Abstract
Reconstruction of the superior capsule is a valuable intervention for some patients in whom massive, irreparable posterosuperior rotator cuff tears are identified. Superior capsular reconstruction techniques most commonly use either tensor fascia lata autograft or dermal allograft. As an alternative to more traditional superior capsular reconstruction, we commonly transpose and incorporate the biceps tendon into the rotator cuff repair construct in such patients instead. This biological superior capsular reconstruction biceps transposition technique (”bio-SCR”), described herein, provides increased structural integrity and supplemental tendon graft using viable cells while potentially serving the role of the superior capsule. As such, transposition of the biceps tendon may offer unique and significant advantages over other techniques and can be an effective and valuable alternative in appropriate cases.
Rotator cuff tears are a common problem in the aging population. The prevalence of massive rotator cuff tears varies in some studies from 10% to 40%.1 In addition, chronic rotator cuff tears are often associated with significant fatty infiltration of the muscles and tendon retraction, both of which make rotator cuff repair more complex. Attempting to repair such tears can indeed be quite challenging even for very experienced surgeons. Atrophy, relatively poor tendon quality, and tendon immobility are commonly seen and make complete repair of these chronic and massive rotator cuff tears more difficult to achieve. Mihata et al.2 published results on superior capsular reconstruction (SCR) using tensor fascia lata (TFL) autograft to treat such tears and found an increased acromiohumeral distance (AHD) postoperatively, along with improved American Shoulder and Elbow Surgeons scores.
In an effort to avoid autograft harvest-site concerns associated with the TFL and to eliminate the necessity for use of a dermal allograft for reasons such as expense, technical challenges, and the potential risk of disease transmission, the long head of the biceps tendon (LHBT) has been proposed as an alternative to standard SCR grafts due in part to its close proximity to the rotator cuff tear. Biomechanical studies have shown that using the biceps tendon as an SCR graft may, in fact, restore glenohumeral stability. Han et al.,3 using a cadaveric rotator cuff tear model, found that shoulders in which the biceps was used as the reconstructed superior capsule showed decreased subacromial peak contact pressures and shifted the humeral head inferiorly. El-shaar et al.4 analyzed 5 sets of matched cadaveric shoulders after a massive rotator cuff tear was created in each shoulder. An SCR was performed using a TFL autograft in one of the cadaveric shoulder pairs, and the biceps tendon was used to reconstruct the superior capsule in the matched contralateral shoulder. The force required to translate the humeral head was then analyzed and compared. The results of El-shaar et al. showed similar and statistically insignificant effects related to stability between the 2 groups, suggesting that SCR using the LHBT is biomechanically equivalent to using TFL autograft.
We have described our approach for biceps transposition as the “bio-SCR” technique to characterize this procedure and to highlight the biological nature of transposing still viable biceps tendon cells as a graft. The transposed biceps tendon not only adds live supplemental tissue to massive rotator cuff repair constructs but also provides for additional structural support through convergence of the rotator cuff tissue to the securely stabilized, transposed biceps tendon. The transposed biceps tendon may also serve effectively in the important stabilizing role of the superior capsule because the biceps tendon is securely fixed both to the superior glenoid, owing to its native attachment, and to the superior humeral head via suture anchor fixation.
Surgical Technique
The surgical procedure can be performed with the patient in either the beach-chair or lateral decubitus position. After the induction of anesthesia, a thorough examination of both shoulders is carried out to evaluate and compare passive range of motion and glenohumeral joint stability. After the shoulder has been prepared and draped in usual fashion, standard posterior and anterior glenohumeral joint portals are made, and via an outside-in technique, an 18-gauge spinal needle is used to localize the anterior portal site (Video 1). A diagnostic arthroscopy, using a 30° arthroscope, is performed within the glenohumeral joint to assess the rotator cuff tear size and pattern and to confirm the presence of the biceps tendon. If the biceps tendon is absent or severely damaged, it cannot be transposed and incorporated into the posterosuperior rotator cuff repair construct. After completion of any intra-articular debridement or other procedures, the arthroscope is placed into the subacromial space using the same posterior portal, and a lateral subacromial portal is created using a spinal needle to localize the position that will allow for maximum access to the rotator cuff tear and subsequently provide for an excellent viewing portal when biceps transposition and rotator cuff repair are later accomplished. A complete subacromial bursectomy is performed to maximize visualization of the massive, retracted rotator cuff tear and to allow for inspection of the rotator cuff tissue for quality, mobility, and tear-pattern assessment (Fig 1). The undersurface of the acromion and coracoacromial ligament is evaluated for mechanical impingement. Evidence of abrasion on the undersurface of the acromion is addressed with an arch-sparing, gentle subacromial smoothing procedure. The acromioclavicular joint is then assessed, and approximately 1 cm of distal clavicle is resected if preoperative evaluation localized significant symptoms to the acromioclavicular joint.
