Abstract
Objective
The coronavirus disease 2019 (COVID-19) pandemic has had a significant impact on imaging utilization across practice settings. The purpose of this study was to quantify the change in the composition of inpatient imaging volumes for modality types and Current Procedural Terminology–coded groups during the COVID-19 pandemic.
Methods
A retrospective study of inpatient imaging volumes in a large health care system was performed, analyzing weekly imaging volumes by modality types (radiography, CT, MRI, ultrasound, interventional radiology, nuclear medicine) in years 2020 and 2019. The data set was split to compare pre-COVID-19 (weeks 1-9) and post-COVID-19 (weeks 10-16) periods. Further subanalyses compared early post-COVID-19 (weeks 10-13) and late post-COVID-19 (weeks 14-16) periods. Statistical comparisons were performed using χ2 and independent-samples t tests.
Results
Compared with 2019, total inpatient imaging volume in 2020 post-COVID-19, early and late post-COVID-19 periods, declined by 13.6% (from 78,902 to 68,168), 16.6% (from 45,221 to 37,732), and 9.6% (from 33,681 to 30,436), respectively. By week 16, inpatient imaging volume rebounded and was only down 4.2% (from 11,003 to 10,546). However, a statistically significant shift (P < .0001) in the 2020 composition mix was observed largely comprised of radiography (74.3%), followed by CT (12.7%), ultrasound (8%), MRI (2.4%), interventional radiology (2.3%), and nuclear medicine (0.4%). Although the vast majority of imaging studies declined, few Current Procedural Terminology–coded groups showed increased trends in imaging volumes in the late post-COVID-19 period, including CT angiography chest, radiography chest, and ultrasound venous duplex.
Discussion
During the COVID-19 pandemic, we observed a decrease in inpatient imaging volumes accompanied by a shift away from cross-sectional imaging toward radiography. These findings could have significant implications in planning for a potential resurgence.
Key Words: COVID-19, CPT-coded examinations, imaging volume, inpatient service, modality types
Introduction
The coronavirus disease 2019 (COVID-19) pandemic continues to significantly impact the health of the population, affecting a total of 1,859,693 people in the United States with 106,927 deaths as of June 2, 2020 [1]. New York state quickly became the US epicenter of COVID-19 disease, with 380,825 cases and 29,988 deaths [1] occurring in a short period of time. Hospitals had to become flexible to quickly expand inpatient units and provide appropriate resources for this rapidly growing cohort. Additionally, this novel disease population posed a challenge for health care providers to anticipate the necessary resources because new information about disease progression and complications was continually becoming available.
As medical resources shifted away from elective and nonurgent procedures toward emergent and critical care of patients with COVID-19, departments were forced to reconfigure their personnel and resources. In particular, many radiology practices rescheduled nonurgent and routine imaging according to recommendations from the ACR [2]. Hence, radiology practices experienced significant declines in imaging volumes, especially in the outpatient setting [3,4]. Although, the inpatient setting was not as severely affected by declines in imaging volumes, a shift was observed in the composition mix of imaging modality types with increased use of radiography relative to cross-sectional imaging [4]. These findings suggest a potential impact on the resource utilization, staffing needs, and reimbursement for radiology practices.
The purpose of this study was to evaluate the change in the inpatient imaging volumes and composition mix during the COVID-19 pandemic. We analyzed the weekly imaging volumes stratified by the imaging modality types and Current Procedural Terminology (CPT)-coded examination groups during the COVID-19 pandemic in a large health care system.
Methods
A retrospective review of the inpatient imaging case volumes in a large integrated health care system [4] was performed from January 1, 2019, to April 18, 2020, to evaluate the change in the imaging volumes and composition mix according to imaging modality types and CPT-coded examination groups during the COVID-19 pandemic. Similar to our prior methods [4], the weekly aggregated imaging volumes were provided in 2020 and 2019 for the inpatient service stratified by the imaging modality types (radiography, ultrasound, CT, MRI, nuclear medicine, and interventional radiology). Individual CPT-coded data within each modality type were also provided as weekly aggregated data to further evaluate the case volumes for specific types of imaging examinations. Overall, there was no significant decline in the number of imaging scanners in our health care system between 2020 and 2019 that could have potentially affected the expected imaging examination volumes during the COVID-19 pandemic. Institutional review board approved a waiver to use the retrospective aggregate data.
At our institution, the first patient testing positive for COVID-19 was confirmed on March 8, 2020 (week 11, day 1). However, the first patient testing positive for COVID-19 was confirmed on March 1, 2020 (week 10, day 1), in New York City. On March 27, 2020 (week 13, day 6), the radiology department released guidelines for inpatient imaging utilization to limit the spread of the coronavirus (severe acute respiratory syndrome coronavirus 2) to health care providers, staff, and patients, as well as to reduce contamination of imaging equipment from scanning patients with COVID-19 [4].
