Abstract
In Japan, the first case of COVID‐19 in dialysis patients was reported on March 1, 2020. A total of 31 cases were reported by April 10, and it increased to 95 by May 15. Thereafter, with the rapid increase in the number of COVID‐19 cases in the general population since late March, there was a not surprising increase in the number of COVID‐19 cases in dialysis patients. The mortality rate is 16.2% (16/99 cases) in dialysis patients, which is higher than 5.3% (874/16 532 cases) in the general population. This higher mortality rate in dialysis patients with COVID‐19 might be related to their age; the majority of COVID‐19 cases are aged between 70 and 90 years old in dialysis patients, compared with between 20 and 60 years old in the general population. As COVID‐19 presents with severe symptoms and is associated with a high mortality rate in dialysis patients, dialysis patients who have contracted severe acute respiratory syndrome coronavirus 2 infection confirmed by polymerase chain reaction testing are required to be hospitalized under Japanese government policy. In cases of COVID‐19 hospitalizations, it is essential to prevent nosocomial infection. Therefore, patients must be sufficiently instructed in infection prevention and robust measures to prevent contraction and spread of the infection must be taken at dialysis facilities.
Keywords: COVID‐19, dialysis, guidance, infection control, severe acute respiratory syndrome coronavirus 2 infection
1. INTRODUCTION
A new coronavirus infection, COVID‐19 (as named by the World Health Organization [WHO]), which was reported in Wuhan City, Hubei Province, China, has spread worldwide since December 2019. On January 30, 2020, WHO Director‐General declared the outbreak as a Public Health Emergency of International Concern, and later characterized COVID‐19 as a pandemic on March 11. 1 As of May 29, the number of confirmed cases of COVID‐19 had reached 5 704 736 and the number of confirmed deaths had reached 357 736, with reported cases in every continent other than Antarctica. 1
In Japan, the first patient with COVID‐19, identified as severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), was detected on January 16, 2020, in patients with pneumonia who had visited Wuhan City. The number of confirmed cases of COVID‐19 in Japan has gradually increased since then, and started rapidly increasing in late March. Therefore, to stem the spread of SARS‐CoV‐2 infection, the Japanese government decided to place all of Japan under a state of emergency on April 16.
To address measures for dialysis facilities, the Japanese Association of Dialysis Physicians has released guidance and its updates for infection control in dialysis patients with COVID‐19 since the outbreak, on February 6, February 26, March 4, and April 4. 2 , 3 , 4 , 5 In addition, the Working Group of COVID‐19 Control was formed on February 28. Following the first reported case of COVID‐19 in dialysis patients on March 1, a nation‐wide online seminar, entitled “Current Status of COVID‐19 and Infection Control at Dialysis Facilities,” was held on March 16 to lay out details of the preparation and practice of infection control.
Herein, we report the current status of COVID‐19 in dialysis patients and the practice of infection control in dialysis facilities in Japan.
2. CURRENT STATUS OF COVID‐19 IN DIALYSIS PATIENTS IN JAPAN (AS OF MAY 29, 2020)
2.1. Number of cases of confirmed COVID‐19 and its mortality in dialysis patients in Japan
The Japanese Association of Dialysis Physicians and the Japanese Society for Dialysis Therapy formed the COVID‐19 Control Joint Committee on April 6, 2020. The Japanese Society of Nephrology joined on May 12; three academic organizations have been running the committee since then. The committee was formed to grasp the number of cases nation‐wide and negotiate with government agencies.
