Abstract
Here, we review modeling predictions for Covid-19 mortality based on recent data. The Imperial College model trusted by the British Government predicted peak mortalities above 170 deaths per million in the United States, and above 215 deaths per million in Great Britain, after more than 2 months from the outbreak, and a length for the outbreak well above 4 months. These predictions drove the world to adopt harsh distancing measures and forget the concept of herd immunity. China had peak mortalities of less than 0.1 deaths per million after 40 days since first deaths, and an 80-day-long outbreak. Italy, Belgium, the Netherlands, Sweden, or Great Britain flattened the curve at 13.6, 28.6, 9.0, 10.6, and 13.9 deaths per million after 40, 39, 33, 44, and 39 days from first deaths, or 31, 29, 24, 38, and 29 days since the daily confirmed deaths reached 0.1 per million people, respectively. The declining curve is much slower for Italy, the Netherlands, or Great Britain than Belgium or Sweden. Opposite to Great Britain, Italy, or Belgium that enforced a complete lockdown, the Netherlands only adopted an “intelligent” lockdown, and Sweden did not adopt any lockdown. However, they achieved better results. Coupled to new evidence for minimal impact of Covid-19 on the healthy population, with the most part not infected even if challenged, or only mild or asymptomatic if infected, there are many good reasons to question the validity of the specific epidemiological model simulations and the policies they produced. Fewer restrictions on the healthy while better protecting the vulnerable would have been a much better option, permitting more sustainable protection of countries otherwise at risk of second waves as soon as the strict measures are lifted.
Keywords: modeling, infectious diseases, Covid-19, policy
Introduction
Modeling of infectious diseases is usually carried out by using “compartmental models” where a population is divided into compartments. Every individual in the same compartment is supposed to have the same characteristics. These models are used to predict the spreading of a disease, the number of infected or deaths, and the duration of the epidemic. The simplest model, the susceptible, infected, recovered or dead (SIR) model by Kermack and McKendrick is dated 1927.1 In this model, S stands for susceptible, I for infected, and R for recovered. This model describes the number of people infected in a closed population over time. It was proposed to explain the rapid rise and fall in the number of infected patients observed during epidemics. The population size is fixed, the incubation period of infection is instantaneous, the duration of infectivity is the same as the length of the disease. The population is also homogeneous with no age, spatial, or social structure, and no comorbidities. The Kermack and McKendrick model went forgotten for 50 years and only returned popular in 1979.2 The model consists of a system of 3 coupled ordinary differential equations,3
where t is the time, β is the infection rate, and γ is the rate of recovery. The average number of days to recover from infection is
and the basic reproduction number is
R 0 is the key parameter governing the time evolution. It is the number of secondary infections caused by a single primary infection. The “recovered” class is better interpreted as the “removed” class of those who had the disease and have recovered, are immune, or had the disease but were isolated until recovered.4 This model can be modified to include the number of deaths. The death rate can be taken equal to the time rate of change of the number of closed cased R
where γ* is the percentage of deaths in closed cases.
The values of γ*, γ, and β are empirically determined. This is a major issue at the start of a new epidemic, as these numbers are not known with accuracy. Furthermore, mathematics is too simple to be effective.
More complicated versions of this basic SIR model have been developed to better reflect the actual epidemiologic of a given disease. However, they still share the same backbones structure of the original SIR,1 and they still depend on information difficult to have at the start of an epidemic. Because of these downfalls, the most of the studies developed in China after the severe acute respiratory syndrome (SARS) epidemic have been mostly fitting techniques,5 and in a fewer cases SIR models,6,7 stochastic individual-based models,8,9 spatiotemporal models10 autoregressive integrated moving average (ARIMA) models,11 and small-world network models.12 The different approaches still rely on empirical evidence, and to be reliable they should be continuously calibrated through comparison with novel evidence.
Despite not that different from the original SIR model, compartmental models such as13-15 were used to inform policy makers more than 2 months ago and have not been revised, yet despite the novel evidence has demonstrated they were wrong. Here, we review the supporting data, and model performances, for the Covid-19 outbreak, and also discuss efficacy and sustainability of the measures they generated.
Covid-19 Statistic
Covid-19 statistics are available from many sources, for example, from the study by Wordometers.16 Different countries are experiencing different severity of the outbreak and sometimes similar outcomes adopting different distancing approaches. Of relevance for Covid-19 is the age statistic or the statistic of comorbidities.16 The probability of dying if infected by the virus and requiring treatment dramatically increases with age and preexisting medical conditions (comorbidities). For those 0 to 50 years of age without any preexisting conditions, the probability of a fatality following infection is less than 1%.16 Data from South Korea, where there has been the best tracking so far from Covid-19, show that more than 99% of the cases in the general population are mild and do not require any medical treatment. The small percentage of cases that require medical treatment is all among those older than 60 years or with comorbidities. Data from Wuhan, China, show the same pattern. Apart from the vulnerable for age or comorbidities, it is not very likely that Covid-19 will produce fatalities.
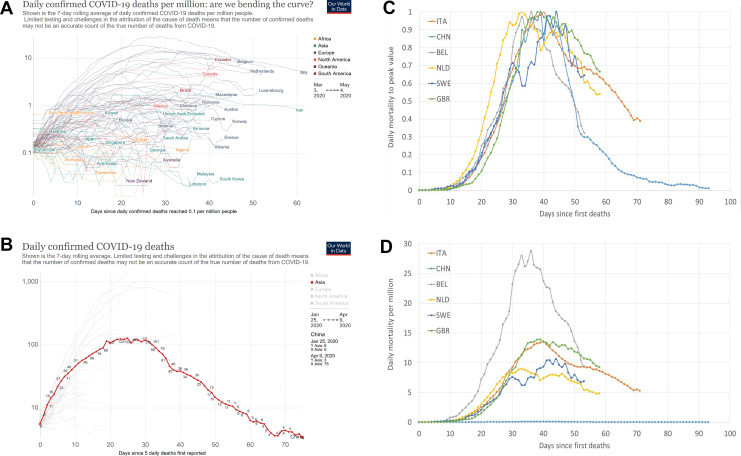
The number of infected is not known with certainty, as testing has been so far very limited, with most of the asymptomatic or mild missing from the statistic. Therefore, it makes sense to focus on the number of deaths. Figure 1 presents in (A) the daily confirmed deaths per million plus in (B) the total mortalities from China, of population 1.5 billion people. Finally, in (C) and (D) is the nondimensional and dimensional daily mortality from China, Italy, Belgium, Great Britain, Sweden, and the Netherlands since daily deaths were first reported. The nondimensional values are normalized versus the peak value. While the infection dynamic for China and Italy has been very different, and similarly very different has been the death rate per million people, the mortality peak has been achieved after the same number of days, with a similar pattern. The total duration of the outbreak in China with more than 5 deaths per day has been 67 days.
