Abstract
Massive rotator cuff tears involving the posterosuperior rotator cuff remain difficult to treat, particularly in the younger population. Fatty infiltration of the muscle, excessive chronic tendon retraction, and degeneration are the main irreversible factors predisposing to high failure rates of direct repair. Many techniques exist for superior capsular reconstruction (SCR), mainly using allograft. However, the higher costs of dermal grafts and morbidity of fascia lata autograft led us to find another option for SCR of the shoulder using the semitendinosus autograft as a pivot in a better biomechanical configuration. The pivot SCR technique has shown good functional and biomechanical results. We have found this technique to be a reliable and less expensive option for irreparable lesions of the rotator cuff.
Massive rotator cuff tears involving the posterosuperior rotator cuff remain difficult to treat, particularly in the younger population. The term “irreparable” has been used with different meanings in the past. For example, the term was frequently used when partial repair of the rotator cuff was performed.1 More recently, a subtle change in meaning was adopted. The term “irreparable” began to be used to describe a rotator cuff that was either predicted to be irreparable based on preoperative characteristics or predicted to have a poor outcome after rotator cuff surgery, regardless of the possibility of achieving current intraoperative repair.2 Fatty infiltration of the muscle, excessive chronic tendon retraction, and degeneration are the main irreversible factors predisposing to high failure rates of direct repair. Some authors have stated that the term “irreparable” should only be applied intraoperatively.1
Superior capsular reconstruction (SCR) was described as a revision operation in a paraplegic patient with an irreparable supraspinatus tendon tear.1,3 During cadaveric studies of patch graft surgery for irreparable rotator cuff tears, one group of authors realized that the graft should be attached medially to the superior glenoid and laterally to the greater tuberosity to improve superior stability of the humeral head in SCR.4 This modification resulted in significant improvements in pain, function, and range of motion in forward flexion and abduction, besides the increase in the subacromial space on the roentgenograms.5 Although reported outcomes were favorable, it is important to note that this technique increases surgical time and carries donor-site morbidity.
Other authors proposed the use of dermal allograft for SCR as opposed to fascia lata.6,7 However, surgical costs remained complex to manage for this procedure, creating a gap for other surgical options.8, 9, 10, 11 This Technical Note aims to present a less expensive technique that uses the semitendinosus graft as a central pivot in a better dynamic configuration for SCR (Video 1).
Surgical Technique
The patient is placed in the beach-chair position under general anesthesia. The semitendinosus tendon is extracted as standardized for anterior cruciate ligament (ACL) reconstruction. The tendon is tensioned and overlapped once in a double-band configuration. Suturing on the final portions of the overlapped graft is performed with No. 5 multifilament polyester suture. This multifilament polyester suture is inserted in a perforated Kirschner wire as used in ACL reconstruction.
The scope is inserted in the posterior portal; an extensive bursectomy is performed, and the lesion can be visualized. The scope is then placed in the lateral portal. Extensive exposure of the scapular neck is performed using a shaver and electrocautery device, with removal of tissue inferior to the supraglenoid tubercle anterior and posterior, to enable easy identification of the bone of the scapular neck, where the graft will pass from posterior to anterior. The labrum is kept intact.
An 18-gauge needle is used to establish the posteromedial portal, which faces the scapular neck just under the glenoid tuberosity. A guide K-wire is inserted through the posteromedial portal and crosses from the posterior (at the 10-o’clock position in the glenoid) to anterior (at the 2- to 3-o’clock position in the glenoid) glenoid neck (Fig 1). A drill the same size as the overlapped semitendinosus tendon is used to create a hole (Fig 2). The perforated K-wire is used to pass the No. 5.0 multifilament polyester suture in 1 final portion of the overlapped graft. Two marks measuring 2 cm are made on each side of the graft to ensure a minimal length on each side. The 2 marks should be visualized by the scope after graft passage. The multifilament polyester suture is pulled through the anterior portal, and the tendon is passed from the posterior to anterior glenoid neck through this hole (Fig 3). With the aid of an atraumatic clamp, both graft legs are placed within the joint, anteriorly in the subcoracoid space and posteriorly in the supraspinatus fossa, exposing the graft terminal fixation and No. 5.0 multifilament polyester suture.
