Abstract
Background
The recently published COMPLETE trial has demonstrated that patients with ST-segment elevation myocardial infarction (STEMI) and multivessel coronary artery disease (MVD), who underwent successful percutaneous coronary intervention (PCI) of both culprit and non-culprit (vs. culprit-only) lesions had a reduced risk of major adverse cardiac events (MACE), but not of cardiovascular or total mortality. The aim of this meta-analysis was to assess the efficacy of complete revascularization on cardiovascular or total mortality reduction using available randomized controlled trials (RCTs) including the COMPLETE trial, in hemodynamically stable STEMI patients with MVD.
Methods
PubMed, MEDLINE, Embase, Scopus, Google Scholar, CENTRAL and ClinicalTrials.gov databases search identified 10 RCTs of 7033 patients with STEMI and MVD which compared complete (n = 3420) vs. only culprit lesion (n = 3613) PCI for a median 27.7 months follow-up. Random effect risk ratios were used to estimate for efficacy and safety outcomes.
Results
Complete revascularization reduced the risk of MACE (10.4% vs.16.6%; RR = 0.59, 95% CI: 0.47 to 0.74, p < 0.0001), CV mortality (2.87% vs. 3.72%; RR = 0.73, 95% CI: 0.56 to 0.95, p = 0.02), reinfarction (5.1% vs. 7.1%; RR = 0.67, 95% CI: 0.52 to 0.86, p = 0.002), urgent revascularization (7.92% vs.17.4%; RR = 0.47, 95% CI: 0.30 to 0.73, p < 0.001), and CV hospitalization (8.68% vs.11.4%; RR = 0.65, 95% CI: 0.44to 0.96, p = 0.03) compared with culprit only revascularization. All-cause mortality, stroke, major bleeding events, or contrast induced nephropathy were not affected by the revascularization strategy.
Conclusion
The findings of this meta-analysis suggest that in patients with STEMI and MVD, complete revascularization is superior to culprit-only PCI in reducing the risk of MACE outcomes, including cardiovascular mortality, without increasing the risk of adverse safety outcomes.
Keywords: Coronary artery disease, ST-segment elevation myocardial infarction, Complete revascularization, Infarct artery only revascularization, Multi-vessel disease
1. Introduction
Primary percutaneous coronary intervention (PCI) is the treatment of choice of patients with ST-segment elevation myocardial infarction (STEMI) [1], [2], [3]. Approximately half of those patients have multivessel disease (MVD) [4], who carry worse clinical outcome after primary PCI compared with those with single vessel coronary artery disease (CAD) [5], [6]. The standard treatment for hemodynamically stable patients with STEMI and MVD is primary PCI of the culprit lesion that aims at early myocardial reperfusion [7], [8]. Historic randomized controlled trials (RCTs) [9], [10], [11] influenced the American College of Cardiology/American Heart Association (ACC/AHA) to update their guidelines recommendation class from III to IIb for the PCI of the non-culprit in hemodynamically stable patients [12]. Another RCT showed that fractional flow reserve (FFR)-guided PCI of non-culprit lesions in patients with MVD resulted in decreased composite cardiovascular (CV) adverse events, compared with only culprit lesion PCI, thus offering new evidence on the value of complete revascularization (CR) in STEMI [13]. These findings prompted the European Society of Cardiology (ESC) to upgrade its guidelines to the recommendation class IIa [2]. However, these trials were limited by their relatively small sample sizes, and it remained uncertain if endpoints other than revascularization were reduced. The recently published COMPLETE trial [14], which included more patients than all previous RCTs combined, confirmed the findings of the previous trials. Moreover, it showed that CR of stable STEMI patients with MVD reduced the risk of all cardiac events including the composite of cardiovascular death and myocardial infarction, with a significant reduction in spontaneous myocardial infarction. However, it is still uncertain whether there is a significant reduction in cardiovascular and total death.
Therefore, we conducted this meta-analysis of randomized clinical trials to assess the efficacy of CR compared with PCI of only culprit lesion in lowering the risk of cardiovascular and total deaths in patients with STEMI and MVD.
2. Methods
We followed the guidelines of the 2009 preferred reporting items for systematic reviews and meta-analysis (PRISMA) statement [15]. Due to the study design (meta-analysis), neither Institutional Review Board (IRB) approval nor patient informed consent was needed.
This meta-analysis was registered on PROSPERO, with number CRD42020149697.