Statistical Analysis
The 2020 and 2019 aggregated weekly (weeks 1-16) imaging case volumes were stratified by imaging modality types (radiography, ultrasound, CT, MRI, nuclear medicine, and interventional radiology) and by individual CPT codes. For the analysis of the CPT-coded data, CPT groups were primarily assigned by anatomic regions (such as head; orbit, face, or neck; chest; abdomen or pelvis; and extremities) within each modality type. Noninvasive vascular imaging was assigned as separate CPT-coded groups according to the modality types and anatomic regions, such as CT angiography (CTA) head and MR angiography head. E-only Supplemental Tables S1 to S6 in the online Supplemental Materials show the categorization of the individual CPT codes into the specific groups used in the analysis.
The data set was split for analysis to compare the pre-COVID-19 (weeks 1-9) and post-COVID-19 (weeks 10-16) periods. Further subanalyses of the post-COVID-19 period was performed by splitting the data set into the early post-COVID-19 (weeks 10-13) period representing the transition phase during the rapid inpatient influx of patients with COVID-19 and the late post-COVID-19 (weeks 14-16) period representing the inpatient imaging volumes during the height of the pandemic. The 2019 week 1 (5 days) aggregate imaging volume was adjusted to reflect the same 4 days of imaging volume acquired in 2020 by removing 1 day of the average daily volume calculated in week 1 from the data analysis for similar comparisons.
The weekly imaging volumes were plotted for weeks 1 to 16 for the total inpatient imaging volume and stratified by imaging modality types and CPT-coded groups for both 2020 and 2019 to demonstrate the trends in service volumes. The number of services performed was aggregated for the total weeks 1 to 16, pre-COVID-19 and post-COVID-19 periods, and early and late post-COVID-19 periods according to the imaging modality types in 2020 and 2019. The 2020 percent difference in the total inpatient imaging volumes was calculated compared with 2019 for the total weeks 1 to 16, pre-COVID-19 and post-COVID-19 periods, early and late post-COVID-19 periods, and week 16. In these analyses, the same weeks in the 2020 and 2019 calendar years were compared with account for monthly or seasonal variation. The composition mix of the 2020 total imaging volume according to modality types during the late post-COVID-19 (weeks 14-16) period was compared with 2019. The χ2 test was used to assess statistical significance among categorical variables between 2020 and 2019.
For each modality type, the mean weekly imaging case volumes were calculated for the total weeks 1 to 16, pre-COVID-19 and post-COVID-19 periods, and early and late post-COVID-19 periods. The 2020 and 2019 mean weekly imaging volumes for each modality type were compared using independent-samples t tests for the total weeks 1-16, early post-COVID-19 (weeks 10-13), and late post-COVID-19 (weeks 14-16) periods. Additionally, the mean weekly imaging case volumes for each modality type were compared for the pre-COVID-19 (weeks 1-9) and post-COVID-19 (weeks 10-16) periods in 2020 and 2019 separately to assess statistical significance of the change in the post-COVD-19 period within the same calendar year. Further analyses were performed comparing the 2020 and 2019 mean weekly imaging case volumes for specific imaging examinations by CPT-coded groups during the late post-COVID-19 (weeks 14-16) period. P < .05 determined statistical significance. SAS version 9.4 (SAS, Cary, North Carolina) was used for all statistical analyses.
Results
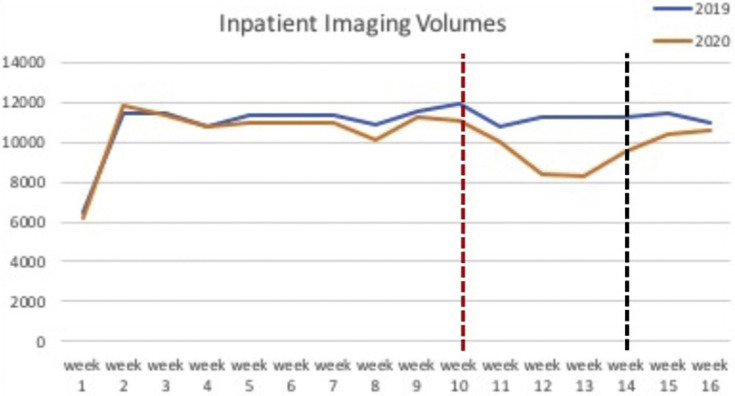
In 2020, the total inpatient imaging volume performed at our institution for weeks 1 to 16 was 162,470 examinations, compared with 175,511 examinations in 2019, representing an overall 7.4% decline. Table 1 shows the comparison of the 2020 and 2019 total inpatient imaging volume stratified by time periods for the total weeks 1 to 16, pre-COVID-19 (weeks 1-9) and post-COVID-19 (weeks 10-16) periods, early post-COVID-19 (weeks 10-13) and late post-COVID-19 (weeks 14-16) periods, and week 16. Overall, the 2020 inpatient imaging volume during the post-COVID-19 (weeks 10-16) period declined by 13.6% (from 78,902 to 68,168) compared with 2019. However, when further analyzing the post-COVID-19 period, a greater decline of 16.6% (from 45,221 to 37,732) was observed in the 2020 early post-COVID-19 (weeks 10-13) period. In the late post-COVID-19 (weeks 14-16) period, the 2020 inpatient imaging volume had a smaller decline of 9.6% (from 33,681 to 30,436). By week 16, the inpatient imaging volume only declined by 4.2% (from 11,003 to 10,546) compared with 2019. Figure 1 reveals the trends in the 2020 and 2019 total inpatient imaging volume across weeks 1 to 16. The 2020 total inpatient imaging volume began to decline in week 10 (when the first patient testing positive for COVID-19 was confirmed in New York City). However, total imaging volume started to increase in week 14, resulting in a smaller decline in the late post-COVID-19 (weeks 14-16) period.
