Abstract
Many therapies have been developed for patients with mass rotator cuff tears. Partial repair is often performed in patients with partially repairable massive rotator cuff tears because it is simpler to perform than superior capsule reconstruction. It may, however, result in rotator cuff retears frequently. This article presents our modified technique of arthroscopic partial reconstruction of the superior capsule using the long head of the biceps tendon with a biceps interposition.
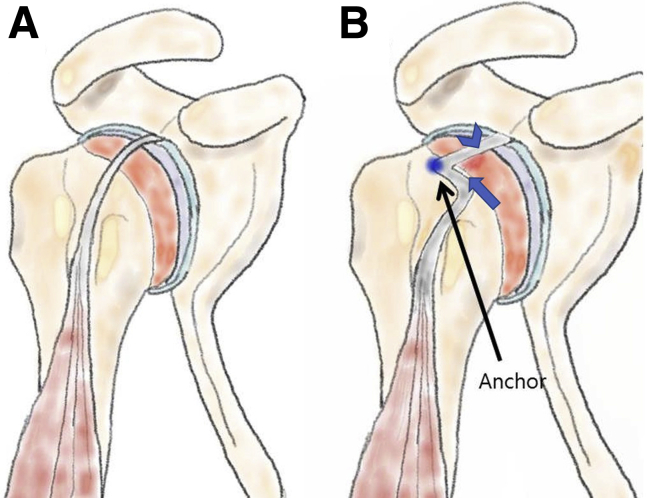
Massive rotator cuff tears (RCTs) are very difficult to treat for shoulder surgeons.1 Many treatments have been developed to manage massive RCTs.2 Superior capsule reconstruction (SCR) is known to be an effective treatment for irreparable massive RCTs.3 However, partial repair is often performed in patients with partially repairable massive RCTs because of the difficulty in performing SCR and the relative simplicity of performing partial repair.4 It may, however, result in frequent retears of the rotator cuff. The technique described in this report is an arthroscopic partial SCR and biceps interposition using the long head of the biceps tendon (LHBT) to ensure preservation in partially repairable massive RCT patients; we call it the biceps tendon L-shape shifting technique (Fig 1, Video 1).
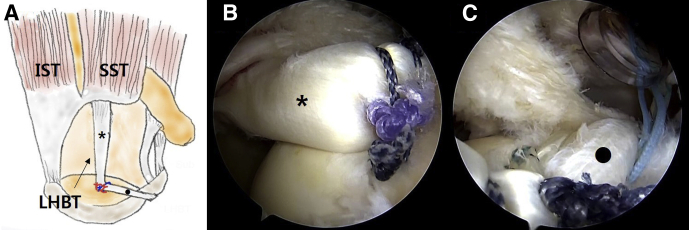
Fig 1.
(A) Technique using intra- and extra-articular portions of the long head of the biceps tendon with preservation of the biceps tendon anchors to the glenoid labrum. (B) Biceps tendon L-shape shifting technique. The arrowhead indicates the partial superior capsule reconstruction. The arrow indicates the interposition.
Surgical Technique
Preoperative Workup
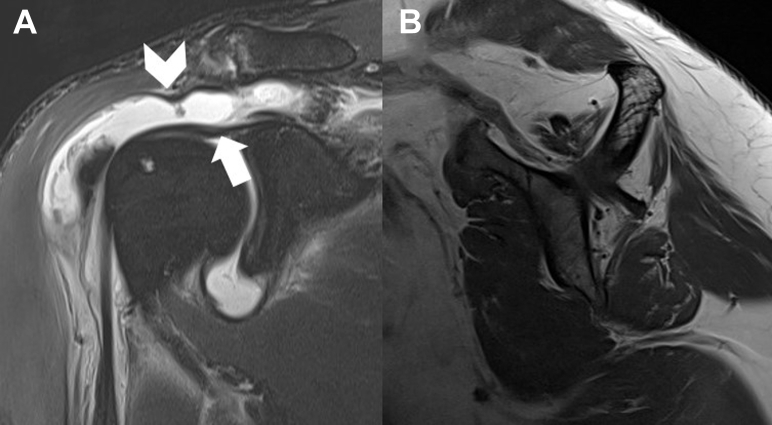
The indications to use the biceps tendon L-shape shifting technique are massive RCTs with poor-quality tendons that have a Goutallier classification of grade 3 to 4 and are partially repairable. Because this technique uses the LHBT, preoperative magnetic resonance imaging should confirm that the LHBT is normal or less than 20% damaged (Fig 2, Table 1).