Fig 1.
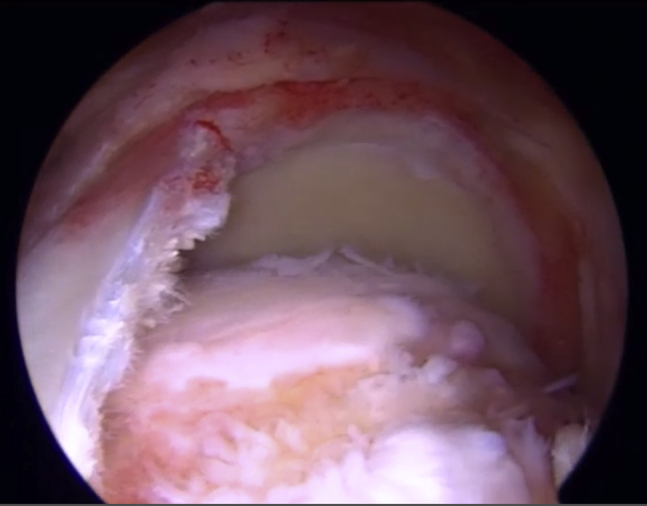
Left shoulder, viewed from the lateral portal in the subacromial space, with the patient in the beach-chair position, showing a massive rotator cuff with retraction of the supraspinatus and infraspinatus tendons. The biceps tendon is intact.
The rotator cuff tendon tear pattern is thoroughly evaluated by pulling lateral traction on the supraspinatus and infraspinatus tendons while viewing from the lateral subacromial portal site. We prefer to assess and repair the rotator cuff tendon using this lateral subacromial portal for viewing because it not only allows for complete visualization of the tear but also provides the ability to see the undersurface of the rotator cuff tear tissue so that the surgeon can appropriately incorporate any undersurface laminated tissue and residual superior capsule into the repair construct. Lateral viewing also improves visualization for release of the glenohumeral joint capsule along with release of any other adhesions that are common in such chronic tears. Capsular release maximizes rotator cuff tissue lateralization and helps to ensure that the rotator cuff tissue can be approximated to the abraded greater tuberosity in a relatively low-tension state (Figs 2 and 3). If, despite thorough mobilization of the rotator cuff tissue, a significant deficit of tissue persists, the quality of the rotator cuff tissue is concerning to us, or we believe that additional tissue would potentially improve the chances for rotator cuff healing, strength of the repair, or stability of the repair construct overall, then the biceps tendon is mobilized and transposed to the superior aspect of the humeral head, where it is subsequently secured to the abraded greater tuberosity using suture anchor–based sutures. The biceps can be easily mobilized by simply releasing the transverse humeral ligament and then using a grasper to transfer the biceps out of the bicipital groove to its new location at the superior humeral head (Fig 4). An arthroscopic shaver (Dyonics; Smith & Nephew, London, England) is used throughout the procedure to perform debridement, to perform capsular and other tissue releases as necessary, and to abrade the greater tuberosity. In the specific case highlighted in Video 1, 2 triple-loaded anchors (Healicoil Reginasorb, 5.5 mm; Smith & Nephew) are placed in the greater tuberosity and used for rotator cuff repair as well as to secure the transposed biceps. Specifically, in Video 1, the biceps is secured to its new location at the greater tuberosity using both circumferential sutures, passed and tied around the biceps tendon, and luggage tag–type sutures placed through the biceps tendon using a lasso-loop technique, as described by Lafosse et al.5 (Fig 5). Subsequently, suture anchor associated sutures are passed through the rotator cuff using a retrograde suture retriever (IDEAL Suture Grasper; DePuy Mitek, Raynham, MA) (Fig 6). A rip-stop configuration for suture passage is used to reattach the anterior portion of the rotator cuff tear to its greater tuberosity in Video 1. Additional sutures are also used to converge the various components of the rotator cuff tissue to each other and to the transposed biceps tendon (Fig 7). In addition, the bio-SCR technique that we have described does not require that the biceps be tenotomized either before or after it has been transposed. The biceps tendon is simply mobilized, transposed, and secured to its new location on the greater tuberosity with no further biceps tendon procedures carried out. The transposed biceps tendon is simply secured to the greater tuberosity and otherwise left intact.
