COVID-19 pandemic presented as a black swan event, and as a measure to curtail it the governments of different countries took various approaches (Tandon, 2020). However, most countries announced complete lockdown, with draconian travel and social restrictions. On March 24, 2020, the Government of India ordered a nationwide lockdown for 21 days, limiting movement of the entire population of 1.3 billion.
Though this was probably a requisite, even short term lockdowns, quarantine and social distancing can precede long term effects such as symptoms of mental stress and disorder, including insomnia, anxiety, depression, and post-traumatic stress symptoms (Wang et al., 2020; Brooks et al., 2020). Although there is a deluge of studies published regarding COVID-19, there is a paucity of published data regarding the mental health status of the general population.
Therefore the present survey was intended to assess the mental health impact of the current lockdown on the population of New Delhi, India, a week after its imposition to assist the government agencies and healthcare professionals in safeguarding the mental health wellbeing of the community.
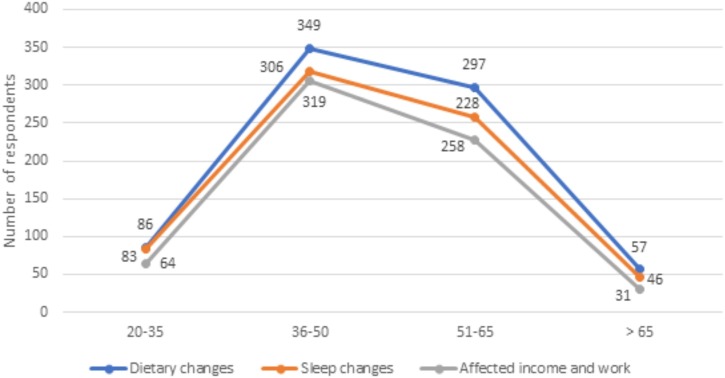
After reviewing the pertinent literature which included scales such as, Impact of Event Scale - Revised (IES-R), Perceived stress scale 10 (PSS-10), and the international guidelines, a self administered, pre-validated web-based questionnaire with 18 questions in English, exploring age and domains of knowledge about COVID-19, understanding reasons for lockdown, stressors which included fear of infection, helplessness and boredom, scarce supplies, and post quarantine stressors related to work, finances and stigma was floated on a famous social media site, Facebook (groups from New Delhi). Those who accepted the invitation and confirmed they were residents of New Delhi, were above 20 years of age and had a minimum graduate level education received the questionnaire. The study population consisted of 992 participants (out of the 2876 invited) of which 11.2 % were aged between 21–35 years, 46.3 % between 36−50 years, 6.5 % were over 65 years of age and the remaining 35 % were between 51–65 years. Ethical clearance and consent were obtained for the same. The data was subjected to statistical analysis using SPSS 20.0. Shapiro-Wilk test indicated the data to be normally distributed. Results were segregated based on the variable of age and domains that indicated significant association with age have been highlighted in Table 1 (p < 0.05). Chi-square indicated significant associations were observed between age groups and the multivariate variables of knowledge about COVID-19, effects of COVID-19 on humankind and how the participants felt about the present situation. Of the bivariate variables, significant association of age was noted with effects on work and income with sleep and diet pattern changes (Graph 1 ).
Table 1.
Descriptive statistics for various domains.