Table 1.
Comparison of the 2020 and 2019 total inpatient imaging case volumes stratified by time periods
| Time Periods | 2020 | 2019 | 2020 Percent Difference |
|---|---|---|---|
| Weeks 1-16 | 162,470 | 175,511 | −7.4 |
| Pre-COVID-19 (weeks 1-9) | 94,302 | 96,609 | −2.4 |
| Post-COVID-19 (weeks 10-16) | 68,168 | 78,902 | −13.6 |
| Early post-COVID-19 (weeks 10-13) | 37,732 | 45,221 | −16.6 |
| Late post-COVID-19 (weeks 14-16) | 30,436 | 33,681 | −9.6 |
| Week 16 | 10,546 | 11,003 | −4.2 |
COVID = coronavirus disease 2019.
Fig 1.
The 2020 and 2019 inpatient imaging case volume trends across weeks 1 to 16 including all imaging modality types (radiography, CT, MRI, ultrasound, interventional radiology, and nuclear medicine). The vertical red line at week 10 indicates when the first patient testing positive for coronavirus disease 2019 (COVID-19) was confirmed in New York City. The vertical black line at week 14 indicates the late post-COVID-19 (weeks 14-16) period. Calendar weeks are presented on the x axis and number of imaging examinations on the y axis.
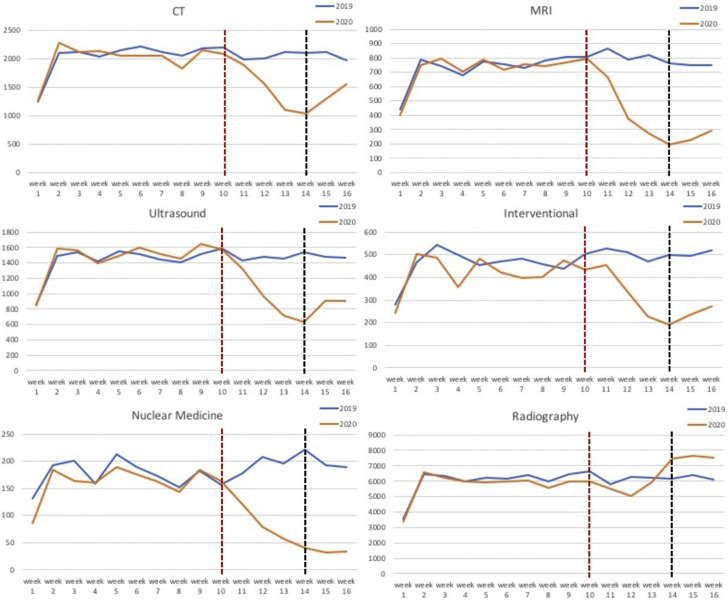
Table 2 compares the mean weekly imaging volumes according to modality types for the total weeks 1 to 16 in years 2020 and 2019. There was a statistically significant decline in the inpatient mean weekly imaging volumes for CT (−264.3, P = .035), MRI (−175.0, P = .012), interventional radiology (−106.4, P = .002), and nuclear medicine (−59.7, P = .001). Although the imaging volumes for radiography and ultrasound declined in 2020, it was not statistically significant. Figure 2 demonstrates the trends in the imaging volumes in years 2020 and 2019 across weeks 1 to 16 stratified by imaging modality types. In the early post-COVID-19 (weeks 10-13) period, the 2020 imaging case volumes declined across all modality types. In the late post-COVID-19 (weeks 14-16) period, increased inpatient imaging volumes are seen for all modality types, except nuclear medicine.
Table 2.