Figure 1.
(A) Daily mortalities per million from countries in Europe, the United States, and Canada, plus South Korea, Australia, and Saudi Arabia, (B) total mortalities from China, of population 1.5 billion people. Images reproduced from https://ourworldindata.org/coronavirus-data. C, Nondimensional daily mortalities per million from selected countries since daily deaths were first reported. The values are normalized versus the peak value. D, Daily mortalities per million from the same selected countries since daily deaths were first reported. Data from the European Centers for Disease Control and Prevention (CDC).
China had peak mortalities of less than 0.1 deaths per million after 40 days since first deaths, and an 80-day-long outbreak. Italy has flattened the curve at 13.6 deaths per million after the same 40 days, and the curve is now declining. This is also after 31 days since the daily confirmed deaths reached 0.1 per million people. The declining curve is, however, much slower. Belgium flattened the curve at 28.8 daily deaths per million, after 39 days from first deaths and 29 days since the daily confirmed deaths reached 0.1 per million people. Belgium had a faster growing rate but also a faster declining rate versus Italy. The Netherlands flattened the curve at 9.0 daily deaths per million, after 33 days from first deaths and 24 days since the daily confirmed deaths reached 0.1 per million people. The Netherlands had an even faster growing rate but also a slow declining similar to Italy. Sweden flattened the curve at 10.6 daily deaths per million, after 44 days from first deaths and 38 days since the daily confirmed deaths reached 0.1 per million people. Sweden slows a rapid decline. Finally, Great Britain flattened the curve at 13.9 daily deaths per million, after 39 days from first deaths and 29 days since the daily confirmed deaths reached 0.1 per million people. Great Britain slows a decline much slower Sweden. Opposite to Great Britain, Italy, or Belgium that enforced a complete lockdown, the Netherlands only adopted an “intelligent” lockdown, and Sweden did not adopt any lockdown. However, they achieved better results.
The above number of deaths also has uncertainties. There are many deaths attributed to Covid-19 without any tests performed. The US Centers for Disease Control and Prevention (CDC’s) National Vital Statistics Service’s explicit instructions say, “It is important to emphasize that coronavirus disease 19, or Covid-19, should be reported for all decedents where the disease caused or is presumed to have caused or contributed to death.” Similar instructions are followed in France, Italy, or Spain. Additionally, regarding the mortality rate, the numbers for Europe and the United States are overestimated also because the number of tests performed is insufficient, and most of the asymptomatic and mild infections are missing. Except for the elderly individual, mortality from the virus is very low without an illness.
The outbreak of Covid-19 in China is not certainly definitively closed, as second waves are still possible. Most of the European countries have already achieved some sort of control. To bring the pandemic to an end, countries have to bend the curve to achieve a plateau and then a decline in the number of daily cases. Those who achieved the bending of the curve with harsh distancing and generalized lockdown measures are now fearing the opportunity of second waves when these measures will be lifted. Those who achieved the same or better results through less distancing, do not have this risk.
Belgium and the Netherlands, which are neighboring countries with common many villages that are divided in Belgian and Dutch sides, are one indication that harsh distancing and generalized lockdown does not pay. Belgium adopted much more severe, and the Netherland much less severe, distancing measures. The Netherlands peaked at less than 9 over a million, while Belgium peaked at almost 29 over a million. Saudi Arabia and South Korea are relatively stable at about 0.1 over a million. China had peak mortalities of less than 0.1 deaths per million after 40 days since first deaths, and an 80-day-long outbreak. Italy flattened the curve at about 13 deaths per million after the same 40 days. South Korea did not prevent any basic freedom because of the pandemic and they also regularly run their elections during the outbreak. Thus, it seems the distancing measures exceeding the sustainable and necessary do not pay.
The Covid-19 death rate for the Hubei Province16 computed as total deaths versus total population is 5.35 × 10−5. The Covid-19 death rate for China16 similarly computed is 2.27 × 10−6. Although some more deaths will certainly occur, these numbers should be compared to the US CDC published death rate for the common flu in the United States, that is, 1.85 × 10−4, one order of magnitude larger than the Hubei Covid-19 death rate, and 2 orders of magnitude larger than the China Covid-19 death rate.17 The US CDC17 estimates 9.7 to 45 million cases of common flu per year in between the 330 million US population, with a need for hospitalization for 140 000 to 810 000, and a death toll of 12 000 to 61 000.
