Abstract
The menisci are fibroelastic structures interposed between the articular surfaces of the femur and tibia. They absorb impact and transmit load. Meniscal injury may compromise function and cause rapid joint degeneration, leading to the development of secondary osteoarthritis. Surgical treatment of meniscal injury is usually performed by arthroscopy, and meniscectomy or meniscal suture may be associated with such treatment. Meniscal suture should be considered when the injury compromises the proper functioning of the meniscus to recover its anatomy and function. Different meniscal suture techniques exist; the most widely used are the inside-out, outside-in, and all-inside techniques. The gold-standard repair technique is the inside-out technique. A drawback of this technique is the need to alternate between intra- and extra-articular structures for every stitch, which makes it even more laborious. We describe the continuous meniscal suture technique, also called “meniscal stitching,” for a medial meniscal bucket-handle injury. This technique is performed from the inside out and allows the surgeon to perform multiple stitches with the same thread quickly and effectively. This surgical technique is performed using a single meniscal suture device that was developed by our group, called the “Meniscus 4 A-II” device.
The menisci are fibroelastic structures interposed between the articular surfaces of the femur and tibia in the medial and lateral compartments inside the knee. Their main functions are to absorb impact and transmit load, besides working as secondary joint stabilizers. They also make an important contribution to knee proprioception and lubrication.1,2
Rupture or meniscal injury may compromise the aforementioned functions and may lead to joint degeneration in a short period, leading to the development of secondary osteoarthritis.3,4 Surgical treatment for meniscal injury is performed by arthroscopy, and meniscectomy or meniscal suture may be performed. Because of the aforementioned factors, meniscal suture should be considered when the meniscal injury compromises the proper functioning of the meniscus to recover its anatomy and function. Several publications have reported the close relation between meniscectomy and secondary osteoarthritis development, as well as the long-term superiority of clinical and functional outcomes of meniscal repair compared with meniscectomy.3, 4, 5, 6
Different types of meniscal suture techniques exist; the most widely used are the outside-in, inside-out, and all-inside techniques. The all-inside meniscal suture has theoretical advantages such as a lower risk of neurovascular injury and a shorter surgical time and does not require additional incisions.7,8
Older publications, as we see in the systematic review by Hantes et al.,9 published in 2006, indicated that the inside-out suture technique yielded better results than the other techniques. This suture technique is still considered the gold standard because it allows for a stable suture combining vertical and longitudinal stitches on both the upper and lower surfaces. One disadvantage is the need for an additional incision to capture the needle outlet in a tight space, which needs to be revisited at every stitch10; thus, the utility of using all-inside devices has been examined, as we see in the systematic review by Kang et al.,8 published in 2019, which showed that both inside-out and all-inside meniscal sutures yielded similar and favorable results.
We have developed a meniscal suture device called the “Meniscus 4 A-II” device that enables the surgeon to perform meniscal suture from the inside out with continuous stitches on several planes without having to alternate between arthroscopic and extra-articular procedures, making the whole process faster and more efficient. In this article, we describe the continuous meniscal suture technique, also called “meniscal stitching,” for a medial meniscal bucket-handle injury. This technique, besides being fast and effective, is very economical because it is possible to repair the entire meniscus with a single repair device and 1 to 2 FiberWire sutures (Arthrex, Naples, FL).
Surgical Technique
The patient undergoes spinal anesthesia, and a pneumatic cuff is attached to the proximal third of the thigh. Asepsis and antisepsis are performed using detergent chlorhexidine followed by alcoholic chlorhexidine. Sterile surgical fields are placed, and the pneumatic cuff is inflated.
Standard arthroscopic portals are made through a transpatellar accessory portal longitudinally in the center of the patellar tendon. Joint exploration is performed, and the medial bucket-handle injury is diagnosed and reduced.