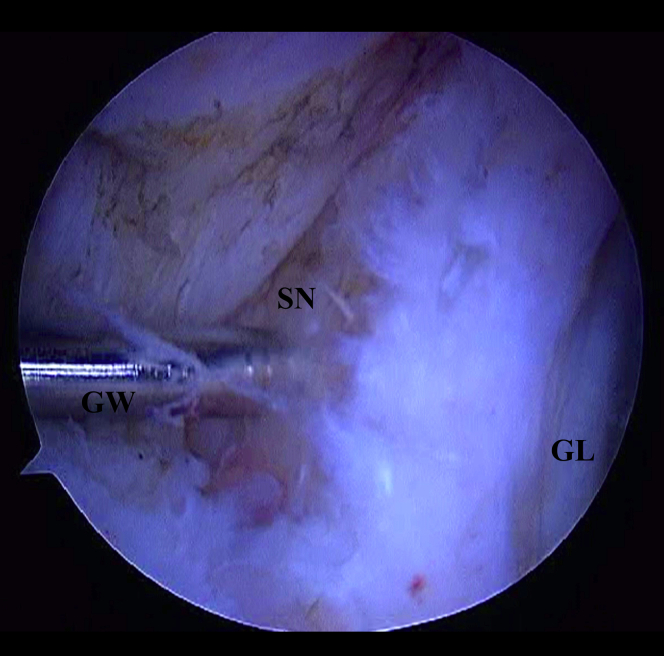
Fig 1.
Right shoulder, posterior visualization with scope through lateral portal. The guidewire (GW) is inserted in the scapular neck (SN) from posterior to anterior. (GL, glenoid.)
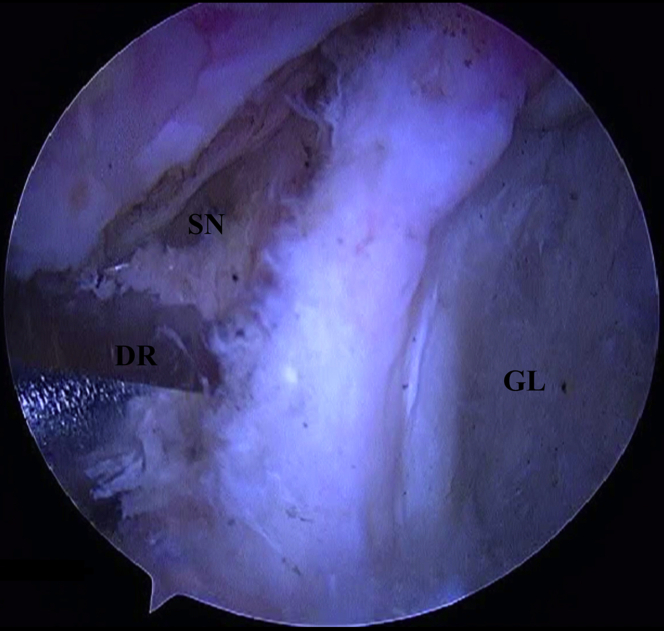
Fig 2.
Right shoulder, posterior visualization with scope through the lateral portal. A drill is used to create a hole. (DR, drill; GL, glenoid; SN, scapular neck.)
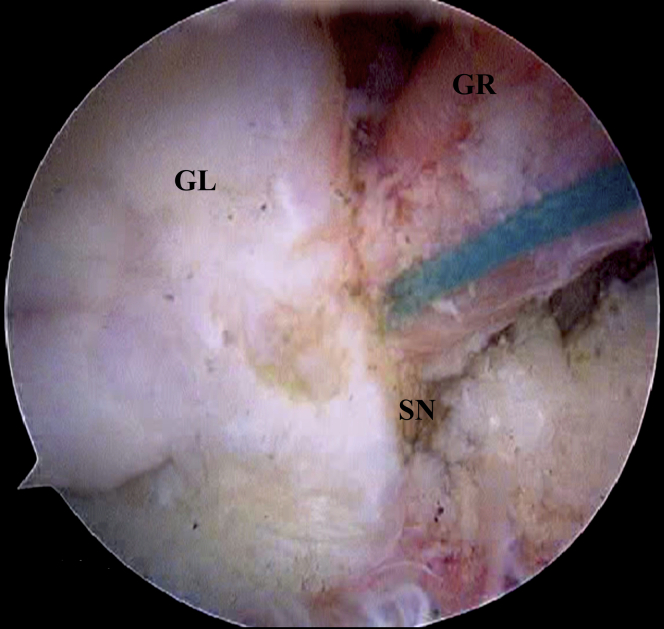
Fig 3.