Fig 2.
(A) Preoperative T2-weighted oblique-coronal magnetic resonance image in a 67-year-old female patient with a massive retracted cuff tear (arrowhead) and intact attachment of the long head of the biceps tendon to the glenoid labrum (arrow). (B) Preoperative T2-weighted sagittal magnetic resonance image showing a Goutallier grade 3 supraspinatus tendon.
Table 1.
Indications for Biceps Tendon–Shifting Technique
| Partially repairable supraspinatus and/or infraspinatus tear |
| Severe shoulder pain with failed conservative management |
| Goutallier grade 3 or 4 supraspinatus and/or infraspinatus |
| Good quality of LHBT anchors to glenoid labrum (normal or <20% partial tear) |
| Minimal to no glenohumeral arthritis |
LHBT, long head of biceps tendon.
Patient Position and Diagnostic Arthroscopy
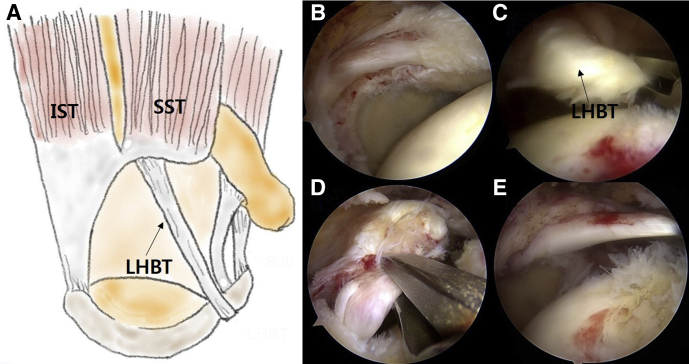
The patient undergoes general anesthesia and is positioned in the beach-chair position with the arms externally rotated, abducted 30°, and fixed with padded arm sleeves (STAR sleeve; Arthrex, Naples, FL). The posterior viewing portal is made approximately 2 cm medial and inferior to the posterolateral corner of the acromion. A standard 30° arthroscope (Arthrex) is introduced, and the anterior portal is made at the rotator interval. Diagnostic arthroscopy is performed to examine the glenohumeral joint, the articular side of the supraspinatus tendon, and the subscapularis tendon, as well as to assess the quality of the LHBT. The mobility of the LHBT should be checked with a tendon grasper (Arthrex) (Fig 3). If the condition of the LHBT at the glenoid labrum position is not favorable to perform the biceps-shifting technique, if the LHBT is not movable, or if the LHBT is partially torn more than 20%, we choose another treatment option.
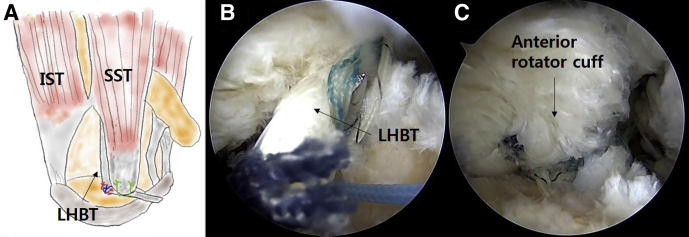
Fig 3.
