Abstract
The humanity is currently facing the COVID-19 pandemic challenge, the largest global health emergency after the Second World War. During summer months, many countries in the northern hemisphere will also have to counteract an imminent seasonal phenomenon, the management of extreme heat events. The novelty this year concerns that the world population will have to deal with a new situation that foresees the application of specific measures, including adjunctive personal protective equipment (i.e. facemasks and gloves), in order to reduce the potential transmission of the SARS-CoV-2 virus. These measures should help to decrease the risk of the infection transmission but will also represent an aggravating factor to counteract the heat effects on the population health both at occupational and environmental level. The use of a specific heat health warning system with personalized information based on individual, behavioural and environmental characteristics represents a necessary strategy to help a fast adaptation of the population at a time where the priority is to live avoiding SARS-CoV-2 infection.
Keywords: Heat-health warning system, Heat-stress, SARS-CoV-2, Personal protective equipment, Facemask, Gloves
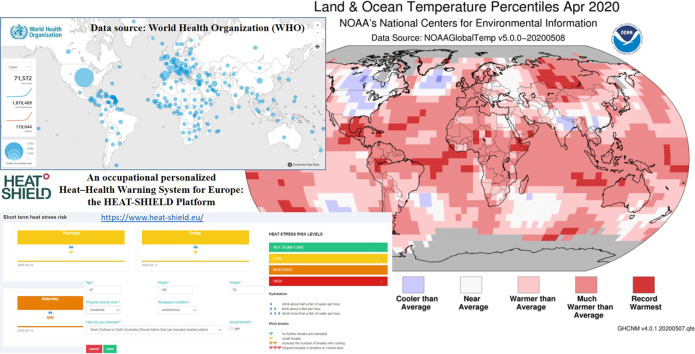
Graphical abstract
Highlights
-
•
WHO produced guidelines about the use of PPE to reduce the transmission of SARS-CoV-2.
-
•
The synergistic effect between heat and anti-COVID-19 measures must be studied.
-
•
Researchers must study how PPE behave when used in outdoor warm condition.
-
•
A PPE-inclusive customized heat-warning system is useful at the time of COVID-19.
-
•
Interventions to review HHWSs in the context of COVID-19 are strongly required.
1. Introduction
On March 11, 2020, the World Health Organization (WHO) announces COVID-19 outbreak as pandemic (WHO, 2020a), one of the largest global health emergencies after the Second World War. The world population is trying to manage this global emergency mainly by protecting human health and also trying in some way to contain the devastating health, economic and sociological effects. Often, as early as the month of May, many countries in the northern hemisphere (starting from those at lower latitudes) will also have to counteract an imminent seasonal phenomenon: the management of extreme heat events that, in the last two decades, is having devastating effects for the world population due to global warming (Mora et al., 2017), another global phenomenon that we are struggling to manage. According to the World Meteorological Organization (WMO), 2019 was the second warmest year and the last five years were the warmest on record (WMO, 2020).
The novelty this year concerns that, in many countries worldwide and depending on the National Government decisions, the whole population, therefore considering students, workers, unemployed, elderly, will have to deal with a new situation to which most people are not accustomed. In particular, the application of a series of specific measures to contain and to counteract the transmission of the SARS-CoV-2 virus are envisaged (WHO, 2020b; WHO, 2020c), including the often-mandatory use of various COVID-19-specific personal protective equipment (PPE-COVID-19) for carrying out several activities outside one's home (both outdoors and indoors) (Chu et al., 2020). The whole population will therefore have to use PPE-COVID-19, such as various types of facemasks (Eikenberry et al., 2020) and gloves available in different disposable materials (WHO, 2020c). In a recent study (Zhang et al., 2020), the authors concluded that the practice of wearing facemasks in public corresponds to the most effective means to prevent interhuman transmission and represents (in conjunction with simultaneous social distancing, quarantine, and contact tracing) the most likely fighting opportunity to stop the COVID-19 pandemic. These PPE are not designed and manufactured for large-scale use and above all are not designed to be used in the outdoor environment for long periods (ECDC, 2020). Based on the fabric thermal proprieties of insulating suits, and depending on the environmental thermal conditions, heat exchange between the body and the environment might be significantly limited or impeded, this way increasing the thermal stress of a person and leading to a decrement in physical performance capabilities and increased risk of heat-stress-related injuries (Xu et al., 2019). In the case of the general public, therefore, the effect of heat can lead to overloads in the healthcare system (Wondmagegn et al., 2019) and, in the situation of very high patient loads requiring intensive care due to the COVID-19 emergency, the capacity of health services and systems to prevent and manage heat stress may be compromised or unavailable. For workers significant impacts are expected on occupational safety and health (Marinaccio et al., 2019) and on their productivity (Kjellstrom et al., 2016; Flouris et al., 2018) with important economic impacts (Ma et al., 2019; Morabito et al., 2020). Forecast scenarios of climate change suggest considering the prevention of occupational exposure to heat waves a priority in occupational safety and health field.