Fig 2.
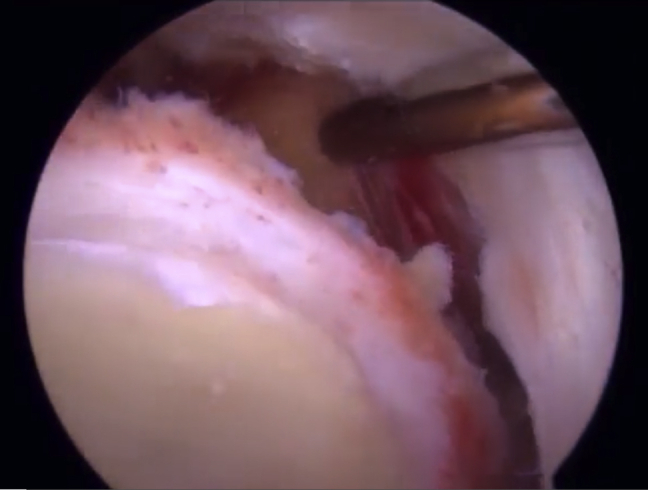
Left shoulder, viewed from the lateral portal, with the patient in the beach-chair position, showing a capsular release to increase tendon lateralization toward the greater tuberosity.
Fig 3.
Left shoulder, viewed from the lateral portal, with the patient in the beach-chair position, showing mobilization of the rotator cuff after medialization of the anatomic footprint.
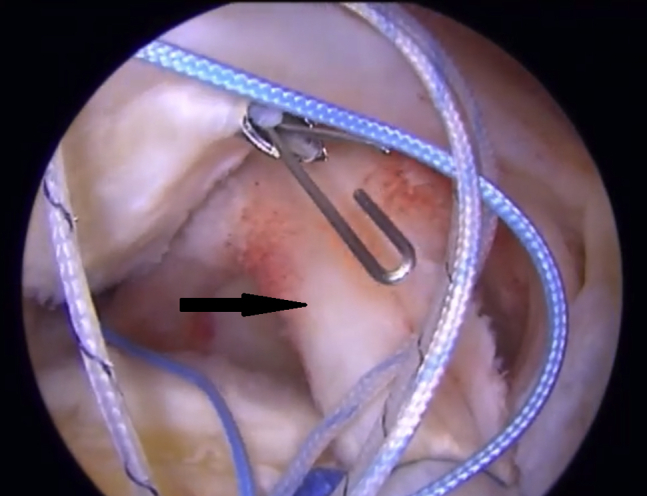
Fig 4.
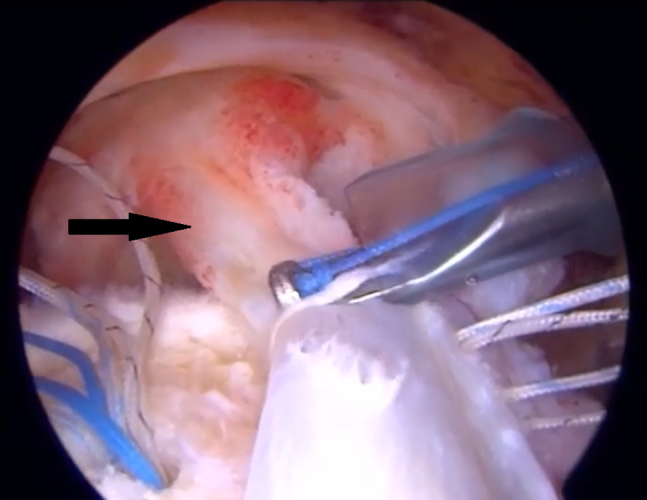
Left shoulder, viewed from the lateral portal, with the patient in the beach-chair position, showing the biceps tendon (arrow) transposed to a more superior position after the transverse humeral ligament is incised.