(A) Massive rotator cuff tear. (B-E) Intra-articular arthroscopic view through posterior portal. (B) A massive rotator cuff tear is observed. (C) The anterior rotator cuff is shown moving sufficiently to allow partial repair. (D) The posterior rotator cuff is shown moving sufficiently to allow partial repair. (E) The long head of the biceps tendon (LHBT) is observed moving sufficiently to perform this technique, and there is no subsequent damage. (IST, infraspinatus tendon; SST, supraspinatus tendon.)
The arthroscope is inserted into the subacromial space through the posterior portal to examine the subacromial space. The lateral portal is made approximately 3 cm lateral to the anterolateral corner of the acromion. Bursectomy is performed using a shaver (Arthrex) that is passed through the lateral portal. Acromioplasty and coracoacromial ligament release are performed with an Arthrocare device (Smith & Nephew, Andover, MA) and burr (Arthrex). The arthroscope is inserted into the lateral portal, and a bursectomy is performed. A portal of Wilmington (viewing portal) is made (Fig 4).
Fig 4.
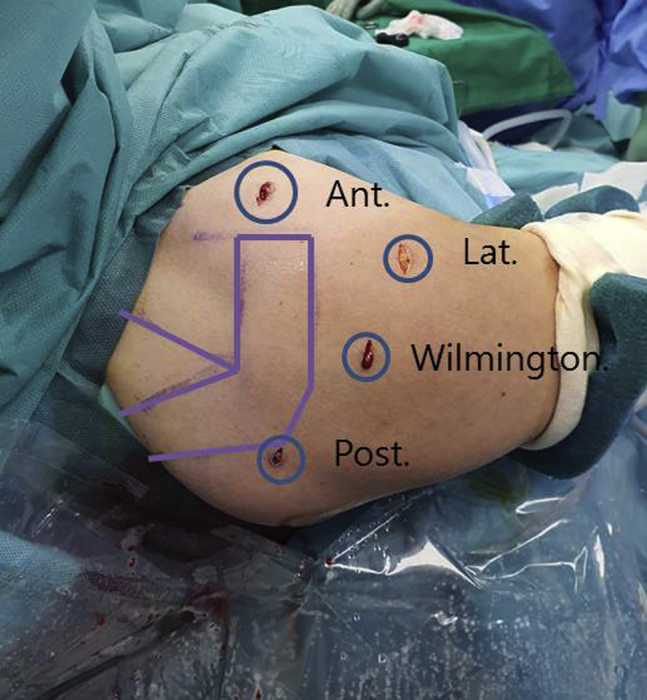
We use the beach-chair position for the biceps-shifting technique. The portals used for this technique are shown, with the posterior portal (Post) and Wilmington portal as viewing portals and the anterior portal (Ant) and lateral portal (Lat) as working portals.
The greater tuberosity of the humeral bone bed is decorticated for LHBT and rotator cuff attachment using a shaver and burr (Fig 5). We use a laser-marked probe (Arthrex) to measure the anterior-to-posterior and medial-to-lateral cuff tear diameter of the LHBT. Cannulas (8.25-mm × 7-cm; Arthrex) are inserted into the anterior and lateral portals to facilitate instrumentation.
Fig 5.
The greater tuberosity of the humeral head is decorticated by a burr (viewed through the lateral portal). The condition of the long head of the biceps tendon must be evaluated before this procedure.