Covid-19 Models Predictions
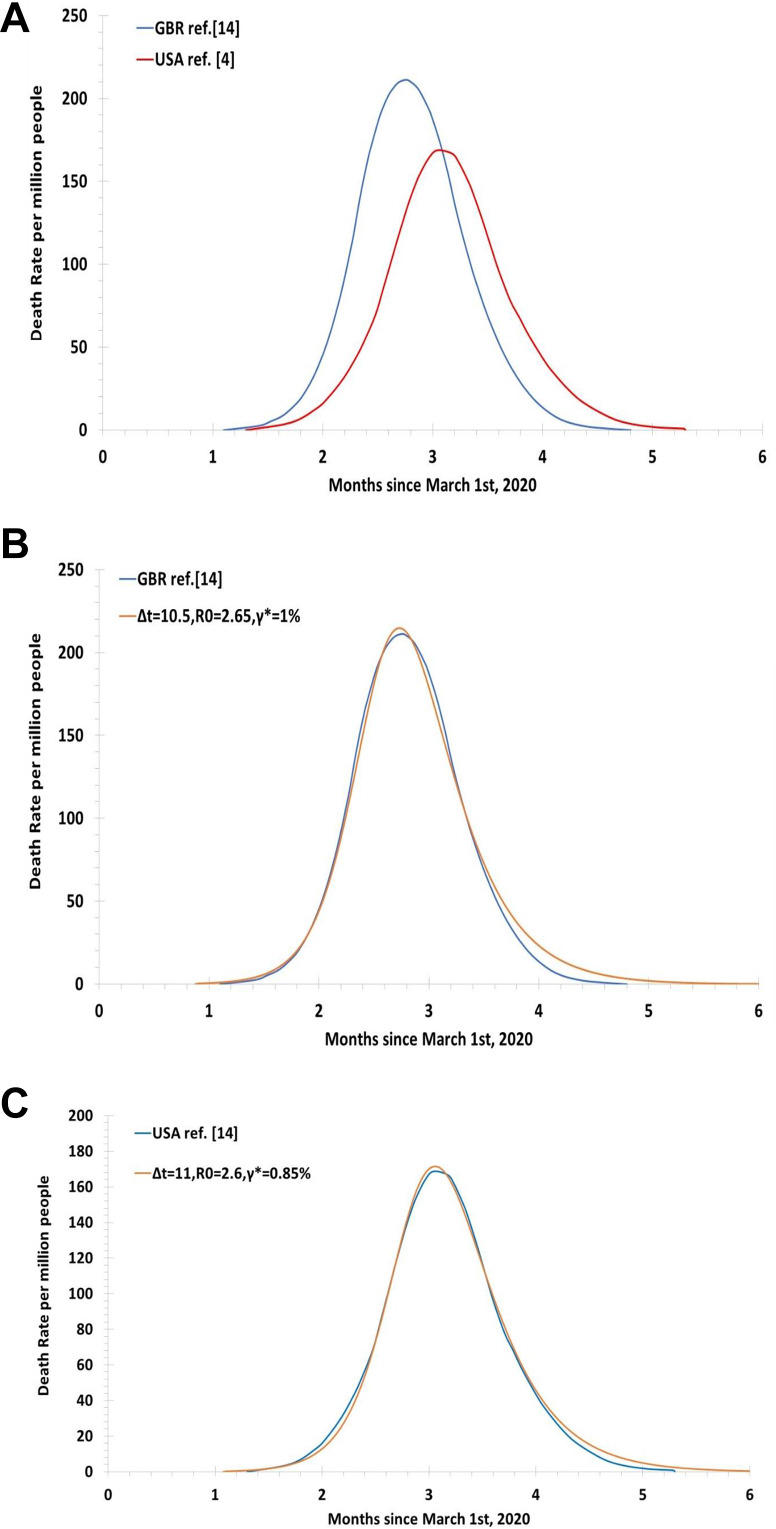
Regarding Covid-19 predictions, according to the US CDC,13 between 160 and 214 million people could be infected only in the United States, and as many as 0.2 to 1.7 million people could die. In all, 1.7 to 330 million people is 5.15 × 10−3. This is roughly 2 orders of magnitude larger than the Hubei experimental death rate, and 3 orders of magnitude larger than the China experimental death rate. British academics are pushing even higher the bar. More than 500 000 deaths in the United Kingdom, and 2.2 million deaths in the United States, were predicted “if the government take no action.”14,15 Figure 2 presents in (A) the computations of the study by Adam and Ferguson et al14,15 and (B) and (C) the comparison of these results with the simple SIR model proposed in the previous section of the listed parameters. More than 4 months of the outbreak are predicted in Great Britain, April, May, June, and July.14,15 Respiratory diseases, including the SARS epidemic, usually remain about 2 months in any given population. The peak of mortality was 21 every 100 000, or 215 per million.14,15 The number of fatalities is extremely worrying. A marginally longer period but with a peak of mortality reduced to 17 every 100 000, or 170 per million, were predicted in the United States.14,15 Also this number of fatalities is extremely worrying.
Figure 2.
A, Computations of the death rate from the study by Adam14 for Great Britain and the United States. Data digitized from the study by Adam and Ferguson et al.14,15 B and C, Comparison of these results with the simple SIR model having the listed parameters.
The US CDC and some British academics thus promoted the view that a large proportion of the population of the United States or Great Britain could only survive through extreme distancing measures, which are much harsher than those adopted in China, Taiwan, South Korea, Japan, the Netherlands, or Sweden, as otherwise there could be 3 orders of magnitude more deaths than China. Not a surprise if-then panicking has been driving the health policy for Covid-19 in Great Britain and the United States.
The source of the information proposed in the work14 is the paper,15 still at the preprint stage, that is, a result that has not passed yet any peer review. Preprint articles have not been finalized by authors, might contain errors, and report information that has not yet been accepted or endorsed in any way by the scientific community. Nevertheless, journalists and policy makers did not consider this aspect, as the work has yet to be evaluated by the scientific community and the information presented may be erroneous. Similarly, they did not consider alternative simulations and do not consider now the opportunity to revise the models.
Models simulating the spreading of diseases are mostly properties of academic groups. These models have similar mathematical principles, sharing the backbones of the SIR model.1 The current compartmental models are more complicated than the SIR model while sharing basic principles. They include additional effects but are reliant on much more empirical evidence to work reasonably well. The latest models need many more assumptions, for example, in some models, it is assumed a perfectly and evenly mixed population, and infected people equally infectious recovery or death. This is rarely the case. Some other models subdivide people into smaller groups by social mixing.14 Apart from the basic modeling assumptions, then the models need information that is impossible to be estimated at the start of an epidemic, such as the mortality rate, or the basic reproduction number R 0 15 estimated that about 0.9% of the infected would die and that R 0 is about 2.6. As discussed later, these numbers appear now overestimated. Because of the lack of adequate testing, those who have been challenged or infected but did not require special care do not appear in the statistic. We simply do not know the details of how many people have been infected with mild symptoms or asymptomatic and have recovered, as nobody is testing for past infections. Similarly, we do not know about immunity,15 subjectively assumed the same incubation time and spreading time, as well as infectivity, in asymptomatic and mild or heavily infected15 and assumed that there is no natural immunity to Covid-19, nor physical barriers to the spreading of the virus.
Models are everything, but detailed representations of the way people behave during a pandemic and are based on many parameters that are simply unknown at the time the simulations are made. If these models fail validation with newly produced evidence, they should be revised.
