Abstract
The world is now plagued by a pandemic of unprecedented nature caused by a novel, emerging, and still poorly understood infectious disease, coronavirus disease 2019 (COVID-19) (Wu and McGoogan, 2020). In addition to the rapidly growing body of scientific and medical literature that is being published, extensive public reports and stories in both the traditional media and social media have served to generate fear, panic, stigmatization, and instances of xenophobia (Zarocostas, 2020).
Keywords: Pandemic, COVID-19, Fear, Infodemic, Rumour
The world is now plagued by a pandemic of unprecedented nature caused by a novel, emerging, and still poorly understood infectious disease, coronavirus disease 2019 (COVID-19) (Wu and McGoogan, 2020). In addition to the rapidly growing body of scientific and medical literature that is being published, extensive public reports and stories in both the traditional media and social media have served to generate fear, panic, stigmatization, and instances of xenophobia (Zarocostas, 2020).
Past experience of pandemics has helped the authorities to prepare well-known strategies for media reporting during health emergencies (WHO, 2007). Cutting-edge approaches such as “Message Maps” provide detailed science-based risk communication materials for use in a range of anticipated and unanticipated circumstances. Message Maps guide effective communications by anticipating the manner in which health risk perceptions affect people’s understanding and responses to the information given (Covello and Hyer, 2020). This is important because perceptions are the reality that underpins people’s understanding and fear. The cognitive and adaptive risk perception factors at work with COVID-19 all heighten the perceived risk (Slovic, 2000). It is normal to fear the unknown, especially if it affects our health and that of our loved ones. If we cannot see who has it, and if we are told it might be fatal, then the fear increases.
Fear can be a positive force. We respond to fear both rationally and irrationally. A rational response is to understand and manage the threat of harm occurring—that is, the risks. An irrational but common response is to panic. Panic occurs when the risk as perceived has characteristics that are “dreaded.” Under these circumstances, even objective, scientifically-based information can increase fear in the general population. As has been seen with COVID-19, sound scientific advice is essential, but not sufficient to dispel fear and avoid panic. Authentic news reporting can increase fears because the threat is novel, unseen, and potentially fatal, especially to those most vulnerable groups in society: the aged and the sick. The very stress caused by the COVID-19 pandemic among members of the population also reduces the ability to absorb anything more than very simplistic messages, and of course certain sections of society are more susceptible to fear and panic than others—those prone to anxiety and those with underlying mental health conditions (McKay et al., 2020).
Fear and panic are worsened by emotive language and when scientists are seen to argue in public. Expressed differences about how transmission of the disease occurs and the relative value of different protective measures only serve to heighten confusion and concern. The established press and media need to understand that they have a responsibility not to inflame fears just to sell its stories or to attract more readers and viewers. However, with COVID-19, where the press and media use words such as “plague” and “apocalypse,” then the effect is to heighten concerns and promote irrational fears. At the same time, social media is unconstrained and with rapid dissemination of information it will pick up and amplify any frightening stories.
Social media now plays an increasingly significant role in communicating information and news through the population. Unfortunately, this is commonly incorrect information or “false news.” This influence is exacerbated because the algorithms used in social media and online news channels are designed to keep the user as engaged with the platform as much as possible, resulting in a constant flow of memes and text echoing key words and themes that may raise anxiety, stress, and even panic. In an analysis of the social media platform “Twitter,” Pulido et al. (2020) found that false information is tweeted more, but retweeted less, than science-based evidence or fact-checking tweets. Science-based evidence and fact-checking tweets capture more engagement than mere facts themselves (Pulido et al., 2020).
Years of research have demonstrated that in times of heightened fear and anxiety, the ability of the populace to absorb and integrate information, even from trusted sources such as local and national health authorities and the World Health Organization (WHO), is substantially reduced. In these situations, communities are likely to understand or to heed only a small percentage of the information provided (Clarke et al., 2006; WHO, 2007; Covello and Hyer, 2020).
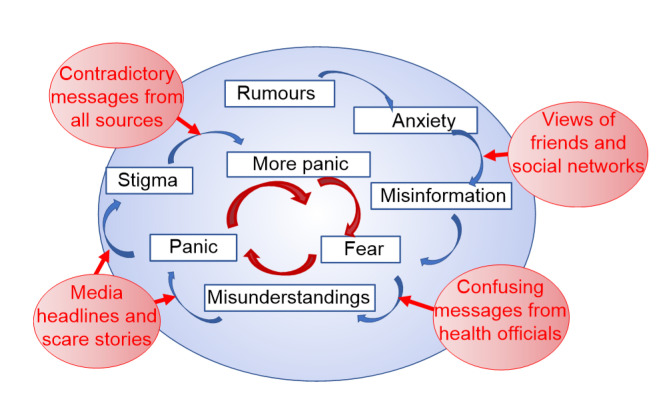
This problem is not simply an example of the social amplification of risk (Kasperson and Kasperson, 2005). Rather, it arises through a vicious circle: social networks→confusing messages from health officials→media headlines and scare stories→ contradictory messages→more panic (Fig. 1). When fear takes hold, people turn to sources of information that reinforce their personal views and pre-conceptions. They also tend to place their trust in the most familiar, but not necessarily the most credible, sources of information, turning, for instance, to social networks that agree with their prejudices. Those who express cynicism or mistrust will become influential—heightening fears and the potential to panic.
Fig. 1.
