Introduction
Northwell Health, a 23-hospital, not-for-profit enterprise in New York, is located at the epicenter of the global coronavirus disease 2019 (COVID-19) pandemic.1, 2, 3 As an entity, Northwell Health serves a large portion of New York City and Long Island. Of its 2 flagship tertiary care academic medical centers, Long Island Jewish Hospital (LIJ) is a 583-bed teaching hospital located in Queens, NY, providing care to the eastern area of the borough and serving one of the most diverse populations in the United States. Anticipating this broad catchment area for the nation’s COVID-19 patients, we proactively enacted multimodal strategies to both increase capacity and provide advanced intensive care to the over 700 afflicted patients admitted to our medical center. Additionally, as one of the larger academic surgery departments, we made substantial adaptations to assignments of trainees and to coverage of the intensive care unit (ICU). Here we outline the rapid and versatile Northwell Acute Care Surgery COVID-19 Consortium Response of preventative measures and strategies of resource allocation which may serve as a road map to potential, future mass casualty disasters.
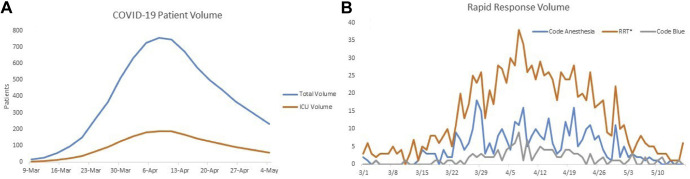
From the initiation of our Northwell Acute Care Surgery COVID Consortium Response Protocol in early March, inpatient COVID cases increased 44-fold from 16 patients to greater than 700 in mid-April. The rates of rapid responses and overhead codes increased dramatically, which required the immense capability to have free staff to address urgent clinical problems. Over time, 25% to 35% of these patients required mechanical ventilation and ICU-level care (Fig 1 ). Although fluctuations of patient volume occurred frequently, roughly 30% of critical care patients were under coverage by the surgery team. The creation of ICU surge areas increased the bed availability in the Surgery Intensive Care Unit from approximately 26 beds to 92 beds.
Fig 1.
Patient volume, total and ICU burden. A. The total patient volume was abstracted from system-provided data. With an average ICU admission rate of approximately 25%, the total ICU burden was approximated. This shows the patient flow into the ICU during the massive COVID+ influx. B. Rapid response volume of patients needing emergent therapy/intubation while in non-ICU settings. ∗RRT – Rapid Response Team
Within the first week of the uptick in COVID-19 admissions in Mar 2020, the Northwell-LIJ Department of Acute Care Surgery division, composed of 4, dual board-certified surgical intensivists and 1 medical intensivist, reconfigured their work flow to augment the COVID care delivered normally by the medical intensivists. To facilitate increased critical care coverage, the usual 75% of emergency general surgery covered by the Acute Care Surgery team (25% of the monthly emergency call schedule is typically covered by noncritical care board-certified general surgery voluntary faculty) was shifted to surgical subspecialists and other non-Acute Care Surgery general surgeons. On March 15, as per the mandate of the Governor of New York State, all elective inpatient operations were cancelled; however, most elective procedures were already tentatively delayed in anticipation of the crisis.
