Highlights
-
•
The COVID-19 pandemic can no longer be mitigated by a nationwide approach of individual nations alone.
-
•
Considering an ‘all hands-on deck’ concept, we present a comprehensive list of tools and entities responsible for and enabling them, as well a conceptual framework to achieve the maximum impact.
-
•
Included are the roles of individuals, communities, government and other sectors such as school systems, health, institutions, and business.
-
•
We call on all countries to act synergistically to minimize everyone's risk, to maximize collaboration, and to commit to shared progress.
Keywords: COVID-19, SARS-COV-2, Pandemic, Mitigation
Abstract
The COVID-19 pandemic can no longer be mitigated by a nationwide approach of individual nations alone. Given its scale and accelerating expansion, COVID-19 requires a coordinated and simultaneous Whole- of-World approach that galvanizes clear global leadership and solidarity from all governments of the world. Considering an ‘all hands-on deck’ concept, we present a comprehensive list of tools and entities responsible for enabling them, as well a conceptual framework to achieve the maximum impact. The list is drawn from pandemic mitigation tools developed in response to past outbreaks including influenza, coronaviruses, and Ebola, and includes tools to minimize transmission in various settings including person-to-person, crowd, funerals, travel, workplace, and events and gatherings including business, social and religious venues. Included are the roles of individuals, communities, government and other sectors such as school systems, health, institutions, and business. While individuals and communities have significant responsibilities to prevent person-to-person transmission, other entities can play a significant role to enable individuals and communities to make use of the tools. Historic and current data indicate the role of political will, whole-of-government approach, and the role of early introduction of mitigation measures. There is also an urgent need to further elucidate the immunologic mechanisms underlying the epidemiological characteristics such as the low disease burden among women, and the role of COVID-19 in inducing Kawasaki-like syndromes in children. Understanding the role of and development of anti-inflammatory strategies based on our understanding of pro-inflammatory cytokines (IL1, IL-6) is also critical. Similarly, the role of oxygen therapy as an anti-inflammatory strategy is evident and access to oxygen therapy should be prioritized to avoid the aggravation of COVID-19 infection. We highlight the need for global solidarity to share both mitigation commodities and infrastructure between countries. Given the global reach of COVID-19 and potential for repeat waves of outbreaks, we call on all countries and communities to act synergistically and emphasize the need for synchronized pan-global mitigation efforts to minimize everyone's risk, to maximize collaboration, and to commit to shared progress.
‘All Hands on Deck’ is an expression of naval origin. Facing a storm or other life-threatening emergency, the ship's captain calls out the command for all sailors (hands) to leave their posts and come to the deck to help navigate the storm (Barrett, 2019). As public health professionals around the world navigate the maelstrom of COVID-19 that is already a global pandemic reaching over 190 nations and accelerating, the time for “All Hands on Deck” has now arrived.
Previous Public Health Emergencies of International Concern have been geographically distinct, affording safe havens outside of the outbreak hotspot (World Health Organization, 2016). For example, at the height of the recent 2018–19 Ebola outbreak in the Democratic Republic of Congo, life in the capital Kinshasa was near normal save occasional public health messages on billboards seen in the streets. Past outbreaks were contained with a national “whole-of-government” approach, where individual countries sought to overcome the limitations of compartmentalized public institutions to advance public policies (Christensen and Lægreid, 2007).
In terms of its reach, contagion and economic impact, the COVID-19 pandemic places unprecedented pressure on individuals, societies, health care systems, businesses and institutions and governments around the world (Abiad et al., 2020, McKinsey and Company, 2020). The COVID-19 pandemic can no longer be mitigated by a nationwide approach of individual nations alone. (Box 1 ) Given its scale and accelerating expansion, COVID-19 requires a coordinated and simultaneous Whole-of-World approach that galvanizes clear global leadership and solidarity from all governments of the world. This is particularly relevant for the interconnected 21st Century world where a specific disease threat in one location can disseminate globally in as little as 36 h, evolving into a global public health security risk (World Health Organization, 2007).
Box 1. Why COVID-19 mandates whole-of-world pandemic mitigation.
-
•
SARS-CoV-2 is the most infectious of the corona viruses which have crossed species from animal host to human host including SARS and MERS.
-
•
SARS-CoV-2 is transmitted via the respiratory and fecal-oral route, survives in droplets for 3 h and on contaminated surfaces for up to 3 days, with viral shedding prior to onset of symptoms and continuing for days after testing for active infection becomes negative (Lan et al., 2020).
-
•
SRS-CoV-2 affects both young adults and elderly. Case fatality rates among young adults are lower but can show intense morbidity in response to infection. Case fatality rates have been higher in the elderly and all persons with underlying comorbidities. This broad demographic profile means its public health burden has enormous economic impacts on both developed and developing nations alike (Guan et al., 2020).
-
•
Herald waves of outbreaks followed by repeat waves may become the norm when a pandemic of this scale is already global and the pathogen can be repeatedly reintroduced to previously mitigated areas. Waves of outbreaks occur as a result of geographic variation in response measures, testing, and quarantining, leading to repeat seeding of infections (Global News, 2020, Neher et al., 2020).