Right shoulder, anterior visualization with scope through lateral portal. The semitendinosus graft (GR) is passed from posterior to anterior. (GL, glenoid; SN, scapular neck.)
A Neviaser portal is made, and a guide K-wire is inserted approximately 1 cm from the medial border of the greater tuberosity on the humeral head until it crosses the lateral humeral cortex; the arm can be abducted to achieve the best position (Fig 4). A drill that is 1 size higher than the double-overlapped tendon’s size is inserted until it touches the contralateral humeral cortex, not crossing it (Fig 5). The anterior and posterior overlapped graft portions are pulled out of the body through the Neviaser portal. The No. 5.0 multifilament polyester suture in the tips of the graft is inserted in the perforated K-wire and is used to pass the graft through the hole in the humeral head (Fig 6). Tensioning of the tendons is performed similarly to that in ACL reconstruction, and fixation is performed with a metallic interference screw (Hexagon, Itapira, Brazil) (Fig 7). The size of the screw is the same as that of the hole.
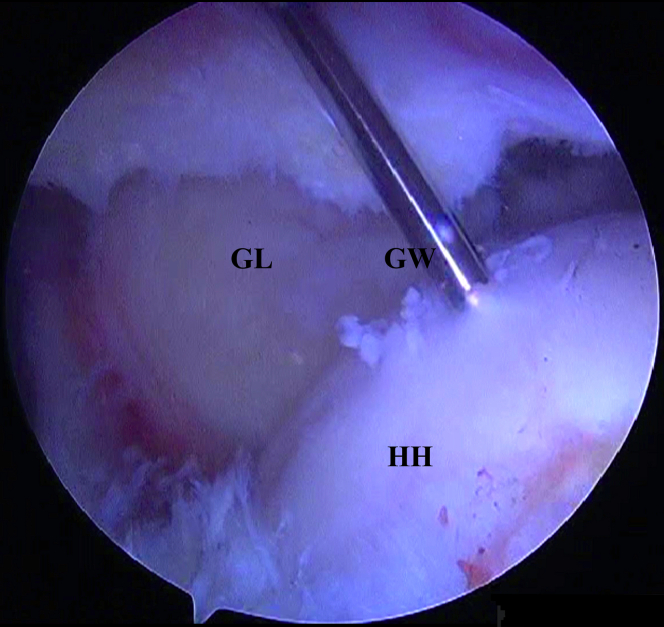
Fig 4.
Right shoulder. With the scope through the lateral portal, the guidewire (GW) is inserted through the Neviaser portal in the humeral head (HH). (GL, glenoid.)
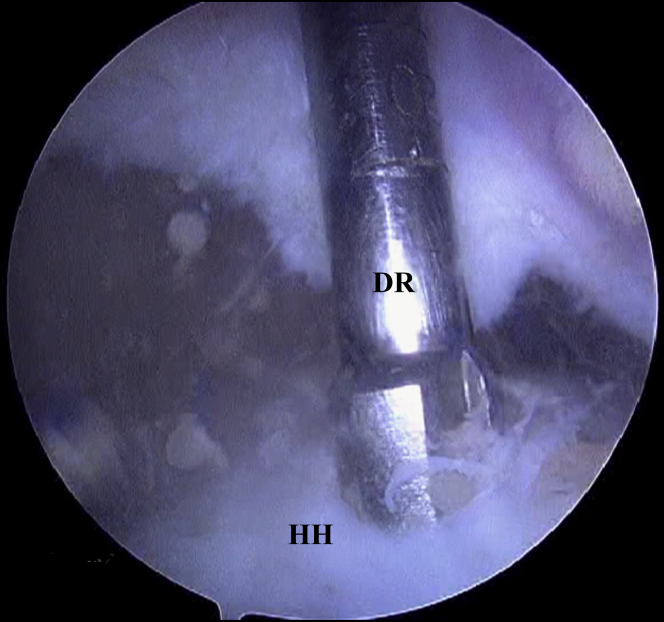
Fig 5.
Right shoulder. With the scope through the lateral portal, the drill (DR) is inserted through the Neviaser portal in the humeral head (HH).