The surgical access incision is executed on the posteromedial aspect of the knee. To perform the incision, we identify 3 anatomic points: the posterior aspect of the tibial plateau, the adductor tubercle, and the joint line. A vertical oblique incision is made starting from the adductor tubercle toward the posterior face of the tibial plateau, passing distally 2 cm from the joint line. Care should be taken to avoid making the incision too posteriorly in relation to the adductor tubercle because the saphenous nerve passes 5 cm posteriorly. The fascia of the sartorius tendon is incised, and deep dissection under the fascia is performed. The incision over the sartorius should be completed as proximally as possible to avoid injury to the gracilis and semitendinosus tendons. After dissection, an anatomic triangle formed by the anterior joint capsule, medial gastrocnemius head posteriorly, and semimembranosus tendon distally is observed. Careful digital dissection is performed between the joint capsule and the medial gastrocnemius, allowing for greater visualization and the passage of neurovascular protectors. These devices can be sterile metal spoons or retractors similar to vaginal specula.10
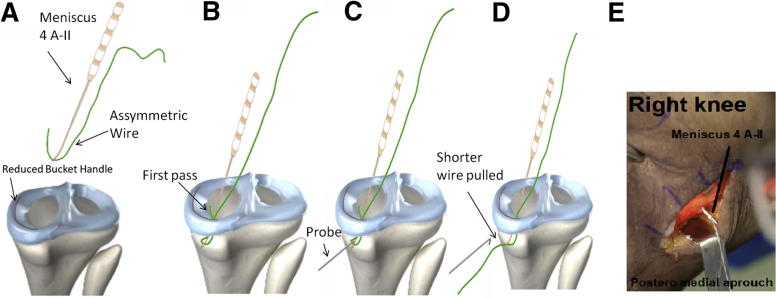
The Meniscus 4 A-II meniscal suturing device is prepared by passing a long nonabsorbable thread (longer than 100 cm) over the end of the device. We generally use a No. 2-0 FiberWire (Arthrex) without a needle. We pass the thread asymmetrically under the suture device. One end of the FiberWire is 10 cm long, and the other is 90 cm long (Fig 1A). We start the continuous suture, entering the clamps through the lateral or central portal, thereby defining the portal that we use according to the extension of the injury.
Fig 1.
(A) The Meniscus 4 A-II device is prepared, passing the FiberWire asymmetrically. (B) The Meniscus 4 A-II device is introduced into the most posterior region of the injured medial meniscus. (C, D) With the aid of a probe or Kelly clamp, the shorter FiberWire is pulled out of the knee. (E) The device is shown after it is introduced into the most posterior region of the injured medial meniscus in the right knee, just after the shortest wire has been pulled.
If the lesion starts at the transition from the posterior horn to the meniscal body, we start the meniscal repair through the lateral portal. If the lesion starts at the posterior horn, we start the meniscal repair through the transpatellar portal. We always start the first stitch through the most posterior injured region of the medial meniscus (Fig 1B).
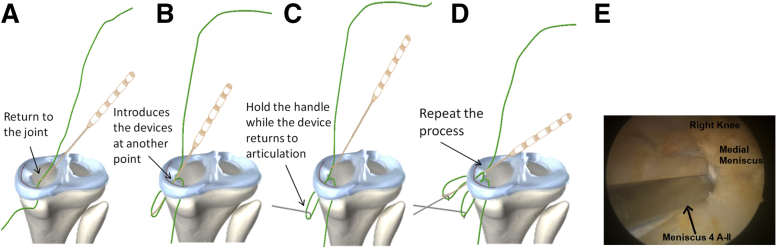
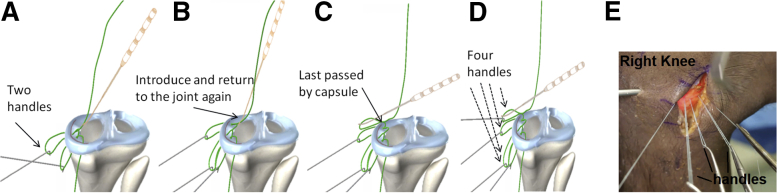
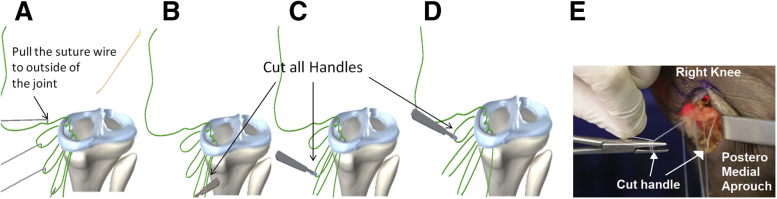
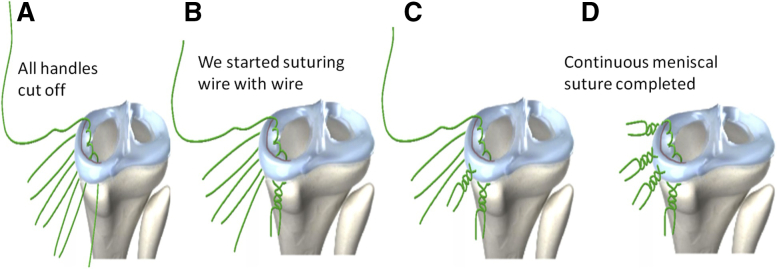