Comparison of the 2020 and 2019 inpatient mean weekly imaging case volumes for the total weeks 1-16 stratified by imaging modality types
| Imaging Modality | 2020, Mean (SD) | 2019, Mean (SD) | P Value |
|---|---|---|---|
| CT | 1,777.8 (414.3) | 2,042.1 (225.4) | .0349∗ |
| MRI | 577.9 (235.0) | 752.9 (94.1) | .0120∗ |
| Ultrasound | 1,257.6 (360.5) | 1,447.0 (164.5) | .0697 |
| Interventional | 369.9 (105.3) | 476.3 (58.9) | .0018∗ |
| Nuclear medicine | 123.9 (59.0) | 183.6 (24.1) | .0013∗ |
| Radiography | 6,047.3 (1,023.6) | 6,067.6 (704.7) | .9481 |
P < .05.
Fig 2.
The 2020 and 2019 inpatient imaging case volume trends across weeks 1 to 16 stratified by imaging modality types. The vertical red line at week 10 indicates when the first patient testing positive for coronavirus disease 2019 (COVID-19) was confirmed in New York City. The vertical black line at week 14 indicates the late post-COVID-19 (weeks 14-16) period. Calendar weeks are presented on the x axis and number of imaging examinations on the y axis.
Table 3 compares the mean weekly imaging volumes for the pre-COVID-19 (weeks 1-9) and post-COVID-19 (weeks 10-16) periods according to modality types in both 2020 and 2019 separately. In 2019, there was no statistically significant change in the inpatient imaging volumes by modality types in weeks 10 to 16 (post-COVID-19 group) compared with weeks 1 to 9 (pre-COVID-19 group). In 2020, there was a statistically significant decline in the imaging volumes during the post-COVID-19 (weeks 10-16) period for CT (−490.0, P = .013), MRI (−312.0, P = .004), ultrasound (−453.4, P = .007), interventional radiology (−110.6, P = .032), and nuclear medicine (−85.6, P = .001), compared with the pre-COVID-19 (weeks 1-9) period. However, radiography imaging volume increased (+711.9, P = .176) during the post-COVID-19 period but was not statistically significant.
Table 3.
Comparison of the inpatient mean weekly imaging case volumes for the pre-COVID-19 (weeks 1-9) and post-COVID-19 (weeks 10-16) periods in years 2020 and 2019 stratified by imaging modality types
| Imaging Modality | 2020 Weeks 1-9, Mean (SD) | 2020 Weeks 10-16, Mean (SD) | P Value | 2019 Weeks 1-9, Mean (SD) | 2019 Weeks 10-16, Mean (SD) | P Value |
|---|---|---|---|---|---|---|
| CT | 1,992.1 (297.0) | 1,502.1 (392.4) | .0129∗ | 2,019.8 (297.6) | 2,070.7 (85.0) | .6361 |
| MRI | 714.4 (121.4) | 402.4 (233.4) | .0037∗ | 722.0 (113.1) | 792.7 (42.4) | .1130 |
| Ultrasound | 1,456.0 (241.2) | 1,002.6 (335.2) | .0070∗ | 1,413.6 (213.6) | 1,490.0 (54.8) | .3286 |
| Interventional | 418.3 (81.5) | 307.7 (104.2) | .0316∗ | 455.4 (71.8) | 503.0 (17.8) | .0873 |
| Nuclear medicine | 161.3 (31.8) | 75.7 (50.3) | .0010∗ | 177.1 (157.2) | 191.9 (20.3) | .2371 |
| Radiography | 5,735.8 (926.6) | 6,447.7 (1,068.6) | .1755 | 5,946.4 (919.3) | 6,223.4 (254.1) | .4096 |
COVID = coronavirus disease 2019.
P < .05.
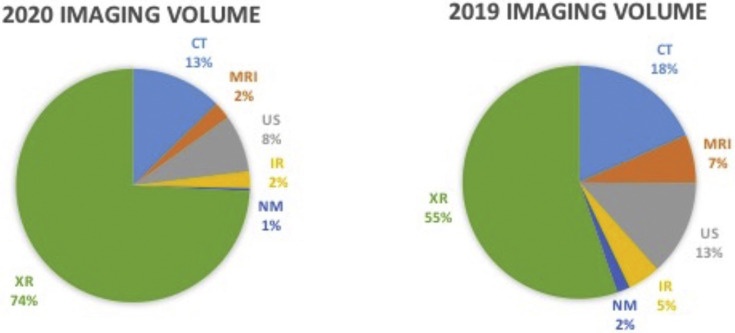
Table 4 compares the 2020 and 2019 mean weekly imaging volumes in the early post-COVID-19 (weeks 10-13) and late post-COVID-19 (weeks 14-16) periods stratified by the modality types. In the early post-COVID-19 period, the 2020 imaging volumes show a statistically significant decline compared with 2019 for only nuclear medicine (−79.0, P = .022). However, in the late post-COVID-19 period, the 2020 imaging volumes for all modality types had statistically significant declines, except for radiography (+1,328.7, P = .0002), which had a statistically significant increased imaging volume. Figure 3 compares the 2020 and 2019 composition mix of the inpatient imaging volumes by modality types for the late post-COVID-19 (weeks 14-16) period to further understand the shift in imaging utilization. There is a statistically significant change (P < .0001) in the composition mix of the 2020 imaging volumes during the late post-COVID-19 period largely comprised of radiography (74.3%), followed by CT (12.7%), ultrasound (8%), MRI (2.4%), interventional radiology (2.3%), and nuclear medicine (0.4%).