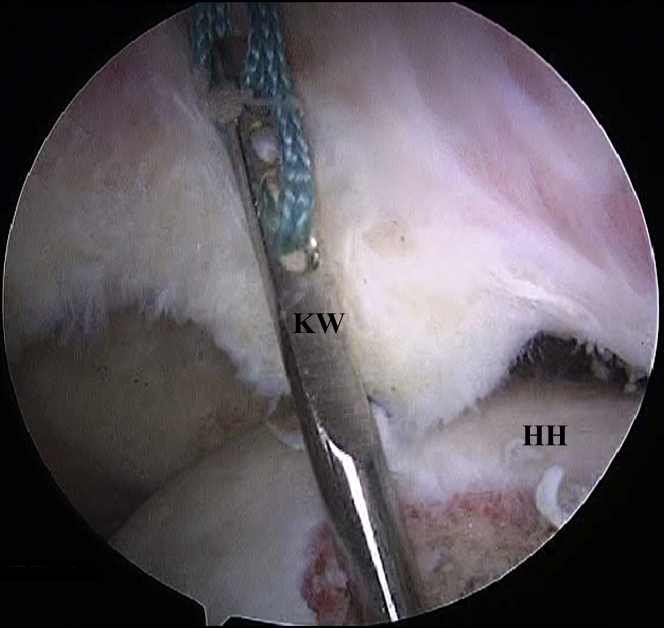
Fig 6.
Right shoulder, visualization with scope through the lateral portal. The perforated Kirschner wire (KW) is passed through the humerus to insert the graft in the same manner as in anterior cruciate ligament reconstruction through the Neviaser portal in the humeral head (HH).
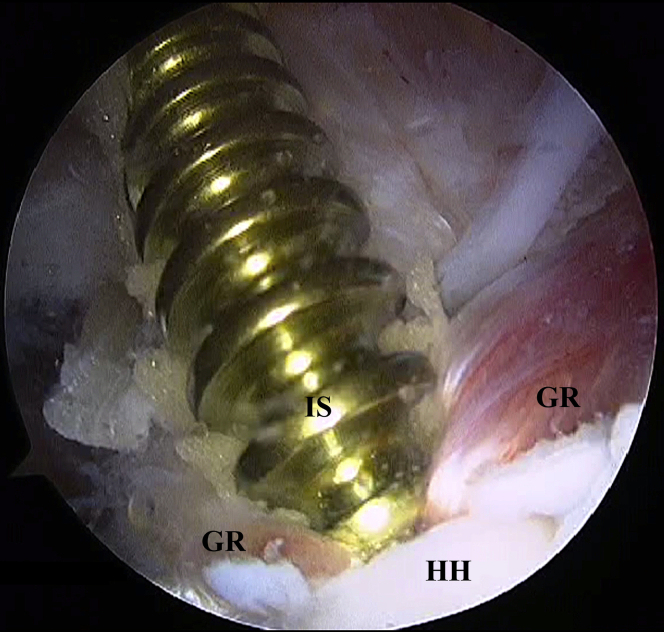
Fig 7.
Right shoulder, visualization with scope through the lateral portal. The interference screw (IS) is inserted to fix the graft (GR) in the humeral head (HH) through the Neviaser portal.
If the surgeon prefers stronger fixation, an EndoButton (Razek, São Carlos, Brazil) can be inserted through the humeral head hole before graft insertion and can be used to pass and fix the graft. A release of the teres minor and infraspinatus should be performed to cover as much area as possible during the repair. The greater tuberosity is free for partial cuff repair or any tendon transfer. Repairable partial and/or full infraspinatus and subscapularis tendon tears must be reconstructed to ensure the restoration of the stabilizing forces in the transverse plane.8
Postoperative radiographs will be useful to see the screw and subacromial space (Fig 8). Without a functional subscapularis or its suture, the reconstruction may fail. Accessory portals—anterior and posterolateral—should be used when necessary. Pearls and pitfalls of our technique are summarized in Table 1. Advantages and disadvantages are summarized in Table 2.
Fig 8.
Postsurgical anteroposterior shoulder roentgenogram.
Table 1.
