To the Editor,
We reported two cases of coronavirus disease 2019 (COVID‐19) patients coinfected with human immunodeficiency virus (HIV). The severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) nucleic acid test of patients turned negative while the clinical symptoms persisted, and interstitial pneumonia gradually deteriorated. The cases provided evidences to clinicians for the diagnosis and treatment of COVID‐19 patients coinfected with HIV.
The outbreak of COVID‐19 in early December 2019 has rapidly spread to all over the world. As announced by World Health Organization (https://www.who.int), there were approximately 4 628 900 people infected with SARS‐CoV‐2, which has killed more than 312 000 people worldwide until 18 May 2020. However, clinical manifestations vary widely from patient to patient. 1
The adaptive immune response plays a key role in all viral infections, during which T cells mediated cell immunity and B lymphocytes mediated humoral immunity. As is known to all, the HIV targets the immune system and mainly destroys CD4+ T lymphocytes. Recently, COVID‐19 patients coinfected with HIV have attracted the interests of some researchers. A 61‐year‐old male patient coinfected with COVID‐19 and HIV was in stable condition and discharged after 20 days of treatment. 2 Another study concluded that SARS‐CoV‐2/HIV coinfected patients are having a more favorable prognosis when already under antiretroviral therapy. 3 In contrast, a study from New York revealed that the mortality of COVID‐19 patients with HIV infection reached up to 78%. 4 Given that, the outcome of SARS‐CoV‐2/HIV coinfected patients seems controversial, and how to uncover the underlying HIV infected in COVID‐19 patients remains to be elucidated.
In the present study, we reported two young male COVID‐19 patients coinfected with HIV and analyzed the clinical and laboratory features of them. It will provide clues for the diagnosis and treatment of COVID‐19 patients coinfected with HIV.
CASE 1
A 37‐year‐old male patient visited the hospital because of fever and positive of the nucleic acid test of SARS‐CoV‐2. The patient stated that he had got an intermittent fever since early January this year accompanied by chest pain, without productive cough, and flustered shortness of breath. The highest body temperature was 39.4°C. The patient was diagnosed with COVID‐19 with the lung computed tomography (CT) scan and detection of SARS‐CoV‐2 nucleic acid and was treated in a hospital for a few days. The symptoms of COVID‐19 were not remission after receiving symptomatic and supportive treatment; the patient called for further treatment from Huoshenshan Hospital in Wuhan on 11 February.
Physical examination of the patient revealed a body temperature of 38.8°C, respiratory rate of 40 breaths per minute, pulse of 119 beats per minute, and blood pressure of 145/93 mm Hg. After admission to the hospital, the patient was given symptomatic supportive treatment such as intermittent low flow oxygen, lianhua qingwen capsule, and antiviral therapy with Abidor. During that period, the patient received detection of SARS‐CoV‐2 nucleic acid or specific immunoglobulin M (IgM) and immunoglobulin G (IgG) antibodies for three times since 11 February, while none of the tests was positive (Supporting Information Figure S1A). The laboratory test results showed that the protein synthesis by hepatocytes like total protein (TP) or albumin (ALB) were decreased and the hepatocellular enzymes alanine aminotransferase (ALT) or aspartate aminotransferase (AST) were significantly increased, the absolute count of lymphocytes was lower than the normal reference value. However, the infection had a limited effect on heart function (Figure 1A) or renal function (Supporting Information Figure S1B). The detailed characteristics of Case 1 were shown in Supporting Information Table S1. Moreover, CT scan images of the lung showed that the high‐density area was gradually increased from 2 February to 20 February (Figure 1B). The patient had an intermittent fever and chest pain, and the highest body temperature was 39.4°C. Most importantly, the patient presented fluctuating dyspnea symptoms for a long time. The number of lymphocytes also fluctuated from normal to far below the reference value, and the lowest lymphocyte count was 0.56 × 109/L. The clinicians evaluated the symptoms and examinations comprehensively and speculated that the patients might suffer from immunodeficiency diseases. Then HIV detection results showed that the patient was HIV‐positive. At last, the patient was transferred to a special hospital for infectious diseases and received further therapy.
Figure 1.