Table 4.
Comparison of the 2020 and 2019 inpatient mean weekly imaging case volumes for the early post-COVID-19 (weeks 10-13) and late post-COVID-19 (weeks 14-16) periods stratified by imaging modality types
| Imaging Modality | 2020 Weeks 10-13, Mean (SD) | 2019 Weeks 10-13, Mean (SD) | P Value | 2020 Weeks 14-16, Mean (SD) | 2019 Weeks 14-16, Mean (SD) | P Value |
|---|---|---|---|---|---|---|
| CT | 1,659.8 (431.0) | 2,075.3 (101.7) | .1480 | 1,292.0 (259.5) | 2,064.7 (77.9) | .0078∗ |
| MRI | 525.8 (245.0) | 821.3 (32.0) | .0937 | 238.0 (49.5) | 754.7 (8.1) | <.0001∗ |
| Ultrasound | 1,146.5 (379.2) | 1,485.8 (69.4) | .1708 | 810.7 (157.3) | 1,495.7 (41.2) | .0019∗ |
| Interventional | 364.3 (103.7) | 503.3 (22.7) | .0720 | 232.3 (39.1) | 502.7 (13.4) | .0003∗ |
| Nuclear medicine | 106.0 (46.9) | 185.0 (21.8) | .0224∗ | 35.3 (4.9) | 201.0 (17.3) | <.0001∗ |
| Radiography | 5,630.8 (445.0) | 6,234.8 (339.5) | .0743 | 7,537.0 (117.0) | 6,208.3 (142.4) | .0002∗ |
COVID = coronavirus disease 2019.
P < .05.
Fig 3.
The 2020 and 2019 inpatient imaging volume composition mix stratified by modality types during the late post-coronavirus disease 2019 (COVID-19; weeks 14-16) period. A statistically significant shift (P < .0001) in the 2020 imaging composition mix (n = 30,436) was observed compared with 2019 (n = 33,681). Specifically, the 2020 imaging volumes for CT, MRI, ultrasound (US), interventional radiology (IR), and nuclear medicine (NM) decreased compared with 2019. However, the 2020 imaging volume for radiography (XR) increased representing almost three-quarters of all imaging performed.
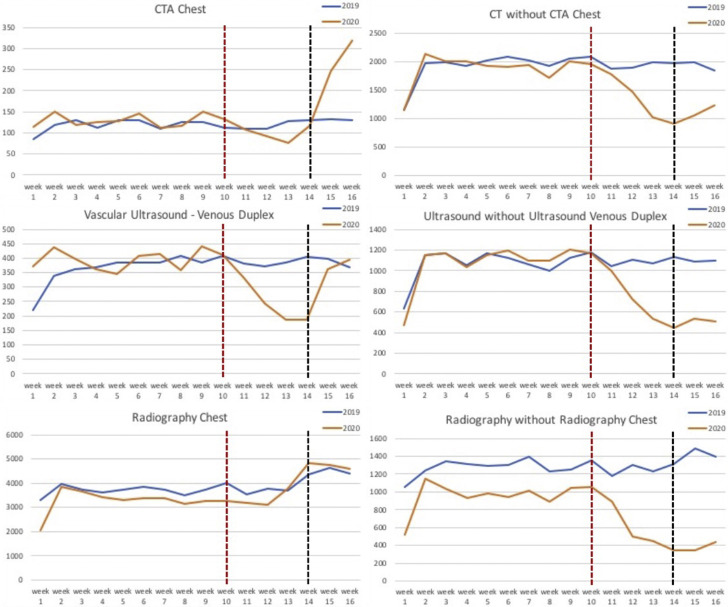
Table 5 compares the 2020 and 2019 mean weekly imaging volumes during the late post-COVID-19 (weeks 14-16) period for each modality type stratified by CPT-coded groups. There was a shift in the imaging volumes by specific imaging examinations. For example, within the CT modality type, all CPT-coded groups significantly declined (P < .05) in 2020 compared with 2019, except for CTA chest (+96.7, P = .176), which showed increased volume in 2020 (although not statistically significant). A similar pattern is seen in the radiography modality with increased volume for radiography chest (+267.3, P = .064) in the 2020 late post-COVID-19 period. Within the ultrasound modality, venous duplex (−75.6, P = .315) declined in the 2020 late post-COVID-19 period compared with 2019; however, this was not statistically significant. Ultrasound head (+5.3, P = .592), ultrasound chest (−4.7, P = .124), MRI cardiac (−3.3, P = .100), and MR angiography abdomen or pelvis (−1.7, P = .279) were not statistically changed in the late post-COVID-19 period, likely because of the small sample size in each group. Figure 4 shows the 2020 and 2019 imaging case volume trends across weeks 1 to 16 for CTA chest, ultrasound venous duplex, and radiography chest, demonstrating the increased imaging volumes in the 2020 late post-COVID-19 (weeks 14-16) period compared with the early post-COVID-19 (weeks 10-13) period.