Although we do not have the code that has been used in the study by Ferguson et al,15 we know about the values of the R 0 and fatality rate used there, which is excessive. Their result is not that far from a simple SIR computation as shown in Figure 2B and C. By using the values of Δt and R 0 plus γ* shown in the images, in the simple SIR model, that is a computation requiring the definition of 4 cells in an excel spreadsheet, the results are close to those of Adam.14
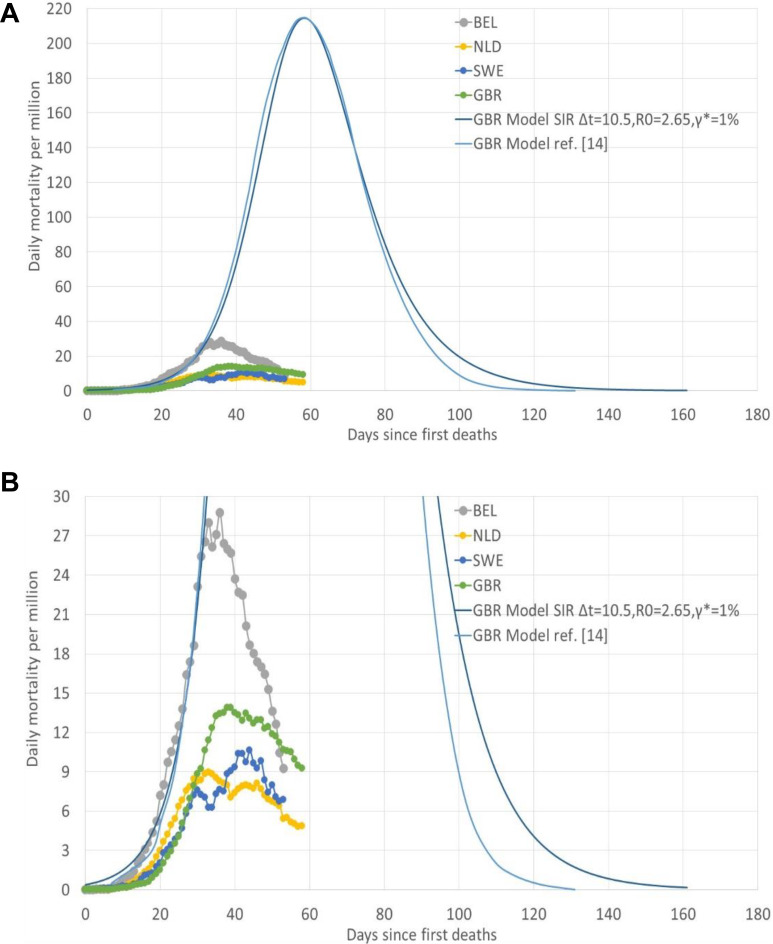
Figure 3 presents a comparison of the predictions14 and the evidence from Sweden, the Netherlands, Belgium, and Great Britain. The difference between modeling and experiments is impressive.
Figure 3.
A and B, Daily mortality rate per million of Belgium, the Netherlands, Sweden, and Great Britain, and comparison with the model predictions14,15 and the SIR simulations of parameters shown.
The work14,15 used the fatality rate from infected fatality rate (IFR), by age group of,18 that unlike,15 published the computer code and data used in the study by Verity et al18,19 based the IFR on incomplete Chinese data from Wuhan of limited statistical significance that was not accounting for asymptomatic or mild infected. Different results suggesting lower IFR by ages were obtained in the study by Levis20 by using the Diamond Princess information, which, however, is still a sample of minimal statistical significance biased by a much larger number of elderly individual or people with comorbidities than the general population. Although the study by Levis20 suggests lower IFR of the study by Ferguson et al15 and Verity et al18 decided to use higher IFR versus15,18 adjusted the IFR estimates of the study by Verity et al18 “to account for a nonuniform attack rate,” without giving further information15 appears to have increased the IFR estimates of the study by Verity et al18 for all 60+ age groups by 19%, without justification. This contributed to an increased, rather than a reduced, total number of fatalities. The Covid-19 models’ predictions15 appear wrong in the dynamic, as they show a pattern very far from the one experienced so far (Figure 1). They propose a result only depending on subjective assumptions not being supported by a proper statistic through a very simple mechanism. Their assumptions were questionable when the simulations were performed. These assumptions are completely wrong after 2 months. Why these simulations have not been revised is an open question.
Herd Immunity
Many models assume a pandemic may be closed only through “herd immunity” and eradication. This rarely happened in human history. It did not happen for SARS or Middle East respiratory syndrome (MERS), as it did not happen for the common flu. Herd immunity is the indirect protection from infectious disease that occurs when a large percentage of a population is immune to an infection. It may be achieved when a large number of people get infected and recover in the healthy population, protecting those who are not immune.21 Individuals with immunity are disruptions in the spread of disease.21 When there is a significant number of disruption, then the infection does not progress. This may be local or global. Eradication is the global herd immunity.
Local herd immunity or eradication through global herd immunity has not been achieved for MERS or SARS. Likely, it will not be achieved also with Covid-19. Nevertheless, the MERS and SARS infections have been placed otherwise under control.
No vaccine has been developed for MERS or SARS and the efficacy of the antivirals proposed for MERS or SARS is at least controversial.
The critical immune proportion of the population, the “herd immunity threshold” (HIT) is according to mathematical models extremely large. This threshold is the product of R 0, the basic reproduction number, and S, the percentage of the population who are susceptible to infection, also equal to 1 − p, where p is the percentage of the immune population.
For SARS, of airborne droplet transmission, it is R 0 = 2-5 and HIT = 0.5-0.8.22
For Ebola, of more controllable bodily fluids transmission, it is R 0 = 1.5-2.5 and HIT = 0.33-0.6.23
For influenza,24 of airborne droplet transmission, it is R 0 = 1.5-1.8 and HIT = 0.33-0.44.
Finally, for Covid-19,25,26 also of airborne droplet transmission, it is R 0 = 1.4-3.9 and HIT = 0.29-0.74. These HIT numbers have not been achieved for SARS and Ebola and will not be achieved with Covid-19. Nevertheless, SARS and Ebola have been controlled. Natural immunity prevents transmission, the same as physical barriers.
Herd immunity through a significant percentage of people who have been infected and has recovered has been briefly considered at the start of this year for Covid-19 and then dropped in the most part of the countries because of the overestimated fatality rate and the neglected large number of immune, mild or asymptomatic.
It is not proven that Sweden has now reached a complete “herd immunity.” Despite no distancing has been enforced, and only the risk categories have been protected, the number of fatalities has reduced any way, in a pattern not dissimilar from other places where more severe distancing measures have been enforced. The available seroprevalence data from Sweden and other countries do not indicate achievement of full “herd immunity” in Sweden better than in other countries. There have been in Sweden only distancing recommendations,27 however effective as evidenced by the decline in the normal rates of influenza and norovirus infections this winter. Sweden has kept large parts of the society open.27 There is no lockdown.27 Also bars are open, as well as street vendors.27 Very little has shut down.27 Use of public transport has dropped naturally, and many work from home. Voluntary social distancing and common sense have been enough to slow the spread of the virus.27 Only gatherings of more than 50 people are banned and visits to elderly care homes. This is very different from being forced at home with permission only to queue for buying groceries or drugs during the few hours in a day permitted by curfews.