-
•
When an outbreak achieves pandemic status, mitigation is the preferred option to sustain societal functions (Madhav et al., 2017) and may require an all-government and all-societal approach including lock-down for a limited time to enable the full range of nonpharmaceutical intervention tools.
-
•
Medical counter measures- whether deploying repurposed or novel agents – all require time for development, implementation and evaluation of their impact, safety and efficacy.
-
•
The demands of a global pandemic exert enormous public health burdens on health care infrastructure and personnel, leading to health workers who themselves become infected, and intense shortages of already scarce and tightly guarded critical medical materiel. Together, these and the inability to care for routine health means that health systems exert a rapid and dramatic contraction in even the most powerful economies (Nuclear Threat Initiative, 2019).
-
•
The 54% of the world population who live in urban areas (The World Bank, 2018) depend on a complex globally interconnected supply chain dynamic to secure necessities. These supply chains are becoming severely strained both internationally where the products are consumed and in the feeder countries that manufacture them.
-
•
Over 168 million people across 50 countries (28 countries in conflict) are estimated to need humanitarian assistance in 2020 (Poole et al., 2020) and many of these countries have suboptimal surveillance and response capabilities.
-
•
24 countries have an adult HIV prevalence of ≥2% and in such populations COVID-19 may be exacerbated due to the prevailing immunodeficiency (World Health Organization, 2019).
Alt-text: Box 1
Pandemic mitigation tools currently available for the suppression of episodic or sustained outbreaks
In the absence of pathogen-specific medical measures, the current COVID-19 scenario demands agile, adaptive, multifaceted, layered, and timely interventions throughout repeat waves of outbreaks defining the entire pandemic period that need to be synchronized among and across countries, regions and the world (Ebrahim et al., 2020, Ferguson et al., 2020, Wilder-Smith and Freedman, 2020, Fisher and Wilder-Smith, 2020, Zastrow, 2020). We provide a summary of available tools and responsibilities (Table 1, Table 2 ). These measures do not include routine health care system interventions for COVID-19 affected persons including isolation and supportive treatment.
Table 1.
Individual centered pandemic mitigation tools.c
| Action items | Individual | Communities | School systems | Health sector | Business sector | Institutionsa | Governmentsb |
|---|---|---|---|---|---|---|---|
| A. Protect yourself | |||||||
| Hand hygiene | R | ||||||
| Avoid touching mouth nose eyes with unwashed hands | R | ||||||
| Avoid close personal contact | R | ||||||
| Physical distancing of 6 feet from other persons | R | E | |||||
| Limit social interactions outside home | R | E | |||||
| Healthy living (food, rest, exercise) | R | ||||||
| Take your medications, keep adequate supply of medicines (e.g.: diabetes) | R | ||||||
| If sick, seek direct or telemedical care and follow health authority advisory | R | R | R | ||||
| B. Protect others | |||||||
| Practice cough hygiene, use facemask if sick | R | ||||||
| Stay home if you have nonemergency illness from non-COVID-19 illness | R | ||||||
| Clean and disinfect frequently touched surfaces | R | ||||||
| Launder all washables (clothes, toys) with hot water | R | ||||||
| If exposed to sick persons, isolate yourself in separate room, use facemask | R | R | |||||
| C. Protect children elderly and the vulnerable | |||||||
| Be a role model for children to practice protection of self and others | R | ||||||
| Interact with school and teachers to make home learning fun | R | R | |||||
| Create a schedule for at home learning | R | E | |||||
| Help children stay socially connected with friends without in person contact | R | E | |||||
| Keep children healthy– provide healthy meals, watch for signs of illness, and promote active outdoor activities without person-to-person contact | R | E | R | ||||
| Avoid kids’ contact with the elderly, and chronically ill persons | R | ||||||
| Limit exposure of elderly and vulnerable persons to others while providing them care or provisions including in institutionalized settings | R | R | R | R | |||
| D. Protect pregnant and breast-feeding women | |||||||
| Promote practice of personal protection measures listed above | R | E | |||||
| E. Protect your home | |||||||
| Clean and disinfect surfaces frequently touched (tables, doorknobs, light switches, phones, keyboards, faucets, toilets etc.) | R | ||||||
| Do not mix clothes from sick people with that of others | R | ||||||
| Do not eat with sick individuals | R | ||||||
| Use gloves when handling materials from sick persons | R | ||||||
| Plan and prepare for outbreaks and related movement restrictions | R | ||||||
| Choose a room in your home to separate sick persons from others | R | ||||||
| Stock non-perishable essential food supplies and necessities for two weeks to 30 days, replenish frequently | R | E | |||||
| F. Manage anxiety and stress | |||||||
| Access credible sources, including health authorities and institutions rather than social media posts (health authority, non-profits, CDC, WHO) | R | E | E | ||||
| Stay virtually connected with friends and relatives | R | ||||||
| Develop community networks for information sharing | R | R | |||||
| Avoid excessive alcohol, tobacco, or other drugs | R | ||||||
| Taking care of yourself and people close to you can help cope with stress | R | ||||||
| Continue outdoor activities that avoid person to person contact | R | ||||||
| Seek professional support when available | R | E | |||||
| Avoid activities that put self or family in harm through non-socially distanced activities | R | E | |||||
| G. Safe burial practices (in countries with home based burial practice) | |||||||
| Avoid contact with dead bodies | R | R | |||||
| Delegate burials to professionals or health authorities | R | E | E | R | |||
aIncludes nonprofit and for profit, Universities, research.
bLocal, state, national.
cDuration of these measures will depend on epidemic dynamics in each jurisdiction. The earlier the adherence, the lower the epidemic progression. Early discontinuation may lead to repeat waves of outbreaks.
dR = key responsibility E = Enabler.