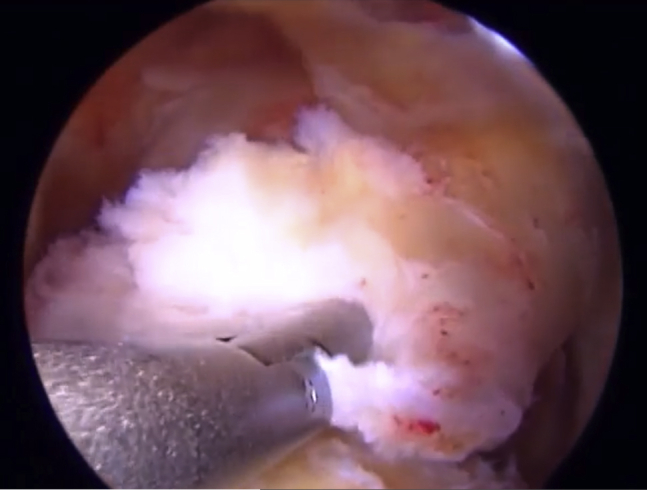
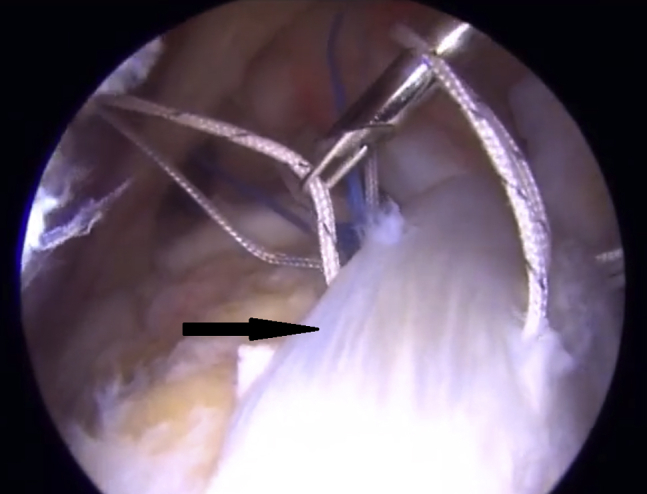
Fig 5.
Left shoulder, viewed from the lateral portal, with the patient in the beach-chair position, showing a luggage tag construct further securing the biceps tendon (arrow) onto the superior aspect of the greater tuberosity.
Fig 6.
Left shoulder, viewed from the lateral portal, with the patient in the beach-chair position, showing suture passage through the rotator cuff tendon (arrow) using a retrograde suture retriever. Below this, the transposed biceps can be seen, which functions as a biological superior capsular reconstruction.
Fig 7.
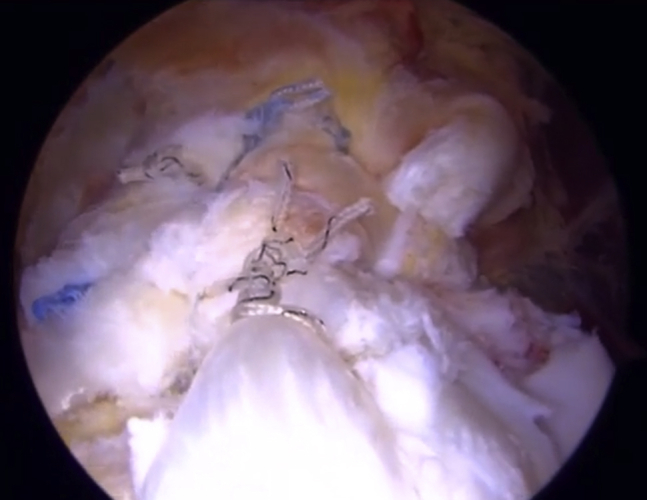
Left shoulder, viewed from the lateral portal, with the patient in the beach-chair position, showing the final repair construct consisting of a rip-stop suture configuration for rotator cuff repair and supplementary biceps tendon transposition.