A technical brief focused on the managing of heat risk during the COVID-19 pandemic, provided by the Global Heat Health Information Network (http://www.ghhin.org/), a system of experts spearheaded by the WHO and WMO Joint Office for Climate and Health, and the United States National Oceanic and Atmospheric Administration (NOAA), clearly stated that the ongoing COVID-19 pandemic amplifies the health risks of hot weather for many people (all people are potentially at risk of ill to both heat stress and COVID-19 if exposed). Then a double jeopardy is expected: people infected with, or recovering from, COVID-19 are presumed (as they are associated with acute kidney injury) more vulnerable to heat stress, including outdoor workers returning to the workplace. In general, the communities ravaged by COVID-19 also include people most vulnerable to extreme heat. In addition, due to COVID-19-related restrictions and policies to contain the pandemic, vulnerable populations may be in more precarious social and economic conditions for various reasons, including from lost wages, increasing isolation, incorrect or inaccurate information obtained through social media networks, and limiting healthcare access because difficulties in making movements with transportation (http://www.ghhin.org/assets/technical-brief-COVID-and-Heat-final.pdf). The more complex management of air conditioning and industrial ventilation systems (effective systems to combat the heat effects and for preventing workplace infection and ill health) for both residential and high occupancy buildings, further complicates the situation because these systems should be inspected, maintained, and cleaned more frequently (together with a frequent sanitization of surfaces) than in a typical summer condition to prevent COVID-19 transmission (Qian and Zheng, 2018). In addition, the use of fans for air circulation in collective spaces and in spaces with minimal outside air exchange should be avoided when several people are present in these spaces (http://www.ghhin.org/heat-and-covid-19/ac-and-ventilation).
It is therefore essential to coordinate with relevant authorities to integrate Heat-Health Action Plans (HHAPs) and specifically Heat-Health Warning Systems (HHWSs) in light of local COVID-19 context and even reviewing and adapting COVID-19 restrictions when significant aggravating impacts on local heatwave risks are expected. WHO/Europe (http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/5/preparing-for-a-long,-hot-summer-with-covid-19) recommends countries and regions to review existing HHAPs to take into consideration measures in place to reduce and prevent COVID-19 transmission. In addition, it is also urgent to comprehend quickly how PPE-COVID-19 behave when used by the general public in daily life and by workers, evaluating the consequences related to the management of heat stress at local (face and hands) and general (whole body) discomfort level, and identifying the most accurate measures for a correct use of PPE according to the type and duration of activity envisaged. The potential synergistic effect with the specific measures to contain and to counteract the transmission of the SARS-CoV-2 virus has to be carefully evaluated by treating specifically public and worker's health issues.
2. Public health issue
In the case of the general public, the study of the interaction between the heat and the PPE used can be very complex, since the population is characterized by a highly varied sample in terms of personal characteristics, age, gender, health status, the activity carried out and habits. Furthermore, the population did not have the opportunity to gradually adapt to this situation and had to use, suddenly and for the first time, various adjunctive PPE (especially masks and gloves) without having an accurate training on the correct use as already foreseen in many occupational areas. Wearing of facemasks among the general population was not mandated and was unpopular in most of the western world during the early outbreak of the pandemic (Zhang et al., 2020). The use of PPE-COVID-19, if carried out appropriately, always paying attention to compliance with adequate hygiene rules (Khan and Parab, 2020), will reduce the infection transmission risk but, at the same time, will certainly represent an aggravating factor to counteract the well-known and detrimental heat effects on the population health (Kovats and Ebi, 2006; Mora et al., 2017), with significant repercussions for the most heat-vulnerable people (Paterson and Godsmark, 2020; Linares et al., 2020). Especially older people when suffering from chronic diseases or living socio-economically disadvantaged (including those marginalized and isolated), people with disabilities, mental health issues, or living in crowded or poor quality housing conditions, people taking certain medications or recovering from previous illness, those who are overweight and obese, pregnant women, infants, children, ethnic minorities, but also people who have, or are recovering from, COVID-19 (which can be associated with acute kidney injury), represent the most vulnerable people to both heat stress and COVID-19 disease. In addition, the vulnerability of many people is further compounded in this generalized situation of fear of contagion caused by COVID-19 pandemic and people may be reluctant or may have greater problems moving because reducing access and options to use of transportation due to local COVID-19-related restrictions and policies, therefore they can be unable to reach cooling centres to counteract the heat stress or to seek emergency medical help.