A verdict of “herd immunity” is impossible as we do not know (1) what it would take to reach HITs, (2) what those thresholds are, (3) how protective are antibodies, (4) how long antibodies (and presumed immunity) last, and (5) how possible is it for some with antibodies to infect others. These points will have to be investigated carefully.
“Herd immunity” through mass vaccination is unlikely to be practical. The time frame to properly develop a vaccine is long, and the result is uncertain. Near past experiences for SARS28 and MERS29 close relatives of Covid-19 have not been successful. Severe acute respiratory syndrome first emerged in China’s Guangdong Province in 2003 before spreading to other countries. The virus infected about 8000 people, claimed almost 800 lives worldwide. Middle East respiratory syndrome was first reported in Saudi Arabia in 2012 and has since spread to several other countries. About 2500 cases have been reported as of January 2020, with more than 800 deaths worldwide. The SARS outbreak ended before the vaccines were ready. After 5 years from the SARS outbreak, in 2008,30 despite vaccine candidates were more successful for this specific coronavirus than for other coronaviruses, efficacy and safety evaluation in humans were still to be started.30 There are presently (2020) only 2 veterinary vaccines in use against coronaviruses. Their efficacy is controversial. As reported in the study by Roper and Rehm,31 “vaccinated animals still display significant disease upon challenge.” As written in the study by Saif,32 “Unfortunately, despite long-term efforts, effective vaccines to prevent enteric CoV infections remain elusive.” Similarly, the MERS coronavirus outbreak is ongoing since 2012. As stated in the study by World Health Organization29 at the end of 2019, no vaccine (or specific treatment) for MERS is currently available.
In case of the “Spanish flu,” the outbreak occurred during the spring of 1918. Over several years, it infected almost 500 million people, one-third of the global population, producing about 50 million deaths.33,34 These numbers are controversial, as other figures are often proposed for the fatalities, both lower and higher. Herd immunity was not achieved after the first wave. The second wave that started in August 1918 was more deadly than the first wave. This was probably because of a mutation of the virus. Opposite to the first wave that killed mostly elderly people, the second wave mostly killed young people. Third and fourth waves then occurred in 1919 and 1920. Then, the lethality of the epidemic rapidly declined. This was because of improved therapies to tackle pneumonia or because of a reduced lethality of the further mutated virus35 or both. With much less than the fatality of the “Spanish flu,” the Covid-19 pandemic may have a similar pattern of outbreak and subsequent waves.
Discussion
In between the very recent updates of a Covid-19 statistic changing almost daily, we must mention 2 important works by a group in Stanford36 and the Oxford Covid-19 evidence center.37 Initial estimations of the mortality rate were extremely large, at about 1% of the infected in the simulations here discussed. The recent work,36 the first investigating the number of those with Covid-19 antibodies in the supposed to be unaffected population, has shown a significant amount of people asymptomatic or mild that did not notice to be infected by the virus. Taking them into account,36 revised the Covid-19 mortality rate at 0.12% to 0.20%. Similar values are now proposed by the Oxford Covid-19 evidence center.37 Their IFR for Covid-19 is somewhere between 0.1% and 0.36% where the higher numbers are suggested by the less complete and significant data sets. The mortality rate of Covid-19 is thus much closer to the normal flu, 0.095%, than the 1% of the modeling studies.
The other relevant aspect of Covid-19 infection from37 is that most part of the fatalities is in between those vulnerable for age or comorbidities, with age and death risk profile very closely related to normal mortality. The world largest peak in the daily death rate was about 29 for Belgium. The neighboring Netherlands had a peak daily death rate of less than 9 despite the less restrictive distancing measures. Other countries without contact bans, such as South Korea and Sweden, have not certainly experienced more negative outcomes. Up to 60% of all Covid-19-related deaths in Italy have occurred in the particularly vulnerable nursing homes that were not protected from infection. France, Spain, or Great Britain also had large mortalities from nursing homes. Panicking and lockdown measure is one cause of the large mortality for Northern Italy, producing the collapse in the care of the elderly individual.
There has been another important fact to mention, the Charles de Gaulle aircraft carrier. Of almost 2000 healthy people on board, all uniformly exposed to the Covid-19 virus (no distancing was possible with small common quarters and small common working rooms), only 1081 got infected.38 Of the 1081, only 24 ended up in hospital, 1057 being mild or asymptomatic.38 After 10 days, only 5 of the 23 are still in hospital.39 This suggests that many are immune and many are mild or asymptomatic within the healthy population, and only a very small number needs medical attention. This further supports the approach of Sweden to only limit contacts for the vulnerable, apart from reasonable and sustainable distancing for the healthy population.
“Intelligent” lockdown as in the Netherlands also worked much better than the lockdown of Great Britain or Belgium. Sweden did much better without any lockdown. Sweden will have no issue reopening shops or schools, as shops and schools never closed. Also the Netherlands will have a less problematic return to normality than Great Britain or Belgium, facing serious challenges removing the distancing measures.
Regarding the length of the outbreak, extreme social distancing can make much longer the outbreak and it may also cost more lives.40 This is the exact opposite of what was depicted based on the models.14,15 Even if the data for a proper comparison are missing, there is the suspicious that common sense and suggested distancing measures while keeping open shops and business are working better than the complete lockdowns. The seroprevalence is higher in New York City than in Sweden, despite near total lockdown in New York City.