| Questions and possible responses |
20−35 (n = 117) |
36−50 (n = 460) |
51−65 (n = 350) |
>65 (n = 65) |
Total (%) | |
|---|---|---|---|---|---|---|
| Family members | 1 | 21 | 19 | 14 | 4 | 58 (5.8) |
| 2−3 | 47 | 164 | 110 | 39 | 360 (36.2) | |
| 3−6 | 30 | 192 | 174 | 12 | 408 (41.3) | |
| >6 | 19 | 85 | 52 | 10 | 166 (16.7) | |
| Knowledge of covid-19* | Serious disease affecting all age group | 101 | 433 | 326 | 56 | 916 (92.3) |
| Serious disease affecting only the elderly | 11 | 13 | 11 | 4 | 39 (3.9) | |
| Just another kind of flu like swine flu | 2 | 9 | 5 | 4 | 20 (2.1) | |
| Seasonal flu | 1 | 1 | 1 | 1 | 4 (0.4) | |
| Other | 2 | 4 | 7 | 0 | 13 (1.3) | |
| Heard about similar pandemic | Yes | 49 | 186 | 151 | 23 | 409 (41.2) |
| No | 55 | 236 | 168 | 38 | 497 (50.3) | |
| Maybe | 13 | 38 | 31 | 4 | 86 (8.6) | |
| Effects on mankind* | It will lead to loss of human life | 61 | 288 | 212 | 36 | 597 (60.2) |
| Bring worldwide economic slowdown | 35 | 123 | 115 | 23 | 296 (29.8) | |
| Just a hype has been created through social media | 7 | 6 | 2 | 3 | 18 (1.9) | |
| Will pass like any other disease | 13 | 28 | 10 | 3 | 54 (5.5) | |
| It will have multiple effects, including global slow &down and mortality | 0 | 1 | 0 | 0 | 1 (0.1) | |
| It will pass but only after giving a permanent scar on the whole &human community | 1 | 0 | 0 | 0 | 1 (0.1) | |
| Financial and human loss | 0 | 1 | 0 | 0 | 1 (0.1) | |
| Others | 0 | 13 | 11 | 0 | 24 (2.3) | |
| Meaning of Social distancing/isolation | Abstaining /staying away from people | 114 | 455 | 347 | 62 | 968 (97.5) |
| Abstaining from social media | 3 | 5 | 3 | 3 | 14 (2.5) | |
| Are you practising Social distancing/isolation | Yes | 113 | 452 | 345 | 64 | 974 (98.2) |
| No | 4 | 8 | 5 | 1 | 18 (1.8) | |
| Feeling about present situation* | Feeling optimistic, together we can fight it | 82 | 357 | 288 | 52 | 779 (78.5) |
| Helpless &depressed can’t do anything about it | 15 | 59 | 40 | 6 | 120 (12.1) | |
| Anxious & restless | 15 | 33 | 18 | 3 | 69 (7.0) | |
| Just another phase | 5 | 11 | 4 | 4 | 24 (2.4) | |
| Activities at home | Work from home | 33 | 133 | 79 | 7 | 252 (25.4) |
| Spending time with family | 25 | 157 | 102 | 16 | 300 (30.3) | |
| Television/mobile/social media | 22 | 66 | 51 | 14 | 153 (15.4) | |
| Household chores | 17 | 68 | 80 | 12 | 167 (16.8) | |
| Hobbies | 20 | 36 | 38 | 16 | 110 (11.1) | |
| Has lockdown affected your income and work* | Yes | 64 | 306 | 228 | 31 | 629 (63.4) |
| No | 53 | 154 | 122 | 34 | 363 (36.6) | |
| Can you sustain lockdown for long | Yes, I can manage | 37 | 157 | 130 | 27 | 351 (35.4) |
| No cannot manage the basic amenities and medical needs | 40 | 166 | 88 | 21 | 315 (31.8) | |
| No i will be emotionally shattered | 40 | 137 | 132 | 17 | 326 (32.8) | |
| Alter/Cancel travel plans | Yes | 99 | 419 | 328 | 63 | 909 (91.6) |
| No | 18 | 41 | 22 | 2 | 83 (8.4) | |
| Fear of acquiring disease/ spreads by meeting people? | Yes | 96 | 382 | 295 | 47 | 820 (82.7) |
| No | 21 | 78 | 55 | 18 | 172 (17.3) | |
| Sleep pattern changes* | More than usual | 23 | 87 | 43 | 4 | 157 (15.8) |
| Trouble in sleeping | 60 | 232 | 215 | 42 | 549 (55.3) | |
| No changes | 34 | 141 | 92 | 19 | 286 (28.9) | |
| Increased smoking and alcohol | Yes | 35 | 101 | 87 | 38 | 261(26.3) |
| No | 82 | 350 | 262 | 37 | 731(73.7) | |
| Diet pattern changes* | Yes | 86 | 349 | 297 | 57 | 789 (79.5) |
| No | 31 | 111 | 53 | 8 | 203 (20.5) | |
| Is COVID-19 a taboo | Yes | 43 | 135 | 90 | 13 | 281 (28.3) |
| No | 74 | 325 | 260 | 52 | 711 (71.7) | |
| Do you have sufficient funds to manage lockdown? | Yes | 59 | 201 | 186 | 47 | 493 (49.7) |
| No | 21 | 106 | 52 | 8 | 187 (18.8) | |
| Maybe | 37 | 153 | 112 | 10 | 312 (31.5) | |
Statistically significant findingsp < 0.05).