For these reasons, some cities (i.e. the City of New York, https://www1.nyc.gov/office-of-the-mayor/news/350-20/mayor-de-blasio-covid-19-heat-wave-plan-protect-vulnerable-new-yorkers) are already organizing themselves to counter this situation identifying existing facilities that can be used as key cooling centres in high-risk communities, even planning to create non-traditional cooling centres in alternative sites (i.e. sports venues and auditoriums) and also organizing special non-congregate transportation for vulnerable people at high COVID-19 complication risk.
3. Worker's health issue
In many occupational areas (medical, agricultural, industrial, construction, transportation, tourism, etc.) the use of PPE-COVID-19 will also be associated with specific and mandatory typical PPE for specific tasks, for example works requiring contact with other sources of heat, chemicals, dust, etc.
In the case of some categories of workers (e.g. those involved in the healthcare sector and the management of infected people or contaminated materials, but not only) also facemask with filters, safety goggles, headphones, gowns or insulating suits equipped with a hood to protect the head against nuclear, chemical, biological and radiological (NCBR insulating suits) risks can be worn (Klompas et al., 2020). Consequently, especially outdoor workers or those working indoors without air conditioning or inadequately cooled conditions for long periods, even if engaged in generally pleasant thermal conditions (if dressed normally), can also experience critical thermal stress conditions if wearing various PPE, with significant dehydration depending also on the type, the duration of the work activity carried out and the time to recover before returning to work. With the aim to enhance the endurance and cognitive performance of workers while wearing PPE, they should lower their body's core temperature at the onset of work and should avoid its significant increase during work (Alhadad et al., 2019). In this case, the appropriate strategies of intervention must concern the thermal status of the worker at the beginning of the work (start work hydrated, cool and recover between shifts) and the behaviour during work addressed to reduce the rise of the body core temperature (i.e. revise work/rest schedules, reduce clothing layers underneath PPE, cool down during breaks prevalently in cool spots or shaded areas, improve efficiency of movements). Particular attention should also be payed to one's general health by improving thermal tolerance through acclimatization and own fitness (McLellan et al., 2013; Cheung et al., 2016).
4. Facemasks and gloves: local microclimate and heat stress
In this discussion paper, an exploratory revision of studies related to the microclimatic conditions that characterize the areas of the body covered by some adjunctive PPE (in particular facemasks and gloves), also evaluating local and global thermal stress, was carried out. This exploratory search was conducted through pre-specified search terms connected to the investigated topic and used by the PubMed database (focused on biomedical topics) and by the Semantic Scholar tool (A free, AI-powered tool for navigating the scientific literature) to identify useful studies without any limitation related to the year of publication. Although there is an urgent need to obtain information on the microclimate inside facemasks and gloves with detailed information on thermal stress at local and global level, the available and often-dated scientific literature (Martin and Callaway, 1974; Nielsen et al., 1987; Hayashi and Tokura, 2004; Li et al., 2005; Yip et al., 2005; Roberge et al., 2012) provides only a partial contribution on this topic.
In general, if gloves are used, the discomfort will be mainly local with profuse hand sweating depending on the environmental thermal conditions (particularly critical if exposed to the sun). In the case of the use of facemasks, which protect the mouth and nose, the limitation of the heat effects can be even more complex, and the situation could potentially become very critical. The hot and wet air cushion that will be created immediately under the mask, therefore in contact with the mouth and nose, will hinder the normal process of breathing. Several authors (Yip et al., 2005) explained that wearing a facemask for a certain period of time could increase the temperature inside the oral cavity by minimising the convection and evaporation of heat from the mouth to the surrounding. Particularly critical microclimatic conditions (very high temperatures and humidity rates, and total absence of ventilation) in contact with the mouth and nose will be created if exposed to heat sources and solar radiation. This situation negatively impacts respiratory and dermal mechanisms of human thermoregulation (Roberge et al., 2012) and, in addition, high temperature and humidity can produce adverse skin reaction such as contact dermatitis (Foo et al., 2006; Al Badri, 2017; Matusiak et al., 2020).