Table 2.
Shared and collective pandemic mitigation tools.c
| Action items | Individual | Communities | Institutionsa | Health sector | Business sector | Governmentsb | Multinational organizations |
|---|---|---|---|---|---|---|---|
| A. Physical/social distancing between individuals (six feet separation between individuals) | |||||||
| Suspension of daycare, schools and universities | R | R | R | ||||
| Closure of social- and viral- contact enhancing business (bars, restaurants, fitness centers, nail and hair salons and spa) | E | R | R | ||||
| Event cancelation or transition to virtual events (prayer, celebrations, music, sports, cultural, entertainment, family gatherings, marriages, funerals, conferences, mass gatherings) | E | R | |||||
| Crowd control (lowest observed, ≥3 persons, Germany) | E | E | R | ||||
| B. Travel restrictions | |||||||
| Minimizing public transport to essential mode (trains, taxis, buses, flights) to sustain travel of essential personnel and transport of commodities | R | R | |||||
| Cancelation of cruise ship trips, family vacation road trips | R | R | R | ||||
| Restrict group travel (schools, sports, celebrations, meetings) | R | R | |||||
| C. Maintain/ration supply of essential commodities, food, over the counter medicines | |||||||
| Develop per person limits and pricing for essential items | E | R | |||||
| Maintain and replenish national stockpile of essential items | R | R | |||||
| Assure distribution of essential items to elderly and people with special needs | R | E | R | ||||
| Innovate delivery with use of drones, robots, and drive through pick up | R | R | R | ||||
| E. Invest in resilience of health care workers, personnel involved in government and societal functions | |||||||
| Prioritize sale and distribution of personal protection equipment to health sector, and other essential personnel | R | R | |||||
| Fix supply chain weakness of personal protection equipment and medical products including with repurposing of business sector. | R | R | |||||
| Massive scale up of telemedicine | E | R | R | ||||
| Innovate drive through capacity for testing and triaging of mild cases | E | E | R | R | |||
| F. Safe surging of health care and public health efforts | |||||||
| Adopt (not reinvent) compatible surveillance systems (e.g. influenza) to implement enhanced COVID-19 syndromic surveillance | E | R | R | ||||
| Develop a roadmap for hospitalization capacity to surge (inventory of unused facilities for triage, virtual procurement systems) | R | R | R | ||||
| Hospitals to cancel elective procedures and counsel patients accordingly | E | R | |||||
| G. Support resilience of resource poor countries | |||||||
| Repurposing of U.N. and other multilateral resources | E | E | E | R | |||
| F. Risk communication | |||||||
| Provide facts at routine intervals, control misinformation in social media | R | R | E | R | R | ||
aIncludes nonprofit and for profit, Universities, research.
bLocal, state, national.
cDuration of these measures will depend on epidemic dynamics in each jurisdiction. The earlier the adherence, the lower the epidemic progression. Early discontinuation may lead to repeat waves of outbreaks.
dR = key responsibility E = Enabler.
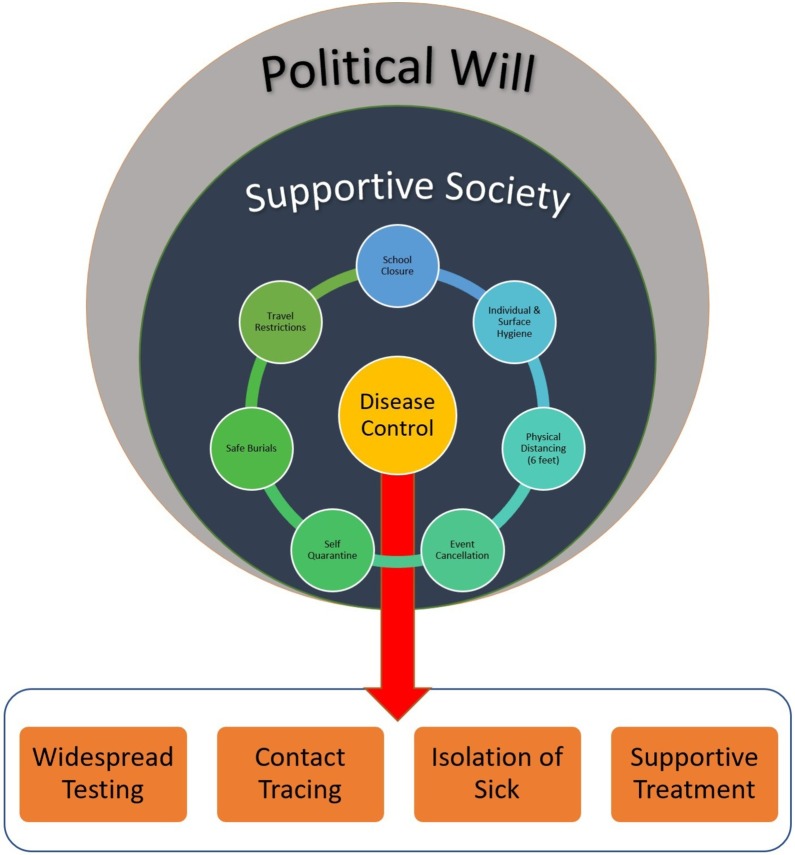
South Korea's pandemic mitigation shows us that the success of these measures depends heavily on political and public will (Fisher and Wilder-Smith, 2020, Zastrow, 2020). Disease control efforts based on case identification require both wide availability of tests to affected people and access to functioning health systems. This can only succeed with societal, fiscal and governmental solidarity (Figure 1 ).