Vicious circle of fear and panic
Confusing and inconsistent official health policy advice on the one hand, and politically-motivated advice on the other, will also exacerbate both mistrust and fear. For instance, lack of clarity in health advice about social distancing and self-isolation, or discrepancies and inconsistencies in different official sources, both at home and overseas only serve to sow the seeds of confusion. Politically-motivated commentary on the other hand, such as seeking to down-play or worse, dismiss the risks of exposure to COVID-19, creates distrust. Against this background of confusion and distrust, fear can then shift people’s behavior into doing unusual things—fighting over goods in supermarkets, selectively denuding the pharmacy shelves of toilet roll and hand wash, and so on. Panic buying in the shops is not only unnecessary; it also reinforces people’s fears and generates even more panic.
At its worst, fear and panic can also lead to stigmatization of those who are wrongly thought to be at fault in some way—in this case, people diagnosed with COVID-19 or even those who have travelled in areas where the outbreak began or has spread. According to the United Nations International Children’s Fund (UNICEF) and the WHO:
“Stigma can undermine social cohesion and prompt possible social isolation of groups, which might contribute to a situation where the virus is more, not less, likely to spread” (Clarke et al., 2006).
In addition to fear of the virus itself, fear of the impact of the virus on daily life through disruption and shortages contributes further to stigmatization and panic.
Both fear and panic also reduce our ability to fight the virus itself. Fear arguably reduces our resistance to fight illness. When fear creates panic and social crises by stimulating anti-social behavior and decision and actions that contradict the best medical and scientific advice (or even common sense), then the virus “wins” and our concerted efforts to control it become even more challenging.
So how do we break this vicious circle? Trust is critical for reducing fear and enabling effective communication and knowledge sharing. We need to identify and support knowledgeable, trusted sources of information and advice within our organizations and communities. To reduce fear and panic, it is essential that people “hear” the more sensible messages about COVID-19 and respond in a more measured way.
We refer to the words of wisdom by Michael O. Leavitt, a former Secretary of the US Department of Health and Human Services spoken on June 13, 2007 at a pandemic influenza leadership forum:
“We don’t know when a pandemic might strike. But we can be sure of two things. Everything we do before a pandemic will seem alarmist. Everything we do after a pandemic will seem inadequate. This is the dilemma we face, but it should not stop us from doing what we can to prepare. We need to reach out to everyone with words that inform, but not inflame. We need to encourage everyone to prepare, but not panic” (Leavitt, 2009).
Consistent, supportive efforts are needed to break the vicious circle of fear and panic in relation to COVID-19. A combination of strategies, required at both the public and individual levels, could include public engagement, support for individual self-adjustment through participation in stress-releasing activities, familial support, and even psychiatric help. As shown in Fig. 1, the following societal-level measures are essential to break the circle of fear and panic:
• False news needs to be exposed rapidly for what it is; otherwise, social media will embed misinformation, such as false causal claims, into the public consciousness.
• The health authorities need to be aware that their statements and advice have health effects themselves. Their guidance—to wear or not to wear a mask, or on the need for and extent of physical (“social”) distancing—needs to be clear and consistent.
• The press and media need to avoid inflammatory language that generates fear and panic.
• The scientific community needs to avoid unnecessary jargon but also resist entering into scientific debates that may have the effect of confusing or undermining health messaging.
The reactions of people to information about and advice on this pandemic will be based on their level of trust in the sources of that information, and on their perception of the risks. This correlation needs to be understood from the outset in order to reduce the potential for normal fear and anxiety to grow into lack of trust spirals into panic that in turn generates stigmatization and xenophobia.
Footnotes
Contributors: Both Kwan Hoong NG and Ray KEMP have taken part equally in the conception, drafting, editing, and approval of the final article.
Compliance with ethics guidelines: Kwan Hoong NG and Ray KEMP declare that they have no conflict of interest.
This article does not contain any studies with human or animal subjects performed by either of the authors.
References
- 1.Clarke L, Chess C, Holmes R, et al. Speaking with one voice: risk communication lessons from the US anthrax attacks. J Conting Crisis Manage. 2006;14(3):160–169. doi: 10.1111/j.1468-5973.2006.00491.x. [DOI] [Google Scholar]
- 2.Covello V, Hyer R. COVID-19: Simple Answers to Top Questions, Risk Communication Guide. Association of State and Territorial Health Officials, Arlington, Virginia, USA; 2020. [Google Scholar]
- 3.Kasperson JX, Kasperson RE. The Social Contours of Risk: Publics, Risk Communication and the Social Amplification of Risk (Volume 1) Earthscan, London, UK; 2005. [Google Scholar]
- 4.Leavitt MO. Quoted by Slepski LA Foreword (p. vii) in Ryan JR. Pandemic Influenza. Emergency Planning and Community Preparedness. CRC Press, Boca Raton, Florida, USA; 2009. [Google Scholar]
- 5.McKay D, Yang HB, Elhai J, et al. Anxiety regarding contracting COVID-19 related to interoceptive anxiety sensations: the moderating role of disgust propensity and sensitivity. J Anxiety Disord, 73:102233. 2020 doi: 10.1016/j.janxdis.2020.102233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pulido CM, Villarejo-Carballido B, Redondo-Sama G, et al. COVID-19 infodemic: more retweets for science-based information on coronavirus than for false information. Int Sociol. 2020;35(4):377–392. doi: 10.1177/0268580920914755. [DOI] [Google Scholar]
- 7.Slovic P. The Perception of Risk. Earthscan Publications, London, UK; 2000. [Google Scholar]
- 8.WHO (World Health Organization) Effective Media Communication During Public Health Emergencies: a WHO Handbook. World Health Organization, Geneva, Switzerland; 2007. [Google Scholar]
- 9.Wu ZY, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 10.Zarocostas J. How to fight an infodemic. Lancet. 2020;395(10225):676. doi: 10.1016/S0140-6736(20)30461-X. [DOI] [PMC free article] [PubMed] [Google Scholar]