Furthermore, when people are exposed to hot conditions, the frequency of breathing tends to increase (also depending on the activity level) and thermal discomfort will not be only local (i.e. limited to the facial surface affected by the mask or in the surrounding areas) but it will be generalized to the whole human body. This aspect was already highlighted many years ago when several authors (Martin and Callaway, 1974; Nielsen et al., 1987) revealed that the use of protective facemask represented an additional factor aggravating heat stress and that the facemask air temperature significantly influenced the thermal sensations of the whole body. Hayashi and Tokura (2004) revealed that during some tests carried out in a climate chamber controlled at an air temperature of 28 °C and a relative humidity of 60%, both the air temperature and the absolute humidity inside the mask significantly increased in subjects wearing a mask made of non-woven fabric and without exhaust valve compared to subjects wearing a mask with exhaust valve. They concluded that preventing an excessive increase of microclimate temperature and humidity inside the facemask was fundamental to reduce the whole-body heat stress. Another study showed that wearing a facemask may increase the oral temperature in healthy subjects (Yip et al., 2005) while other authors (Li et al., 2005) revealed that different microclimates of N95 respirator and surgical facemasks significantly influenced the heart rate, the thermal stress and the subjective discomfort perception. On the basis of a review (Roberge et al., 2012), local dermal effects, increased temperature of breathing air, elevated core temperature, or psychophysiological responses, were identified as facial heat complaints negatively associated to the use of protective facemasks, including surgical facemasks. Just the latter have been widely distributed to the whole population in Italy as a measure to counteract the SARS-CoV-2 infection (however considering that many people organized themselves with homemade cloth masks or other improvised face coverings). They were prevalently the three-ply (three layers) single-use surgical masks (UNI EN 14683, 2019) or certified similar to the surgical ones made up of a melt-blown polymer, most commonly polypropylene, placed between non-woven fabrics. In some cases, also the FFP1 (generally used as a mask against powders and liquids without particular toxicity) or the N95 respirator (particulate-filtering facepiece respirator) facemasks could also be worn by the general public. While the FFP2 and FFP3 facemasks were generally used by healthcare workers and the staff engaged in intensive care respectively. The gloves usually used by the general population were often plastic or latex models.
However, the PPE for specific body parts distributed to the general population have not been tested for the microclimate and specifically for thermal stress. In fact, the performance requirements of the surgical facemasks (UNI EN 14683, 2019) include bacteria filtration efficiency, breathability, differential pressure, splash resistance, microbial cleaning and biocompatibility. Although the air permeability of the mask is measured by determining the pressure difference across the mask in specific conditions of air flow, temperature and humidity, no tests are specifically addressed to the microclimate and the evaluation of thermal comfort. Therefore, no reports on the thermophysiological responses in participants wearing masks in outdoor warm environments and directly exposed to solar radiation are available. Some authors (Roberge et al., 2012) have stated that the intolerance to the thermal effects of protective facemasks leads to decreased use and concomitant decreased protection for the user.
For this reason, as part of an Italian project (WORKLIMATE) we also started field trial tests specifically addressed to the interaction between the use of some PPE and the heat stress. In particular, several monitoring of different healthy people over an hour and during various activities (sedentary and walking) were carried out and various parameters (physiological and environmental), including microclimatic monitoring (temperature and humidity of the skin) inside the surgical facemask and latex gloves, were collected. Preliminary results revealed a rapid increase of the moisture content of the skin on the hands in the first 30 min of activity, reaching the saturation and then stabilizing. Considering 1 h-test average environmental temperatures varying between 22 and 27 °C, black globe temperature between 35 and 45 °C, relative humidity between 30 and 55% and calm wind (depending on the tests), both the air temperature and humidity inside the mask (the air between the mask and the skin) were significantly (p < 0.001) higher than the external ones (above 4 °C and 10% for air temperature and humidity respectively), revealing a general increase of the perceived thermal discomfort at local (face and hands) and global (whole body) level, further increasing if exposed to direct solar radiation. These findings are confirmed by the fact that the heat strain caused by PPE is a result of excess body heat storage which can be attributed to the combined effect of PPE characteristics, environmental conditions, and the level of physical activity (Xu et al., 2016).
