volunteers. Anesthesiology. 2010;112:682‐687. [DOI] [PubMed] [Google Scholar]
- 27. Hlastala MP, Bernard SL, Erickson HH, et al. Pulmonary blood flow distribution in standing horses is not dominated by gravity. J Appl Physiol. 1996;81(3):1051‐1061. [DOI] [PubMed] [Google Scholar]
- 28. Pelletier N, Robinson NE, Kaiser L, Derksen FJ. Regional differences in endothelial function in horse lungs: possible role in blood flow distribution? J Appl Physiol. 1998;85(2):537‐542. [DOI] [PubMed] [Google Scholar]
- 29. Rimeika D, Nyrén S, Wiklund NP, et al. Regulation of regional lung perfusion by nitric oxide. Am J Respir Crit Care Med. 2004;170(4):450‐455. [DOI] [PubMed] [Google Scholar]