2.1. Search strategy
We systematically searched PubMed-Medline, EMBASE, Scopus, Google Scholar, the Cochrane Central Registry of Controlled Trials and ClinicalTrial.gov, up to September 2019, using the following key words: “percutaneous coronary intervention” OR “PCI” AND “myocardial infarction” OR “ST elevation myocardial infarction” OR “STEMI” OR “multi vessel” AND “Culprit artery” OR “target vessel revascularization” OR “infarct related artery revascularization” OR “non-culprit artery” OR “complete”. Additional searches for potential trials included the references of review articles on that issue, and the abstracts from selected congresses: scientific sessions of the European Society of Cardiology (ESC), the American Heart Association (AHA), American College of Cardiology (ACC) and European Society of Atherosclerosis (EAS). The wild-card term ‘‘*’’ was used to increase the sensitivity of the search strategy. The literature search was limited to articles published in English. Two reviewers (IB and HJ) independently evaluated each article separately. No filters were applied. The remaining articles were obtained in full-text and assessed again by the same two researchers who evaluated each article independently, carried out data extraction and quality assessment. Disagreements were resolved by discussion with a third party (GB).
2.2. Eligibility criteria
Selected studies had to fulfill the following criteria: (i) Studies with hemodynamically stable STEMI patients with low clinical and anatomical complexity; (ii) Randomized design comparing CR and culprit only revascularization; and (iii) Outcome data at follow-up. None of the studies evaluated in this meta-analysis included hemodynamically unstable patients complicated with heart failure or shock.
2.3. Data extraction
Eligible studies were reviewed and the following data were abstracted: (1) first author's name; (2) year of publication; (3) name of clinical trial; (4) country where the study was performed; (5) number of centers; (6) study design; (7) number of participants in the two groups of STEMI revascularization and (8) clinical data of interest as well as number of events with respect to clinical outcomes were extracted.
2.4. Outcomes and definitions
The primary outcomes tested were major adverse cardiac events (MACE), which were considered as per-study definition, all-cause mortality, cardiac mortality, non-fatal myocardial infarction, revascularization, stroke, contrast induced nephropathy and major bleeding (Supplementary Table 1). Complete revascularization was defined as revascularization of non-culprit lesions in STEMI patients, either during the same procedure or staged during index hospitalization or after discharge. Only culprit lesion revascularization was defined as PCI of the only infarct related artery.
2.5. Quality assessment
Assessment of risk of bias in the included studies was evaluated by the same investigators for each study and was performed systematically using the Cochrane quality assessment tool for RCTs [16]. The Cochrane tool has 7 criteria for quality assessment: random sequence generation (selection bias), allocation sequence concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias) and other potential sources of bias. The risk of bias in each study was classified as “low”, “high” or “unclear”.
2.6. Statistical analysis
The meta-analysis was performed using the RevMan (Review Manager [RevMan] Version 5.1, The Cochrane Collaboration, Copenhagen, Denmark), with two-tailed p value < 0.05 considered as significant [17]. The baseline characteristics are reported as median and range. Mean and standard deviation (SD) values were estimated using the method described by Hozo et al [18]. The analysis is presented in forest plots. Meta-analyses were performed with a fixed-effects model and a random effect model was used if heterogeneity was encountered. Heterogeneity between studies was assessed using Cochrane Q test and I2 index. As a guide, I2 < 25% indicated low, 25–50% moderate and > 50% high heterogeneity [19]. Based on value of hazard ratio when it is 1, above or below we calculated the risk relative risk for CV events [20]. Publication bias was assessed using visual inspection of funnel plots and Egger’s test.
3. Results
3.1. Search results and trial flow
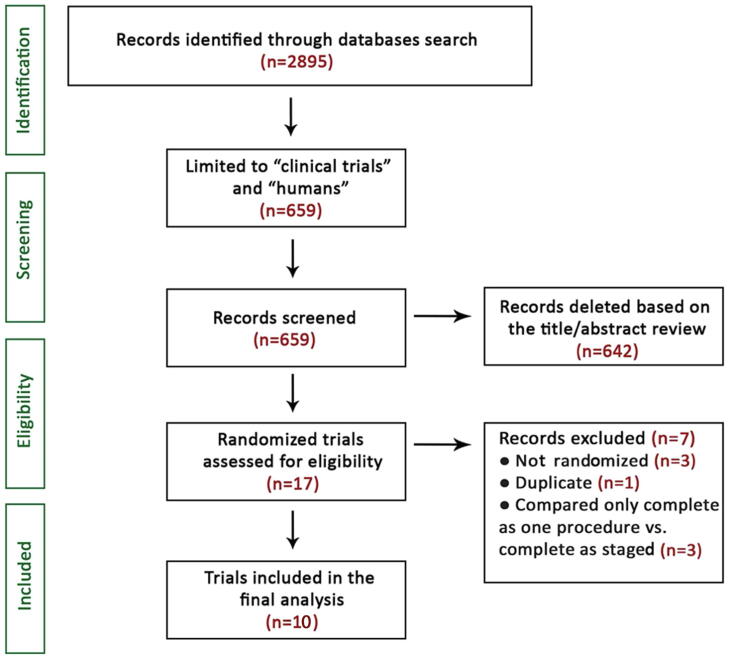
Of 2895 articles identified in the initial searches, 659 studies were screened as potentially relevant, but following critical scrutiny only 10 RCTs [9], [10], [11], [13], [14], [21], [22], [23], [24], [25] deemed appropriate for inclusion (Fig. 1). Three studies which compared complete revascularization at staged procedure vs. indexed procedure were also excluded having failed the preset definition of randomization [26], [27], [28]. FFR was systematically used to stratify patients with MVD only in two studies [11], [24].