Graph 1.
Significant association of bivariate variables.
Pearson’s correlation analysis of bivariate variables indicated that an increased understanding of the meaning of social distancing enabled its increased practice. Also, negative correlation between age and travel plans indicated that decreasing age was associated with increasing possibility of modifications in travel plans. While an increase in fear of acquiring COVID-19 by meeting people was correlated with an increase in dietary pattern changes, it displayed negative correlation to sleep pattern changes.
The COVID-19 outbreak has led to diversified mental health responses depending on the individual’s strengths and weaknesses (Wang et al., 2020). Knowledge about the disease and the reasons for lockdown are vital tools for successful disease containment (Brooks et al., 2020). In the present study, 92.5 % and 97.5 % respondents were well acquainted with the knowledge of COVID-19 and social distancing or isolation respectively, with 98.2 % following it (p < 0.05). There was a positive correlation between the awareness of social distancing or isolation and those who were practicing it. Present survey revealed 78.5 % participants were optimistic and believed that together the disease could be curtailed (p < 0.05). However, it has been contemplated that greater the number of individuals following updates about the same, higher are the anxiety levels (Moghanibashi-Mansourieh, 2020). Although social media has played a pivotal role in these times with a splurge of knowledge, information must be gathered from health authorities in order to help distinguish facts from rumours, as facts can help minimize fears. 12.1 % participants felt helpless & depressed suggesting that containment, loss of daily schedule, and diminished social and physical contact with others can cause mental fatigue, dissatisfaction, and a feeling of confinement from the remainder of the world. 12.1 % participants felt helpless & depressed suggesting that containment, loss of daily schedule, and diminished social and physical contact with others can cause mental fatigue, dissatisfaction, and a feeling of confinement from the remainder of the world (Brooks et al., 2020).
Following the imposition of the lockdown, 91.6 % of respondents altered or canceled their travel plans. When asked about effects of the disease on mankind, 60.2 % believed that it would lead to loss of human lives, 29.8 % people were concerned about possible economic slowdown while 1.9 % people believed it to be a mere social media hype. When enquired about the activities during the lockdown, only 11 % were occupied with hobbies whereas WHO advises engaging in regular exercising, daily chores, and hobbies during the present COVID-19 pandemic for mental health well-being (WHO, 2020). Significant associations were observed between age groups and the multivariate variables of knowledge about COVID 19, effects of COVID 19 on mankind and how the participants felt about the present situation.