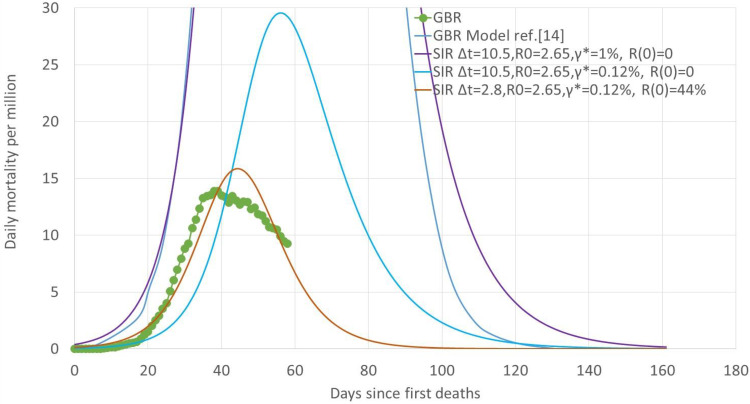
There are simply no data to understand the share of the population that has been exposed but is immune, or the share of the population that only had mild or no symptoms, in the countries we considered. The only further considerations that can be made are through application of the SIR model. Figure 4 presents the daily mortality rate per million of Great Britain, and comparison with the model predictions14,15 and the SIR simulations of the parameters shown. To obtain a result similar to the study by Adam and Ferguson et al,14,15 it is necessary to use Δt = 10.5, γ* = 1%, while R 0 = 2.65 and R(0) = 0 (all the population subjected to infection). By simply correcting for the fatality rate γ* = 0.12%, the curve obtained is still very far from the experimental evidence. To obtain a much closer pattern, while keeping R 0 unaltered, it is necessary to use not only much smaller values of Δt (Δt = 2.8) but also a large initial percentage of removed R(0) (R(0) = 44%). The percentage of removed includes those that are immune and those who have been prevented from being challenged by the virus. The initial percentage of removed is similarly large also to match the experimental evidence for Belgium, the Netherlands, and Sweden (Figure 3A and B). Within the limits of a model that is not adequate, this suggests that the restrictive measure may only increase the fatality rate, protecting less the vulnerable, but producing a similar or even larger percentage of infected. Difficult to factor, is the “panic effect,” that may also bias upward the fatality rate, and the effect of the different therapeutic approaches or care for those hospitalized.
Figure 4.
Daily mortality rate per million of Great Britain and comparison with the model predictions14,15 and the SIR simulations of parameters.
With a mortality rate at about 0.1%, a rapid natural immunization of the general population, while protecting the vulnerable, the elderly individual and those sick, would have been a better choice. Wrong models suggested the opposite. Once the damages to society and economy are factored, the non-necessary segregation measures may claim more lives than the virus itself.
Despite Covid-19, very likely China will have this year, because of distancing, fewer fatalities for common flu plus Covid-19, than the fatalities for the common flu from the year before. Very likely, at the end of the first outbreak, the total number of deaths in the United States for Covid-19 will be much less than the prediction by the CDC, with or without harsh distancing. For similarity with the epidemic evolution in Europe (Figure 1), it was possible to forecast on April 20 for the United States a peak in the mortality rate about the beginning of May, at the most about 12 deaths per million, and duration of the outbreak above 2 months, for a total number of fatalities about 160,000. This is roughly what happened, even if the number of fatalities has been inflated by the attributing in some areas, for example, New York City, every death to Covid-19 by default, without any test, even if occurred for other morbidities. This mortality estimate does not consider the option of a short-term second wave, that is, a problem when flattening the curve is obtained through harsh distancing extended to every sector of the population, the healthy same of the risk categories.
The simulations that are driving the world’s response to Covid-19 are exaggerated. New epidemiological models must be developed to better represent the experimental evidence. The epidemic in Asia seems under control, and in continental Europe, the numbers of deaths as well as infections are both reducing. It is time to revise the models. Models should be continuously updated and validated country by country to match the experimental evidence, to provide reliable advice to policy makers. Science is a dialogue with nature, not a monologue, as theoreticians (and some governments) prefer to believe.41
Epidemiologic models do not account for therapies, in that opposite can make a significant difference in the mortality rate. Therapeutic changes and more general improvements in the health care response may change model parameters during an epidemic. They also do not account for viral mutations, that unfortunately in some cases such as the Spanish flu, were extremely negative from the first to the second wave during 1918.
The review of the simulations driving the Covid-19 response is in principle not unique. Both the popular media and the peer-reviewed literature have covered the subject. For example, the denominator inflation is already reported in the study by Li et al.42 The focus is on the specific compartmental model,14,15 that is basically a simple SIR model, because these have been the simulations that drove the Covid-19 harsh distancing in Europe. These models are not the universe of models being used for epidemiological analysis. They often form the base for more complex models. For example, the US CDC track a set of 10 models43: The Los Alamos model, for example, uses a rate-changing exponential and assumes underestimation of the total cases. The statistical accuracy of the Covid-19 daily death rates prediction is also considered in the study by Marchant et al.44
It has already been discussed as most of the studies developed in China after the SARS epidemic5 have been mostly fitting techniques, and only in a fewer cases SIR models,6,7 plus stochastic individual-based models,8,9 spatiotemporal models,10 ARIMA models,11 and small-world network models.12 The novelty here is having shown as the specific simulations14,15 that drove the world to lockdown are nothing more than a 3-equation 2-parameter SIR model with one further assumption for fatality.
An additional novelty of this contribution is the claim that simulations do not help if not revised continuously with good data. Science is a dialogue with nature and not a monologue. The weakness of the simulations14,15 is the lack of experimental support. Static simulations do not help with evolving epidemics. Only artificial intelligence-based approaches properly supported by continuously updated experimental evidence should be used to support policies.
The other novelty here is the criticism of the policy inferred from the simulations.14,15 Sweden or the Netherlands should have had a huge number of fatalities versus Great Britain or Belgium. It has been exactly the opposite. The peak daily mortality rate has been achieved after about same number of days, and the value per million has been much lower in Sweden and the Netherlands rather than Belgium or Great Britain. With sustainable distancing is more logic to expect a progress toward herd immunity, and the solution is more stable. With harsh distancing, short-term second waves are much more likely to follow.
The article also makes a good case that many CDC have introduced errors into the counts of Covid-19 deaths. The focusing on testing also has been misleading. The relevance on contact tracking for this type of disease also is questionable. The general public is confused and no wonder since the advice from public health experts does not match what most people see in their communities: In the United States, there are few if any deaths in many counties, empty hospitals, deaths that are mostly very sick people in nursing homes. Mainstream media plays up cases of younger healthy people, but they seem to be very rare. Something is very wrong with the claims by experts that guide the policies of many countries. Many nations prepared for a pandemic that did not reach most communities. It also appears that perhaps 25% of the population of many countries had or has Covid-19, but was not sick enough to notice. If so, then the true case fatality rate is very low.