Table 5.
Comparison of the 2020 and 2019 inpatient mean weekly imaging case volumes for the late post-COVID-19 (weeks 14-16) period stratified by CPT-coded groups
| Imaging Modality CPT-Coded Groups | 2020 |
2019 |
P Value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| CT | |||||
| Head | 393.3 | 64.9 | 552.7 | 25.0 | .0375∗ |
| Orbit, face, or neck | 11.7 | 4.9 | 34.7 | 9.1 | .0293∗ |
| Spine | 36.7 | 8.1 | 73.7 | 8.1 | .0050∗ |
| Extremities | 26.6 | 4.2 | 68.3 | 9.3 | .0075∗ |
| Abdomen or pelvis | 228.7 | 48.0 | 471.3 | 24.4 | .0045∗ |
| Chest | 195.3 | 11.1 | 395.0 | 17.7 | .0002∗ |
| Head or neck | 51.0 | 16.1 | 83.3 | 9.2 | .0392∗ |
| Chest | 227.0 | 101.8 | 130.3 | 2.3 | .1756 |
| Abdomen or pelvis | 18.7 | 3.8 | 40.0 | 8.7 | .0357∗ |
| Cardiac | 4.3 | 3.2 | 18.7 | 5.7 | .0292∗ |
| MRI | |||||
| Brain | 111.0 | 24.2 | 300.3 | 8.6 | .0025∗ |
| Spine | 42.7 | 16.8 | 154.3 | 6.8 | .0030∗ |
| Abdomen or pelvis | 23.7 | 2.3 | 81.0 | 4.4 | .0002∗ |
| Extremities | 10.0 | 2.6 | 59.7 | 6.7 | .0023∗ |
| Cardiac | 1.7 | 0.6 | 5.0 | 2.6 | .1000 |
| Head | 15.0 | 3.6 | 63.0 | 5.6 | .0006∗ |
| Neck | 7.0 | 1.7 | 40.7 | 5.8 | .0060∗ |
| Abdomen or pelvis | 1.3 | 1.2 | 3.0 | 2.0 | .2794 |
| Ultrasound | |||||
| Neck | 3.7 | 1.5 | 18.3 | 2.5 | .0023∗ |
| Pelvis | 14.3 | 1.2 | 42.7 | 9.9 | .0366∗ |
| Head | 41.3 | 15.3 | 36.0 | 4.4 | .5921 |
| Chest | 2.0 | 2.6 | 6.7 | 3.2 | .1242 |
| Abdomen | 257.0 | 29.5 | 537.7 | 15.5 | .0007∗ |
| Obstetrics | 6.0 | 2.0 | 16.7 | 2.1 | .0031∗ |
| Extremities | 4.0 | 2.6 | 16.7 | 3.1 | .0059∗ |
| Spine | 4.7 | 0.6 | 3.3 | 0.6 | .0474∗ |
| Vascular (arterial) | 33.0 | 9.6 | 177.3 | 5.0 | <.0001∗ |
| Venous duplex | 314.7 | 112.6 | 390.3 | 19.7 | .3154 |
| Interventional | 268.3 | 57.5 | 509.0 | 40.3 | .0057∗ |
| Nuclear medicine | |||||
| Pulmonary | 9.0 | 2.6 | 28.7 | 3.1 | .0012∗ |
| Other | 18.0 | 3.6 | 105.0 | 20.0 | .0148∗ |
| Radiography | |||||
| Chest | 4,726.0 | 113.2 | 4,458.7 | 142.4 | .0636 |
| Spine | 9.0 | 8.2 | 77.0 | 10.1 | .0010∗ |
| Other bones | 148.3 | 19.6 | 689.0 | 72.3 | .0037∗ |
| Abdomen | 202.0 | 21.0 | 480.3 | 24.6 | .0001∗ |
| Head or neck | 1.0 | 0 | 6.0 | 1.7 | .0377∗ |
| Fluoroscopy | 12.3 | 3.2 | 149.7 | 19.6 | .0056∗ |
COVID = coronavirus disease 2019; CPT = Current Procedural Terminology.
P < .05.
Fig 4.