In Japan, the first case of COVID‐19 in dialysis patients was reported on March 1, 2020. A total of 31 cases were reported by April 10, and then 99 by May 29 (Table 1). With the rapid increase in the number of COVID‐19 cases in the general population since late March, increase in the number of COVID‐19 cases in dialysis patients was expected. We started data collection regarding the incident COVID‐19 patients on dialysis since April 9 as well as known patients with the disease until then. The COVID‐19 Control Joint Committee asked all dialysis facilities in Japan to report any patients who were confirmed to have COVID‐19 to the committee by using a dedicated Excel file. The collected data included patient background, medical history, the clinical course relating to COVID‐19, symptoms, findings in chest X‐ray or CT, and treatments against the disease. The data collection was approved by the ethical committee of the Japanese Society for Dialysis Therapy (approval #1‐8). Confirmed cases of COVID‐19 were more likely to be male (69 vs 29 cases, and one missing information), which may be the reflection of the gender ratio of the entire dialysis population in part. A total of 39 of 62 cases (62.9%, excluding the number of cases with missing information) had confirmed contact with a person with SARS‐CoV‐2 positive, in other words remaining 23 patients were considered infected without any known sources.
TABLE 1.
Cumulative number of confirmed COVID‐19 cases and death due to COVID‐19 in dialysis patients in Japan
| April 10 | April 17 | April 24 | May 1 | May 8 | May 15 | May 22 | May 29 | |
|---|---|---|---|---|---|---|---|---|
| COVID‐19, n | 31 | 47 | 59 | 70 | 76 | 95 | 96 | 99 |
| Death due to COVID‐19, n | 3 | 4 | 4 | 6 | 9 | 12 | 14 | 16 |
The mortality rate was 16.2% (16/99 cases) in dialysis patients, which was higher than 5.3% (874/16 532 cases) in the general population. However, the high mortality rate in dialysis patients with COVID‐19 might be related to their age; the majority of COVID‐19 cases are aged between 70 and 90 years old in dialysis patients, compared with between 20 and 60 years old in the general population. In general, mortality rapidly increases after age 70 years old (Figures 1 and 2). The mortality rate was 1.6 times higher in dialysis patients compared to the general population (30.4% [7/23 cases] vs 18.9% [327/1733 cases]) in those aged ≥80 years old; however, the gap is smaller.
FIGURE 1.
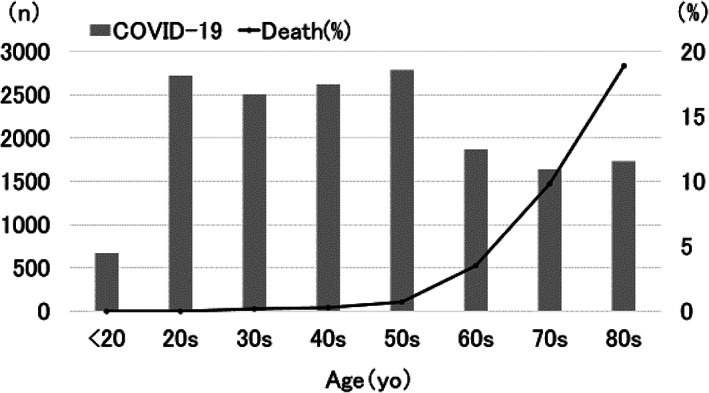
Cases with COVID‐19 in the general population in Japan (as of May 27, 2020). Data are based on the report of the Japanese Ministry of Health, Labour and Welfare as on May 27, 2020, at 6 pm. The mortality rate is higher in cases aged ≥70 years old compared to 5.3% in the overall general population
FIGURE 2.