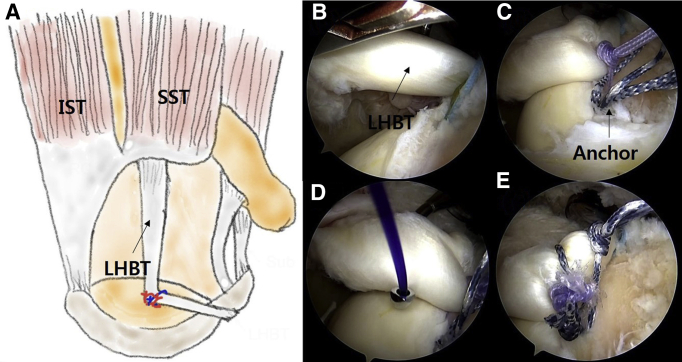
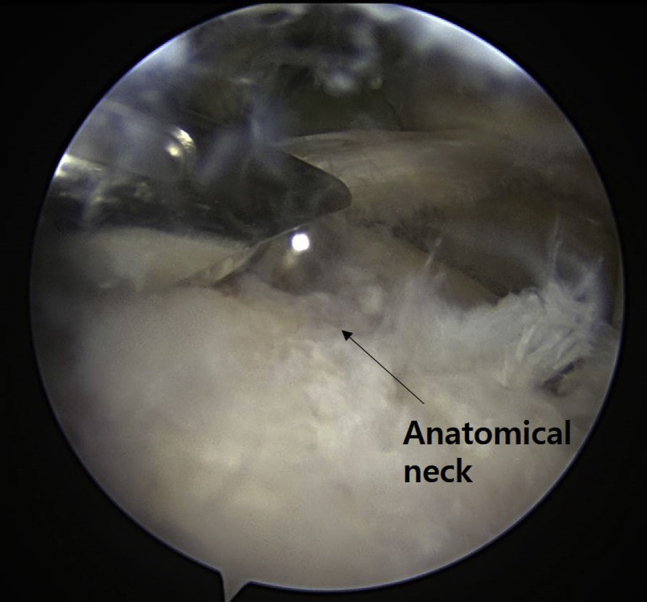
Biceps Tendon Shifting and Fixation and Partial SCR
The anchor portal is positioned using an arthroscope and spinal needle. Through the anchor portal, the anchor (HEALIX triple-loaded suture anchor; DePuy Mitek, Raynham, MA) is inserted at the position where the posterior rotator cuff and LHBT would overlap and be sutured. This is confirmed by moving the posterior rotator cuff to the humeral head area using the tendon grasper (Arthrex). This position is usually a posterosuperior position, 1 to 2 cm from the bicipital groove. A suture hook (Arthrex) is prepared with No. 1 polydioxanone suture (Ethicon, Somerville, NJ) and introduced through the anterior portal for knot tying by the SMC technique. The first suture limb should pass through the LHBT to capture the tendon at the anchor site. The second suture limb wraps around the LHBT and is then tied. The third suture limb passes through the LHBT to secure fixation at the anchor site (Fig 6). Owing to shifting and fixing the LHBT at the anchor site, the LHBT from the anchor to the glenoid attachment site serves as a partial SCR. The LHBT from the anchor site to the bicipital groove uses a biceps tendon interposition between the RCT and humeral head, aiding in biological healing and strengthening poor-quality rotator cuff tendons (Fig 7).
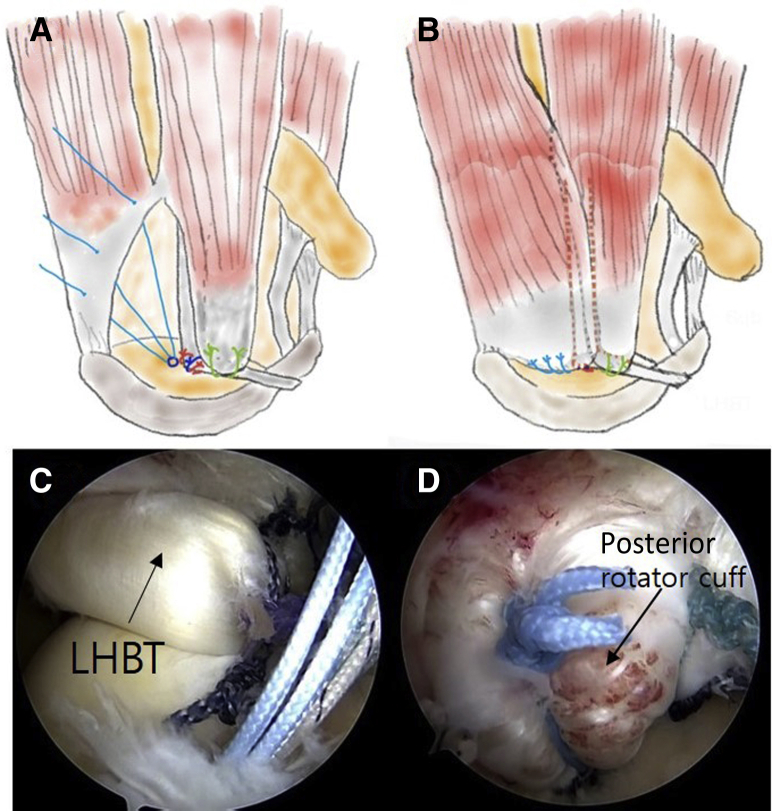
Fig 6.