Sleep disturbances have been shown to be a risk factor for mental disorders. Also, sleep quality has been found to be dependent on anxiety, stress and self-efficacy (Xiao et al., 2020). Moreover, short sleep duration in some individuals has been associated with suicidal tendencies (Weber et al., 2020). In current study 55.3 % complained of trouble sleeping during this lockdown period, of which people who feared contracting the disease and participants between the age group 35–50 years witnessed maximum alteration in sleep. This could be associated with high levels of anxiety and stress because of isolation, indicating adverse mental health. (Rajkumar, 2020)
Nutritional factors are interlaced with human behaviour, and emotions while playing a critical role in not just the initiation, but also the severity and duration of depression. Numerous reports support the view that stress can either increase or decrease caloric intake, and chronic stress exposure can lead to either obesity or anorexia (Sathyanarayana Rao et al., 2008). Variations in eating patterns were observed in the present study in 79.5 % of participants, with people aged 35–50 years experiencing maximum alterations in diet patterns that were positively correlated with the practice of social distancing and fear of acquiring the disease on meeting someone. Though not significant, 26.3 % of respondents stated that they started consuming more alcohol/drugs/tobacco, raising an alarm, as isolation might lead to an escalation in alcohol misuse and probable development of alcohol use disorder in high-risk persons during and after the pandemic (Clay and Parker, 2020).
It has been reported that during quarantine, inadequate basic supplies can cause resentment. 35.4 % of the participants commented that they could sustain lockdown; however majority of the respondents could not manage either due to lack of basic amenities and medical needs (31.8 %) or due to emotional reasons (32.8 %) Blendon RJ also stated that lack of regular medical care was a concern for participants (Brooks et al., 2020). Financial hardships are often experienced by individuals during quarantine. Lockdown majorly affected the work and income of 63.4 % of the population that was positively related to people aged 35–50 years, followed by 50–65 years, impacting their financial status. Even though 49.7 % of the study population claimed to have sufficient funds to manage the lockdown situation, remaining were either uncertain about it or did not have the resources to sustain it. Monetary loss is a stressor during and post isolation because people are unable to work and professional activities are interrupted unprecedentedly; the effects appear to be long lasting. Financial loss due to quarantine created severe socio-economic distress (Pellecchia et al., 2015) and was established to be a contributing factor for symptoms of mental health disorders, anger and anxiety (Mihashi et al., 2009).
Although stigma has aggravated the anguish from many major epidemics in the past, with various studies suggesting that patients were being treated differently, being avoided, treated with fear and suspicion and received critical comments (Wilken et al., 2017), in the current study 71.7 % believed that acquiring COVID-19 was not a social taboo.
The present lockdown which was initially proposed for 21 days was eventually extended for another 3 weeks. Longer quarantines have a direct correlation with the mental health outcomes and the duration of the lockdown is a predominant stressor affecting the mental health of individuals (Brooks et al., 2020).During the SARS outbreak, many studies investigated the mental health impact on the non-infected community, revealing significant psychiatric morbidities (Sim et al., 2010).
Even when people adhere to the lockdown, rather than comply, various moral and mental health issues are raised, creating a debate about individual rights versus such public health interventions during a crisis. However, if authorities are strategic in their planning, lockdowns may become more effective and with fewer effects on the mental health of people.
Author contributions
-
1
Dr. Anuraj Singh Kochhar: Conception and design of the study, acquisition of data and analysis of the same. Drafting the article, critically evaluating and giving final approval for the same.
-
2
Dr. Ritasha Bhasin: Conception of design, drafting the article, and critically evaluating it. Approving the final version.
-
3
Dr. Gulsheen Kaur Kochhar: Conception of design for the study, analysis of the data, drafting the article, revising it and critically evaluating it. Approving the final version.
-
4
Dr. Himanshu Dadlani: Conception and design of the study, acquisition of data, or analysis and interpretation of data, drafting the article, critically evaluating and giving final approval.
-
5
Dr. Viral Vijay Mehta: The conception and design of the study supervising the acquisition of data along with analysis and interpretation of data. Critically evaluating the article and giving the final approval.
-
6
Ms. Roseleen Kaur: Conception and design of the study, acquisition of data and analysis of the same. Drafting the article, revising it, critically evaluating and giving final approval for the same.
-
7
Ms. Charanpreet Kaur Bhasin: Condensing the article in its present form.