Fig. 1.
PRISMA study selection flow chart.
3.2. Characteristics of included studies
The ten qualified studies had a total of 7033 patients, 3420 in the CR group and 3613 in the culprit-only revascularization group. The duration of the follow-up ranged from 4 to 38 months (median 27.7 months). The mean age of patients was 61.8 years, 81% male, 24% diabetes, 40.4% arterial hypertension, 34.6% dyslipidemia and 51.2% smokers (Supplementary Table 1).
3.3. Clinical outcomes
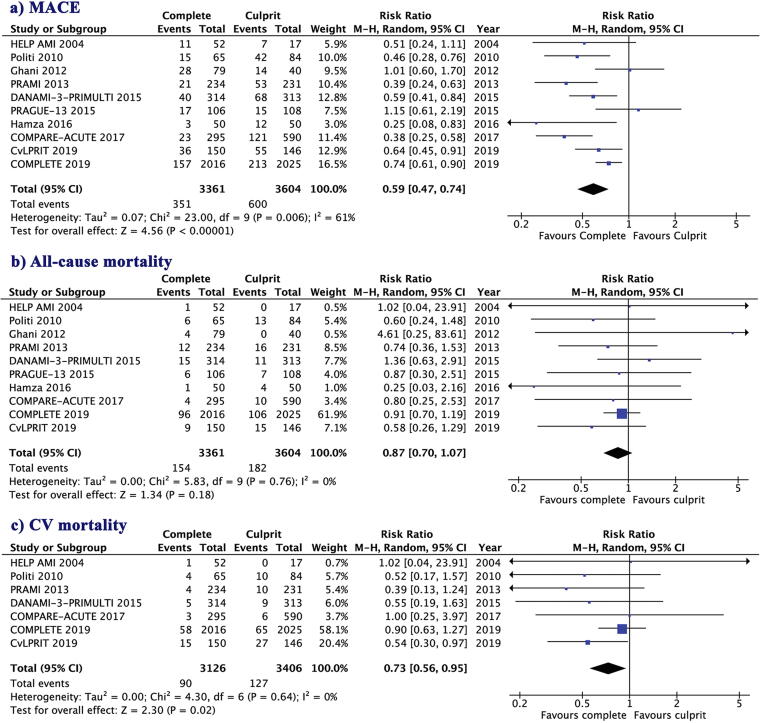
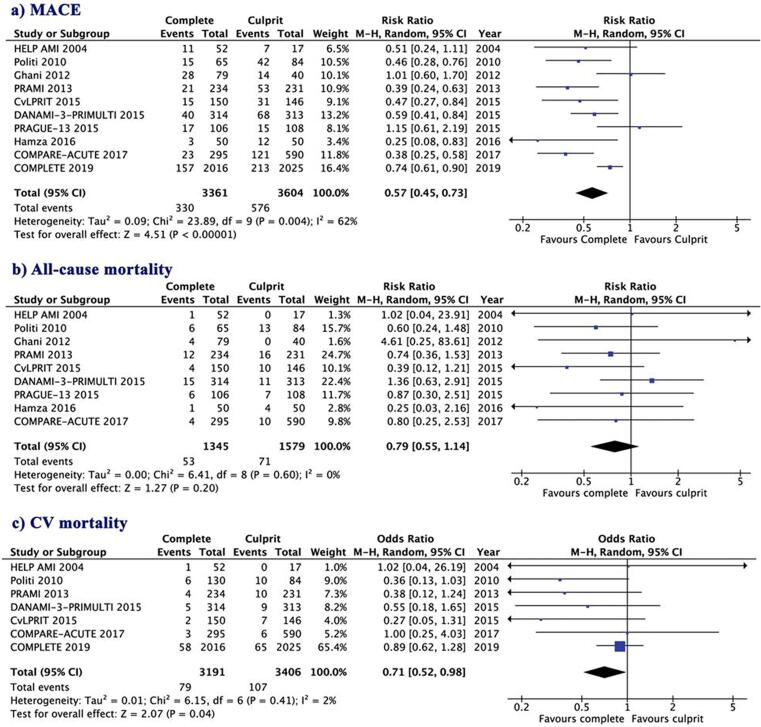
MACE was reported in all trials, but its definition differed among studies (Supplementary Table 2). In comparison to culprit-only, the CR strategy was associated with lower risk for MACE (10.4% vs.16.6%; RR = 0.59, 95% CI: 0.47 to 0.74, p < 0.0001, I2 = 61%, Fig. 2a) and CV mortality (2.87% vs. 3.72%; RR = 0.73, 95% CI: 0.56 to 0.95, p = 0.02, I2 = 0%, Fig. 2c). Whereas the risk of all-cause mortality (4.58% vs. 5.04%; RR = 0.87, 95% CI: 0.70 to 1.07, p = 0.18, I2 = 0%, Fig. 2b) did not differ between groups. A meta-regression analysis showed that follow-up was associated with higher MACE in the two group of revascularization (p = 0.04 for both), all-cause mortality (p < 0.001 and p = 0.03, respectively) and CV mortality (p < 0.001 for both, Supplementary Fig. 1).