(A) Biceps tendon fixation. We use the Wilmington portal as the viewing portal. (B) The anchor (HEALIX triple-loaded suture anchor) is inserted into the greater tuberosity of the humeral head to secure the long head of the biceps tendon (LHBT). (C) The first suture limb should be tied after passing the LHBT. (D) The second suture limb wraps around the LHBT and is then tied. (E) The third suture limb is sutured through the LHBT to strengthen the anchoring force. (IST, infraspinatus tendon; SST, supraspinatus tendon.)
Fig 7.
(A) Function of each part of biceps tendon. (B) The long head of the biceps tendon (LHBT) from the anchor site to the glenoid attachment site serves the role of a partial superior capsule (asterisk). (C) The LHBT from the anchor site to the bicipital groove functions as an interposition for the anterior rotator cuff (circle). (IST, infraspinatus tendon; SST, supraspinatus tendon.)
Anterior Rotator Cuff Repair
An additional anchor (HEALIX triple-loaded suture anchor) is attached behind the LHBT for an anterior RCT repair. Each bundle is fixed with a single-row tie through the anterior rotator cuff and the augmented LHBT (Fig 8). This achieves a complete repair of the anterior rotator cuff using the LHBT.
Fig 8.
(A) Anterior rotator cuff repair. (B) Sutures are tied through the rotator cuff and the interposed long head of the biceps tendon (LHBT). (C) The anterior rotator cuff is repaired. Sealing with the interposed LHBT provides an increased thickness and holding force. (IST, infraspinatus tendon; SST, supraspinatus tendon.)
Posterior Rotator Cuff Repair
An additional anchor is inserted posterolaterally into the greater tuberosity of the humeral head just behind the LHBT fixation site for posterior RCT repair. Posterior RCTs are treated using a single-row repair with a suture anchor (HEALIX triple-loaded suture anchor) (Fig 9). This is performed to increase the thickness of the posterior-superior capsule by overlapping the LHBT and posterior rotator cuff.
Fig 9.
(A, B) Posterior rotator cuff repair. (C) The anchor is inserted posterolaterally into the greater tuberosity of the humeral head just behind the long head of the biceps tendon (LHBT) fixation site. (D) The posterior rotator cuff is repaired. The overlapping of the LHBT and posterior rotator cuff will improve the thickness of the superior capsule.