Financial disclosure
No fees and grants from, employment by, consultancy for, shared ownership in, or any close relationship with, an organisation whose interests, financial or otherwise, has been received by any of the authors.
Ethical declaration
-
1
Authorship of the paper: Authorship has been limited to only those who have made a significant contribution to the conception, design, execution, or interpretation of the reported study. CRediT author statement attached with the cover letter.
-
2
Originality and plagiarism: The authors have ensured that they have written entirely original manuscript, and if the authors have used the work and/or words of others, that has been appropriately cited or quoted.
-
3
Data access and retention: The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
-
4
Multiple, redundant or concurrent publication: This manuscript has not been published before and is neither under consideration for publication elsewhere since it was originally submitted to Asian Journal of Psychiatry. The manuscript in its current form is approved by all authors.
-
5
Acknowledgement of sources: Proper acknowledgment of the work of others has been specified wherever used.
-
6
Disclosure and conflicts of interest: Submitted separately
-
7
Fundamental errors in published works: When ever such an error would be noted / discovered, it will be promptly notified to the journal editor or publisher and cooperated with the editor to retract or correct the paper.
-
8
Reporting standards: Work is accurately performed and discussed in its significance.
-
9
Hazards and human or animal subjects: There was no indication of unfavorable effects on safety/risk to the participants of the study.
-
10
Use of patient images or case details: Ethical committee approval and informed consent of volunteers obtained, which is documented in the manuscript.
Declaration of Competing Interest
No conflict of interest reported by any of the authors.
References
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/s0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clay J.M., Parker M.O. Alcohol use and misuse during the COVID-19 pandemic: a potential public health crisis? Lancet Public Health. 2020 doi: 10.1016/s2468-2667(20)30088-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihashi M., Otsubo Y., Yinjuan X., Nagatomi K., Hoshiko M., Ishitake T. Predictive factors of psychological disorder development during recovery following SARS outbreak. Health Psychol. 2009;28(1):91–100. doi: 10.1037/a0013674. [DOI] [PubMed] [Google Scholar]
- Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatry. 2020 doi: 10.1016/j.ajp.2020.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellecchia U., Crestani R., Decroo T., Van den Bergh R., Al-Kourdi Y. Social consequences of Ebola containment measures in Liberia. PLoS One. 2015;10(12) doi: 10.1371/journal.pone.0143036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J. Psychiatry. 2020;52 doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sathyanarayana Rao T., Asha M., Ramesh B., Jagannatha Rao K. Understanding nutrition, depression and mental illnesses. Indian J. Psychiatry. 2008;50(2):77. doi: 10.4103/0019-5545.42391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim K., Huak Chan Y., Chong P.N., Chua H.C., Wen Soon S. Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. J. Psychosom. Res. 2010;68(2):195–202. doi: 10.1016/j.jpsychores.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandon R. The COVID-19 pandemic, personal reflections on editorial responsibility. Asian J. Psychiatry. 2020;50 doi: 10.1016/j.ajp.2020.102100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber F.C., Norra C., Wetter T.C. Sleep disturbances and suicidality in posttraumatic stress disorder: an overview of the literature. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.00167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (2020, March 19). WHO World Health Organization. https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf.
- Wilken J.A., Pordell P., Goode B., Jarteh R., Miller Z., Saygar B.G., Maximore L., Borbor W.M., Carmue M., Walker G.W., Yeiah A. Knowledge, attitudes, and practices among members of households actively monitored or quarantined to prevent transmission of Ebola virus disease — Margibi County, Liberia: February-March 2015. Prehosp. Disaster Med. 2017;32(6):673–678. doi: 10.1017/s1049023x17006720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao H., Zhang Y., Kong D., Li S., Yang N. Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Med. Sci. Monit. 2020;26 doi: 10.12659/msm.923921. [DOI] [PMC free article] [PubMed] [Google Scholar]