Fig. 2.
Risk ratios of outcome with complete revascularization versus culprit-only revascularization; (a) MACE; (b) All-cause mortality; (c) CV mortality.
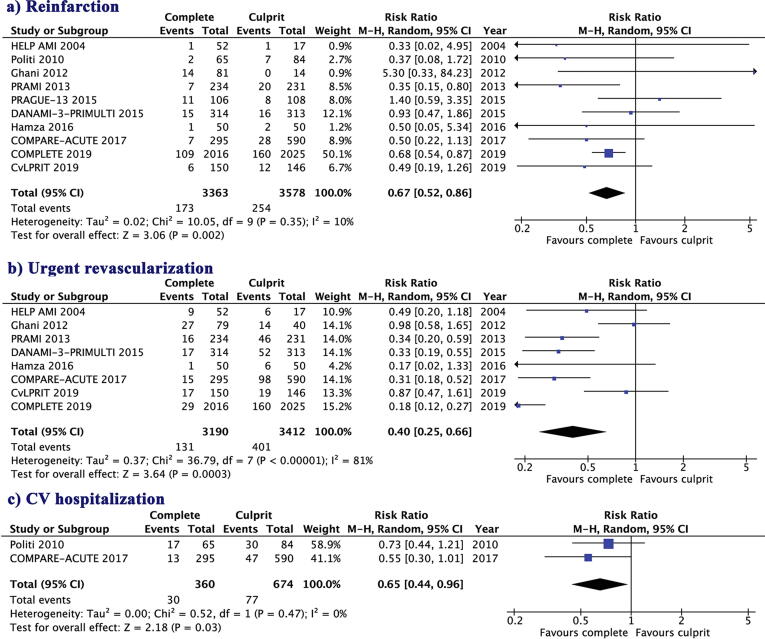
Furthermore, the other clinical outcome measures including reinfarction (5.1% vs. 7.1%; RR = 0.67, 95% CI: 0.52 to 0.86, p = 0.002, I2 = 10%, Fig. 3a), urgent revascularization (7.92% vs.17.4%; RR = 0.40, 95% CI: 0.25 to 0.66, p < 0.001, I2 = 81%) and CV hospitalization (8.68% vs.11.4%; RR = 0.65, 95% CI: 0.44 to 0.96, p = 0.03, I2 = 0%) were higher in the culprit-only group compared with the CR group (Fig. 3b & c). There was no evidence for publication bias according to the Egger’s test used, for any of the outcomes assessed. Clinical outcomes of the meta analysis are summarized in Supplementary Fig. 2.
Fig. 3.
Risk ratios of outcome with complete revascularization versus culprit-only revascularization; (a) Reinfarction; (b) Urgent revascularization; (c) Hospitalization.
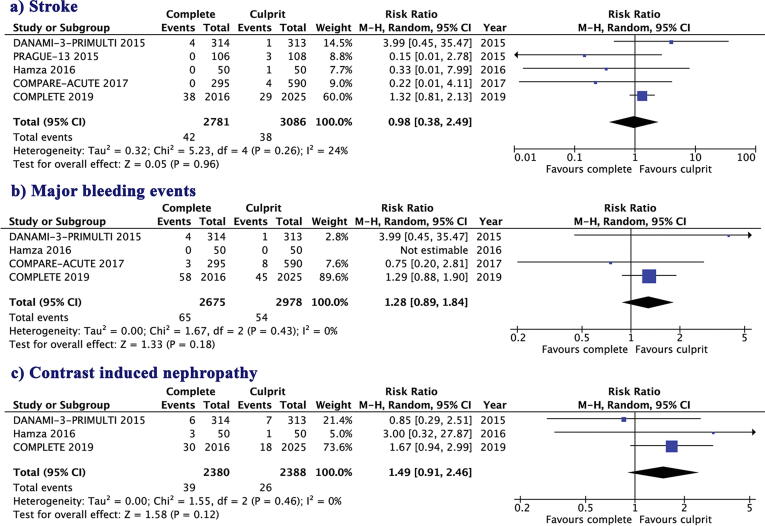
3.4. Safety outcomes
Complete revascularization was associated with similar risk of stroke (1.52% vs.1.23%; RR = 0.98, 95% CI: 0.38 to 2.49, p = 0.96, I2 = 24%), major bleeding events (2.42% vs.1.81%; RR = 1.28, 95% CI: 0.89 to 1.84, p = 0.18, I2 = 0%) and contrast induced nephropathy (1.62% vs.1.11%; RR = 1.49, 95% CI: 0.91 to 2.46, p = 0.12, I2 = 0%, Fig. 4a-c) to culprit-only revascularization. There was no evidence for publication of bias with Egger’s test for any of the outcomes assessed.