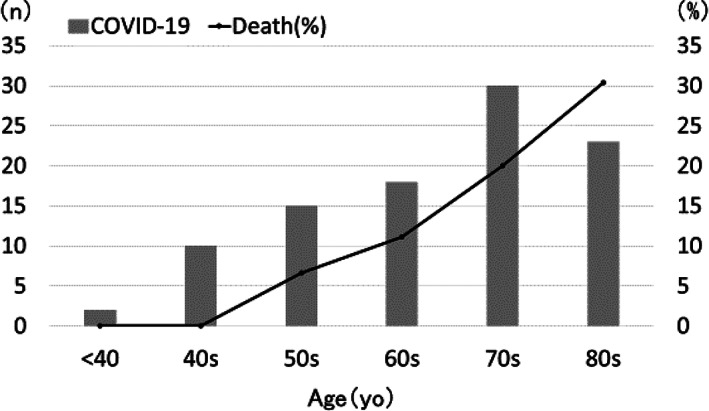
Cases with COVID‐19 in dialysis patients in Japan (as of May 29, 2020). Data is based on the case report from dialysis facilities in COVID‐19 Control Joint Committee as of May 29, 2020, at 8 am. The mortality rate is higher in cases aged ≥70 years old compared to 16.2% in overall dialysis patients
2.2. Initial symptoms, computed tomographic imaging, and treatment
The common symptom at the onset of illness was fever (body temperature of 37.5°C or higher), which was reported in 95.1% (79/83 cases, excluding the number of cases with missing information). This is partly due to that the body temperature elevation was the trigger to test COVID‐19 on the patients. Cough was reported in 63.5% (47/74 cases, excluding the number of cases with missing information). Patients with fever should be suspected of having COVID‐19 and undergo polymerase chain reaction (PCR) testing and/or CT imaging. CT imaging would help to diagnose COVID‐19; 89.2% (50/56 cases, excluding the number of cases with missing information) presented the typical CT features of COVID‐19 pneumonia.
About half of the total cases underwent hypoxemia treatment (including oxygenation in 37 cases, mechanical ventilation in 12 cases, and extracorporeal membrane oxygenation in three cases). Therefore, in Japan, COVID‐19‐suspected dialysis patients are immediately hospitalized to prevent worsening conditions.
Among 51 patients who had data for anti‐viral therapy, anti‐influenza drug favipiravir was administered in 31 cases, and inhaled corticosteroid ciclesonide was administered in 15 cases. At the time of preparation of this manuscript, the outcomes of patients were not clear since most of the cases were still hospitalized and underwent treatment.
3. MEASURES FOR COVID‐19 IN DIALYSIS FACILITIES IN JAPAN
3.1. Medical care system for patients with COVID‐19
Due to the Japanese government policy, dialysis patients who have contracted SARS‐CoV‐2 infection as confirmed by PCR testing must be hospitalized, even in the absence of symptoms consistent with COVID‐19, while the general population can be quarantined in designated accommodations outside of hospitals if they have no or little symptom. This is because dialysis patients are more likely to express more severe symptoms and this cohort's mortality rate is higher than that of the general population. Under these circumstances, the local government and medical professionals involved in dialysis treatment (eg, dialysis coordinators) must work together to secure hospital beds and determine hospitalization destinations based on severity.
3.2. Measures for COVID‐19 in dialysis facilities (2‐5)
The guidance issued by the Japanese Association of Dialysis Physicians instructs the facilities to follow the following measures against COVID‐19:
Instruct patients to measure body temperature and keep track of his/her health condition daily.
Instruct the patients to call dialysis facility to report fever or colds before their visit.
The doctor who receives the call from the patient makes a comprehensive judgment and contacts the COVID‐19 consultation center if COVID‐19 is suspected.
If the COVID‐19 consultation center determines that a PCR test is necessary, a COVID‐19 specialized outpatient clinic performs the test; the patient should be hospitalized if the PCR results show SARS‐CoV‐2 infection positive.
Instruct the patient to wear a mask and not use public transportation when he/she is suspected of having COVID‐19 and visits the dialysis facility until receiving PCR results.
Instruct the patient to maintain sufficient distance from all other patients upon arrival at the facility.
In the dialysis station, take measures to prevent droplet and contact infections in addition to standard preventive measures.
Private room isolation is recommended for dialysis; when private room isolation dialysis is not available, perform dialysis while maintaining a distance of at least 2 m from other beds (considering the spray distance of 2 m).
Use appropriate personal protective equipment (PPE), including disposable gowns, surgical masks, goggles or face shields, and disposable gloves, to protect healthcare personnel when dialysis is performed.
Use disposable equipment as much as possible; if disposable equipment is not available, use non‐disposable equipment exclusively for infected patients and properly disinfect them after each dialysis.
Discard contaminated or potentially contaminated items as infectious waste in a waste container prepared at the bedside of each patient.
Discard PPE brought to the dialysis station in the prepared dedicated waste container as infectious waste before leaving the infected area.