Radiographic Results
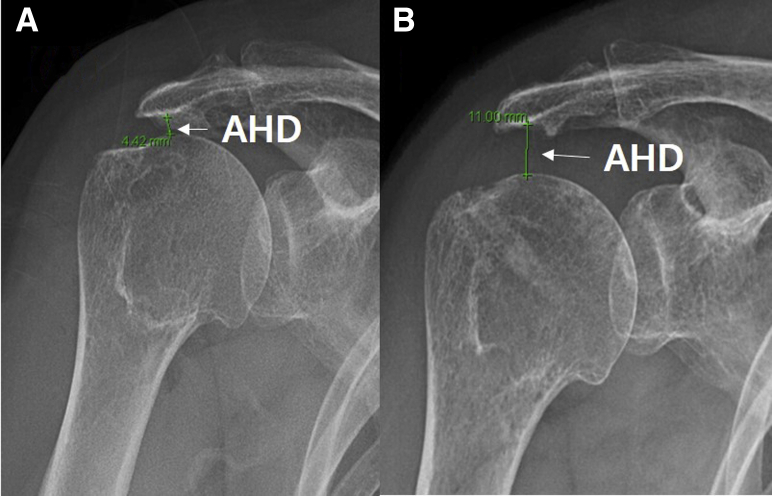
Comparison of preoperative and postoperative radiographs indicated an increased acromiohumeral distance. This finding suggests that the arthroscopic biceps-shifting technique may improve the static stability of the glenohumeral joint of the shoulder. Moreover, a restored center of rotation of the humeral head was noted (Fig 10, Table 2).
Fig 10.
Rockwood-view radiographs of shoulder preoperatively and postoperatively in a 67-year-old female patient. (A) The preoperative radiograph shows superior humeral head migration (Hamada grade II). (B) The postoperative radiograph shows inferior humeral head migration (from 4.4 mm to 11 mm) compared with the preoperative radiograph. (AHD, acromiohumeral distance.)
Table 2.
Key Surgical Steps With Pearls and Pitfalls
| Key Steps | Pearls | Pitfalls |
|---|---|---|
| Diagnostic arthroscopy | The surgeon should check the attachment of the LHBT to the glenoid labrum. The surgeon should make sure the LHBT is moved to the area where it will be fixed. |
If a >20% partial tear of the LHBT is present, one cannot perform this technique. |
| Acromioplasty, coracoacromial ligament release, and bursectomy | Bursectomy should be performed sufficiently to view the entire cuff tear and glenoid. | |
| Humeral and glenoid bone bed preparation and anchor insertion | A spinal needle should be used to localize the portals. The bone bed should be debrided sufficiently. |
In the case of insufficient bone bed decortication, biological fixation may result. |
| Biceps shifting and fixation | Too much shifting can cause pain and erosion of the biceps tendon. | |
| Anterior rotator cuff repair | The surgeon should not apply too much tension when performing partial repair. The surgeon should seal the LHBT and anterior rotator cuff together. |
The surgeon should not perform repair of 1 bundle with another bundle. |
| Posterior rotator cuff repair | The surgeon should not apply too much tension when performing partial repair. | The surgeon should not perform repair of 1 bundle with another bundle. |
LHBT, long head of biceps tendon.
Postoperative Care
Postoperatively, patients are treated by our massive RCT repair protocol. After surgery, a shoulder abduction brace is applied immediately in the operating room. Shoulder joint movement is restricted during the period of abduction brace application. Passive motion is started 8 weeks postoperatively, after removal of the abduction brace. Active range of motion is performed after 12 weeks, and external rotation–strengthening exercises are started after 16 weeks.
Discussion
The superior capsule is a static stabilizer of the glenohumeral joint.5 Therefore, its absence causes superior migration of the humeral head and hastens rotator cuff arthropathy.5 This is the reason SCR has recently been recommended.
However, many operators often perform partial repair rather than SCR when partial repair is possible in patients with massive RCTs. This may be because of the difficulty of performing the SCR. However, in massive RCT patients, the use of only partial repair was found to result in a retear rate of about 50%.6 This is because the tendon quality of the rotator cuff that was repaired is low, and it can be thought that it is caused by failure to restore the superior capsule. Tensor fascia lata autograft is most commonly used in SCR.3 This autograft has side effects that can cause pain at the harvest site. It also requires several medical staff members to operate on both sites, and the operative duration is quite long.