We insert the device into the injured face of the meniscus while using one of the retractors and pulling the medial gastrocnemius posteriorly. Digital palpation is used to locate the place where the tip of the device will come out on the posterior aspect of the knee. Palpation is possible because of the stiffness of the suture device before it completely crosses the joint capsule. After identifying the site, we introduce the Meniscus 4 A-II device further by visualizing and pulling the shorter FiberWire out of the knee (Fig 1 C and D). After this step, we hold this shorter end of the FiberWire with Kelly clamps (Fig 1 E). We return the Meniscus 4 A-II device to the inside of the knee and choose the next entry point of the suture (Fig 2A). We can perform horizontal or vertical points according to the lesion’s configuration. We repeat the aforementioned steps, always being attentive to protect the posterior knee structures, fully introducing the device and visualizing the FiberWire as we pull it into a loop. The loop is held out of the joint by the posteromedial access, and the suture device is pulled back into the joint (Fig 2C). Attention should be paid when the device is returned to the joint because the end of the handle that is coming out of the arthroscopic portal must be the same end that passes through the interior of the device. If the end of the loop passing through the device is the one that was introduced by the meniscus, an error will occur, requiring the continuous meniscal suture to be restarted. We choose the next entry point of the suture through the meniscus, passing the medial Meniscus 4 A-II device and keeping the newly formed handle with the same care as previously mentioned so that the device can return to the inside of the joint (Fig 2C). Returning to the joint, we reinsert the device several times (Fig 2E) according to the length of the FiberWire and the size of the lesion (Fig 3 A-C). After all the loops are formed (Figs 3 D and E and 4A), we cut them in their central region (Fig 4B) to keep the 2 formed FiberWire tips symmetrical (Fig 4 C-E). We then perform several stitches of FiberWire to FiberWire (formed after cutting the handles), completing the continuous meniscal suture (Fig 5). For bucket-handle injuries, we recommend 6 to 8 sutures on the proximal side of the meniscus and 4 to 6 sutures on the distal side (Video 1).
Fig 2.
The Meniscus 4 A-II device is returned to the joint (A), and the device is introduced into another location of the injured meniscus (B). (C) The handle is held while the device is returned to the joint. (D) The process is repeated. (E) Arthroscopic view through the anteromedial portal of Meniscus 4 A-II device in injured medial meniscus in right knee. The continuous meniscal suture is performed.
Fig 3.
With 2 handles formed (A), the device is introduced again, and meniscal stitching is performed (B). (C) The last pass is performed by the joint capsule. (D) Four handles are formed. (E) Right knee. Handles formed outside of joint, viewed through posteromedial surgical approach.
Fig 4.
(A) The end of the last handle formed is pulled and transported from the arthroscopic portal to the medial posterior access point. (B-D) All the handles are cut in its central region, leaving it symmetrical. (E) Cut handle with suturing of its ends in right knee.
Fig 5.
