Abstract
The financial implications of breast cancer diagnosis may be greater among rural and black women. Women with incident breast cancer were recruited as part of the Carolina Breast Cancer Study. We compared unadjusted and adjusted prevalence of cancer-related job or income loss, and a composite measure of either outcome, by rural residence and stratified by race. We included 2435 women: 11.7% were rural; 48.5% were black; and 38.0% reported employment changes after diagnosis. Rural women more often reported employment effects, including reduced household income (43.6% vs 35.4%, two-sided χ2 test P = .04). Rural white, rural black, and urban black women each more often reported income reduction (statistically significant vs. urban white women), although these groups did not meaningfully differ from each other. In multivariable regression, rural differences were mediated by socioeconomic factors, but racial differences remained. Programs and policies to reduce financial toxicity in vulnerable patients should address indirect costs of cancer, including lost wages and employment.
Patients with cancer face substantial financial burden associated with their diagnosis and treatment, including high out-of-pocket costs, time away from work, and difficulty coordinating clinical care (1). Financial burden as a result of cancer has been associated with reduced quality of life, lower medication adherence, and increased mortality (2–4).
Cancer’s effect on an individual’s ability to work has garnered considerable attention (5). Research suggests that uninsured, younger, and minority populations are at higher risk for employment changes following cancer diagnosis (1,6), but rural patients—a population with disparate cancer outcomes including later-stage diagnoses (7), less guideline-concordant care (8), and higher mortality (9,10)—remain understudied. We used a population-based cohort study oversampling black women and women aged younger than 50 years to examine the interaction of rurality and race on employment following breast cancer diagnosis.
Data are from the Carolina Breast Cancer Study (CBCS); the study design has been published previously (6). From the period 2008 to 2013, 2998 women across 44 North Carolina counties were identified and recruited at the time of breast cancer diagnosis, and they completed a medical history survey questionnaire. Women provided written informed consent, and all study activities were approved by the University of North Carolina’s institutional review board. Approximately 25 months after their diagnosis, 2506 women (83.5%) answered additional questions assessing financial effects. Women reported cancer-related job loss (Did you lose your job due to your diagnosis of breast cancer?) and income reduction (Has there been a decrease in your family income since your diagnosis of breast cancer?). A composite measure of any employment effect was created, indicating women answering yes to either question. Women who reported never working were excluded (n = 59).
Rurality was defined using 2013 Rural-Urban Continuum Codes (RUCCs) matched to county of residence at diagnosis (11). The 9-level RUCC was collapsed into a binary variable, with metropolitan counties (RUCC < 4) designated as urban and all other counties (RUCC ≥ 4) designated as rural. Race was defined via self-report as either black or white, with other races (n = 12) excluded because of small numbers. We performed χ2 analysis to examine rural-urban differences in participant characteristics and multivariable logistic regression to determine the relationship between rural residence, race, and employment-related factors, adjusting for clinical and socioeconomic characteristics. Analyses incorporated survey weights to account for oversampling by race and were performed with Stata 15 (College Station, TX). All statistical tests were two-sided and a P value of less than .05 was considered statistically significant.
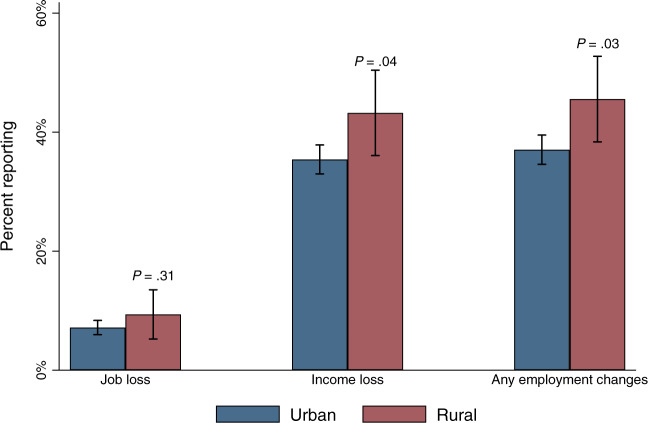
Of 2435 women included, half were black (48.5%; n = 1191; Supplementary Table 1 [available online]), and 11.7% lived in a rural area (n = 285). Rural women reported lower household incomes (41.4% vs. 31.3% less than $30 000 per year, X2 test = P < .001) and were less likely to work in white-collar occupations (55.1% vs 72.4%, P < .001), but had no statistically significant differences in stage at diagnosis (P = .33). Compared with urban women, rural women were more likely to report income loss (43.3% vs 35.4%, P = .04) or any employment effect (45.6% vs 37.1%, P = .03) (Figure 1). Job loss following breast cancer diagnosis was similar for urban and rural women (9.4% vs 7.2%, P = .31). When further stratified by race (Figure 2), we found that rural white (44.8%, P = .02), rural black (47.9%, P = .001), and urban black women (50.2%, P < .001) were all at statistically significantly higher risk for cancer-related employment effects relative to urban white women (33.5%).
Figure 1.