Fig. 4.
Risk ratios of safety procedure with complete revascularization versus culprit-only revascularization; (a) Stroke; (b) Major bleeding events; (c) Contrast induced nephropathy.
3.5. Influence analysis
The influence analysis was not performed as a classic leave-one-out analysis but only by excluding the COMPLETE trial. Exclusion of the COMPLETE trial, which represented more than 50% of the study population did not change the results of our analysis, Fig. 5, Supplementary Figs. 3-4).
Fig. 5.
Risk ratios of outcome with complete revascularization versus culprit-only revascularization with the exclusion of COMPLETE trial 2019; (a) MACE; (b) All-cause mortality; (c) CV mortality.
3.6. Risk of bias assessment
The assessment of risk of bias and applicability concerns based on the Quality Assessment of Diagnostic Accuracy Studies questionnaire (QUADAS-2) was used on our study questions (Supplementary Table 3) [15]. All of the criteria domains for risk of bias and applicability were analyzed. The risk of bias was assessed as ‘‘low risk,’’ ‘‘high risk,’’ or ‘‘unclear risk’’. Most studies had high quality (high or moderate level) and clearly defined objectives and the main outcomes (Supplementary Table 4, Supplementary Fig. 5). All domains had low risk of bias (<20%), and no evidence for publication bias based on the Egger’s test.
4. Discussion
This meta-analysis of RCTs compared the efficacy and safety of CR versus a culprit-only PCI strategy in hemodynamically stable patients with STEMI. The main findings can be summarized as follows: (1) CR is associated with a significant reduction in the risk for MACE over a median of 27.7 months (range 38–42 months). This benefit is derived from significant reduction in re-infarction and the need for urgent revascularization and hospitalization; (2) CR significantly reduced CV mortality, when compared with culprit-only revascularization strategy; and (3) CR is safe in this group of stable patients with regards to procedure related stroke, contrast-induced nephropathy and major bleeding events.
The previous evidence for CR of patients with STEMI and MVD in hemodynamically stable patients, based on which the current guidelines recommendation class IIb (ACC/AHA) [12] and IIa (ESC) [2] is limited. On the other hand, the COMPLETE trial with its larger number of patients provided a stronger evidence supporting CR over and above culprit-only revascularization for such patients. CR resulted in reduced risk for the composite of CV death or recurrent myocardial infarction during the follow-up period [14]. However, this benefit was driven mainly by a reduction in myocardial infarction, since CV mortality and all-cause mortality were not significantly different between groups.
The pooled analysis of all data from included RCTs [9], [10], [11], [13], [14], [21], [22], [23], [24], [25] found a significant difference between the CR strategy and culprit only strategy on all-cause mortality. It should be appreciated that the evidence for significant clinical benefit from CR over and above culprit-only revascularization was not clear from the older data [9], [10], [11], [13], [14], [21], [22], [23]. Older trials and meta analyses did not support an additional benefit from CR, probably because of different inclusion criteria of patients and studies as well as different means for measuring clinical outcome [29], [30], [31], [32], [33], [34], [35], [36], [37]. We believe that the results of the current meta analysis are of clinical relevance based on reduced MACE at mid-term follow up which is what concerns most patients. Apart from the cost, our analysis did not show any significant difference in the other potential CR related complications when compared with culprit only revascularization, thus supporting the CR approach. Finally, the extra cost itself should be assessed in comparison with the cost of readmission and myocardial infarction, which might result in significant irreversible myocardial loss.
In view of the findings of this meta-analysis and the discussion above we anticipate that the current clinical guidelines should benefit from advancing the recommendation for CR in stable STEMI patients as a routine strategy when it is feasible. In this line, a recent meta-analysis of the revascularization strategy in patients with STEMI and multivessel disease [38] demonstrated a reduction of CV mortality in patients who underwent complete revascularization. This meta-analysis, assessed by inverse variance, included 6 RCTs and was focused on CV mortality as the main outcome. The CV mortality reduction in favor of complete revascularization strategy in this meta-analysis was less significant compared with our results. Moreover, we included 10 RCTs, including the updated CvLPRIT (with follow-up 3.6 years). Thus, our results are supportive of the previously published meta-analysis [38].