Pearls and Pitfalls
| Pearls and Pitfalls | |
|---|---|
| Semitendinosus graft | The graft needs to be large enough to suitably pass through the scapular neck and allow fixation on the humeral head. |
| Scapular neck perforation | This is the most important step of the described technique. A minimal distance of 7-8 mm is required to avoid articular damage and fracture. |
| Cleaning of space | Suitable cleaning of the shoulder is needed to allow appropriate visualization of the entire articulation, as well as the scapular neck. Cleaning of the anterior exit point area needs to be highlighted to confirm its correct location and to preserve the subscapularis. |
| Humeral perforation | The location is 1 cm from the footprint, within the cartilage of the humeral head nearest the central line perpendicular to the middle of the footprint. |
| Direction | The direction of the perforation needs to be as anterior or anterolateral as possible to avoid the neurologic structures of the arm. |
Table 2.
Advantages and Disadvantages Comparing Pivot SCR and Traditional SCR
| Pivot SCR | Traditional SCR | |
|---|---|---|
| Graft | Semitendinosus: autograft or allograft | Fascia lata: autograft or allograft, dermal allograft, or xenograft |
| Fixation | 1 interference screw | 5-7 suture anchors |
| Price | + | +++ |
| Duration | ++ | +++ |
| Graft stress in internal and/or external rotation | + | +++ |
| Possible association with transfers | Preserves humeral footprint to insert transferred tendons | Does not preserve humeral footprint to insert transferred tendons |
NOTE. + = low; ++ = medium; +++ = high.
SCR, superior capsular reconstruction.
Postoperative Protocol
We recommend the use of an abduction pillow for 4 weeks after reconstruction surgery. After the immobilization period, passive and active-assisted exercises begin. Eight weeks after surgery, patients can start rotator cuff and scapular stabilization exercises. More than 10 patients have undergone the described procedure, and their results were better than those of traditional SCR in our hands.
Discussion
Despite growing interest in the use of SCR using dermal allograft technology, its cost is a potential impediment.8 It is important to note that other techniques using the long head of the biceps tendon as autologous graft, with partial repair of the rotator cuff or side-by-side suturing, have been described and cited by several authors as options over traditional SCR.8, 9, 10, 11, 12 We suggest that our surgical procedure using the semitendinosus tendon is easier and presents low costs and good outcomes. This double-overlapped graft measures at least 8 mm in diameter, which is the diameter related to the best results after ACL reconstruction.13,14
Reconstructions of other articulations use the graft insertion as close as possible to the rotational center in the least restrictive manner possible. In our technique, the surgeon inserts the semitendinosus graft in a single pivot configuration nearer the rotational center of the humerus, considering its axial plane. Regarding fixation, double fixation using an EndoButton and interference screw seems to ensure strength enough to stabilize the system until the entire healing process is complete.
A scapular neck fracture is possible; however, in our experience, this will not occur if the exit hole is located at a safe distance from the glenoid. A humeral head fracture is also a hypothetical possibility. Finally, one important consideration is that the exit point needs to be at the 2- to 3-o’clock position; an inferior exit point can put the brachial plexus at risk.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.C.G. is a Latin America consultant for Zimmer-Biomet and a consultant for Razek, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
After bursectomy, the scapular neck is exposed by use of the lateral portal (visualization is performed with optics in the lateral portal, and exposure is performed with electrocautery and a soft-tissue shaver). The region medial to the 10-o’clock position in the glenoid needs to be exposed until the bone is visible (with the scope through the lateral portal). A K-wire is inserted in this region and leaves the bone at the 2- to 3-o’clock position. If the surgeon considers the amount of bone sufficient, he or she can drill the scapular neck. The size of the drill is the same as that of the double-overlapped graft. A perforated K-wire inserts the polyester wires of the graft through the scapular neck, similarly to anterior cruciate ligament reconstruction. The polyester is pulled out through the anterior portal, and the graft passes from posterior to anterior through the bone tunnel. The final portions of the graft are pulled out of the bone through the Neviaser portal. Through this portal, a guide K-wire and a drill are inserted 1 cm medial to the tuberosity, in the humeral head cartilage. The size of the drill is the same as that of the double-overlapped semitendinosus graft. A perforated K-wire inserts the guide polyester suture through this hole in the humeral head. The anterior and posterior parts of the graft are inserted within the humeral head. An interference screw presenting the same diameter as the hole is inserted, and the reconstruction is completed.