To overcome these disadvantages, the SCR method involving the rerouting of the LHBT has been presented.7 The LHBT can be harvested easily during shoulder surgery, and it is unnecessary to prepare other parts of the harvest site, such as the hip and knee, for autograft harvesting. Because autografts are used, the possibility of infection after surgery is lower than that with allograft involvement. Mihata et al.3 recommended using autografts with a thickness of at least 8 mm. The thickness of the LHBT, however, is 5 to 10 mm, which was sufficient for SCR. However, rerouting techniques require a bony procedure to be performed somewhere other than the anatomic position of the bicipital groove. Moreover, they can cause increased tension on the biceps tendon. Subsequently, this may lead to erosion and pain.
A method of repairing the rotator cuff by interpositioning the LHBT between the RCT and the humeral head bone bed has also been described.8 This method uses tenotomized LHBT to repair massive RCTs to prevent undue tension on the biceps tendon. However, there is a disadvantage in that the strength of the superior capsule region cannot be reinforced owing to the tenotomized LHBT. Moreover, this technique cannot be performed if the cuff defect is larger than the diameter of the tenotomized biceps.
We combine 2 previous surgical techniques that use the LHBT, leading to the design of a technique that can be used in patients with massive RCTs, which are not completely repairable. This may be better than a simple partial repair. This technique can give downward forces to the humeral head as in the rerouting technique of the LHBT. Moreover, without additional formation of the bicipital groove, determining the fixed position of the LHBT, by checking the mobility of the posterior rotator cuff, will avoid undue tension or erosion. Biceps interposition may enhance the biological healing of the anterior rotator cuff by this technique. The overlap of the damaged rotator cuff with the LHBT will make the superior capsule thicker and harder. The operation time is also reduced compared with previous procedures.
A limitation is that our technique needs high-quality LHBT. This technique cannot be indicated in patients with a more than 20% partial tear of the biceps tendon itself or severe biceps tendinitis. So, it is important to check the quality of the LHBT anchors with preoperative magnetic resonance imaging and physical examination. In addition, because this technique moves and repairs the LHBT, further research is needed to determine whether side effects such as pain or erosion occur. Moreover, future research on clinical outcomes is critical to pursue.
Footnotes
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Modified technique of arthroscopic partial reconstruction of the superior capsule and biceps augmentation using the long head of the biceps tendon (LHBT) to treat partially repairable massive rotator cuff tears (RCTs). Diagnostic arthroscopy is performed through the posterior portal. After a massive cuff tear is identified, it is important to verify that the anterior rotator cuff and posterior rotator cuff are partially repaired. It is also important to check the quality of the LHBT anchors to the labrum and assess damage to the LHBT. An anchor is inserted in the area where the LHBT will be fixed to the humeral head. The first suture is passed through the LHBT and tied, and the second suture wraps around the LHBT and is then tied. The third suture is tied back through the LHBT. Because of shifting and fixing of the LHBT by the anchor, the anchor site to the glenoid attachment site of the LHBT serves as a partial superior capsule reconstruction. The LHBT from the anchor site to the bicipital groove functions as a biceps augmentation. An additional anchor is inserted between the bicipital groove and the LHBT fixation site for anterior RCT repair. Each bundle is fixed with a single-row tie through the anterior rotator cuff and the augmented LHBT. This achieves a complete repair of the anterior rotator cuff using the LHBT. In addition, the LHBT can be used to increase the thickness of the anterior superior capsule. An additional anchor is inserted posterolaterally into the greater tuberosity of the humeral head just behind the LHBT fixation site for posterior RCT repair. Posterior rotator cuff repair is performed using single-row anchor sutures. The posterior rotator cuff should be repaired to cover the LHBT from the glenoid to the anchor site. This is performed to increase the thickness of the posterior-superior capsule by overlapping the LHBT and the posterior rotator cuff. Repair is performed with little tension on the rotator cuff. Furthermore, the rotator cuff thickness is confirmed to be thicker. The final reconstructed capsule is visualized via the viewing portal.