4.1. Limitations
Like most meta-analyses of RCTs based on systematic search of the published literature, our meta-analysis is also subject to several limitations. This is a study-level meta analysis and therefore we could not adjust our results for several patient characteristics that might influence the study outcomes. Lack of sufficient data to perform subgroup analyses of the different outcome between the two strategies of complete revascularization strategy, index vs. staged procedure, is another limitation. We consider that the time when CR is performed may be important in line with previous suggestion of 72 h [39]. We were not able to use the hazard ratio to measure the effect of CR procedure, due to considerable heterogeneity in the follow-up duration. The safety outcome was not reported in all trials. Although most of the RCTs had high quality and all domain had low risk of bias, there was a moderate degree of heterogeneity in MACE and urgent revascularization. Also, not all RCTs included all assessed outcomes. Finally, the definition of non-culprit significant stenosis, using angiographic or functional criteria, was heterogeneous in the included RCTs. However, recent meta-analysis that compared the two different approaches [40] suggested the need of dedicated prospective studies that will directly compare angiography with physiology-guided CR strategy in STEMI patients.
5. Conclusion
The current meta-analysis demonstrates that the risk of MACE, CV mortality, reinfarction, need for urgent revascularization and hospitalization for patients with STEMI and multi-vessel disease undergoing primary PCI are reduced by complete revascularization compared with the culprit-only coronary artery strategy. PCI related complications were not different between the two strategies.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijcha.2020.100549.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References:
- 1.Keeley E.C., Boura J.A., Grines C.L. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361(9351):13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 2.Ibanez B., James S., Agewall S., Antunes M.J., Bucciarelli-Ducci C., Bueno H. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur. Heart J. 2018;39(2):119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 3.Wong G.C., Welsford M., Ainsworth C., Abuzeid W., Fordyce C.B., Greene J. 2019 Canadian Cardiovascular Society/Canadian Association of Interventional Cardiology Guidelines on the Acute Management of ST-Elevation Myocardial Infarction: Focused Update on Regionalization and Reperfusion. Can. J. Cardiol. 2019;35(2):107–132. doi: 10.1016/j.cjca.2018.11.031. [DOI] [PubMed] [Google Scholar]
- 4.Cardarelli F., Bellasi A., Ou F.S., Shaw L.J., Veledar E., Roe M.T. Combined impact of age and estimated glomerular filtration rate on in-hospital mortality after percutaneous coronary intervention for acute myocardial infarction (from the American College of Cardiology National Cardiovascular Data Registry) Am. J. Cardiol. 2009;103(6):766–771. doi: 10.1016/j.amjcard.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 5.Sorajja P., Gersh B.J., Cox D.A., McLaughlin M.G., Zimetbaum P., Costantini C. Impact of multivessel disease on reperfusion success and clinical outcomes in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Eur. Heart J. 2007;28(14):1709–1716. doi: 10.1093/eurheartj/ehm184. [DOI] [PubMed] [Google Scholar]
- 6.Jaski B.E., Cohen J.D., Trausch J., Marsh D.G., Bail G.R., Overlie P.A. Outcome of urgent percutaneous transluminal coronary angioplasty in acute myocardial infarction: comparison of single-vessel versus multivessel coronary artery disease. Am. Heart J. 1992;124(6):1427–1433. doi: 10.1016/0002-8703(92)90053-x. [DOI] [PubMed] [Google Scholar]
- 7.Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC)1, P.G. Steg, S.K. James, D. Atar, L.P. Badano, C. Blömstrom-Lundqvist, M.A. Borger, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 33(20) (2012) 2569–2619. [DOI] [PubMed]
- 8.O'Gara P.T., Kushner F.G., Ascheim D.D., Casey D.E., Jr, Chung M.K., de Lemos J.A. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127(4):e362–e425. doi: 10.1161/CIR.0b013e3182742cf6. [DOI] [PubMed] [Google Scholar]
- 9.Wald D.S., Morris J.K., Wald N.J., Chase A.J., Edwards R.J., Hughes L.O. Randomized trial of preventive angioplasty in myocardial infarction. N. Engl. J. Med. 2013;369(12):1115–1123. doi: 10.1056/NEJMoa1305520. [DOI] [PubMed] [Google Scholar]