After all the handles are sectioned (A), suturing FiberWire by FiberWire is started (B, C). (D) After FiberWire suturing, the continuous meniscal suture is complete.
Discussion
Medial meniscal injuries should be repaired whenever possible, seeking mainly to recover the properties of load absorption, load distribution, and secondary knee stabilization. Studies have shown that the lateral meniscus accounts for 70% of impact absorption in the lateral compartment and the medial meniscus, 50% in the medial compartment.2,8,11,12
Musahl et al.13 showed that in knees with both medial meniscal and anterior cruciate ligament (ACL) injuries, anterior tibial subluxation at 30° increased considerably compared with knees with isolated ACL injuries. Meniscal nonrepair is a poor prognostic factor for both the recovery of stability and long-term evolution to osteoarthritis in patients undergoing ACL reconstruction.
The inside-out meniscal suture procedure remains the gold-standard technique for surgical treatment of meniscal bucket-handle injuries despite advances in all-inside suture devices that enable repair without additional incisions.14 This type of meniscal injury presents as a challenge for knee surgeons. The procedure is quite extensive and requires multiple stitches. At each stitch, the surgeon needs to alternate between suturing the meniscus with arthroscopic vision while protecting the neurovascular structures and capturing the needle outlet in the accessory incision. In addition, the surgeon needs to enter and exit the joint with various suture devices, one for each stitch.5
Studies have shown that procedures for suturing bucket-handle injuries have yielded inferior results compared with suturing of smaller injuries; thus, the optimal choice of surgical technique to treat these injuries is essential for favorable results.15, 16, 17 Samuelsen et al.18 compared the results of patients with bucket-handle injuries who underwent meniscal suturing with the all-inside versus inside-out technique. They evaluated and followed up 40 patients for an average of 4.4 years, observing similar clinical and functional results and a failure rate of approximately 20% in both groups. They also found that despite the evolution of all-inside devices with increasingly better results, the inside-out technique allows more stitches to be performed owing to easier suture passage and smaller needle holes (10.9 ± 3.2 stitches for the inside-out technique vs 5.1 ± 1.2 stitches for the all-inside technique).
Laurendon et al.19 conducted a similar study evaluating the prognostic factors of meniscal repair treated with all-inside devices. Eighty-seven patients with meniscal lesions were evaluated for an average of 31 months. The authors found that patients with a body mass index above 25 and bucket-handle lesions had a worse prognosis. They also observed an overall failure rate of 14.9% when meniscal injuries were treated with all-inside devices.
Yik et al.20 published a new meniscal suture technique using a hybrid approach with an inside-out suture device that passes proximal and distal threads vertically into the capsule without perforating the meniscal tissue, thus reducing the bucket-handle tear. While maintaining the reduction of the meniscal bucket-handle tear, suturing of the entire meniscus is initiated using all-inside meniscal suturing devices.
There are several inside-out suture devices on the market. Some, such as the No. 2-0 FiberWire Meniscus Repair Needle (Arthrex), consist of a long suture thread attached to 2 long, malleable needles. The disadvantage is that these needles allow only 1 stitch for each suture kit. Because of the great malleability of the needle, the device can follow an unwanted path, putting the neurovascular structures at risk.21
There are also soft lumen needles that allow the use of a single kit at more than 1 point, such as the Protector Meniscus (Arthrex). The disadvantage of these needles is that the strap that attaches to the suture is fragile and breaks easily.13,22,23
The Meniscus 4 A-II device has several advantages as a suture device used in meniscal repair. The device is rigid and has either straight- or curved-end options, making it easy to stitch in multiple directions with full control of needle-tip output at the desired location. Furthermore, the device is resistant. As a result, it can be used in surgery making several sutures in the meniscus, with a minimal chance of breaking the device, reducing the cost of the surgical procedure.
The device described in this article allows the surgeon to perform multiple stitches continuously and quickly. This reduces the surgical time and facilitates the performance of the surgical technique (Table 1).
Table 1.