The 2020 and 2019 inpatient imaging case volume trends across weeks 1 to 16 for CT angiography (CTA) chest, ultrasound venous duplex, radiography chest (left column). The trend data for the respective imaging modality type including all other Current Procedural Terminology codes are displayed for comparison (right column). The vertical red line at week 10 indicates when the first patient testing positive for coronavirus disease 2019 (COVID-19) was confirmed in New York City. The vertical black line at week 14 indicates the late post-COVID-19 (weeks 14-16) period. Calendar weeks are presented on the x axis and number of imaging examinations on the y axis.
Discussion
In a short time, the COVID-19 pandemic has had a substantial economic impact on health care institutions. Many radiology practices experienced a rapid decline in imaging case volumes [3,4] as a consequence of public policy, financial hardship, and patient fear. In particular, outpatient imaging was expected to have the greatest decline in imaging volumes across all modality types [4]. Even though inpatient imaging was less affected by the declines in imaging volume during the post-COVID-19 (weeks 10-16) period, it is important to be aware that there was a significant shift in the composition mix of the imaging modality types and specific CPT-coded examinations.
The results from this study revealed an overall 13.6% decline in the total imaging volume in the inpatient setting over the first 7-week period during the COVID-19 pandemic, compared with 2019, including all imaging modality types. For further analysis of the post-COVID-19 (weeks 10-16) period, the data set was split to represent the early post-COVID-19 (weeks 10-13) and late post-COVID-19 (weeks 14-16) periods. There was a greater decline of 16.6% in the total inpatient imaging volume during the early post-COVID-19 period immediately after the first patient testing positive for COVID-19 was confirmed in New York City (week 10, day 1). This may be partly explained by the preemptive response to lower the overall inpatient census by delaying elective procedures to increase capacity for the expected influx of patients with COVID-19. However, the inpatient imaging volume increased in the late post-COVID-19 (weeks 14-16) period, resulting in only a 9.6% decline in year-over-year imaging volume, likely due to the surge of patients with COVID-19 requiring hospitalization. By week 16, the inpatient imaging volume was down only 4.2% compared with the same period in 2019.
Despite the relatively modest level of inpatient imaging volume decline compared with the outpatient and emergency settings [4], this study revealed that the 2020 imaging volume composition mix changed significantly (P < .0001) during the COVID-19 pandemic. A significant shift in the imaging modality types was observed in the 2020 late post-COVID-19 (weeks 14-16) period with the greatest percentage comprised of radiography (74.3%), followed in descending order by CT (12.7%), ultrasound (8.0%), MRI (2.4%), interventional radiology (2.3%), and nuclear medicine (0.4%). This may be partly explained by the departmental guidelines recommending judicious use of cross-sectional imaging, ultrasound, and interventional radiology to prevent spread of COVID-19 disease to patients and health care providers.
When we further examined the specific CPT-coded groups within imaging modality types during the 2020 late post-COVID-19 (weeks 14-16) period, we found that the mean weekly imaging volumes statistically declined for all CPT-coded groups in CT and radiography modality types, except for CTA chest and radiography chest, compared with 2019. The imaging volumes actually increased for CTA chest and radiography chest in the late post-COVID-19 period, although this change was not statistically significant. In addition, the 2020 trend data revealed an increase in the imaging volumes in the late post-COVID-19 (weeks 14-16) period for CTA chest, radiography chest, and ultrasound venous duplex, relative to the early post-COVID-19 (weeks 10-13) period. From the growing literature in this area, we are now aware that changes in the prothrombotic factors occur in severe COVID-19 infection inducing a hypercoagulable state [5,6]. These patients have been reported with elevated d-dimer, fibrinogen, and factor VIII [5,6], with marked increased frequency of venous thromboembolism and pulmonary embolism seen in up to one-third of patients with COVID-19 in the intensive care unit [7,8]. The imaging workup for the diagnosis of these clinical manifestations includes radiography chest, CTA chest, and ultrasound venous duplex, likely explaining the shift in the imaging composition mix observed in this study.
To our knowledge, no prior publications have evaluated the change in the inpatient imaging volumes and composition mix during the COVID-19 pandemic stratified by imaging modality types and CPT-coded groups. The results from this study may have significant implications for leaders preparing for a potential resurgence of the COVID-19 crisis. These real-world data should be useful in preparing for potential resource utilization and staffing requirements. In particular, these results may be helpful in developing new imaging utilization guidelines and departmental policies aimed at optimally accommodating the unique imaging needs for patients with COVID-19. Radiology practices can plan in advance for adequate staffing, as well as develop safe and efficient decontamination procedures in specific imaging modalities (radiography, ultrasound, and CT). Additionally, radiologists with clinical expertise for the specific CPT-coded imaging examinations (radiography chest, CTA chest, and ultrasound venous duplex) will be valuable in providing high-quality care.