- 10.Gershlick A.H., Banning A.S., Parker E., Wang D., Budgeon C.A., Kelly D.J. Long-Term Follow-Up of Complete Versus Lesion-Only Revascularization in STEMI and Multivessel Disease: The CvLPRIT Trial. J. Am. Coll. Cardiol. 2019;74(25):3083–3094. doi: 10.1016/j.jacc.2019.10.033. [DOI] [PubMed] [Google Scholar]
- 11.Engstrøm T., Kelbæk H., Helqvist S., Høfsten D.E., Kløvgaard L., Holmvang L. Complete revascularization versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3-PRIMULTI): an open-label, randomized controlled trial. Lancet. 2015;386(9994):665–671. doi: 10.1016/s0140-6736(15)60648-1. [DOI] [PubMed] [Google Scholar]
- 12.Levine G.N., Bates E.R., Blankenship J.C., Bailey S.R., Bittl J.A., Cercek B. 2015 ACC/AHA/SCAI Focused Update on Primary Percutaneous Coronary Intervention for Patients With ST-Elevation Myocardial Infarction: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. J. Am. Coll. Cardiol. 2016;67(10):1235–1250. doi: 10.1016/j.jacc.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 13.Smits P.C., Abdel-Wahab M., Neumann F.J., Boxma-de Klerk B.M., Lunde K., Schotborgh C.E. Fractional Flow Reserve-Guided Multivessel Angioplasty in Myocardial Infarction. N. Engl. J. Med. 2017;376(13):1234–1244. doi: 10.1056/NEJMoa1701067. [DOI] [PubMed] [Google Scholar]
- 14.S.R. Mehta, D.A. Wood, R.F. Storey, R. Mehran, K.R. Bainey, H. Nguyen, et al. for the COMPLETE Trial Steering Committee and Investigators. for the COMPLETE Trial Steering Committee and Investigators. N. Engl. J. Med. 381(15) (2019) 1411–1421. [DOI] [PubMed]
- 15.D. Moher, A. Liberati, J. Tetzlaff, D.G. Altman, P. Group, Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009; 339: b2535. [DOI] [PMC free article] [PubMed]
- 16.Green S. Cochrane handbook for systematic reviews of interventions version 5.1. 0 [updated March 2011] Cochr. Collabor. 2011 [Google Scholar]
- 17.Cooper H.M., Hedges L.V. Russell Sage Foundation; New York: 1994. The Handbook of Research Synthesis. [Google Scholar]
- 18.Hozo S.P., Djulbegovic B., Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.J. Abramson, Z. Abramsonm, Making Sense of Data: A Self-Instruction Manual on the Interpretation of Epidemiological Data. Oxford University Press. ISBN 0‐19‐514525‐9, 2001.
- 21.Politi L., Sgura F., Rossi R., Monopoli D., Guerri E., Leuzzi C. A randomised trial of target-vessel versus multi-vessel revascularisation in ST-elevation myocardial infarction: major adverse cardiac events during long-term follow-up. Heart Br. Card Soc. 2010;96(9):662–667. doi: 10.1136/hrt.2009.177162. [DOI] [PubMed] [Google Scholar]
- 22.Hamza M., Elgendy I.Y. A Randomized Trial of Complete Versus Culprit-Only Revascularization During Primary Percutaneous Coronary Intervention in Diabetic Patients With Acute ST Elevation Myocardial Infarction and Multi Vessel Disease. J. Intervent. Cardiol. 2016;29(3):241–247. doi: 10.1111/joic.12293. [DOI] [PubMed] [Google Scholar]
- 23.O. Hlinomaz, Multivessel coronary disease diagnosed at the time of primary PCI for STEMI: complete revascularization versus conservative strategy (PRAGUE 13 trial). Pap Present Eur 2015 Paris Fr.
- 24.A. Ghani, J.-H.E. Dambrink, A.W.J. van ’t Hof, J.P. Ottervanger, A.T.M. Gosselink, J.C.A. Hoorntje, Treatment of non-culprit lesions detected during primary PCI: long-term follow-up of a randomised clinical trial. Neth. Heart J. Mon. J. Neth. Soc. Cardiol. Neth. Heart Found. 20(9) (2012) 347–353. [DOI] [PMC free article] [PubMed]
- 25.Di Mario C., Mara S., Flavio A., Imad S., Antonio M., Anna P. Single vs multivessel treatment during primary angioplasty: results of the multicentre randomised HEpacoat for cuLPrit or multivessel stenting for Acute Myocardial Infarction (HELP AMI) Study. Int. J. Cardiovasc. Intervent. 2004;6(3–4):128–133. doi: 10.1080/14628840310030441. [DOI] [PubMed] [Google Scholar]
- 26.Maamoun W., Elkhaeat N., Elarasy R. Safety and feasibility of complete simultaneous revascularization during primary PCI in patients with STEMI and multi-vessel disease. Egypt Heart J. 2012;63(39):43. [Google Scholar]