References
- 1.Schmidt C.C., Jarrett C.D., Brown B.T. Management of rotator cuff tears. J Hand Surg Am. 2015;40:399–408. doi: 10.1016/j.jhsa.2014.06.122. [DOI] [PubMed] [Google Scholar]
- 2.Thorsness R., Romeo A. Massive rotator cuff tears: Trends in surgical management. Orthopedics. 2016;39:145–151. doi: 10.3928/01477447-20160503-07. [DOI] [PubMed] [Google Scholar]
- 3.Mihata T., Lee T.Q., Watanabe C. Five-year follow-up of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. J Bone Joint Surg Am. 2019;101:1921–1930. doi: 10.2106/JBJS.19.00135. [DOI] [PubMed] [Google Scholar]
- 4.Oh J.H., Park M.S., Rhee S.M. Treatment strategy for irreparable rotator cuff tears. Clin Orthop Surg. 2018;10:119–134. doi: 10.4055/cios.2018.10.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ishihara Y., Mihata T., Tamboli M. Role of the superior shoulder capsule in passive stability of the glenohumeral joint. J Shoulder Elbow Surg. 2014;23:642–648. doi: 10.1016/j.jse.2013.09.025. [DOI] [PubMed] [Google Scholar]
- 6.Malahias M.A., Kostretzis L., Chronopoulos E., Brilakis E., Avramidis G., Antonogiannakis E. Arthroscopic partial repair for massive rotator cuff tear: Does it work? A systematic review. Sports Med Open. 2019;11(5):13. doi: 10.1186/s40798-019-0186-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim Y.S., Lee H.J., Park I., Sung G.Y., Kim D.J., Kim J.H. Arthroscopic in situ superior capsular reconstruction using the long head of the biceps tendon. Arthrosc Tech. 2018;7:e97–e103. doi: 10.1016/j.eats.2017.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park S.R., Sun D.H., Kim J., Lee H.J., Kim J.B., Kim Y.S. Is augmentation with the long head of the biceps tendon helpful in arthroscopic treatment of irreparable rotator cuff tears? J Shoulder Elbow Surg. 2018;27:1969–1977. doi: 10.1016/j.jse.2018.04.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Modified technique of arthroscopic partial reconstruction of the superior capsule and biceps augmentation using the long head of the biceps tendon (LHBT) to treat partially repairable massive rotator cuff tears (RCTs). Diagnostic arthroscopy is performed through the posterior portal. After a massive cuff tear is identified, it is important to verify that the anterior rotator cuff and posterior rotator cuff are partially repaired. It is also important to check the quality of the LHBT anchors to the labrum and assess damage to the LHBT. An anchor is inserted in the area where the LHBT will be fixed to the humeral head. The first suture is passed through the LHBT and tied, and the second suture wraps around the LHBT and is then tied. The third suture is tied back through the LHBT. Because of shifting and fixing of the LHBT by the anchor, the anchor site to the glenoid attachment site of the LHBT serves as a partial superior capsule reconstruction. The LHBT from the anchor site to the bicipital groove functions as a biceps augmentation. An additional anchor is inserted between the bicipital groove and the LHBT fixation site for anterior RCT repair. Each bundle is fixed with a single-row tie through the anterior rotator cuff and the augmented LHBT. This achieves a complete repair of the anterior rotator cuff using the LHBT. In addition, the LHBT can be used to increase the thickness of the anterior superior capsule. An additional anchor is inserted posterolaterally into the greater tuberosity of the humeral head just behind the LHBT fixation site for posterior RCT repair. Posterior rotator cuff repair is performed using single-row anchor sutures. The posterior rotator cuff should be repaired to cover the LHBT from the glenoid to the anchor site. This is performed to increase the thickness of the posterior-superior capsule by overlapping the LHBT and the posterior rotator cuff. Repair is performed with little tension on the rotator cuff. Furthermore, the rotator cuff thickness is confirmed to be thicker. The final reconstructed capsule is visualized via the viewing portal.