It is therefore necessary to deepen these investigations by fully understanding the impact linked to the use of these indispensable adjunctive PPE (Eikenberry et al., 2020) on thermal stress at the local but also whole-body level, also using detailed simulations with multi-node thermo-physiological models. In this way it will be possible to develop effective adaptation measures to manage the heat stress while keeping the anti-COVID-19 measures as a priority.
5. Adaptation strategies to counteract the heat effect by keeping anti-COVID-19 procedures active
At the international level, there are few examples that go precisely in this direction. For example, as part of the ongoing European H2020 project (HEAT-SHIELD, https://www.heat-shield.eu/), a team of international experts with skills in the field of physiology, clothing science, medicine, meteorology, climatology and public health with particular attention to the occupational sector, developed a multilingual web-platform concerning a customized occupational heat-related warning system valid for all of Europe (Morabito et al., 2019). This already operational system allows to take into account the use of some PPE (not yet anti-COVID-19 facemasks and gloves) as well to provide personal daily maximum heat stress risk levels by using ISO-standard thermal stress approaches and behavioural suggestions (hydration and work breaks recommended) to be taken in the short term (5 days) together with long-term heat risk forecasts, up to 46 days, useful for planning working activities for employers, organizations and operators in charge of safeguarding health and productivity in various occupational areas. Another example is the ongoing EU ClimApp project (http://www.jpi-climate.eu/nl/25223441-ClimApp.html) which aims to translate climate service information into personalized warnings and adaptation strategies to cope with thermal stress (Petersson et al., 2019). Even this tool, which uses part of the knowledge acquired with the HEAT-SHIELD project, allows a personalization of the information considering also the physical work intensity (metabolic rate) and clothing thermal insulation data. The integration of multi-node thermo-physiological models with weather forecast data represents a future challenge to predict accurately thermal stress accounting for the impact of various PPE (such as masks and gloves) at local level and evaluating the potential impact on thermal stress at a whole-body level (Xu et al., 2016; Petersson et al., 2019). In this way it will be also possible to perform modelling analysis to predict specific endurance times under representative environmental conditions (Xu et al., 2016).
These and other tools that could be developed in other projects, e.g. in the Italian WORKLIMATE project which will continue the research to improve HHWSs and to carry out further case studies in various occupational areas, represent useful tools and strategies also helpful to plan a better management of these adjunctive PPE in hot conditions and a fast heat-related adaptation strategy for the general public at a time where the priority is to live avoiding SARS-CoV-2 infection. These are particularly useful interventions in light of the fact that based on a recent scientific evidence (Zhang et al., 2020) the use of facemasks in public represents one of the most effective measures to stop the COVID-19 pandemic, and then to face and manage other future health emergencies that will require similar measures. Another important aspect that will be investigated in the project will be the perception of heat risk and how it will interconnect with the perception of the COVID-19 risk (Cori et al., 2020). These aspects may be useful in planning communication actions for the health and safety of workers and more generally of the population.
With the aim to be able to integrate the essential measures against the spread of COVID-19 and those to counter the known heat-stress effects, it will therefore be necessary to review also the previous HHWSs and planning the use of personalized ones (Table 1 ). Personalized information, based on individual (e.g. weight, height, age), behavioural (type of activity carried out and clothing worn) characteristics, and depending on the environment and occupational situation (if outdoors exposed to the sun or in shaded areas, or indoors), are able to provide useful advices (in terms of recommended breaks, rests in shaded areas, hydration, management of shifts and working hours, distribution of the various tasks breaks, etc.) that aim to alleviate the heat-stress situation. In this way, it will be possible to avoid health complications for the general population and in particular in subjects with chronic diseases (i.e. lung diseases) with consequent overloads of healthcare systems, and to allow the continuation of work activities taking appropriate precautions, also reducing the productivity losses and economic consequences.
Table 1.