Figure 1.
Framework of pandemic mitigation in societal and political context.
Because an infected individual remains the major source of infection in a community, the benefit of individual, family, and community contributions to mitigation (Table 1) will serve as the foundation for the health sector to implement specific disease control activities. Sharply tailored mitigation strategies – including tailored quarantine – can only be achieved with deep engagement of the public health infrastructure at the household level. Further, compliance with individual, family, and community responsibilities must remain feasible throughout the pandemic period, although the national and global and opportunity costs are not fully known (Photo 1 ).
Photo 1.
Preparing isolation ward at a provincial hospital in Cambodia, Credit: Shahul Ebrahim.
Closure of school and childcare systems is most impactful in enabling community level mitigation efforts. Enabling teachers to sustain learning opportunities using remote, including online, platforms and continuation of school-based meal programs enables pupils to be engaged, enhances community resilience, and reduces population movements from neighborhoods to school buildings where some of the highest population densities in communities are found- inside classrooms and assembly rooms and playgrounds (Public Health Agency of Canada, 2020, Centers for Disease Control and Prevention (CDC), 2020).
Health systems of all categories and their diverse governing and regulating entities will vary in their responses depending on the severity of outbreak in geographic areas. Paramount for all healthcare systems must be keeping the health care staff COVID-19-free: without a robust healthcare force, the crisis deepens and perpetuates (Gawande Atul, 2020, World Health Organization, 2020a).
Classic disease control strategies such as early detection, case isolation, contact testing, health care infection control, and clinical care remain the responsibility of the health care system. However, when the system is overwhelmed or when public health reach has been chronically underfunded, in the pandemic setting, not only health care systems but also governments may restrict services to providing care for the critically ill while delegating the isolation of contacts and less severe infections to the individuals, individual care providers, and communitiesphoto 1. At times of large outbreaks, contact testing may not be sustainable, and testing may be confined to the confirmation of the severely ill, leading to exaggerated case fatality rates and an increased number of COVID-19 suspects, which itself depletes the health care system capacity.
The role of home-managed funerals in sustaining disease transmission emerged during the 2014 Ebola outbreak, and is relevant for many developing countries (Pandey et al., 2014). Joint efforts by anthropologists and religious leaders were crucial in engaging communities to minimize such risk.
We have used the arbitrary term “institutions” to reflect a broad range of not-for profit and non-governmental entities (academic, advocacy, funding, research) and may include health, economy, commerce, policy, politics, and technology sectors. Institutional contributions may include redirection of and supplementing pandemic mitigation efforts of the health system, academic institutions or governments. Such institutions can advance hybrid governmental and private sector responses. Universities can help seamless information flow, dedicated information sites, and support to corporate telehealth initiatives, and can participate in research. The Johns Hopkins University COVID-19 Resource Center is an example. In May the Task Force for Global Health convened a virtual meeting across 46 global entities representing pharmaceutical commodity donors, implementing partners and shippers, under WHO leadership to assess and respond to anticipated interruptions in the critical supply chain of deworming drugs. This rapid consultation across multilaterals and private sector entities helped rapidly access existing platforms such as the DHL Control Tower for Humanitarian Supply Chain to assist the movement of medical supplies and other essential drugs from China to the rest of the world.
The business sector is a critical determinant of modern societal functions worldwide and has huge stakes in making pandemic mitigation successful. For example, N-95 masks may be made in Cambodia by a U.S. owned corporation but sold in Canada or Chile. Virtual inventories can make it possible to divert shipments to countries where they are most needed. Currently there is no cohesive data base of critical medical materials across governmental and private sector producers (existing inventories are diverse and un-linked).
The business sector can enhance service delivery (for example rapid test kit availability), innovation, or production of countermeasures such as pharmaceuticals, vaccines, and novel delivery systems including drone and robotics assets in multiple countries. Elsewhere, online and drive-through delivery options may need massive upscaling, directly contributing to mitigation while augmenting social distancing. Repurposing factories to fill in gaps for commodities and pandemic-specific products for fast-moving mitigation efforts can ease the impact of the pandemic on communities while creating jobs.
