To the editor
With a potential COVID19-induced ventilator shortage, supporting multiple patients on a single ventilator seems a simple solution to maximize resources. Described by Neyman et al. [1], this practice has anecdotally been used in the 2017 Las Vegas mass shooting and more recently in Italy and New York during the COVID-19 pandemic. However, a recent consensus statement from relevant medical associations discouraged the practice based on safety concerns [2]. Beyond cross-contamination and increased dead space, matching patients to ensure appropriate individual ventilation peak pressures (Ppeak), tidal volumes (Vtidal), and positive end-expiratory pressures (PEEP) is a concern, especially given the dynamic clinical presentation of the COVID19 patients with complicated acute respiratory distress syndrome (ARDS). The central question remains: What does it mean to match patients? How much can they differ before we are no longer saving two lives but risking both?
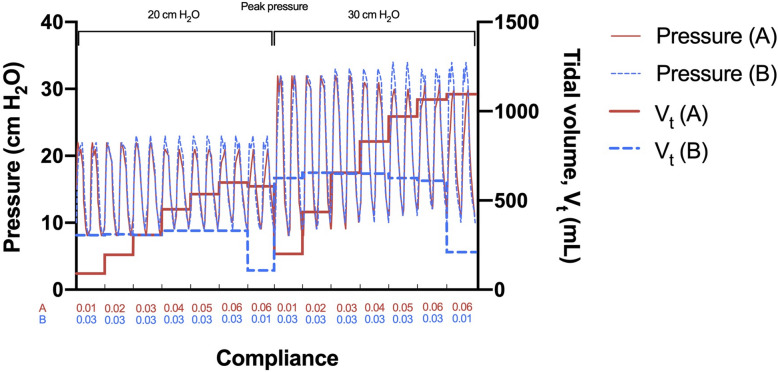
To illustrate the effect of progressive mismatching, we ventilated two mechanical lungs (TTL3, Michigan Instruments) on a ventilator (840, Puritan Bennett™) using pressure control mode and ARDS-compatible settings (Ppeak = 20–30 cmH2O; R = 20 bpm; Ftotal = 24 l/min; I = 1.5 s; PEEP = 8 cmH2O) [3]. While keeping patient B at constant pulmonary compliance (0.03 l/cmH2O), we let patient A progressively deteriorate in compliance from 0.06 to 0.01 l/cmH2O, finally creating a maximum mismatch between patients (see Fig. 1). One-way valves on both inspiratory and expiratory limbs ensured unidirectional flow, which both reduces functional dead space and the risk of cross-contamination between patient A and B, and seemingly also facilitated stable ventilation of B as A deteriorated. Importantly though, simultaneous and opposite changes in compliance made it possible to fatally hypo-ventilate one patient and hyper-ventilate the other without triggering alarms. As ventilator alarms are triggered only by changes in the sum of the pressure/volume of both patients on the circuit, we recommend a narrow alarm range (e.g., Vtidal ± 200 ml; Ftotal ± 1 L; Ppeak ± 5 cmH2O). The one-way valves on each expiratory limb prevent backflow but introduce a risk of competing exhalation: a slightly earlier or more forceful expiration from A can (partly) impair B and worsen breath staggering, particularly at higher respiration rates.
Fig. 1.
Patients A (red line) and B (blue line) pressure curves and average tidal volumes during positive pressure ventilation, using pressure control mode mechanical ventilation at 20 and 30 cmH2O and PEEP of 8 cmH2O. One-way valves ensured stable tidal volumes of B while A deteriorated; however, a severe mismatch holds the potential for fatal simultaneous hyper- and hypo-ventilation without triggering alarms
Frequent or constant monitoring of patients and shuffling when a mismatch arises is recommended. Asthma or COPD may increase the rate of fatal mismatch, making the method even more unpredictable. Finally, each class of ventilators requires a specific set up; if the method is considered, use the calm before the patient surge to familiarize, and ameliorate the many risks associated with sharing a ventilator.
Acknowledgements
The authors acknowledge UCSD from deans, chairs, and staff for allowing work directed to meet the medical emergency.
Authors’ contributions
All authors contributed equally to the data collection, analysis, and interpretation. All authors edited the letter and approved the final version prior to submission. The author(s) read and approved the final manuscript.
Funding
No funding was applied for this work.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
N/A
Consent for publication
N/A
Competing interests
The authors declare that they have no competing interests financial or otherwise.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Neyman G, Irvin CB. A single ventilator for multiple simulated patients to meet disaster surge. Acad Emerg Med. 2006;13(11):1246–1249. doi: 10.1197/j.aem.2006.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Joint Statement on Multiple Patients Per Ventilator. The Society of Critical Care Medicine (SCCM), American Association for Respiratory Care (AARC), American Society of Anesthesiologists (ASA), Anesthesia Patient Safety Foundation (APSF), American Association of Critical-Care Nurses (AACN), and American College of Chest Physicians (CHEST). March 26, 2020 (https://www.asahq.org/about-asa/newsroom/news-releases/2020/03/joint-statement-on-multiple-patients-per-ventilator)..
- 3.Beitler JR, Kallet R, Kacmarek R, Branson R, Brodie D, Mittel AM, Olson M, Hill LL, Hess D, Thompson BT. Ventilator sharing protocol: dual-patient ventilation with a single mechanical ventilator for use during critical ventilator shortages. Columbia University College of Physicians & Surgeons, New York-Presbyterian Hospital. Version 3: March 24, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.