Suggested interventions to review Heat-Health Warning Systems in the context of COVID-19. The information contained in this table has also been partially updated based on recent recommendations provided by the Global Heat Health Information Network (http://www.ghhin.org/heat-and-covid-19).
| Suggested interventions to review Heat-Health Warning Systems in the context of COVID-19 | |
|---|---|
| Intervention | Characteristics of interventions |
| Adjust advisory thresholds considering additional vulnerabilities due to COVID-19. | Adjustments of both epidemiological (based on human health outcomes, i.e. mortality, hospitalization, work injury data, etc.) and biometeorological (based on various heat-stress-related indicators) thresholds. This may lead to rise the warning risk level (yellow → orange; orange → red) compared to the pre-COVID-19 situation. |
| Customize the determination of whether an “action trigger” is likely to be exceeded in the near future. | Customization based on personal characteristics (e.g. weight, height, age), the type of activity carried out, the clothing worn (including the use of various PPE-COVID-19), depending on the environment (outdoors exposed to the sun or in shaded areas, indoors) and the occupational situation (contact with other sources of heat). |
| Adjust the issuance of heat warning messages varying it between different population target. | For the general public:
|
| Coordinate public messaging with relevant authorities. | Evaluate to review COVID-19 restrictions by coordinating across different levels of government and various stakeholders when high heat-risk levels are forecasted and minimize the risk of heatwave information contradicting COVID-19 messaging. |
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This study received funding from the European Union's Horizon 2020 research and innovation programme under grant agreement No. 668786, as part of the Project “Integrated inter-sector framework to increase the thermal resilience of European workers in the context of global warming” (HEAT-SHIELD). Members of the WORKLIMATE Collaborative Group: Alessandra Binazzi, Michela Bonafede, Alfonso Crisci, Francesca de'Donato, Tiziana Falcone, Simona Del Ferraro, Bernardo Gozzini, Valentina Grasso, Daniele Grifoni, Miriam Levi, Alessandro Marinaccio, Alessandro Messeri, Paola Michelozzi, Vincenzo Molinaro, Stefano Monti, Marco Morabito, Antonio Moschetto, Pietro Nataletti, Francesco Pasi, Emma Pietrafesa, Iole Pinto. The authors thank NOAA's National Centers for Environmental Information (NCEI) for providing the global temperature for April 2020 (https://www.ncei.noaa.gov/news/global-climate-202003) and the WHO for providing COVID-19 disease map at 15 April 2020 (https://who.sprinklr.com/) needed to create the graphical abstract.
Editor: Scott Sheridan
References
- Al Badri F.M. Surgical mask contact dermatitis and epidemiology of contact dermatitis in healthcare workers. Curr. Allergy Clin. Im. 2017;30:183–188. [Google Scholar]
- Alhadad S.B., Tan P.M., Lee J.K. Efficacy of heat mitigation strategies on core temperature and endurance exercise: a meta-analysis. Front. Physiol. 2019;10:71. doi: 10.3389/fphys.2019.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung S., Lee J.K.W., Oksa J. Thermal stress, human performance and physical employment standards. Appl. Physiol. Nutr. Metab. 2016;41:S148–S164. doi: 10.1139/apnm-2015-0518. [DOI] [PubMed] [Google Scholar]
- Chu D.K., Akl E.A., Duda S., Solo K., Yaacoub S., Schünemann H.J., COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020 doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cori L., Bianchi F., Cadum E., Anthonj C. Risk perception and COVID-19. Int. J. Environ. Res. Public Health. 2020;17:3114. doi: 10.3390/ijerph17093114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ECDC (European Centre for Disease Prevention and Control) Using face masks in the community - reducing COVID-19 transmission from potentially asymptomatic or pre-symptomatic people through the use of face masks. Technical report, Stockholm (Sweden) 2020. https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-use-face-masks-community.pdf