Whole-of-government approaches are aimed at maintaining social order, activating or enforcing social distancing measures and crowd control, reducing travel opportunities to minimize import or export of infections while allowing essential travel, movement of products and essential personnel, the redirection of essential services (including of health) to triage and treat seriously ill patients, and enhancing national capacity for contact testing surveillance and testing.
Additional government efforts focusing on the economic security of respective countries include investments in research, economy boosters and incentives as has been proposed in the USA. These include reduction of interest rates or extension of tax deadlines and suspension of taxes, job creation, and unemployment benefits.
The World Health Organization's convening role (in addition to the implementation of the International Health Regulations) to guide the strategic and tactic actions to contain, mitigate and suppress the pandemic becomes even more important. Irrespective of their lack of enforcement authority, multilateral and multinational entities can be powerful stewards of convening governments and experts with varying priorities and capacities to provide unbiased scientific and policy direction on pandemic mitigation.
The peacekeeping missions of the United Nations (World Health Organization, 2016) and the African Union are examples of international stewardship for security. Such options must be explored for mitigation efforts where needed. For example, if a country's defense or health sector is severely affected by absenteeism from illness or lacking resources to maintain mitigation measures or maintain law and order, multilateral peacekeeping missions and staff may be deployed for assistance.
A globally synchronized application of mitigation measures is needed to get ahead of the virus
Although most of the tools presented in Table 1, Table 2 are local and national actions, to achieve full benefit of these efforts, these should be coordinated internationally. Russia and Saudi Arabia are some of the countries that did not wait for cases to emerge as a benchmark for initiating emphatic mitigation measures, and the subsequent spread of COVID -19 in those countries has been slow compared to countries that waited for infections to peak before embarking on mitigation. Experience in Taiwan also demonstrates the value of early introduction of nonpharmaceutical interventions and disease control strategies (Wang et al., 2020).
Pandemic mitigation measures in nations seeking to escape escalating pandemics should ideally begin before clinical cases are identified. Given the asymptomatic shedding of SARS-COV-2, and limited test availability, non-recognition of a case or slow spread in one geographical location should not lead to complacency (Madhav et al., 2017, Wang et al., 2020, Knaus and Doherty, 2020, Baird, 2020).
The aphorism, “A case anywhere is a threat everywhere” must be the overriding impetus for the activation of definitive mitigation measures. A patchwork of different timings of mitigation measures in multiple countries will only help SARS-CoV-2 maintain reservoirs awaiting reintroduction to nations that lift mitigation efforts prematurely. China and Hong Kong may be in the early stages of successive waves. It is premature to discern if all countries will have a similar trajectory. As such, while extreme measures may be relaxed based on data, they should not minimize the importance of continuity of individual and community measures.
If countries are financially and organizationally capable and have reached an interval between pandemic waves, some of these skills and resources can be shared with more challenged countries, as has been done by China in Italy. There is a need to simplify international procedures for countries communicating and collaborating to repatriation of stranded citizens (consider the U.S. and U.K. citizens marooned in Peru), the sharing of relevant epidemic data, sharing of transparent outcome data in real-time including both successes and challenges with mitigation measures, and the leveraging of nation-specific capacities (Hamzah et al., 2020, O’Carroll, 2020, Kelly, 2020).
Stringent measures will no doubt lead to economic hardships for all. Our resolve will be judged not by how we prevented the economic impact, but how we mitigated the pandemic, related illness and deaths (Abiad et al., 2020, Anzai et al., 2020, United Nations Conference on Trade and Development, 2020, World Health Organization, 2020b).
Prepare for an adaptive, not fixed, duration of mitigation
An adaptive rather than a fixed strategy for restrictive mitigations strategies is required, one that is sufficient to avoid repeat waves of outbreaks. Based on the incubation period, countries are using a 14 to 21 day period as rule of thumb for extreme measures such as “lockdown”, “shelter-in-place” or declaration of emergency”, yet it is vital to note that at least two incubation cycles or longer would provide reasonable time to flatten the epidemic curve, and most countries expanded the time frame. Social distancing measures would need to be practiced even after extreme measures. For Ebola, the current practice is to continue mitigation efforts for two cycles of 21 days each (42 days total) after the detection of the final case. However, an exit plan is necessary at the end of the lock-down. Successive waves of infections must be anticipated and prepared for (Ferguson et al., 2020, Anzai et al., 2020, United Nations Conference on Trade and Development, 2020, Ebrahim and Memish, 2020).