Pediatric, oncologic, minimally invasive, and colorectal surgery were easily folded into the general surgery schedule,4 and it should be noted that we are not a designated adult trauma hospital. Critical care-trained physicians were made readily available for discussion of case-by-case issues or for general questions by our non-ICU physicians. Once medical ICU space was filled, the reserve volume of surgical critical care areas were utilized and subsequently filled after the large influx of COVID-positive patients requiring ICU level of care. The rush of admissions mandated patient overflow into surgical floors and multiple ICU-capable makeshift units. In order to create physical space, the postanesthesia recovery unit, preoperative holding area, interventional recovery suite, and pediatric postanesthesia recovery unit (attached to Cohen Children’s Medical Center) were converted to ICU-capable units. Each unit was then labeled as a surge area (SURGE1, SURGE2, etc) and entered into the electronic medical record system as such. The stable and chronically ill were kept within the actual ICUs, and all new admissions were brought to the SURGE areas and surrounding converted spaces. This approach allowed the noncritical care surgeons (subspecialists) to care for the stably ill in a single location and lessened the burden on the critical care-boarded intensivists rounding on unstable patients. The Acute Care Surgery team was able to dedicate their time to the critically ill patients, supervise noncritical care surgeons deployed to COVID units, supervise residents and expand the available pool of intensivists. Noncritical care surgeons were paired with a surgical intensivist and refreshed on critical care rounding, checklists, and goals. An educational overview of ventilator strategies, antibiotic stewardship, and COVID-related treatments/protocols was provided for roughly 1 week before sole management of critical care patients. Weekly critical care meetings via web-based conferencing allowed up-to-date information to be disseminated and discussed. An effort was made to have chronically ill and/or stable patients transferred to the areas in which noncritical care surgeons would be rounding, leaving the unstable and new admissions for the surgical intensivists. The noncritical care surgeons managing COVID-ICU patients in the Surgery Intensive Care Unit were buttressed by the capable surgical ICU nurses with whom the surgeons and the nurses alike were accustomed to working.
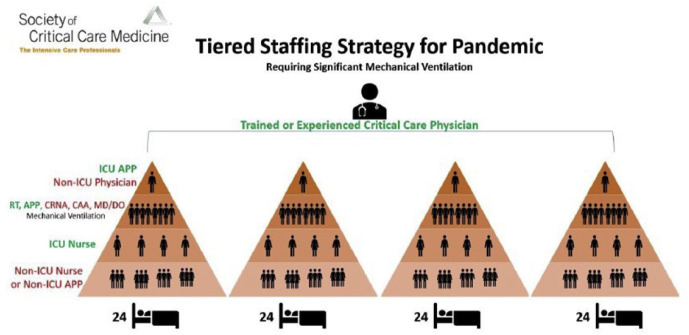
We adapted the tiered staffing strategy for the pandemic provided by the Society of Critical Care Medicine4 (Fig.2 ) as a model for how we would staff our ICUs. This strategy was proposed to the hospital leadership and incorporated into the broader institutional response. Each ICU provider had their unit/area specified for a 7 or 4 day/night rotation, allowing the surgical intensivist simultaneously to oversee non-ICU surgeon’s care within their respective units. An attempt to physically co-locate these units produced an easy commute to other areas of care. We deployed teams consisting of ICU physicians, non-ICU physicians, residents, physician assistants (PAs), and nursing staff. This approach allowed for rapid expansion of the physical capability to provide patient care. The PAs were fully competent in all phases of care of the surgical patient, including floor management and critical care, because they rotate through all these areas on a regular basis. Every PA takes a Fundamentals of Critical Care Support course sponsored by LIJ. From very early on in the pandemic, as elective surgical cases came to a halt, we averaged 1 to 3 emergency operations daily, and the census of surgical patients on the floor decreased. This allowed all the surgical PAs to be reassigned to cover COVID ICUs throughout the hospital. Having all PAs on the surgical service ICU-trained and capable is a unique feature of Long Island Jewish Medical Center compared to most Northwell hospitals.
Fig 2.
Adaptation from SCCM pandemic response protocol. Using a tiered approach, intensivists were used to oversee a large group of non-critical care surgeons and advanced clinical care providers. Residents were dispersed as above and were highly fluid within each group. ∗Used with permission from SCCM.
The Multidisciplinary Anesthesia/surgical Trainees COVID Response Team was developed on March 21, which included 158 trainees across the residency training programs in general surgery, integrated cardiothoracic surgery, integrated plastic surgery, orthopedic surgery, urology, anesthesiology, podiatry, and oral and maxillofacial surgery and the surgical specialty fellowships. The availability of surgery residents to cover the COVID units increased due to the halting of elective surgery. In addition, we pulled in 6 of our residents currently on hiatus for research to cover additional COVID ICUs. Within 48 hours, residents were staffing multiple ICUs.