Our postoperative protocol after bio-SCR biceps transposition and rotator cuff repair is not delayed because of the biceps transposition. Conversely, we believe that because the biceps is very well secured using anchor fixation on the humeral side and owing to the strength of fixation afforded by the native biceps attachment on the glenoid side, a more aggressive rehabilitation progression can often be applied, on a case-by-case basis. Postoperative rehabilitation typically centers on management of the repaired massive rotator cuff tear itself, and its initiation is usually delayed 4 weeks. Once physical therapy is started, passive and active-assisted range-of-motion exercises are begun, subsequently followed by gentle strengthening at 6 to 8 weeks postoperatively. This delay is, in part, based on the time requirements for development of mechanical strength on the basis of ingrowth and remodeling for the graft material used,6 but as mentioned previously, this may not be applicable given the fact that the bio-SCR biceps graft remains viable after transposition and almost certainly heals and incorporates into the repair much more quickly than a free autograft devoid of blood supply or a dermal allograft. At approximately 10 weeks postoperatively, a more functionally progressive rehabilitation regimen is carried out.7,8
Discussion
With the increasing average age of the population, the prevalence of chronic rotator cuff tears increases in tandem. The natural history of these tears leads to consequent, progressive increases in tear size and in fatty atrophy. Although surgeons have an improved understanding of tear progression and use improved techniques to repair chronic and massive rotator cuff tears, some tears are not completely repairable because of retraction and relative immobility. Massive tears such as these may be best managed surgically using either arthroscopic debridement, partial rotator cuff repair, tendon transfer, SCR, or reverse shoulder arthroplasty. Determining the best surgical treatment that is most likely necessary to improve an individual patient's outcome is a difficult and complicated dilemma for the surgeon. Iagulli et al.9 evaluated 97 of the senior author's (L.D.F.) consecutive massive rotator cuff repairs, comparing 45 tears that underwent partial rotator cuff repair with 52 tears that underwent complete repair, and found no differences postoperatively in outcomes between the 2 groups. This finding suggests that partial repair can be effective given proper indications and clinical circumstances but that repairing that rotator cuff tissue that is repairable is likely important toward restoring and preserving function, as initially proposed by Burkhart et al.10 With the biceps tendon in close proximity to the rotator cuff and already anchored to the supraglenoid tubercle, it can be easily transposed to augment the repair of such tears, providing supplemental tissue for these tears with often poor rotator cuff tendon quality and/or mobility. Our bio-SCR technique offers the option of using the biceps tendon to improve the strength and stability of these massive rotator cuff repairs.