Integrate research to response to further elucidate the natural history of COVID-19
Although we have discerned substantial knowledge on SARS-COV-2 and COVID-19 in the past few months in pandemic speed, additional epidemiological, virologic, and clinical data on SARS-CoV-2 and COVID-19 would help consolidate and verify the known facts. The severity of the disease depends on the efficiency of the immune system (Conti and Younes, 2020, Conti et al., 2020a, Conti et al., 2020b, Ronconi et al., 2020). Clinical and epidemiological data suggest that women are less likely to acquire SARS-COV-2. This may be due to variation in immunologic response in men and women and should be confirmed. The immune regulatory genes encoded by the X chromosome in the female gender cause lower viral load levels, and less inflammation than in men; the levels of activation of the immune cells are higher in women than in men; women generally produce higher levels of antibodies which remain in the circulation longer; and testosterone in males predisposes them to cardiovascular inflammation (Conti and Younes, 2020). There is an urgent need to study the role of pro-inflammatory cytokines, an important modulator of COVID-19, and drugs that bind to IL-1, IL-1R, IL-37, IL38 and tumor necrosis factor (TNF) (Conti et al., 2020a, Ronconi et al., 2020). Recent evidence suggests an urgent need to assess the impact of COVID-19 on child health. Inflammatory cytokines may play role in the reported aggravation of Kawasaki disease in children by COVID-19, and also in the development of SARS-CoV-2 induced disease similar to Kawasaki illness (Conti et al., 2020b). Along with home quarantine and other community mitigation measures, Conti et al. have called for better understanding of the role of oxygen therapy and the mode of action of O3 that has been proven to be beneficial to inhibit viral replication and improvement of lung function. Access to oxygen therapy should be assured to reduce aggravation of clinical symptoms. Understanding these immunological paradigms evidenced among women and children by epidemiological data will also help inform our efforts to develop antiviral agents and vaccine research.
Guiding principles for easing mitigation efforts
Effects of both mitigation efforts and unmitigated progression of COVID-19 on human life are real. The primary goal of easing mitigation (reopening the economy to avert unintended consequences of mitigation) should be to maximize the number of lives saved. The impact of prolonged periods of mitigation may vary greatly by socio-economic status of populations. Mitigation efforts may exacerbate or lead to starvation, prolong economic disruption, and increase morbidity and mortality from deferred medical care, mental health problems, domestic violence, and reversal of socio-economic development investments such as in education.
Timing of easing mitigation interventions
-
•
Declining test positivity over a 14-day period where testing is adequate to meet demands of all symptomatic persons and contacts
-
•
Declining hospitalization over a 14-day period
-
•
Declining intensive care utilization over a 14-day period
Key requirements for easing mitigation interventions include
-
•
Surveillance innovation and testing capacity to monitor disease burden
-
•
Strategy, speed, and capacity for contact tracing
-
•
Per-capita hospital bed utilization trends and capacity for potential surge
-
•
Per-capita intensive care utilization trends and capacity for potential surge
-
•
Adequacy of critical health care workforce
SARS-CoV-2 test capacity should be sufficient for symptomatic persons and contacts. Test kits also will be required for population-based surveillance, and surge related testing. Environmental (sewage) sample testing may provide a proxy for population level monitoring. Algorithms can help discern outbreaks through self-reporting of signs and symptoms. Innovation in contact testing includes proximity tracking and other personal electronic tracking concepts subject to ethical considerations and feasibility.
Considerations for prioritization of staggered easing of pandemic mitigation interventions
-
•
Essential nature of the service or entity
-
•
Severity of adverse consequences on human behavior and survival of absence or an activity or event
-
•
Existence or potential for COVID-19 epidemic risk factors in a service or entity
-
•
Availability of potential minimal risk operational options in a service or entity
-
•
Transportation or geographic proximity for inward populations movements
-
•
Population density of target geographic area for easing interventions
-
•
Social well-being and cultural sensitivities such as for burials and family functions
-
•
Opportunity for crowd size restrictions and innovation in hygienic operations
As capacities and epidemic profiles of countries vary, specific recommendations are challenging. The following decision trees can inform local deliberations.
Childcare: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/Childcare-Decision-Tree.pdf
Camps: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/Camps-Decision-Tree.pdf
Schools: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/Schools-Decision-Tree.pdf
Workplaces: https://www.cdc.gov/coronavirus/2019-ncov/downloads/community/workplace-decision-tree.pdf
Restaurants Bars: https://www.cdc.gov/coronavirus/2019-ncov/downloads/community/restaurants-and-bars-decision-tree.pdf
Mass Transit: https://www.cdc.gov/coronavirus/2019-ncov/community/pdf/MassTransit-DecisionTree.pdf
The way forward
Pandemic COVID-19 has created a new norm, a challenge to the globalized and interconnected system that defines humanity in the 21st Century. Such challenges can only be effectively addressed through a pan-global mindset. Although all countries may be affected by the time of the publication of this paper, some communities may not have detected their first case. We appeal to all communities to get ahead of the virus and take measures to keep the common enemy out. Not having a huge caseload is no assurance of freedom from COVID-19. The only difference is that those that take early, broad and proactive measures will have the least burden and will be best prepared to weather the pandemic. We emphasize the need for synchronized pan-global mitigation efforts to minimize everyone's risk, maximize collaboration and to commit to shared progress. Such an outcome requires concerted efforts from ‘All Hands on Deck’- all individuals, communities, governments, systems, each operating in the tightly-woven global framework that is our world.
Conflict of interest
None of the authors declared COI.
Funding source
No funding for this project.
Ethical approval
Not applicable.