Advantages, Disadvantages, Risks, and Limitations Associated With Use of Meniscus 4 A-II Device
| Advantages |
| Greater control over device needle exit point |
| Lower risk of neurovascular injury |
| Multiple sutures in several planes continuously |
| Greater agility to meniscal repair process |
| Low cost—single device allows suturing of entire meniscus |
| Resistant device |
| Disadvantages |
| Need to use posteromedial approach for neurovascular protection |
| Need to repair each loop of suture stitch |
| Risks |
| Chondral injury with tip of device |
| Neurovascular injury if posteromedial protector is not properly positioned |
| Limitations |
| A long nonabsorbable thread is necessary. |
| The device can be deformed at its extremity if it is pressed in an erroneous way, for example, if it is pressed against the tibial plateau or femoral condyle. |
| The technique can only be performed with the Meniscus 4 A-II device. |
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.L.R.d.F. has a patent pending for Dispositivo de Sutura Meniscal. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
On joint inspection, we visualized a broad longitudinal lesion simulating a reduced bucket-handle injury in a right cadaveric knee. The meniscal suture device, Meniscus 4 A-II, was prepared by passing a long, nonabsorbable, needleless thread over it. We threaded the FiberWire asymmetrically under the device with the front end of the FiberWire being 10 cm long. We inserted the device into the injured face of the meniscus. After identifying the device, we introduced and visualized it, pulling the shorter FiberWire out of the knee. After this step, we repaired this end of the FiberWire with a Kelly clamp. We returned the Meniscus 4 A-II device into the knee and chose the next entry point. We reinserted the Meniscus 4 A-II device, visualizing the FiberWire, and pulled it into a FiberWire loop. The loop should be formed so that the FiberWire exiting the arthroscopic portal is the same as the one passing through the suture device whereas the other end of the loop is the previously repaired FiberWire. The suture device was pulled back into the joint. We chose the new waypoint through the meniscus and introduced it by reidentifying the FiberWire handle and keeping the new handle with the same care as previously mentioned. We repeated these steps several times, depending on the size of the FiberWire and size of the lesion. Multiple loops were formed, and after all loops were formed, we sectioned them in their central region to make the lengths of the threads symmetrical and then sutured thread by thread. We cut the handle and continued to suture thread by thread. We observed that an anterior region of the meniscal body remained injured. We chose to perform 3 continuous sutures vertically. We reinserted the suture in the desired location, removed soft parts to exit the Meniscus 4 A-II device, and pulled the thread located in the anterior region of the suture device, which should always be the shortest. We repaired this. We returned the suture device to the inside of the joint, introduced the Meniscus 4 A-II device in the new desired location, formed the extra-articular handle according to the precautions mentioned earlier, repaired the handle, and returned to the joint. We introduced the device into a new location, forming a new meniscal loop; repaired it; returned to the interior of the joint; reinserted the meniscal suture device; and removed the FiberWire from within the device into the extra-articular region. In this way, we produced 2 handles and 2 ends of FiberWire. We passed the tip of the posterior extremity inside the most posterior loop and did the same with the tip of the anterior extremity, passing it through the anterior loop, and then pulled them. Locking the system, we then performed multiple sutures with the remaining 2 ends, fixing the lesion. Finally, we performed a continuous meniscal suture on the distal face of the meniscal lesion, repeating the process used for the continuous suture on the proximal face of the meniscal lesion, thus completing the surgical procedure.