There are several potential advantages of using the bio-SCR technique in appropriately indicated cases (Table 1). First, the biceps tendon is autologous tissue in close proximity to and in a similar orientation to the rotator cuff tissue being repaired. The biceps tendon can be easily mobilized, transposed, and incorporated into the rotator cuff repair. Likewise, this transposed tendon provides a static, and potentially dynamic, inferiorly directed force vector that may potentially serve to help maintain glenohumeral joint congruity in such cases because superior humeral head translation is commonly seen and contributes negatively to overall shoulder function. Transposition of the biceps tendon in such clinical situations has been shown clinically to increase the AHD postoperatively.11 Second, the transposed biceps tendon can potentially serve in the role of the superior capsule and, as described by Kim et al.,11 avoids associated remote donor-site morbidity. Third, compared with the operative time required to perform an SCR using either a TFL autograft or an allograft tissue, mobilization and transposition of the LHBT necessitate dramatically less operative time and can be accomplished routinely in less than 5 minutes. Likewise, when the biceps tendon is transposed, it obviates remote autograft harvest or measurement and construction of this autograft tissue. Similarly, use of the biceps eliminates the requirement that an appropriately measured and constructed dermal allograft be fashioned. Moreover, because no additional anchors are usually required when performing this biceps tendon transposition technique, very significant time and expense are saved. In comparison with the more commonly performed and established allograft SCR techniques, dramatic cost savings are possible. Most SCR techniques encourage the use of a minimum of 6 anchors (with even more anchors often recommended), and when the costs of these anchors are added to the cost of the allograft material implanted, very extensive cost savings are possible with our technique. The senior author has used the described bio-SCR technique over 30 times in the past 2 years and has seen no untoward effects believed to be directly attributable to biceps tendon transposition in these patients. Only 1 patient has remarked that he had mild “cramping” develop in the area of the biceps in the first few weeks postoperatively, but this symptom resolved completely by 6 weeks after surgery. Likewise, we have not seen any biceps asymmetry or Popeye deformities in any of these patients postoperatively. Currently, the senior author uses the biceps tendon as the default SCR graft when it is found intraoperatively to be present and reasonably healthy in cases for which an SCR is believed to be indicated or advisable as dictated by both preoperative and intraoperative assessment. Preoperative imaging and clinical examination are valuable in helping to confirm the presence of an intra-articular biceps tendon. Currently, a dermal allograft is used by the senior author to perform SCR only when an acceptable biceps tendon is not available or when the biceps tendon is considered of insufficient size to provide adequate humeral head coverage. However, all patients who may require an SCR are counseled preoperatively regarding both the bio-SCR procedure and the allograft SCR; they provide consent for the allograft SCR in case an acceptable biceps tendon is not available intraoperatively or arthroscopic assessment dictates that a dermal allograft SCR may be better suited to address the pathology. No comparative studies have been published to date related to biceps transposition in this SCR role versus the more commonly used allograft SCR procedure.
Table 1.
Advantages and Disadvantages of LHBT Transposition for SCR
| Advantages |
| The close proximity of the biceps tendon to the rotator cuff tear simplifies transfer and incorporation of the biceps tendon into the rotator cuff repair. |
| The donor-site morbidity associated with TFL autograft is avoided. |
| The operative time for bio-SCR technique is decreased compared with other SCR techniques. |
| The technique potentially provides an effective downward vector to aid in reducing superior head migration. |
| The technique is much less technically demanding and less expensive than allograft SCR. |
| The biceps tendon blood supply is not compromised and remains abundant in tenocytes and fibroblasts, thus likely improving the healing potential of the rotator cuff repair. |
| The technique obviates harvesting remote autograft tissue or using allograft tissue. |
| Disadvantages |
| The technique cannot be used if the LHBT is ruptured or very severely damaged. |
| The effects, if any, related to local biceps symptoms or biceps function have not been fully elucidated to date. |
bio-SCR, biological superior capsular reconstruction; LHBT, long head of biceps tendon; SCR, superior capsular reconstruction; TFL, tensor fascia lata.
It has not been determined what clinical ramifications, if any, there may be when the biceps is transposed to supplement and strengthen the repair of massive rotator cuff tears. Obviously, removing the biceps from its anatomic groove and securing it in a nonanatomic location may potentially have negative consequences. Potentially, however, there may be advantages related to the inferiorly directed force vector that is likely enhanced by transposing the biceps to the superior humeral head. Hopefully, future research will aid in elucidating an inferior humeral head translational effect, if any. Veen et al.12 published a systematic review assessing rotator cuff repairs in patients for whom biceps autograft was used to support the repairs. Of the 8 studies included in their review, 6 showed an improvement in range of motion postoperatively and 5 showed a decrease in reported visual analog scale scores.