References
- Abiad A., Arao R.M., Dagli S. Asian Development Bank; 2020. The economic impact of the COVID-19 outbreak on developing Asia [Internet] Available from: https://www.adb.org/publications/economic-impact-covid19-developing-asia [cited 14.03.20] [Google Scholar]
- Anzai A., Kobayashi T., Linton N.M., Kinoshita R., Hayashi K., Suzuki A. Assessing the impact of reduced travel on exportation dynamics of novel coronavirus infection (COVID-19) J Clin Med. 2020;9(2) doi: 10.3390/jcm9020601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baird Robert P. The New Yorker; 2020. Why widespread coronavirus testing isn’t coming anytime soon [Internet] Available from: https://www.newyorker.com/news/news-desk/why-widespread-coronavirus-testing-isnt-coming-anytime-soon [cited 26.03.20] [Google Scholar]
- Barrett C. Lyons Press; Guilford, Connecticut: 2019. Three sheets to the wind: the nautical origins of everyday expressions. 192 pp. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) 2020. Implementation of mitigation strategies for communities with local COVID-19 transmission; p. 10. [Google Scholar]
- Christensen T., Lægreid P. The whole-of-government approach to public sector reform. Public Adm Rev. 2007;67(6):1059–1066. [Google Scholar]
- Conti P., Younes A. Coronavirus COV-19/SARS-CoV-2 affects women less than men: clinical response to viral infection. J Biol Regul Homeost Agents. 2020;34(2) doi: 10.23812/Editorial-Conti-3. [DOI] [PubMed] [Google Scholar]
- Conti P., Gallenga C.E., Tetè G., Caraffa A., Ronconi G., Younes A. How to reduce the likelihood of coronavirus-19 (CoV-19 or SARS-CoV-2) infection and lung inflammation mediated by IL-1. JBRHA 34, No. 2, March–April, 2020/Journal of Biological Regulators and Homeostatic Agents. J Biol Regul Homeost Agents. 2020;34(2) doi: 10.23812/Editorial-Conti-2. [DOI] [PubMed] [Google Scholar]
- Conti P., Ronconi G., Caraffa A., Gallenga C.E., Ross R., Frydas I. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies. J Biol Regul Homeost Agents. 2020;34(2) doi: 10.23812/CONTI-E. pii: 1. [DOI] [PubMed] [Google Scholar]
- Ebrahim S.H., Memish Z.A. COVID-19: preparing for superspreader potential among Umrah pilgrims to Saudi Arabia. Lancet. 2020;395(10227):e48. doi: 10.1016/S0140-6736(20)30466-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahim S.H., Ahmed Q.A., Gozzer E., Schlagenhauf P., Memish Z.A. Covid-19 and community mitigation strategies in a pandemic. BMJ. 2020:m1066. doi: 10.1136/bmj.m1066. [DOI] [PubMed] [Google Scholar]
- Ferguson N.M., Laydon D., Nedjati-Gilani G., Imai N., Ainslie K., Baguelin M. 2020. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand; p. 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher D., Wilder-Smith A. The global community needs to swiftly ramp up the response to contain COVID-19. Lancet. 2020 doi: 10.1016/S0140-6736(20)30679-6. pii: S0140-6736(20)30679-6. [Epub ahead of print] No abstract available. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gawande Atul A. The New Yorker; 2020. Keeping the coronavirus from infecting health-care workers [Internet] Available from: https://www.newyorker.com/news/news-desk/keeping-the-coronavirus-from-infecting-health-care-workers [cited 26.03.20] [Google Scholar]
- Global News . Global News; 2020. A 2nd wave of COVID-19 is possible. Here's what that means for Canada [Internet] Available from: https://globalnews.ca/news/6729472/coronavirus-canada-second-wave/ [cited 25.03.20] [Google Scholar]
- Guan W., Ni Z., Hu Y., Liang W., Ou C., He J. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamzah F.A.B., Lau C.H., Nazri H., Ligot D.V., Lee G., Tan C.L. 2020. CoronaTracker: world-wide COVID-19 outbreak data analysis and prediction [Internet]. nCoV. Available from: http://www.who.int/bulletin/online_first/20-255695.pdf [cited 26.03.20] [Google Scholar]
- Kelly L. TheHill [Internet]; 2020. Hundreds of Americans stranded in Peru amid coronavirus closures. Available from: https://thehill.com/policy/international/488126-hundreds-of-americans-stranded-in-peru-amid-coronavirus-closures [cited 26.03.20] [Google Scholar]
- Knaus C., Doherty B. Global shortage of Covid-19 test kits hits Australia as other nations limit exports. The Guardian [Internet] 2020 Available from: https://www.theguardian.com/australia-news/2020/mar/13/global-shortage-of-covid-19-test-kits-hits-australia-as-other-nations-limit-exports [cited 26.03.20] [Google Scholar]
- Lan L., Xu D., Ye G., Xia C., Wang S., Li Y. Positive RT-PCR test results in patients recovered from COVID-19. JAMA [Internet] 2020 doi: 10.1001/jama.2020.2783. Available from: https://jamanetwork.com/journals/jama/fullarticle/2762452 [cited 25.03.20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madhav N., Oppenheim B., Gallivan M., Mulembakani P., Rubin E., Wolfe N. Pandemics: risks, impacts, and mitigation. In: Jamison D.T., Gelband H., Horton S., Jha P., Laxminarayan R., Mock C.N., editors. Disease control priorities: improving health and reducing poverty [Internet] 3rd ed. The International Bank for Reconstruction and Development/The World Bank; Washington (DC): 2017. Available from: http://www.ncbi.nlm.nih.gov/books/NBK525302/ [cited 25.03.20] [Google Scholar]
- McKinsey and Company. COVID-19: Briefing note. Global health and crisis response [Internet]. McKinsey and Company; McKinsey. Available from: https://www.mckinsey.com/∼/media/McKinsey/Business%20Functions/Risk/Our%20Insights/COVID%2019%20Implications%20for%20business/COVID%2019%20March%2025/COVID-19-Facts-and-Insights-March-25-vF.ashx.