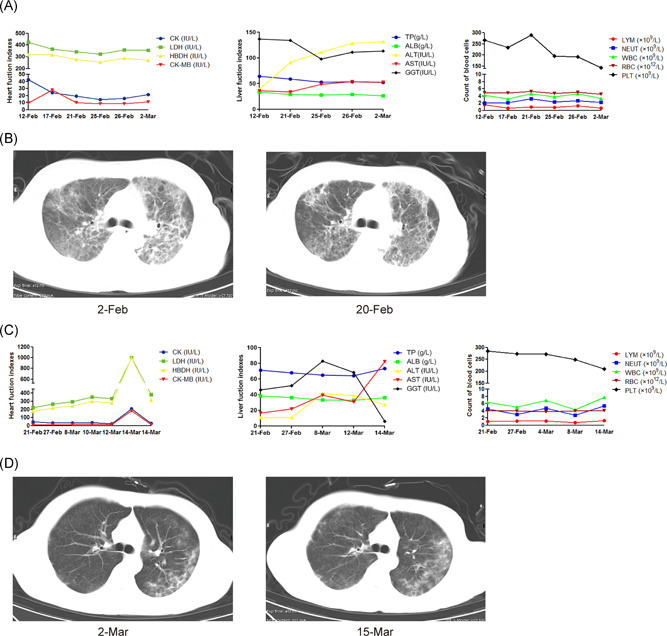
The dynamic blood test results and CT images of lungs from Case 1 and Case 2 after admission. A, The heart (left) and liver (middle) function indexes and count of peripheral blood cells (right) from Case 1. B, The CT images of lungs from Case 1 on 2nd and 20th February. C, The heart (left) and liver (middle) function indexes and count of peripheral blood cells (right) from Case 2. D, The CT images of lungs from Case 2 on 2nd and 15th March. ALB, albumin; ALT, alanine aminotransferase; AST, aspartate aminotransferase; CK, creations kinase; CK‐MB, creative kinase isoenzyme MB; CT, computed tomography; GGT, gamma‐glutamyl transferase; HBDH, hydroxybutyrate dehydrogenase; LDH, lactate dehydrogenase; LYM, lymphocyte; NEUT, neutrophil; PLT, platelet; RBC, red blood cell; TP, total protein; WBC, white blood cell
CASE 2
A 24‐year‐old male patient visited the hospital because of fever and dyspnea. The patient stated that he had got an intermittent fever accompanied by cough, fatigue, poor appetite, dizziness, chest tightness, and shortness of breath after activity since 8 February. The highest body temperature was 40°C. The patient was diagnosed with COVID‐19 based on the examination from a chest CT scan and the nucleic acid test of SARS‐CoV‐2. The symptoms of COVID‐19 were not remission after receiving symptomatic and supportive treatment; the patient was transferred to Huoshenshan Hospital in Wuhan on 20 February.
Physical examination of the patient revealed a body temperature of 36.5°C, respiratory rate of 22 breaths per minute, pulse of 102 beats per minute, and blood pressure of 125/88 mm Hg. After admission to the hospital, the patient was given symptomatic supportive treatment such as intermittent low flow oxygen, antiviral therapy with Abidor, and antibodies therapy toward to interleukin 6 (IL‐6) receptor with tocilizumab. During that period, the patient received SARS‐CoV‐2 nucleic acid detection seven times since 28 February, while none of the tests was positive (Supporting Information Figure S1C). The SARS‐CoV‐2–specific IgM and IgG were positive only on 4 March, while negative on 15 March. The laboratory test results showed that the myocardial enzymes such as lactate dehydrogenase (LDH), hydroxyhutyrate dehydrogenase (HBDH), creations kinase (CK), and creative kinase isoenzyme MB (CK‐MB) were gradually increased, the liver function index TP or ALB was decreased and ALT or AST was increased, the absolute count of lymphocytes was lower than the normal reference value (Figure 1C). The level of IL‐6 was significantly increased (Supporting Information S1D), while the effect of infection on renal function was limited (Supporting Information Figure S1E). The detailed characteristics of Case 2 were shown in Supporting Information Table S1. Moreover, the CT scan of the lung showed that the high‐density area was gradually increased from 2 March to 15 March (Figure 1D). The patient had an intermittent fever and cough, and the highest body temperature was 40.2°C. Most importantly, the symptom of dyspnea had gradually worsened. To validate whether the patient simultaneously suffered from immune deficiency diseases, HIV detection tests were performed. The results showed that the patient was coinfected with HIV. At last, the patient was transferred to a special hospital for infectious diseases and received further therapy.