- Eikenberry S.E., Mancuso M., Iboi E., Phan T., Eikenberry K., Kuang Y., Kostelich E., Gumel A.B. To mask or not to mask: modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect. Dis. Model. 2020 doi: 10.1016/j.idm.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flouris A.D., Dinas P.C., Ioannou L.G., Nybo L., Havenith G., Kenny G.P., Kjellstrom T. Workers' health and productivity under occupational heat strain: a systematic review and meta-analysis. Lancet Planet Health. 2018;2:e521–e531. doi: 10.1016/S2542-5196(18)30237-7. [DOI] [PubMed] [Google Scholar]
- Foo C.C., Goon A.T., Leow Y.H., Goh C.L. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome – a descriptive study in Singapore. Contact Dermatitis. 2006;55:291–294. doi: 10.1111/j.1600-0536.2006.00953.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi C., Tokura H. The effects of two kinds of mask (with or without exhaust valve) on clothing microclimates inside the mask in participants wearing protective clothing for spraying pesticides. Int. Arch. Occup. Environ. Health. 2004;77:73–78. doi: 10.1007/s00420-003-0472-3. [DOI] [PubMed] [Google Scholar]
- Khan M.M., Parab S.R. Safety guidelines for sterility of face shields during COVID 19 pandemic. Indian J Otolaryngol Head Neck Surg. 2020 doi: 10.1007/s12070-020-01865-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kjellstrom T., Briggs D., Freyberg C., Lemke B., Otto M., Hyatt O. Heat, human performance, and occupational health: a key issue for the assessment of global climate change impacts. Annu. Rev. Public Health. 2016;37:97–112. doi: 10.1146/annurev-publhealth-032315-021740. [DOI] [PubMed] [Google Scholar]
- Klompas M., Morris C.A., Sinclair J., Pearson M., Shenoy E.S. Universal masking in hospitals in the Covid-19 era. N. Engl. J. Med. 2020;382:e63. doi: 10.1056/NEJMp2006372. [DOI] [PubMed] [Google Scholar]
- Kovats R.S., Ebi K.L. Heatwaves and public health in Europe. Europ. J. Pub. Health. 2006;16:592–599. doi: 10.1093/eurpub/ckl049. [DOI] [PubMed] [Google Scholar]
- Li Y., Tokura H., Guo Y.P., Wong A.S., Wong T., Chung J., Newton E. Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. Int. Arch. Occup. Environ. Health. 2005;78:501–509. doi: 10.1007/s00420-004-0584-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linares C., Díaz J., Negev M., Martínez G.S., Debono R., Paz S. Impacts of climate change on the public health of the Mediterranean Basin population - current situation, projections, preparedness and adaptation. Environ. Res. 2020;182 doi: 10.1016/j.envres.2019.109107. [DOI] [PubMed] [Google Scholar]
- Ma R., Zhong S., Morabito M., Hajat S., Xu Z., He Y., Bao J., Sheng R., Li C., Fu C., Huang C. Estimation of work-related injury and economic burden attributable to heat stress in Guangzhou, China. Sci. Total Environ. 2019;666:147–154. doi: 10.1016/j.scitotenv.2019.02.201. [DOI] [PubMed] [Google Scholar]
- Marinaccio A., Scortichini M., Gariazzo C., Leva A., Bonafede M., De’ Donato F.K., Stafoggia M., Viegi G., Michelozzi P., BEEP Collaborative Group Nationwide epidemiological study for estimating the effect of extreme outdoor temperature on occupational injuries in Italy. Environ. Int. 2019;133(Pt A) doi: 10.1016/j.envint.2019.105176. [DOI] [PubMed] [Google Scholar]
- Martin H., Callaway S. An evaluation of the heat stress of a protective face mask. Ergonomics. 1974;17:221–231. doi: 10.1080/00140137408931341. [DOI] [PubMed] [Google Scholar]
- Matusiak Ł., Szepietowska M., Krajewski P., Białynicki-Birula R., Szepietowski J.C. Inconveniences due to the use of face masks during the COVID-19 pandemic: a survey study of 876 young people. Dermatol. Ther. 2020 doi: 10.1111/dth.13567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan T.M., Daanen H.A., Cheung S.S. Encapsulated environment. Comprehensive Physiology. 2013;3:1363–1391. doi: 10.1002/cphy.c130002. [DOI] [PubMed] [Google Scholar]
- Mora C., Dousset B., Caldwell I.R., Powell F.E., Geronimo R.C., Bielecki C.R., Counsell C.W.W., Dietrich B.S., Johnston E.T., Louis L.V., Lucas M.P., McKenzie M.M., Shea A.G., Tseng H., Giambelluca T.W., Leon L.R., Hawkins E., Trauernicht C. Global risk of deadly heat. Nat. Clim. Chang. 2017;7:501–506. doi: 10.1038/nclimate3322. [DOI] [Google Scholar]