- Neher R.A., Dyrdak R., Druelle V., Hodcroft E.B., Albert J. Potential impact of seasonal forcing on a SARS-CoV-2 pandemic. Swiss Med Wkly [Internet] 2020;150(1112) doi: 10.4414/smw.2020.20224. Available from: https://smw.ch/article/doi/smw.2020.20224 [cited 25.03.20] [DOI] [PubMed] [Google Scholar]
- Nuclear Threat Initiative, Johns Hopkins University . The Global Health Security Index; 2019. The economist; p. 324. [Google Scholar]
- O’Carroll D.C.L. The Guardian [Internet]; 2020. Britons stranded in Peru could be flown home early next week. Available from: https://www.theguardian.com/world/2020/mar/21/foreign-office-working-furiously-to-repatriate-400-britons-stranded-in-peru [cited 26.03.20] [Google Scholar]
- Pandey A., Atkins K.E., Medlock J., Wenzel N., Townsend J.P., Childs J.E. Strategies for containing Ebola in West Africa. Science. 2014;346(6212):991–995. doi: 10.1126/science.1260612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poole D.N., Escudero D.J., Gostin L.O., Leblang D., Talbot E.A. Responding to the COVID-19 pandemic in complex humanitarian crises. Int J Equity Health [Internet] 2020:19. doi: 10.1186/s12939-020-01162-y. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7085188/ [cited 25.03.20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health Agency of Canada . 2020. Community-based measures to mitigate the spread of coronavirus disease (COVID-19) in Canada [Internet]. aem. Available from: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/public-health-measures-mitigate-covid-19.html [cited 26.03.20] [Google Scholar]
- Ronconi G., Teté G., Kritas S.K., Gallenga C.E., Caraffa A., Ross R. SARS-CoV-2, which induces COVID-19, causes kawasaki-like disease in children: role of pro-inflammatory and anti-inflammatory cytokines. J Biol Regul Homeost Agents. 2020;34(3) doi: 10.23812/EDITORIAL-RONCONI-E-59. [DOI] [PubMed] [Google Scholar]
- The World Bank . 2018. Urban population (% of total population) | Data [Internet] Available from: https://data.worldbank.org/indicator/SP.URB.TOTL.IN.ZS [cited 24.03.20] [Google Scholar]
- United Nations Conference on Trade and Development . UNCTAD; 2020. The Coronavirus Shock: a story of another global crisis foretold and what policimakers should be doing about it [Internet] Available from: https://unctad.org/en/PublicationsLibrary/gds_tdr2019_update_coronavirus.pdf. [Google Scholar]
- Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA. 2020 doi: 10.1001/jama.2020.3151. Published online March 03. [DOI] [PubMed] [Google Scholar]
- Wilder-Smith A., Freedman D.O. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27(2) doi: 10.1093/jtm/taaa020. pii: taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; Genf: 2007. Global public health security in the 21st century: global public health security. 170 pp. (The World Health Report 2007) [Google Scholar]
- World Health Organization . 3rd ed. World Health Organization; Geneva, Switzerland: 2016. International health regulations. 80 pp. [Google Scholar]
- World Health Organization. Global Health Observatory . WHO. World Health Organization; 2019. Prevalence of HIV among adults aged 15 to 49 – estimates by country [Internet] Available from: https://apps.who.int/gho/data/node.main.622?lang=en [cited 27.03.20] [Google Scholar]
- World Health Organization . 2020. Coronavirus disease (COVID-19) outbreak: rights, roles and responsibilities of health workers, including key considerations for occupational safety and health [Internet] Available from: https://www.who.int/docs/default-source/coronaviruse/who-rights-roles-respon-hw-covid-19.pdf?sfvrsn=bcabd401_0. [Google Scholar]
- World Health Organization . 2020. Coronavirus disease 2019 (COVID-19) Situation Report – 66 [Internet] Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200326-sitrep-66-covid-19.pdf?sfvrsn=81b94e61_2. [Google Scholar]
- Zastrow M. South Korea is reporting intimate details of COVID-19 cases: has it helped? Nature [Internet] 2020 doi: 10.1038/d41586-020-00740-y. Available from: https://www.nature.com/articles/d41586-020-00740-y [cited 25.03.20] [DOI] [PubMed] [Google Scholar]