Employment effects following breast cancer diagnosis by urban or rural status. The statistical significance of the differences between urban and rural were assessed using a two-sided X2 test; results are weighted to account for designed oversampling. Bars represent 95% confidence intervals.
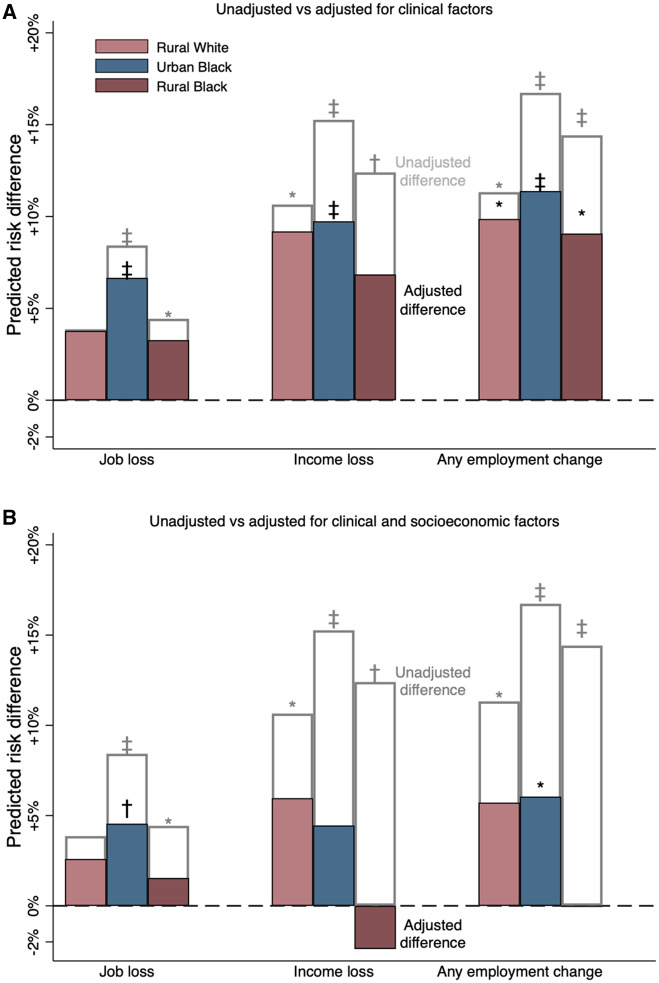
Figure 2.
Adjusted difference in cancer-related employment effects relative to white women. Unfilled bars indicate unadjusted risk difference; filled bars represent differences after adjusting for [Panel A] clinical characteristics (age, stage at diagnosis, comorbidity burden, and receipt of chemotherapy, radiation, adjuvant endocrine therapy, Herceptin, and surgery) or [Panel B] clinical and socioeconomic characteristics (household income, educational attainment, employment sector, insurance source, and marital status). Statistical significance of the difference from urban white women was assessed using a two-sided Wald test. * P < .05; † P < .01; ‡ P < .001.
To understand factors that mediate the relationship between race, rurality, and employment, we controlled for selected clinical and socioeconomic factors. Clinical factors included age and stage at diagnosis, treatments received (chemotherapy, radiation, trastuzumab, endocrine therapy, and mastectomy), and comorbidities (obesity, diabetes, and hypertension). Socioeconomic factors included household income, education, employment sector (white-collar vs any other sector [12]), insurance type, and marital status.
After adjusting for clinical differences (Figure 2A), risk of cancer-related employment effects remained higher in rural white (risk difference [RD] = 9.5, 95% confidence interval [CI] = 0.5 to 19.2), urban black (RD = 11.4, 95% CI = 6.6 to 16.1), and rural black (RD = 9.1, 95% CI = 0.3 to 17.8), relative to urban White women. Controlling both for clinical and socioeconomic differences, a small gap remained for rural white (RD = 5.7, 95% CI = −3.5 to 15.0) and urban black (RD = 6.1, 95% CI = 0.8 to 11.3) relative to urban white women (Figure 2B); this difference was statistically significant only for urban black women (P = .02). For rural black women, the increased risk of employment effects was explained fully by clinical and socioeconomic differences. Characteristics that increased the risk of employment effects were younger age at diagnosis, receipt of chemotherapy, being separated or divorced, and lacking insurance (Supplementary Table 2, available online).
We found that the indirect financial burden of breast cancer was high—38.0% of women reported changes in employment within 2 years of diagnosis. Rural and nonwhite women were at a higher risk for experiencing employment effects related to their cancer diagnosis compared with urban white women. For both rural white and rural black women, socioeconomic differences appear to be the primary mediator of increased risk. Lower paying, blue-collar jobs—a disproportionate source of employment for rural and racial minority women—are less likely to have flexible work schedules and paid leave and may be more physically intensive, making it harder to continue working during treatment (13). For urban black women, higher risk for employment effects may be because of sources of disadvantage not accounted for, including unobserved characteristics of jobs and differential levels of social support (14).