- Morabito M., Messeri A., Noti P., Casanueva A., Crisci A., Kotlarski S., Orlandini S., Schwierz C., Spirig C., Kingma B.R., Flouris A.D., Nybo L. An occupational heat–health warning system for Europe: the HEAT-SHIELD platform. Int. J. Environ. Res. Public Health. 2019;16:2890. doi: 10.3390/ijerph16162890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morabito M., Messeri A., Crisci A., Bao J., Ma R., Orlandini S., Huang C., Kjellstrom T. Heat-related productivity loss: benefits derived by working in the shade or work-time shifting. Int. J. Prod. Perform. Manag. 2020 doi: 10.1108/IJPPM-10-2019-0500. [DOI] [Google Scholar]
- Nielsen R., Berglund L.G., Gwosdow A.R., Dubois A.B. Thermal sensation of the body as influenced by the thermal microclimate in a face mask. Ergonomics. 1987;30:1689–1703. doi: 10.1080/00140138708966058. [DOI] [PubMed] [Google Scholar]
- Paterson S.K., Godsmark C.N. Heat-health vulnerability in temperate climates: lessons and response options from Ireland. Glob. Health. 2020;16:29. doi: 10.1186/s12992-020-00554-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersson J., Kuklane K., Gao C. Is there a need to integrate human thermal models with weather forecasts to predict thermal stress? Int. J. Environ. Res. Public Health. 2019;16:4586. doi: 10.3390/ijerph16224586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian H., Zheng X. Ventilation control for airborne transmission of human exhaled bio-aerosols in buildings. J. Thorac. Dis. 2018;10:S2295–S2304. doi: 10.21037/jtd.2018.01.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberge R.J., Kim J.-H., Coca A. Protective facemask impact on human thermoregulation: an overview. Ann. Occup. Hyg. 2012;56:102–112. doi: 10.1093/annhyg/mer069. [DOI] [PubMed] [Google Scholar]
- UNI EN 14683 . European Committee for Standardization, CEN-CENELEC Management CentreCEN-CENELEC Management Centre, Rue de la Science 23, B-1040 Brussels. 2019. Medical face masks - requirements and test methods. [Google Scholar]
- WHO WHO director-General's opening remarks at the media briefing on COVID-19 - 11 march 2020. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- WHO . World Health Organization; Geneva: 2020. Infection Prevention and Control during Health Care when COVID-19 Is Suspected - Interim Guidance, Updated March 2020. (WHO Ref. N.: WHO/2019-nCoV/IPC/2020.3) [Google Scholar]
- WHO . World Health Organization; Geneva: 2020. Advice on the Use of Masks in the Context of COVID-19 - Interim Guidance, Updated June 2020. (WHO Ref. N.: WHO/2019-nCov/IPC_Masks/2020.4) [Google Scholar]
- WMO WMO confirms 2019 as second hottest year on record. Press release number: 01/15/2020. 2020. https://public.wmo.int/en/media/press-release/wmo-confirms-2019-second-hottest-year-record
- Wondmagegn B.Y., Xiang J., Williams S., Pisaniello D., Bi P. What do we know about the healthcare costs of extreme heat exposure? A comprehensive literature review. Sci. Total Environ. 2019;657:608–618. doi: 10.1016/j.scitotenv.2018.11.479. [DOI] [PubMed] [Google Scholar]
- Xu X., Gonzalez J.A., Santee W.R., Blanchard L.A., Hoyt R.W. Heat strain imposed by personal protective ensembles: quantitative analysis using a thermoregulation model. Int. J. Biometeorol. 2016;60:1065–1074. doi: 10.1007/s00484-015-1100-0. [DOI] [PubMed] [Google Scholar]
- Xu X., Rioux T.P., Pomerantz N., Tew S., Blanchard L.A. Heat strain in chemical protective ensembles: effects of fabric thermal properties. J. Therm. Biol. 2019;86 doi: 10.1016/j.jtherbio.2019.102435. [DOI] [PubMed] [Google Scholar]
- Yip W.L., Leung L.P., Lau P.F., Tong H.K. The effect of wearing a face mask on body temperature. Hong Kong Journal of Emergency Medicine. 2005;12:23–27. doi: 10.1177/102490790501200102. [DOI] [Google Scholar]
- Zhang R., Li Y., Zhang A.L., Wang Y., Molina M.J. Identifying airborne transmission as the dominant route for the spread of COVID-19. PNAS. 2020 doi: 10.1073/pnas.2009637117. [DOI] [PMC free article] [PubMed] [Google Scholar]