By creating the aforementioned areas for patient care, the ability to spread critical care surgeons throughout ICUs with supplementary noncritical care surgeons afforded the hospital the means to deal with the daily influx of crashing patients. As shown in Fig 1, rapid responses and intubations on the medical floor increased dramatically and reflected the need for open ICU spaces to allow the rapid transport of patients. The physical allocation of COVID patients shifted over time to a renovated single COVID unit with capacity for greater than 60 patients. Once the numbers of new admission decreased and the ICU volume waned, this area became the center for medical and surgical COVID-patient care.
Recommendations and pitfalls to avoid
Potential pitfalls of using the tiered approach to pandemic response is overestimating the capability of the staff involved with direct patient care. We were able to be adequately staffed with enough intensivists and surgeons to allow continuity over a 5 to 7 day shifts with separate night coverage. The schedule was rotated so that we were able to maximize the contiguous days in-house and days off. If there is a paucity of critical care physicians, a tight and grueling schedule may lead to rapid burnout. In large part due to assiduous adherence to universal precautions and the hospital’s provision of adequate personal protective equipment to frontline workers, very few of our essential staff became infected and required time off during their illness. Planning for coverage should a staff member fall ill is a contingency which must be calculated into the schedule. Without adequate physician extenders, the tiered approach may be top-heavy and increase the burden on physicians and decrease the time they may spend with the critically ill.
In conclusion, this report differs from other surgical publications on the management of uniquely surgical issues (prioritization of surgical diseases and operating room utilization, surgical procedural teams, etc) in that we describe here how surgeons can be utilized as medical intensivists and how noncritical care-certified surgeons are trained rapidly to manage COVID-19 patients with supervision. The ability of our staff to adapt during this crisis that affected such an enormous number of patients is an important contribution. At the time of this writing, the medical community has been covered by an avalanche of publications from our medical, pulmonary, cardiology, and pediatric colleagues and relatively few from the perspective of surgeons managing medical disasters. The lessons of rapid triage, personal safety of the health care workers, team dynamics, and transport of patients to tertiary facilities from the widely successful educational campaigns hosted by the American College of Surgeons-Committee on Trauma and the Society of Critical Care Medicine were leveraged successfully by our surgical faculty, residents, and advanced care practitioners during this COVID-19 crisis.
Finally, the effort of the surgical staff to cross-cover their own specialty and critical care, to be redeployed, and to work with new team members was nothing short of Herculean. Given our unique training spanning from both the immediate response required during a mass casualty event (airplane crashes, mass shootings, bombings, etc), to the stabilization phase in the operating room, and ultimately to the recovery/rehabilitation phase, we were well prepared to apply our skills to contributing towards the global action required to restore healthy safety to our society. Our surgical staff exemplified Northwell’s primary mission of patient care. Continued support and the physical presence of administration and leadership created an environment where we were truly “in this together”, and where togetherness would triumph in an era of isolation. This response, based on the American College of Surgeons-Committee on Trauma and the Society of Critical Care Medicine guidance, underpins the importance of courses like Advanced Trauma Life Support, Fellowship in the American College of Critical Care Medicine and the leadership of the Accreditation Council for Graduate Medical Education. Most importantly, this highlights the significance of the critical care training requirements in preparing a versatile workforce capable of handling both traumatic and medical mass casualty events.
Conflict of interest/Disclosure
There are no personal conflicts of interests nor is there any financial compensation attached to this publication.
Funding/Support
There is no outside funding.
References
- 1.World Health Organization Coronavirus disease (COVID-19) pandemic; 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Accessed June 2, 2020.
- 2.New York Times. New York coronavirus map and case count; 2020. https://www.nytimes.com/interactive/2020/us/new-york-coronavirus-cases.html Accessed June 2, 2020.
- 3.Richardson S., Hirsch J.S., Narasimhan M. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DePeralta D.K., Hong A.R., Choy C. Primer for intensive care unit (ICU) redeployment of the noncritical care surgeon: insights from the epicenter of the coronavirus disease 2019 (COVID-19) pandemic. Surgery. 2020;168:215–217. doi: 10.1016/j.surg.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]