References
- 1.Renstrom P., Johnson R.J. Anatomy and biomechanics of the menisci. Clin Sports Med. 1990;9:523–538. [PubMed] [Google Scholar]
- 2.Seedhom B.B., Dowson D., Wright V. Proceedings: Functions of the menisci. A preliminary study. Ann Rheum Dis. 1974;33:111. doi: 10.1136/ard.33.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petty C.A., Lubowitz J.H. Does arthroscopic partial meniscectomy result in knee osteoarthritis? A systematic review with a minimum of 8 years’ follow-up. Arthroscopy. 2011;27:419–424. doi: 10.1016/j.arthro.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 4.Dong Y., Hu H., Dong Y., Hu Y., Xu Q. The effect of meniscal tears and resultant partial meniscectomies on the knee contact stresses: A finite element analysis. Comput Methods Biomech Biomed Engin. 2014;17:1452–1463. doi: 10.1080/10255842.2012.753063. [DOI] [PubMed] [Google Scholar]
- 5.Xu C., Zhao J. A meta-analysis comparing meniscal repair with meniscectomy in the treatment of meniscal tears: The more meniscus, the better outcome? Knee Surg Sports Traumatol Arthrosc. 2015;23:164–170. doi: 10.1007/s00167-013-2528-6. [DOI] [PubMed] [Google Scholar]
- 6.Beaufils P., Pujol N. Management of traumatic meniscal tear and degenerative meniscal lesions. Save the meniscus. Orthop Traumatol Surg Res. 2017;103:S237–S244. doi: 10.1016/j.otsr.2017.08.003. (suppl) [DOI] [PubMed] [Google Scholar]
- 7.Jurist K.A., Greene P.W., III, Shirkhoda A. Peroneal nerve dysfunction as a complication of lateral meniscus repair: A case report and anatomic dissection. Arthroscopy. 1989;5:141–147. doi: 10.1016/0749-8063(89)90010-8. [DOI] [PubMed] [Google Scholar]
- 8.Kang D.G., Park Y.J., Yu J.H., Oh J.B., Lee D.Y. A systematic review and meta-analysis of arthroscopic meniscus repair in young patients: Comparison of all-inside and inside-out suture techniques. Knee Surg Relat Res. 2019;31:1. doi: 10.5792/ksrr.17.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hantes M.E., Zachos V.C., Varitimidis S.E., Dailiana Z.H., Karachalios T., Malizos K.N. Arthroscopic meniscal repair: A comparative study between three different surgical techniques. Knee Surg Sports Traumatol Arthrosc. 2006;14:1232–1237. doi: 10.1007/s00167-006-0094-x. [DOI] [PubMed] [Google Scholar]
- 10.Chahla J., Serra Cruz R., Cram T.R., Dean C.S., LaPrade R.F. Inside-out meniscal repair: Medial and lateral approach. Arthrosc Tech. 2016;5:e163–e168. doi: 10.1016/j.eats.2015.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fox A.J.S., Bedi A., Rodeo S.A. The basic science of human knee menisci: Structure, composition, and function. Sports Health. 2012;4:340–351. doi: 10.1177/1941738111429419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walker P.S., Erkman M.J. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. 1975;109:184–192. doi: 10.1097/00003086-197506000-00027. [DOI] [PubMed] [Google Scholar]
- 13.Musahl V., Citak M., O’Loughlin P.F., Choi D., Bedi A., Pearle A.D. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament–deficient knee. Am J Sports Med. 2010;38:1591–1597. doi: 10.1177/0363546510364402. [DOI] [PubMed] [Google Scholar]
- 14.Laible C., Stein D.A., Kiridly D.N. Meniscal repair. J Am Acad Orthop Surg. 2013;21:204–213. doi: 10.5435/JAAOS-21-04-204. [DOI] [PubMed] [Google Scholar]
- 15.Krych A.J., McIntosh A.L., Voll A.E., Stuart M.J., Dahm D.L. Arthroscopic repair of isolated meniscal tears in patients 18 years and younger. Am J Sports Med. 2008;36:1283–1289. doi: 10.1177/0363546508314411. [DOI] [PubMed] [Google Scholar]
- 16.Rubman M.H., Noyes F.R., Barber-Westin S.D. Arthroscopic repair of meniscal tears that extend into the avascular zone: A review of 198 single and complex tears. Am J Sports Med. 1998;26:87–95. doi: 10.1177/03635465980260013301. [DOI] [PubMed] [Google Scholar]
- 17.Rubman M.H., Noyes F.R., Barber-Westin S.D. Technical considerations in the management of complex meniscus tears. Clin Sports Med. 1996;15:511–530. [PubMed] [Google Scholar]
- 18.Samuelsen B.T., Johnson N.R., Hevesi M. Comparative outcomes of all-inside versus inside-out repair of bucket-handle meniscal tears: A propensity-matched analysis. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118779045. 2325967118779045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laurendon L., Neri T., Farizon F., Philippot R. Prognostic factors for all-inside meniscal repair. A 87 case series. Orthop Traumatol Surg Res. 2017;103:1017–1020. doi: 10.1016/j.otsr.2017.05.025. [DOI] [PubMed] [Google Scholar]