We reported two cases of COVID‐19 patients coinfected with HIV. Although there is a lack of epidemiological investigation on whether HIV patients are susceptible to COVID‐19, the above cases presented the following distinctive clinical course and manifestations. First, the symptom of dyspnea persisted, and the exudative inflammation of lung was gradually increased, though the test of SARS‐CoV‐2 nucleic acid and specific IgM or IgG rapidly turned negative after receiving standard combination therapy. Second, previous studies showed that the median hospital time of COVID‐19 patients was 12.32 or 14.8 days; 5 , 6 however, these two young patients had a longer course of the disease and more severe symptoms. Third, the laboratory test showed that the liver function of Case 1 and heart function of Case 2 was obviously damaged. It has been reported that SARS‐CoV‐2 caused not only lung dysfunction, but also liver, heart, and kidney damage. 7 , 8 , 9 What's more, the lymphocyte count of these two patients was evidently lower than patients infected with SARS‐CoV‐2 only (data not shown). Generally, the clinical symptoms and treatment outcome of these two patients were significantly different from most of the patients especially young patients. This may be related to the immunosuppressive state of HIV patients. Consistent with it, other immunocompromised patients, such as cancer, 10 HIV, 4 or HBV infection, 11 might be at increased risk of COVID‐19 and have a poorer prognosis.
Based on the above cases, we proposed some strategies for clinicians when treating some special COVID‐19 patients. If the tests of SARS‐CoV‐2 nucleic acid and antibodies are inconsistent with clinical symptoms of the patient, the possibility of accompanied immunodeficiency disease should be excluded to provide further treatment in time. In addition, more intensive surveillance or treatment should be considered for HIV patients who are infected with SARS‐CoV‐2. Especially, clinicians should pay more attention to the damage of key organs in those patients. Most importantly, immunocompromised patients should strengthen personal protection to avoid SARS‐CoV‐2 infection.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
Supporting information
Supporting information
ACKNOWLEDGMENTS
We thank for the work and contribution of all the health providers from the Huoshenshan Hospital. This study was supported by Scientific Research Foundation for Introduced High‐level Personnel in Chongqing Medical University (41021300160256).
Funding Information Chongqing Medical University, Grant/Award Number: 41021300160256
Wei Li and Qiang Ma contributed equally to this study.
Contributor Information
Jie Lin, Email: linjiechn@163.com.
Bin Xiao, Email: binxiaocqmu@cqmu.edu.cn.
REFERENCES
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhu F, Cao Y, Xu S, Zhou M. Co‐infection of SARS‐CoV‐2 and HIV in a patient in Wuhan city, China. J Med Virol. 2020;92(6):529‐530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Patel RH, Pella PM. COVID‐19 in a patient with HIV infection. J Med Virol. 2020:1‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Suwanwongse K, Shabarek N. Clinical features and outcome of HIV/SARS‐CoV‐2 co‐infected patients in the Bronx, New York City. J Med Virol. 2020:1‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zheng Y, Xu H, Yang M, et al. Epidemiological characteristics and clinical features of 32 critical and 67 noncritical cases of COVID‐19 in Chengdu. J Clin Virol. 2020;127:104366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang R, Pan M, Zhang X, et al. Epidemiological and clinical features of 125 hospitalized patients with COVID‐19 in Fuyang, Anhui, China. Int J Infect Dis. 2020;95:421‐428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fan Z, Chen L, Li J, et al. Clinical features of COVID‐19‐related liver damage. Clin Gastroenterol Hepatol. 2020;18(7):1561‐1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cui Y, Tian M, Huang D, et al. A 55‐day‐old female infant infected with COVID 19: presenting with pneumonia, liver injury, and heart damage. J Infect Dis. 2020;221(11):1775‐1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fanelli V, Fiorentino M, Cantaluppi V, et al. Acute kidney injury in SARS‐CoV‐2 infected patients. Crit Care. 2020;24(1):155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Liang W, Guan W, Chen R, et al. Cancer patients in SARS‐CoV‐2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335‐337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chen X, Jiang Q, Ma Z, et al. Clinical characteristics of hospitalized patients with SARS‐CoV‐2 and Hepatitis B virus co‐infection. medRxiv, 10.1101/2020.03.23.20040733 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information