We note several limitations and strengths of the study. Place of residence, marital status, and insurance were captured only at baseline and may have changed between diagnosis and follow-up. Household income was captured only at baseline; therefore, we are unable to compare with self-report of lost income. Finally, the population represents a single state, and, therefore, differences for rural populations may be narrowed in states with expanded Medicaid programs or wider employment protections than North Carolina’s. However, this work is strengthened by the intentional oversampling of black participants, as well as questions that specifically assess employment changes resulting from breast cancer.
Our findings suggest that employment changes after breast cancer diagnosis vary by both race and geography, with higher burden among rural and black women. Whereas clinical and socioeconomic differences may explain some of this risk, the extent to which these attenuate disparities also varies by population, suggesting different mechanisms and potentially different solutions for rural, minority, and rural minority groups. Researchers, policymakers, and practitioners seeking to reduce cancer-related financial burden must consider the indirect costs imposed on patients through employment changes, particularly for populations likely to be in jobs with fewer protections.
Funding
This research was supported, in part, by the University of North Carolina’s Cancer Care Quality Training Program (T32 CA116339) funded by the National Cancer Institute. It was also supported by the Cancer Prevention and Control Research Network (Cooperative Agreement Number U48-DP005017; 3 U48 DP005000-01S2, 3 U48 DP005014-01S2, 3 U48 DP005013-01S1A3, 5 U48 DP005006-05) funded by the Centers for Disease Control and Prevention, Prevention Research Centers Program, and the National Cancer Institute. Melinda Davis was supported by an NCI K07 award (1K07CA211971-01A1).
The CBCS Phase III was supported by the University Cancer Research Fund of North Carolina and the National Cancer Institute Specialized Program of Research Excellence in Breast Cancer (NIH/NCI P50-CA58223). Additional support has been obtained from the National Cancer Institute (P01CA151135) and the Susan B. Komen Foundation (CCR 15333140). The contents are solely the responsibility of the authors and do not necessarily represent the official view of the funders.
Notes
The funders had no role in the conception or design of the study; the collection, analysis, and interpretation of the data; the writing of the manuscript; or the decision to submit the manuscript for publication. The contents are solely the responsibility of the authors and do not necessarily represent the official view of the funders.
SBW receives unrelated grant funding to her institution from Pfizer. The other authors have no disclosures.
Supplementary Material
References
- 1. Yabroff KR, Dowling EC, Guy GP, et al. Financial hardship associated with cancer in the United States: findings from a population-based sample of adult cancer survivors. J Clin Oncol. 2016;34(3):259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ramsey SD, Bansal A, Fedorenko CR, et al. Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol. 2016;34(9):980–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lathan CS, Cronin A, Tucker-Seeley R, Zafar SY, Ayanian JZ, Schrag D.. Association of financial strain with symptom burden and quality of life for patients with lung or colorectal cancer. J Clin Oncol. 2016;34(15):1732–1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zafar SY, McNeil RB, Thomas CM, Lathan CS, Ayanian JZ, Provenzale D.. Population-based assessment of cancer survivors’ financial burden and quality of life: a prospective cohort study. J Oncol Pract. 2015;11(2):145–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NCI. Financial Toxicity and Cancer Treatment (PDQ®)-Health Professional Version. Bethesda, MD: NCI; 2018. [Google Scholar]
- 6. Wheeler SB, Spencer JC, Pinheiro LC, Carey LA, Olshan AF, Reeder-Hayes KE.. Financial impact of breast cancer in black versus white women. J Clin Oncol. 2018;36(17):1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nguyen-Pham S, Leung J, McLaughlin D.. Disparities in breast cancer stage at diagnosis in urban and rural adult women: a systematic review and meta-analysis. Ann Epidemiol. 2014;24(3):228–235. [DOI] [PubMed] [Google Scholar]
- 8. Wheeler SB, Kuo T-M, Durham D, Frizzelle B, Reeder-Hayes K, Meyer A-M.. Effects of distance to care and rural or urban residence on receipt of radiation therapy among North Carolina Medicare enrollees with breast cancer. N C Med J. 2014;75(4):239–246. [DOI] [PubMed] [Google Scholar]
- 9. Mokdad AH, Dwyer-Lindgren L, Fitzmaurice C, et al. Trends and patterns of disparities in cancer mortality among US counties, 1980-2014. JAMA. 2017;317(4):388.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Charlton M, Schlichting J, Chioreso C, Ward M, Vikas P.. Challenges of rural cancer care in the United States. Oncology (Williston Park). 2015;29(9):633–640. [PubMed] [Google Scholar]
- 11.United States Department of Agriculture. Rural-Urban Continuum Codes-2010. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx. Accessed July 14, 2018.
- 12. Arheart KL, Fleming LE, Lee DJ, et al. Occupational vs. industry sector classification of the US workforce: Which approach is more strongly associated with worker health outcomes? Am J Ind Med. 2011;54(10):748–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vanderpool RC, Swanberg JE, Chambers MD.. A narrative review of the confluence of breast cancer and low-wage employment and its impact on receipt of guideline-recommended treatment. Glob Adv Health Med. 2013;2(5):75–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Probst JC, Moore CG, Glover SH, Samuels ME.. Person and place: the compounding effects of race/ethnicity and rurality on health. Am J Public Health. 2004;94(10):1695–1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.