The main limitations of this study are similar to our prior work [4] using a retrospective study design analyzing aggregated and anonymized data. However, this study provided more detailed analyses of individual CPT-coded groups within each modality type. Within the ultrasound modality, point-of-care ultrasound was excluded in the aggregated volume data. Although another limitation affecting the generalizability of these findings is that our health care system is located in the epicenter of the COVID-19 pandemic [4], these results may be helpful in establishing a worst-case scenario. Further studies evaluating the inpatient imaging volumes and composition mix in radiology practices located outside the epicenter would also be a valuable addition to the literature.
In summary, the results from this study provide real-world data to inform radiology practices regarding not only the decline in inpatient imaging volumes but more importantly the significant shift in the imaging composition mix during the COVID-19 pandemic. This study may assist in guiding inpatient practice decisions based on the shift in the imaging volumes across different modality types and specific CPT-coded groups to provide optimal access and availability of the imaging resources necessary during the COVID-19 pandemic.
Take-Home Points
-
▪
This study revealed an overall 13.6% decline in the inpatient imaging volume during the COVID-19 pandemic (7 weeks) including all imaging modality types.
-
▪
Imaging volume deterioration varied in the post-COVID-19 (weeks 10-16) period with the greatest decline (16.6%) observed in the early post-COVID-19 (weeks 10-13) period. Inpatient imaging volume started to increase in the late post-COVID-19 (weeks 14-16) period. By week 16, the inpatient imaging volume only declined by 4.2%.
-
▪
A statistically significant shift in the 2020 imaging volume composition mix was observed in the late post-COVID-19 (weeks 14-16) period, largely comprised of radiography (74.3%), followed by CT (12.7%), ultrasound (8%), MRI (2.4%), interventional radiology (2.3%), and nuclear medicine (0.4%).
-
▪
The trend data revealed increased imaging volumes for specific CPT-coded groups in the late post-COVID-19 (weeks 14-16) period for CTA chest, radiography chest, and ultrasound venous duplex.
-
▪
These data may be useful to radiology practices in preparing for the possibility of a second wave of the COVID-19 pandemic.
Acknowledgments
Funding support was received from the Harvey L. Neiman Health Policy Institute through a research partnership. We acknowledge Frank Rizzo, Morgan O’Hare, and Chen (Shirley) Liu from the finance department at our institution for contributing the aggregated data used in the analyses in this study. We acknowledge the Northwell Health COVID-19 Research Consortium.
Footnotes
Dr Boltyenkov is a shareholder of Siemens Healthineers. Dr Hughes reports grants from Harvey L. Neiman Health Policy Institute, outside the submitted work. Dr Sanelli reports grants from Harvey L. Neiman Health Policy Institute, during the conduct of the study, and grants and nonfinancial support from Siemens Healthineers, Inc, outside the submitted work. The other authors state that they have no conflict of interest related to the material discussed in this article. Dr Naidich, Dr Boltyenkov, Dr Wang, Dr Chusid, Dr Hughes, and Dr Sanelli are non-partnership track employees.
Additional Resources
Additional resources can be found online at: https://doi.org/10.1016/j.jacr.2020.06.011.
Additional Resources
References
- 1.Worldometer United States. https://www.worldometers.info/coronavirus/country/us/ Available at: Updated June 2, 2020. Accessed June 2, 2020.
- 2.ACR ACR COVID-19 clinical resources for radiologists. https://www.acr.org/Clinical-Resources/COVID-19-Radiology-Resources Available at: Updated April 28, 2020. Accessed May 3, 2020.
- 3.Cavallo J.J., Forman H.P. The economic impact of the COVID-19 pandemic on radiology practices [E-pub ahead of print] Radiology. 2020:201495. doi: 10.1148/radiol.2020201495. PubMed PMID: 32293225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naidich J.J., Boltyenkov A., Wang J.J., Chusid J., Hughes D., Sanelli P.C. Impact of the COVID-19 pandemic on imaging case volumes [E-pub ahead of print] J Am Coll Radiol. 2020 doi: 10.1016/j.jacr.2020.05.004. PubMed PMID: 32425710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Panigada M., Bottino N., Tagliabue P. Hypercoagulability of COVID-19 patients in intensive care unit. A report of thromboelastography findings and other parameters of hemostasis [E-pub ahead of print] J Thromb Haemost. 2020 doi: 10.1111/jth.14850. PubMed PMID: 32302438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ranucci M., Ballotta A., Di Dedda U. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome [E-pub ahead of print] J Thromb Haemost. 2020 doi: 10.1111/jth.14854. PubMed PMID: 32302448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Menter T., Haslbauer J.D., Nienhold R. Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction [E-pub ahead of print] Histopathology. 2020 doi: 10.1111/his.14134. PubMed PMID: 32364264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wichmann D., Sperhake J.P., Lütgehetmann M. Autopsy findings and venous thromboembolism in patients with COVID-19 [E-pub ahead of print] Ann Intern Med. 2020:M20–M2003. doi: 10.7326/M20-2003. PubMed PMID: 32374815. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.