- 27.Saad M., Rashed A., El-kilany W., El-Haddad M., Elgendy Y. Preliminary Report on the Safety and Efficacy of Staged versus Complete Revascularization in Patients with Multivessel Disease at the Time of Primary Percutaneous Coronary Intervention. Int. J. Angiol. 2017;26(3):143–147. doi: 10.1055/s-0036-1572522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Corpus R., House J., Marso S., Grantham J., Huber K., Laster S. Multivessel percutaneous coronary intervention in patients with multivessel disease and acute myocardial infarction. Am. Heart J. 2004;148:493–500. doi: 10.1016/j.ahj.2004.03.051. [DOI] [PubMed] [Google Scholar]
- 29.Bajraktari G., Jashari H., Ibrahimi P., Alfonso F., Jashari F., Ndrepepa G., Elezi S., Henein M.Y. Complete revascularization for patients with ST-segment elevation myocardial infarction and multivessel coronary artery disease: a meta-analysis of randomized trials. Coron. Artery Dis. 2018;29(3):204–215. doi: 10.1097/MCA.0000000000000602. [DOI] [PubMed] [Google Scholar]
- 30.Witberg G., Kornowski R. Current perspectives on revascularization in multivessel ST elevation myocardial infarction. Coron. Artery Dis. 2017;28(6):498–506. doi: 10.1097/MCA.0000000000000496. [DOI] [PubMed] [Google Scholar]
- 31.Anantha Narayanan M., Reddy Y.N.V., Sundaram V., Reddy Y.N.V., Baskaran J., Agnihotri K. What is the optimal approach to a non- culprit stenosis after ST-elevation myocardial infarction - Conservative therapy or upfront revascularization? An updated meta-analysis of randomized trials. Int. J. Cardiol. 2016;1(216):18–24. doi: 10.1016/j.ijcard.2016.04.054. [DOI] [PubMed] [Google Scholar]
- 32.Elgendy Islam Y., Mahmoud Ahmed N., Kumbhani Dharam J., Bhatt Deepak L., Bavry Anthony A. Complete or Culprit-Only Revascularization for Patients With Multivessel Coronary Artery Disease Undergoing Percutaneous Coronary Intervention. JACC: Cardiovasc. Intervent. 2017;10(4):315–324. doi: 10.1016/j.jcin.2016.11.047. [DOI] [PubMed] [Google Scholar]
- 33.Shah R., Berzingi C., Mumtaz M., Jasper J.B., Goswami R., Morsy M.S. Meta-Analysis Comparing Complete Revascularization Versus Infarct-Related Only Strategies for Patients With ST-Segment Elevation Myocardial Infarction and Multivessel Coronary Artery Disease. Am. J. Cardiol. 2016;118(10):1466–1472. doi: 10.1016/j.amjcard.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 34.Vaidya S.R., Qamar A., Arora S., Devarapally S.R., Kondur A., Kaul P. Culprit versus multivessel coronary intervention in ST-segment elevation myocardial infarction: a meta-analysis of randomized trials. Coron. Artery Dis. 2017 doi: 10.1097/MCA.0000000000000578. [DOI] [PubMed] [Google Scholar]
- 35.Qamar A., Bhatt D.L. Culprit-Only vs. Complete Revascularization During ST-Segment Elevation Myocardial Infarction. Prog. Cardiovasc. Diseases. 2015;58(3):260–266. doi: 10.1016/j.pcad.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 36.Gupta A., Bajaj N.S., Arora P., Arora G., Qamar A., Bhatt D.L. FFR-guided multivessel stenting reduces urgent revascularization compared with infarct-related artery only stenting in STelevation myocardial infarction: A meta-analysis of randomized controlled trials. Int. J. Cardiol. 2018;1(252):63–67. doi: 10.1016/j.ijcard.2017.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bravo C.A., Hirji S.A., Bhatt D.L., Kataria R., Faxon D.P., Ohman E.M. Complete versus culprit-only revascularisation in ST elevation myocardial infarction with multi-vessel disease. Cochrane Database Syst. Rev. 2017;2017(5):CD011986. doi: 10.1002/14651858.CD011986.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.R. Pavasini, S. Biscaglia, E. Barbato, M. Tebaldi, D. Dudek, J. Escaned, et al. Complete revascularization reduces cardiovascular death in patients with ST-segment elevation myocardial infarction and multivessel disease: systematic review and meta-analysis of randomized clinical trials. Eur. Heart J. 2019 Dec 31. pii: ehz896. [DOI] [PubMed]
- 39.Fortuni F., Crimi G., Angelini F., Leonardi S., D'Ascenzo F., Ferlini M. Early Complete Revascularization in Hemodynamically Stable Patients With ST-Segment Elevation Myocardial Infarction and Multivessel Disease. Can. J. Cardiol. 2019;35(8):1047–1057. doi: 10.1016/j.cjca.2019.03.006. [DOI] [PubMed] [Google Scholar]
- 40.G. Gallone, F. Angelini, F. Fortuni, M. Gnecchi, O. De Filippo, L. Baldetti, et al. Angiography- versus physiology guided complete revascularization in patients with STEMI and multivessel disease: who's the better gatekeeper in this setting? Eur. Heart J. Qual. Care Clin. Outcomes. 2020 Feb 3. pii: qcaa007. doi: 10.1093/ehjqcco/qcaa007. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.