The management of massive rotator cuff tears presents a complex clinical dilemma and daunting surgical challenge for the surgeon due, in part, to the limitations in repairability of these tears as a result of intrinsic changes related to poor tendon quality, retraction, and relative immobility. Although SCR procedures using both TFL autograft and dermal allograft have shown promising results, these procedures are highly technically demanding, time-consuming, and expensive to perform. Our bio-SCR technique provides the surgeon with a technically easy, inexpensive alternative that can be quickly carried out in selected patients. Transposition as well as incorporation of the biceps tendon into the rotator cuff repair adds native tissue, rich in live tenocytes and fibroblasts, to the repair. Furthermore, it provides potential biomechanical advantages not only because of the increased strength of the overall rotator cuff repair afforded by incorporation of the stabilized biceps tendon but also because of the ability of the transposed biceps tendon to increase the AHD and thus more concentrically align the glenohumeral joint in patients with superior humeral head migration.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: L.D.F. receives consulting income from Smith & Nephew and research and educational support from Arthrex, Mitek, and Smith & Nephew. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic massive rotator cuff repair is shown using the transposed long head of the biceps tendon as a supplemental graft to produce a biological superior capsular reconstruction. This procedure is performed in a left shoulder with the patient in the beach-chair position.
References
- 1.Bedi A., Dines J., Warren R.F., Dines D.M. Massive tears of the rotator cuff. J Bone Joint Surg Am. 2010;92:1894–1908. doi: 10.2106/JBJS.I.01531. [DOI] [PubMed] [Google Scholar]
- 2.Mihata T., Lee T.Q., Watanabe C. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 3.Han F., Kong C.H., Hasan M.Y., Ramruttun A.K., Kumar V.P. Superior capsular reconstruction for irreparable supraspinatus tendon tears using the long head of the biceps: A biomechanical study on cadavers. Orthop Traumatol Surg Res. 2019;105:257–263. doi: 10.1016/j.otsr.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 4.El-shaar R., Sandeep S., Nicandri G., Maloney M., Voloshin I. Superior capsular reconstruction with a long head of the biceps tendon autograft. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118785365. 2325967118785365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lafosse L., Van Raebroeckx A., Brzoska R. A new technique to improve tissue grip: “The lasso-loop stitch. Arthroscopy. 2006;22:1246.e1–1246.e3. doi: 10.1016/j.arthro.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 6.Adams J.E., Zobitz M.E., Reach J.S., Jr., An K.N., Steinmann S.P. Rotator cuff repair using an acellular dermal matrix graft: An in vivo study in a canine model. Arthroscopy. 2006;22:700–709. doi: 10.1016/j.arthro.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 7.Altintas B., Bradley H., Logan C., Delvecchio B., Anderson N., Millett P.J. Rehabilitation following subscapularis tendon repair. Int J Sports Phys Ther. 2019;14:318–332. [PMC free article] [PubMed] [Google Scholar]
- 8.Thigpen C.A., Shaffer M.A., Gaunt B.W., Leggin B.G., Williams G.R., Wilcox R.B. The American Society of Shoulder and Elbow Therapists’ consensus statement on rehabilitation following arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25:521–535. doi: 10.1016/j.jse.2015.12.018. [DOI] [PubMed] [Google Scholar]
- 9.Iagulli N., Field L., Hobgood E.R., Ramsey J.R., Savoie F. Comparison of partial versus complete arthroscopic repair of massive rotator cuff tears. Am J Sports Med. 2012;40:1022–1026. doi: 10.1177/0363546512438763. [DOI] [PubMed] [Google Scholar]
- 10.Burkhart S.S., Nottage W.M., Ogilvie-Harris D.J., Kohn H.S., Pachelli A. Partial repair of irreparable rotator cuff tears. Arthroscopy. 1994;10:363–370. doi: 10.1016/s0749-8063(05)80186-0. [DOI] [PubMed] [Google Scholar]
- 11.Kim Y.S., Lee H.J., Park I., Sung G.Y., Kim D.J., Kim J.H. Arthroscopic in situ superior capsular reconstruction using the long head of the biceps tendon. Arthrosc Tech. 2018;7:e97–e103. doi: 10.1016/j.eats.2017.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Veen E., Stevens M., Diercks R. Biceps autograft augmentation for rotator cuff repair: A systematic review. Arthroscopy. 2018;34:1297–1305. doi: 10.1016/j.arthro.2017.10.044. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic massive rotator cuff repair is shown using the transposed long head of the biceps tendon as a supplemental graft to produce a biological superior capsular reconstruction. This procedure is performed in a left shoulder with the patient in the beach-chair position.