Limitations of the Study
The present work is limited by the quality of the data available. As testing has been very limited and often unreliable, there is no information yet about the number of challenged and infected mild or asymptomatic. This is the reason why the article has been focused on the number of deaths. This number also has dramatic biases upward, especially in some European countries and the United States, where it has been explicitly requested by the CDC to write Covid19 in the death certificate “for all decedents where the disease caused or is presumed to have caused or contributed to death.” This has produced the attribution to Covid-19 of mortalities that were triggered by other pathologies. Worth to mention is also the collapse in the care of the elderly individual because of panicking and lockdowns that has resulted in a much larger number of fatalities. Also the questionable overuse of intubation and similarly inappropriate therapies is believed to have contributed to larger mortalities.
Conclusions
Experiences with past infections, from SARS to MERS, demonstrated that the current mathematical tools to predict outcomes for viral infections are likely wrong at the beginning of the pandemics, simply because the relevant parameters are largely overestimated in the first phase of the outbreaks. Experiences with Covid-19 also prove mathematical tools were wrong also for this viral infection. This means that there is an urgent need to improve them. There is a need for real-time good information, to make statistical samples reliable and permit real-time model validation and refinement.
Continuous update is the key to success. Epidemiologic models should not be proposed at the beginning of an epidemic and never be updated, no matter which is the real-world response to the pandemic. As soon as new information is made available, models should always be updated. Computations failing experimental confirmation are not science. For sure, they are not “the best science.” Similar to model predictions, also polices should be revised as soon as much different epidemiologic patterns become clear.
One major issue with Covid-19 harsh distancing policies of individual countries is the plan to return to normality. In addition to the problem of reopening shops and business within a country, there is the problem of international movements. Although sealed borders cannot certainly go on forever, a strengthening of the control of the movement will be certainly necessary after the first wave of the outbreak will be over, to avoid other waves from imported cases. Generalized lockdown or exposure of the healthy population to flatten the curve will make a significant difference.
There was no scientific reason to overrate model predictions and vilify not only herd immunity approaches45 but also “intelligent” lockdown,46 to support everything but sustainable harsh distancing.
Clearly, models need to be adjusted and we can see a pretty consistent story about flattening of the death rate and at rates much lower than had been feared and estimated. About same results have been obtained with harsh distancing or more intelligent measures. The difference will be enormous in the months to come. With harsh distancing, the total duration of the outbreak will be extended, there will be always the risk of second waves whether imported or domestic, more lives will be lost while damaging democracy, society, and economy.
Additional to the need for continuous real-time update of modeling predictions and policies during a pandemic, the other major conclusion of this work is the implications of the much lower fatality rates, and the large number of not infected, mild, or asymptomatic in the healthy population, that suggest reconsideration of the herd immunity concept for public health policy. The vulnerable must be protected. The healthy must be left free to conduct their business while only adopting reasonable measure. However, although herd immunity is appealing, we may nevertheless have to live with the Covid-19 virus and mutations without herd immunity. Here, much more sustainable approaches as the one of Sweden will definitively provide better results.
Author Biography
Alberto Boretti received his MSc in Engineering in 1984 and his PhD also in Engineering in 1988. He has been working for about 2 decades in industry as researcher and manager, and about 2 decades in the university, as senior research fellow, associate professor and professor. He is the author of about 550 works, Subjects are Engineering, Environmental Science, Energy, Mathematics, Physics and Astronomy, Chemical Engineering, Computer Science, Earth and Planetary Sciences, Agricultural and Biological Sciences, and Materials Science, Medicine, Multidisciplinary, Biochemistry, Genetics and Molecular Biology, Social Sciences, Nursing, Chemistry, Health Professions and Arts and Humanities.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Alberto Boretti  https://orcid.org/0000-0002-3374-0238
https://orcid.org/0000-0002-3374-0238
References
- 1. Kermack WO, McKendrick AG. A contribution to the mathematical theory of epidemics. Proc R Soc Lond Ser A. 1927;115(772):700–721. [Google Scholar]
- 2. Anderson RM, May RM. Population biology of infectious diseases: part I. Nature. 1979;280(5721):361–367. [DOI] [PubMed] [Google Scholar]
- 3. Smith D, Moore L. The SIR model for spread of disease: the differential equation model. Convergence. 2004. www.maa.org/press/periodicals/loci/joma/the-sir-model-for-spread-of-disease-the-differential-equation-model. Accessed April 29, 2020.
- 4. Murray JD. Mathematical Biology: I. An Introduction (Vol. 17). Springer Science & Business Media; 2007. [Google Scholar]
- 5. Han XN, De Vlas SJ, Fang LQ, Feng D, Cao WC, Habbema JDF. Mathematical modelling of SARS and other infectious diseases in China: a review. Trop Med Int Health. 2009;14(suppl 1):92–100. [DOI] [PubMed] [Google Scholar]
- 6. Anderson RM, Anderson B, May RM. Infectious Diseases of Humans: Dynamics and Control. Oxford University Press, 1992. [Google Scholar]
- 7. Diekmann O, Heesterbeek JAP. Mathematical Epidemiology of Infectious Diseases: Model Building, Analysis and Interpretation. John Wiley and Sons, 2000. [Google Scholar]
- 8. Ferguson NM, Cummings DA, Cauchemez S, et al. Strategies for containing an emerging influenza pandemic in Southeast Asia. Nature. 2005;437(7056):209–214. [DOI] [PubMed] [Google Scholar]
- 9. Longini IM, Jr, Nizam A, Xu S, et al. Containing pandemic influenza at the source. Science. 2005;309(5737):1083–1087. [DOI] [PubMed] [Google Scholar]
- 10. Li M, Shi X, Li X, Ma W, He J, Liu T. Epidemic forest: a spatiotemporal model for communicable diseases. Ann Am Assoc Geograph. 2019;109(3):812–836. [Google Scholar]
- 11. Earnest A, Chen MI, Ng D, Sin LY. Using autoregressive integrated moving average (ARIMA) models to predict and monitor the number of beds occupied during a SARS outbreak in a tertiary hospital in Singapore. BMC Health Serv Res. 2005;5(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Watts DJ, Strogatz SH. Collective dynamics of ‘small-world’ networks. Nature. 1998;393(6684):440–442. [DOI] [PubMed] [Google Scholar]
- 13. Fink S. Worst-case estimates for U.S. coronavirus deaths. 2020. www.nytimes.com/2020/03/13/us/coronavirus-deaths-estimate.html. Accessed April 29, 2020.