- 20.Yik J.H., Koh B.T.H., Wang W. A novel technique for modified all-inside repair of bucket-handle meniscus tears using standard arthroscopic portals. J Orthop Surg Res. 2017;12:188. doi: 10.1186/s13018-017-0692-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Naqui S.Z., Thiryayi W.A., Hopgood P., Ryan W.G. A biomechanical comparison of the Mitek RapidLoc, Mitek Meniscal repair system, Clearfix screws and vertical PDS and Ti-Cron sutures. Knee. 2006;13:151–157. doi: 10.1016/j.knee.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 22.Fillingham Y.A., Riboh J.C., Erickson B.J., Bach B.R., Yanke A.B. Inside-out versus all-inside repair of isolated meniscal tears. Am J Sports Med. 2017;45:234–242. doi: 10.1177/0363546516632504. [DOI] [PubMed] [Google Scholar]
- 23.Vaquero-Picado A., Rodríguez-Merchán E.C. Arthroscopic repair of the meniscus: Surgical management and clinical outcomes. EFORT Open Rev. 2018;3:584–594. doi: 10.1302/2058-5241.3.170059. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
On joint inspection, we visualized a broad longitudinal lesion simulating a reduced bucket-handle injury in a right cadaveric knee. The meniscal suture device, Meniscus 4 A-II, was prepared by passing a long, nonabsorbable, needleless thread over it. We threaded the FiberWire asymmetrically under the device with the front end of the FiberWire being 10 cm long. We inserted the device into the injured face of the meniscus. After identifying the device, we introduced and visualized it, pulling the shorter FiberWire out of the knee. After this step, we repaired this end of the FiberWire with a Kelly clamp. We returned the Meniscus 4 A-II device into the knee and chose the next entry point. We reinserted the Meniscus 4 A-II device, visualizing the FiberWire, and pulled it into a FiberWire loop. The loop should be formed so that the FiberWire exiting the arthroscopic portal is the same as the one passing through the suture device whereas the other end of the loop is the previously repaired FiberWire. The suture device was pulled back into the joint. We chose the new waypoint through the meniscus and introduced it by reidentifying the FiberWire handle and keeping the new handle with the same care as previously mentioned. We repeated these steps several times, depending on the size of the FiberWire and size of the lesion. Multiple loops were formed, and after all loops were formed, we sectioned them in their central region to make the lengths of the threads symmetrical and then sutured thread by thread. We cut the handle and continued to suture thread by thread. We observed that an anterior region of the meniscal body remained injured. We chose to perform 3 continuous sutures vertically. We reinserted the suture in the desired location, removed soft parts to exit the Meniscus 4 A-II device, and pulled the thread located in the anterior region of the suture device, which should always be the shortest. We repaired this. We returned the suture device to the inside of the joint, introduced the Meniscus 4 A-II device in the new desired location, formed the extra-articular handle according to the precautions mentioned earlier, repaired the handle, and returned to the joint. We introduced the device into a new location, forming a new meniscal loop; repaired it; returned to the interior of the joint; reinserted the meniscal suture device; and removed the FiberWire from within the device into the extra-articular region. In this way, we produced 2 handles and 2 ends of FiberWire. We passed the tip of the posterior extremity inside the most posterior loop and did the same with the tip of the anterior extremity, passing it through the anterior loop, and then pulled them. Locking the system, we then performed multiple sutures with the remaining 2 ends, fixing the lesion. Finally, we performed a continuous meniscal suture on the distal face of the meniscal lesion, repeating the process used for the continuous suture on the proximal face of the meniscal lesion, thus completing the surgical procedure.