References
- 1.Hartzler R.U., Burkhart S.S. Superior capsular reconstruction. Orthopedics. 2017;40:271–280. doi: 10.3928/01477447-20170920-02. [DOI] [PubMed] [Google Scholar]
- 2.Ek E.T., Neukom L., Catanzaro S., Gerber C. Reverse total shoulder arthroplasty for massive irreparable rotator cuff tears in patients younger than 65 years old: Results after five to fifteen years. J Shoulder Elbow Surg. 2013;22:1199–1208. doi: 10.1016/j.jse.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 3.Hanada K., Fukuda H., Hamada K., Nakajima T. Rotator cuff tears in the patient with paraplegia. J Shoulder Elbow Surg. 1993;2:64–69. doi: 10.1016/1058-2746(93)90002-X. [DOI] [PubMed] [Google Scholar]
- 4.Mihata T., McGarry M., Pirolo J., Lee M. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am J Sports Med. 2012;40:2248–2255. doi: 10.1177/0363546512456195. [DOI] [PubMed] [Google Scholar]
- 5.Mihata T., Lee T.Q., Watanabe C. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 6.Hirahara A.M., Adams C.R. Arthroscopic superior capsular reconstruction for treatment of massive irreparable rotator cuff tears. Arthrosc Tech. 2015;4:e637–e641. doi: 10.1016/j.eats.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Denard P.J., Brady P.C., Adams C.R., Tokish J.M., Burkhart S.S. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy. 2018;34:93–99. doi: 10.1016/j.arthro.2017.08.265. [DOI] [PubMed] [Google Scholar]
- 8.Boutsiadis A., Chen S., Jiang C., Lenoir H., Delsol P., Barth J. Long head of the biceps as a suitable available local tissue autograft for superior capsular reconstruction: “The Chinese way”. Arthrosc Tech. 2017;6:e1559–e1566. doi: 10.1016/j.eats.2017.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hermanowicz K., Góralczyk A., Malinowski K., Jancewicz P., Domzalski M. Long head biceps tendon natural patch for massive irreparable rotator cuff tears. Arthrosc Tech. 2018;7:e473–e478. doi: 10.1016/j.eats.2017.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chillemi C., Mantovani M., Gigante A. Superior capsular reconstruction of the shoulder: The ABC (Arthroscopic Biceps Chillemi) technique. Eur J Orthop Surg Traumatol. 2018;28:1215–1223. doi: 10.1007/s00590-018-2183-1. [DOI] [PubMed] [Google Scholar]
- 11.Kim Y.S., Lee H.J., Park I., Sung G.Y., Kim D.J., Kim J.H. Arthroscopic in situ superior capsular reconstruction using the long head of the biceps tendon. Arthrosc Tech. 2018;7:e97–e103. doi: 10.1016/j.eats.2017.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garcia J.C., Jr., Barcelos M.R., Amaral F.M., Raffaelli M.P., Cardoso A.M., Jr. Principles of the superior capsule reconstruction of the shoulder. Int J Orthop. 2019;6:1012–1015. [Google Scholar]
- 13.Magnussen R.A., Lawrence J.T., West R.L. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28:526–531. doi: 10.1016/j.arthro.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 14.Figueroa F., Figueroa D., Espregueira-Mendes J. Hamstring autograft size importance in anterior cruciate ligament repair surgery. EFORT Open Rev. 2018;3:93–97. doi: 10.1302/2058-5241.3.170038. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
After bursectomy, the scapular neck is exposed by use of the lateral portal (visualization is performed with optics in the lateral portal, and exposure is performed with electrocautery and a soft-tissue shaver). The region medial to the 10-o’clock position in the glenoid needs to be exposed until the bone is visible (with the scope through the lateral portal). A K-wire is inserted in this region and leaves the bone at the 2- to 3-o’clock position. If the surgeon considers the amount of bone sufficient, he or she can drill the scapular neck. The size of the drill is the same as that of the double-overlapped graft. A perforated K-wire inserts the polyester wires of the graft through the scapular neck, similarly to anterior cruciate ligament reconstruction. The polyester is pulled out through the anterior portal, and the graft passes from posterior to anterior through the bone tunnel. The final portions of the graft are pulled out of the bone through the Neviaser portal. Through this portal, a guide K-wire and a drill are inserted 1 cm medial to the tuberosity, in the humeral head cartilage. The size of the drill is the same as that of the double-overlapped semitendinosus graft. A perforated K-wire inserts the guide polyester suture through this hole in the humeral head. The anterior and posterior parts of the graft are inserted within the humeral head. An interference screw presenting the same diameter as the hole is inserted, and the reconstruction is completed.