- 14. Adam D. Special report: the simulations driving the world’s response to COVID-19 how epidemiologists rushed to model the coronavirus pandemic. Nature. 2020;580:316–318. www.nature.com/articles/d41586-020-01003-6 [DOI] [PubMed] [Google Scholar]
- 15. Ferguson NM, Laydon D, Nedjati-Gilani G, et al. Report 9: Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand. Preprint at Spiral 2020. doi:10.25561/77482 [DOI] [PMC free article] [PubMed]
- 16. Wordometers. Coronavirus age sex demographics. 2020. www.worldometers.info/coronavirus/coronavirus-age-sex-demographics/. Accessed April 29, 2020.
- 17. US Centers for Disease Control and Prevention. Flu. 2020. www.cdc.gov/flu/about/burden/index.html
- 18. Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of COVID-19 disease. Preprint at medRxiv; 2020. www.medrxiv.org/content/10.1101/2020.03.09.20033357v1
- 19. Verity R, Okell LC, Dorigatti I, et al. COVID19_CFR_submission. Github 2020. github.com/mrc-ide/COVID19_CFR_submission
- 20. Levis N. COVID-19: updated data implies that UK modelling hugely overestimates the expected death rates from infection. 2020. judithcurry.com/2020/03/25/covid-19-updated-data-implies-that-uk-modelling-hugely-overestimates-the-expected-death-rates-from-infection/#_edn3. Accessed April 29, 2020.
- 21. Fine P, Eames K, Heymann DL. . “Herd immunity”: a rough guide. Clin Infect Dis. 2011;52(7);911–916. [DOI] [PubMed] [Google Scholar]
- 22. Wallinga J, Teunis P. Different epidemic curves for severe acute respiratory syndrome reveal similar impacts of control measures. Am J Epidemiol. 2004;160(6):509–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Althaus CL. Estimating the reproduction number of Ebola virus (EBOV) during the 2014 outbreak in West Africa. PLoS Curr. 2014;6 doi:10.1371/currents.outbreaks.91afb5e0f279e7f29e7056095255b288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Biggerstaff M, Cauchemez S, Reed C, Gambhir M, Finelli L. Estimates of the reproduction number for seasonal, pandemic, and zoonotic influenza: a systematic review of the literature. BMC Infect Dis. 2014;14(1):480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi:10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Riou J, Althaus CL. Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020. Eurosurveillance. 2020. doi:10.2807/1560-7917.ES.2020.25.4.2000058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Savage M. Coronavirus: has Sweden got its science right? 2020. www.bbc.com/news/world-europe-52395866. Accessed April 29, 2020.
- 28. World Health Organization. SARS (severe acute respiratory syndrome). 2019. www.who.int/ith/diseases/sars/en/. Accessed April 29, 2020.
- 29. World Health Organization. Middle East respiratory syndrome coronavirus (MERS-CoV). 2019. www.who.int/news-room/q-a-detail/middle-east-respiratory-syndrome-coronavirus-(mers-cov). Accessed April 29, 2020.
- 30. Enjuanes L, DeDiego ML, Álvarez E, Deming D, Sheahan T, Baric R. Vaccines to prevent severe acute respiratory syndrome coronavirus-induced disease. Virus Res. 2008;133(1):45–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Roper RL, Rehm KE. SARS vaccines: where are we? Expert Rev Vaccines. 2009;8(7):887–898. www.medscape.com/viewarticle/706717_1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Saif LJ. Animal coronavirus vaccines: lessons for SARS. Dev Biol. 2004;119:129–140. [PubMed] [Google Scholar]
- 33. Taubenberger JK, Morens DM. 1918 influenza: the mother of all pandemics. Emerg Infect Dis. 2006;12(1):15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Johnson NP, Mueller J. Updating the accounts: global mortality of the 1918-1920 “Spanish” influenza pandemic”. Bull Hist Med. 2002;76(1):105–115. [DOI] [PubMed] [Google Scholar]
- 35. Barry JM. The site of origin of the 1918 influenza pandemic and its public health implications. J Transl Med. 2004;2(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bendavid E, Mulaney B, Sood N, et al. COVID-19 antibody seroprevalence in Santa Clara County, California. 2020. www.medrxiv.org/content/10.1101/2020.04.14.20062463v1.full.pdf. Accessed April 29, 2020. [DOI] [PMC free article] [PubMed]
- 37. Oke J, Heneghan C. Oxford Covid19 evidence center (Updated 20 April 2020). 2020. www.cebm.net/covid-19/global-covid-19-case-fatality-rates/
- 38. Sinkins JD. French carrier surpasses Theodore Roosevelt with over 1,000 confirmed cases of COVID-19. 2020. www.navytimes.com/news/your-navy/2020/04/20/french-carrier-surpasses-theodore-roosevelt-with-over-1000-confirmed-cases-of-covid-19/
- 39. Cei M. Coronavirus sur le « Charles de Gaulle »: Cinq marins toujours hospitalisés, le porte-avions totalement désinfecté. 2020. www.20minutes.fr/societe/2770163-20200429-coronavirus-bord-charles-gaulle-cinq-marins-toujours-hospitalises-porte-totalement-desinfecte. Accessed April 29, 2020.
- 40. Kulldorf M. Delaying herd immunity is costing lives. 2020. www.spiked-online.com/2020/04/29/delaying-herd-immunity-is-costing-lives/. Accessed April 29, 2020.
- 41. Loab A. Theoretical physics is pointless without experimental tests. 2018. blogs.scientificamerican.com/observations/theoretical-physics-is-pointless-without-experimental-tests/. Accessed April 29, 2020.
- 42. Li D, Lv J, Botwin G, et al. Estimating the scale of COVID-19 epidemic in the United States: simulations based on air traffic directly from Wuhan, China. 2020. www.medrxiv.org/content/10.1101/2020.03.06.20031880v1
- 43. US Centers for Disease Control and Prevention. Why forecasting COVID-19 deaths in the US is critical. 2020. www.cdc.gov/coronavirus/2019-ncov/covid-data/forecasting-us.html. Accessed April 29, 2020.
- 44. Marchant R, Samia NI, Rosen O, Tanner MA, Cripps S. Learning as We Go: an examination of the statistical accuracy of COVID19 daily death count predictions. arXiv preprint 2020 arXiv:2004.04734.
- 45. Savage M. Lockdown, what lockdown? Sweden’s unusual response to coronavirus. 2020. www.bbc.com/news/world-europe-52076293. Accessed April 29, 2020.
- 46. Holligan A. Coronavirus: why Dutch lockdown may be a high-risk strategy. 2020. www.bbc.com/news/world-europe-52135814. Accessed April 29, 2020.