Abstract
Background and aims
Cardiac biomarkers like cardiac troponins and natriuretic peptides are elevated in a substantial proportion of patients with coronavirus disease 2019 (COVID-19). We propose an algorithmic approach using cardiac biomarkers to triage, risk-stratify and prognosticate patients with severe COVID-19.
Methods
We systematically searched the PubMed and Google Scholar databases until May 31st, 2020, and accessed the available data on the role of cardiac biomarkers in patients with COVID-19.
Results
COVID-19 is associated with acute cardiac injury in around 7–28% of patients, significantly increasing its associated complications and mortality. Patients with underlying cardiovascular disease are more prone to develop acute cardiac injury as a result of COVID-19. The use of cardiac biomarkers may aid in differentiating the cardiac cause of dyspnea in patients with severe COVID-19. Cardiac biomarkers may also aid in triaging, risk-stratification, clinical decision-making, and prognostication of patients with COVID-19. However, there are concerns that routine testing in all patients with COVID-19 irrespective of severity, may result in unnecessary downstream investigations which may be misleading. In this brief review, using an algorithmic approach, we have tried to rationalize the use of cardiac biomarkers among patients with severe COVID-19. This approach is also likely to lessen the infection exposure risk to the cardiovascular team attending patients with severe COVID-19.
Conclusion
It appears beneficial to triage, risk-stratify, and prognosticate patients with COVID-19 based on the evidence of myocardial injury and the presence of underlying cardiovascular disease. Future research studies are, however, needed to validate these proposed benefits.
Keywords: COVID-19, Cardiac injury, Troponin, B-type natriuretic peptide
Highlights
-
•
Cardiac biomarker measurement in all patients with coronavirus disease 2019 (COVID-19) is not routinely recommended.
-
•
It is recommended only when type 1 myocardial infarction or heart failure is strongly suspected on clinical grounds.
-
•
We propose a simple cardiac biomarker-based risk-stratification algorithm to be used in patients with severe COVID-19.
-
•
This algorithm is likely to aid in triaging, risk-prognostication, and management of patients with severe COVID-19.
-
•
The use of this algorithmic approach might also limit infection exposure risk to the attending cardiovascular team.
Coronavirus disease-19 (COVID-19) has caused the demolition of healthcare economies throughout the globe and has generated enormous anxiety in the minds of healthcare personnel. Even the most developed countries with the best of healthcare facilities have succumbed to the unprecedented damage and mortality caused by COVID-19. With the number of patients with COVID-19 expected to increase further in the coming days, which might overwhelm the available healthcare resources, especially in countries with low income and poor healthcare resources, it becomes imperative to identify tools to risk-stratify and triage these patients, albeit with minimal resource utilization.
As cardiovascular physicians, we need to identify patients with COVID-19 who would require an electrocardiogram (ECG), cardiology consultation and imaging, and who would not. This approach is necessary to minimize infection exposure to cardiovascular team personnel and ensure the proper utilization of health care facilities and PPE (personal protective equipment) in countries with limited resources.
The morbidity and mortality in COVID 19 are primarily related to respiratory and or circulatory failure. COVID-19 patients with mild/uncomplicated course do not require hospital admission (except for isolation/quarantine purposes), and further cardiac evaluation. The dilemma arises in patients with severe COVID-19, who usually present with respiratory rate>30/minute, low arterial saturation, and lung infiltrates. The respiratory distress in patients with severe COVID-19 may be the result of the combination of lung injury (Pneumonia/Acute respiratory distress syndrome) and heart failure because of acute coronary syndrome or myocardial injury. Identification of the cardiac origin of respiratory distress, hypoxemia, and circulatory failure is vital in the effective management of these sick patients.
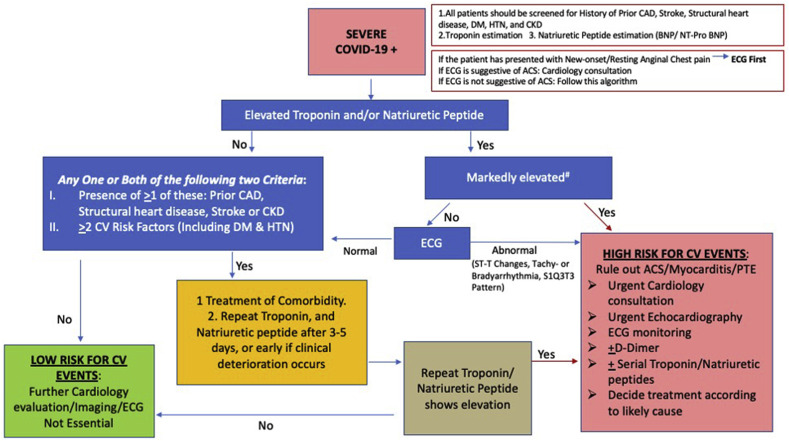
With the ever-evolving recognition of the interplay between COVID-19 and the cardiovascular system, studies have shown that nearly 7–28% of severe COVID-19 patients develop acute cardiac injury (measured by elevated Troponin levels) during illness, which significantly increases the COVID-19 associated complications and mortality [[1], [2], [3]]. Multiple mechanisms have been described for this acute cardiac injury, including acute myocardial infarction (Type 1 MI), myocardial demand-supply mismatch (Type 2 MI), viral myocarditis, and inflammation and oxidative stress-induced myocardial damage [2]. We strongly advocate the role of estimating troponin and natriuretic peptides [BNP (B-type natriuretic peptide) or NT-pro BNP (N-terminal-pro hormone BNP)] for cardiac risk stratification and prognostication of patients with severe COVID-19 (See Fig. 1 for the proposed algorithm).