Properly take off PPE to avoid contact infection.
Change linens such as bed sheets and pillowcases for each patient; other equipment including bed fences, tables, and dialysis machines, should be appropriately disinfected after each dialysis.
Use sodium hypochlorite 0.05% to 0.1% or alcohol 60% to 70% to disinfect equipment at the dialysis station.
Properly ventilate the dialysis station after dialysis.
4. DISCUSSION
This is the first report of the national status of COVID‐19 in dialysis patients in Japan. Patients with chronic kidney disease and maintenance hemodialysis patients are at increased risk for COVID‐19 due to immunosuppression due along with presence of multiple comorbid conditions. Case series of 5700 patients with COVID‐19 admitted to 12 hospitals in New York within the Northwell Health system showed baseline comorbidities of chronic kidney disease in 5% and end stage kidney disease in 3.5% of patients hospitalized with COVID‐19, respectively. 6 Further, analysis of 20 133 patients in hospital with COVID‐19 at 208 acute care hospitals in UK revealed that chronic kidney disease was one of the commonest comorbidities (16%). 7 The logistical aspects within a dialysis facility further increase the risk of disease transmission. 8 Although the number of prevalent dialysis patients in Japan is 339 841 and is the second most per population in the world, 9 the number of COVID‐19 infection in dialysis patients was unexpectedly small. The number of COVID‐19 infection per general population in Japan is also the smallest among G7 countries, and this is a mystery. There can be several reasons including cultural background, that is, wearing masks in the winter and lack of customs of shaking hands or hugs. In addition, we believe that our practice of infection in dialysis facilities in Japan worked well.
An important question is whether the prognosis of dialysis patients is bad. The original observation in China suggested that dialysis patients might show milder disease phenotypes and die of cardiovascular complications rather than direct consequence of COVI‐19 infection. 10 One potential explanation for mild clinical disease in dialysis patients is immunosuppressive status in dialysis patients, which may preclude cytokine storm, a critical mediator of aggravation of COVID‐19. 11 Another potential explanation for this is usage of anti‐coagulants during dialysis treatment as hypercoagulation plays a critical role in aggravation of COVID‐19. 12
However, Goicoechea et al reported a mortality rate of 30.5% of dialysis patients that were admitted to a tertiary hospital in Madrid. 13 Further, Alberici et al reported the high rate of overall mortality (29%) at four outpatient dialysis facilities that are part of “Brescia Renal COVID task force” in spite of the mild form of symptomatology at presentation. 14 In addition, while certain patients were deemed more stable and managed in the outpatient facility, three of those subsequently died and a substantial portion had significant worsening of their symptoms. Of note, one should pay attention to absence of symptoms even in the presence of hypoxia in patients with COVID‐19, which is called “happy hypoxia” or “silent hypoxia.” 15 The dialysis patients have higher prevalence of heart failure or lung congestion by which they experience chronic hypoxia [NEJM 363:1833, 2010]. They may not experience dyspnea even if they have low oxygen tension. The early detection or recognition of this disease is warranted by other popular symptoms such as fever observed in this study, especially in these hypoxia‐prone patients. While the mortality rate of dialysis patients in Japan was higher than that of the general population (16.2% vs 5.3%), the difference becomes smaller if the age factor is considered. To conclude whether the prognosis of dialysis patients with COVID‐19 is worse than the general population, we need to perform multivariate analysis, taking various factors such as age and comorbidities into account.
The patients got various treatments, but the effects of these treatments remain obscure. In the urgency of treatment, many clinical trials of COVID‐19 are small, do not include an appropriate control group, and do not test drugs on enough number of patients to provide statistically meaningful power. 16 We definitely need more rigorous and scientific approach to find out appropriate treatment against COVID‐19.
5. CONCLUSION
This is a report of the current status of COVID‐19 in dialysis patients and the practice guidance of infection control in dialysis facilities in Japan. Dialysis patients are at high risk of severe symptoms and death during the COVID‐19 outbreak; thus, preventing infection of severe acute respiratory syndrome coronavirus 2 is mandatory. Instructing patients on how to prevent infection and to abide by appropriate preventive measures for COVID‐19 in dialysis facilities is essential to prevent the spread of the infection.
6. CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
COVID‐19 Task Force Committee of the Japanese Association of Dialysis Physicians The Japanese Society for Dialysis Therapy The Japanese Society of Nephrology Kikuchi K, Nangaku M, Ryuzaki M, et al. COVID‐19 of dialysis patients in Japan: Current status and guidance on preventive measures. Ther Apher Dial. 2020;24:361–365. 10.1111/1744-9987.13531
Contributor Information
Kan Kikuchi, Email: kankikuchi@nifty.com.
Tadao Akizawa, Email: akizawa@med.showa-u.ac.jp.
REFERENCES
- 1. World Health Organization . Coronavirus disease (COVID‐19) pandemic [cited 2020 Mar 11]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- 2. The Japanese Association of Dialysis Physicians . The first issue on the measures against SARS‐CoV2 associated pneumonia in dialysis facilities [in Japanese]. Available from: http://www.touseki‐ikai.or.jp/htm/03_info/doc/20200204_corona_virus_1.pdf
- 3. The Japanese Association of Dialysis Physicians . The second issue on the measures against SARS‐CoV2 associated pneumonia in dialysis facilities [in Japanese]. Available from: http://www.touseki‐ikai.or.jp/htm/03_info/doc/20200226_corona_virus_4.pdf
- 4. The Japanese Association of Dialysis Physicians . The third issue on the measures against COVID‐19 in dialysis facilities [in Japanese]. Available from: http://www.touseki-ikai.or.jp/htm/03_info/doc/20200304_corona_virus_6.pdf
- 5. The Japanese Association of Dialysis Physicians . The third issue on the measures against COVID‐19 in dialysis facilities [in Japanese]. Available from: http://www.touseki-ikai.or.jp/htm/03_info/doc/20200401_corona_virus_11.pdf
- 6. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID‐19 in the new York City area. JAMA. 2020;e206775. 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Docherty AB, Harrison EM, Green CA, et al. ISARIC4C investigators. Features of 20 133 UK patients in hospital with covid‐19 using the ISARIC WHO clinical characterisation protocol: Prospective observational cohort study. BMJ. 2020;369:m1985. 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ikizler TA. COVID‐19 in dialysis patients: Adding a few more pieces to the puzzle. Kidney Int. 10.1016/j.kint.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harris DCH, Davies SJ, Finkelstein FO, et al. Increasing access to integrated ESKD care as part of universal health coverage. Kidney Int. 2019;95(suppl):S1–S33. [DOI] [PubMed] [Google Scholar]
- 10. Naicker S, Yang C‐W, Hwang S‐J, Liu B‐C, Chen J‐H, Jha V. The novel coronavirus 2019 epidemic and kidneys. Kidney Int. 2020;97:824–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zhang X, Tan Y, Ling Y, et al. Viral and host factors related to the clinical outcome of COVID‐19. Nature. 2020. 10.1038/s41586-020-2355-0. [DOI] [PubMed] [Google Scholar]
- 12. Tang N, Li D, Wang X, Sun Z, Tang N, et al. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Goicoechea M, Sánchez Cámara LA, Macías N, et al. COVID‐19: Clinical course and outcomes of 36 maintenance hemodialysis patients from a single center in Spain. Kidney Int. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Alberici F, Delbarba E, Manenti C, et al. A report from the Brescia Renal COVID task force on the clinical characteristics and short‐term outcome of hemodialysis patients with SARS‐CoV‐2 infection. Kidney Int. 2020. 10.1016/j.kint.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Couzin‐Frankel J. The mystery of the pandemic's “happy hypoxia”. Science. 2020;368:455–456. [DOI] [PubMed] [Google Scholar]
- 16. Editorial . Coronavirus drugs trials must get bigger and more collaborative. Nature. 2020;581:120. [DOI] [PubMed] [Google Scholar]