Fig. 1.
Algorithm to assess acute cardiac injury and risk stratify a patient with severe coronavirus disease.
#Marked elevation refers to Troponin level >3 times ULN; BNP level >100 pg/mL, and NT-Pro BNP level >450, 900 and 1800 pg/mL for ages less than 50 years, between 50 and 75 years, and older than 75 years of age.
Abbreviations- COVID-19=Corona Virus Disease-2019, CAD=Coronary Artery Disease, DM=Diabetes Mellitus, HTN=Hypertension, CKD=Chronic Kidney Disease, BNP=Brain Natriuretic Peptide, NT-proBNP=N Terminal pro Brain Natriuretic Peptide, ECG=Electrocardiogram, ACS=Acute Coronary Syndrome, CV=Cardiovascular, PTE=Pulmonary Thromboembolism
The above statement becomes crucial in the context of a recent advisory from the American College of Cardiology (ACC), which recommended against the measurement of Troponin in COVID-19 patients unless the diagnosis of acute myocardial infarction is strongly suspected on the clinical grounds [4]. This approach was recommended on the basis that Troponin elevation in patients with COVID-19 is likely to be non-specific and multifactorial, and less likely to be due to atherothrombotic coronary occlusion; therefore, this approach would favour unnecessarily downstream testing. ACC did not mention any words regarding its prognostic role. Furthermore, ACC made a similar recommendation for measuring natriuretic peptides in COVID patients, recommending its use only if one suspects heart failure on clinical grounds [4].
However, in a study by Shaobo Shi et al. [2], involving 416 patients hospitalized with COVID-19, acute cardiac injury (elevated high sensitivity Troponin I levels) was demonstrated in 82 (19.7%) patients. Complications were significantly higher, and mortality was almost ten times higher in patients with acute cardiac injury than those without. Furthermore, the Cox regression model analysis revealed that the patients with vs. those without cardiac injury were at a higher risk of death, both during the time from symptom onset (hazard ratio, 4.26 [95% CI, 1.92–9.49]) and admission to endpoint (hazard ratio, 3.41 [95% CI, 1.62–7.16]) [2]. These findings were echoed in another recent study by Guo et al. [3], which showed that 52 (27.8%) out of 187 confirmed severe COVID-19 patients developed acute cardiac injury (measured by elevated Troponin T in this study). Troponin levels showed a high and significantly positive linear correlation with NT-pro BNP levels. Interestingly, there was a dynamic escalation of difference in Troponin T and NT-pro BNP levels between the patients who died and those who recovered/discharged successfully. Both Troponin T and NT-pro BNP levels increased significantly during hospitalization in those who ultimately died, but no such dynamic changes of Troponin T or NT-pro BNP levels were evident in survivors. This study also revealed an important finding that the risk of mortality was higher in patients with elevated Troponin T and underlying cardiovascular disease compared to those with elevated Troponin T but without underlying cardiovascular disease.
Thus, it is evident that cardiac injury plays a significant role in the disease progression and outcome associated with COVID-19. Thus, it is reasonable to include the indicators of cardiac injury in the patient’s diagnosis, triaging, treatment, and prognosis, while recognizing that their abnormality may not be related to direct coronary involvement. The usefulness is enhanced among patients with prior cardiovascular disease. If we continue to ignore their importance, we are likely to miss a significant number of ischemic and non-ischemic causes of myocardial injury associated with COVID-19. Eventually, many patients are going to be mismanaged and deprived of potentially useful therapies like inotropes, vasopressors, and diuretics for heart failure, and perhaps immunosuppressants for myocarditis. The use of biomarker-based risk stratification may identify a substantial proportion of severe COVID-19 patients with normal or mildly elevated Troponin and BNP values (<3 times the upper limit of normal), thus avoiding the need for further cardiac consultation, electrocardiogram, and echocardiogram. This strategy will translate into lesser infection exposure to the cardiovascular team and a reduction in the need for additional PPE.
Therefore, in this COVID-19 era, we urge the cardiology community to stop using troponin just as a test to rule out myocardial infarction and to decide whether patients should be shifted for coronary angiography or not. Instead, we propose using both troponin and natriuretic peptides in all severe COVID-19 patients for risk stratification (as advised in our proposed algorithm), clinical decision making, rationale use of ECG/echocardiography, initiating aggressive treatment strategies, and for risk prognostication of the patients. Such an approach might enhance cardiovascular care among COVID-19 patients, as well as reduce the risk of infection exposure to the cardiovascular care team. However, future research is needed to validate whether cardiac biomarker testing improves triage, assists in treatment decisions, and alters outcomes.
Sources of funding
No specific funding was obtained for this study.
Disclosures
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Declaration of competing interest
Sir we declare that there is no conflict of interest involved and once accepted all the copyrights of this manuscript would stay with Diabetes & Metabolic Syndrome: Clinical Research & Reviews.
References
- 1.Mahajan K., Chandra K.S. Cardiovascular comorbidities and complications associated with coronavirus disease 2019 [published online ahead of print, 2020 May 27th] Med J Armed Forces India. 2020 doi: 10.1016/j.mjafi.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020 March 25th doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guo T., Fan Y., Chen M., Wu X., Zhang L., He T. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 March 27th doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American College of Cardiology Troponin and BNP use in COVID-19. https://www.acc.org/latest-in- cardiology/articles/2020/03/18/15/25/troponin- and-bnp-use-in-covid19 Available online at. Last accessed April 24th 2020.