Abstract
Objective
Higher level impairments and activity limitation among those scheduled for total knee arthroplasty (TKA) is known. Sex differences in participation restriction which is the final domain of disablement pathway is not known. No data from developing countries exist on sex differences in disability levels at the time of TKA.
Methods
In a cross‐sectional analysis of 240 patients (188 women; 72 men) scheduled for TKA, impairment (pain, symptoms, quadricep muscle strength, and knee range of motion [ROM]), activity limitation (self‐reported and objective performance‐based measurements), and participation restriction were compared. Multivariable regression analyses were used to adjust for key sociodemographic and clinical characteristics. Associations between impairments and participation restriction were analyzed.
Results
Compared with men, women were more likely to have higher levels of impairment (knee injury and osteoarthritis outcome pain score adjusted mean difference [aMD]: −6.9 [95% confidence interval {CI} −13.7 to −0.18]; flexion ROM of less than 100° adjusted odds ratio: 5.7 [95% CI 1.6‐20.3]; and 36% lower muscle strength [95% CI 24%‐49%]) and lower objectively measured functional ability (walking speed aMD: −0.12 m/s [95% CI −0.23 to −0.02]; stair climbing time aMD: 9.5 s [95% CI 1.5‐17.5]). Participation restriction was higher in women compared with men. Of the impairment measures (pain, ROM, and muscle strength), pain contributed to participation restriction in both sexes.
Conclusion
This study demonstrated higher levels of disability in women than in men at the time of TKA. Effect of pain on participation restriction was higher compared with muscle strength and ROM. Evidence of delay in decision‐making to undergo TKA and reasons for delay need to be studied specifically in the context of lower middle–income countries.
Significance & Innovations.
In a sample of 240 patients from India scheduled for total knee arthroplasty, after adjusting for several confounders, women presented with higher levels of disability than men.
The study also showed the impairment measure (pain, muscle strength, and range of motion) of knee pain to be most important factor in the disability pathway in both sexes.
The present study is the first in India to report the patient‐important outcomes and the differences between men and women at the time of surgery. These findings are clinically relevant because they highlight the need consider sex differences in future presurgical interventions and during presurgery counseling.
Introduction
Osteoarthritis (OA) of the hip and knee is ranked as the 12th highest contributor to global disability and the 38th highest contributor in disability‐adjusted life years (DALYs) (1). Women are at a higher risk of developing OA and have a greater prevalence of the disease than men (4794 cases vs. 3145 cases per 100000 persons globally and 4276 cases vs. 2513 cases per 100 000 persons in India) (2). DALYs due to OA are also higher in women than in men (151.4 vs. 100.2 per 100 000 persons globally and 133.9 vs.79.9 per 100 000 persons in India) (2). Total knee arthroplasty (TKA) is the gold‐standard treatment for end stage OA and improves function (3, 4) and quality of life (QoL) (5, 6). The dramatic increase in utilization of TKA over the last two decades is well documented both in developed (7, 8) and developing countries (9). This increase can be attributed to the rising epidemic of obesity, increased life span, higher acceptability for this procedure, and broadening indications for TKA (10). More women undergo arthroplasty worldwide, but they may differ in important ways from men undergoing the procedure.
Several biological reasons have been proposed to explain the higher susceptibility to OA and faster disease progression (11) in women compared with men. Despite the sex differences in pathophysiology of OA, at the time of scheduling for TKA, it is expected that men and women have similar levels of disability. However, previous studies (12, 13, 14, 15) have demonstrated higher levels of impairments and functional limitations in women than in men among those scheduled for TKA. Delayed care‐seeking and delayed treatment among women for OA (16) as well as several other health conditions have been previously documented (17, 18, 19). Higher disability among those scheduled for TKA could be due to more than just biological reasons (20).
Although sex differences among those scheduled for TKA have been shown previously, there are certain gaps in previous evidence. First, sex differences in impairments and functional limitations at the time of surgery have not been studied in developing countries such as India, where sociocultural norms (21) are considerably different from those in developed countries. Hence, generating this evidence on the magnitude of sex differences in impairments, functional (activity) limitation is more likely to change practice and improve quality of care in developing countries.
Second, in defining overall health and any health‐related condition, the World Health Organization‐International classification of functioning, disability, and health (ICF) recommends assessment of impairments in body structure and function, activity limitation, and participation restriction (22). Of the three domains, sex disparity in participation restriction, which is defined as “an individual's involvement in daily situations” (23), has not been studied. This is important because women tend to neglect symptoms and functional decline, until it becomes unbearable or affects their ability to cope with their routine work (17, 18, 19). Hence, it is possible that given the local sociocultural norms, women may have higher levels of impairments with less effect on participation in routine activities compared with men at the time of surgery. Collecting information on all three domains will help to explore whether association of knee impairments with participation restriction vary by sex.
Finally, previous studies on this topic have not adjusted for potential confounders that might have overestimated the sex differences. Therefore, the differences in impairments and functioning ability previously demonstrated (12, 13, 14, 15) may in part be due to the effect of potential variables such as social support, education, and comorbidities.
The primary objective of this cross‐sectional analysis was to compare impairments, activity limitation, and participation restriction between men and women scheduled for TKA, after adjusting for relevant confounders. We hypothesized that women would have poorer outcomes compared with men. Secondary objectives were to evaluate the contribution of impairment parameters (pain, range of motion [ROM], and quadricep muscle strength) on participation restriction and to explore if sex moderated the association between impairments and participation restriction. We hypothesized that participation restriction due to impairments would have a smaller effect on women than on men.
Patients and Methods
Study setting
Data analyzed for this study were part of the baseline assessment from a prospective cohort study conducted at an academic referral government‐funded hospital in New Delhi, India. Only the cost of the prosthesis was borne by the individual.
Study participants
Consecutive patients aged 18 years or greater of both sexes who were admitted to the hospital to undergo unilateral/bilateral TKA for primary degenerative OA were invited to participate in this cohort study. We excluded individuals with serious terminal illness, severe visual or hearing defects, or cognitive dysfunction and those undergoing revision TKA, TKA indicated for rheumatoid arthritis, or planned unicompartment knee arthroplasty. Consenting eligible patients who lived in the city and neighboring states and who were able to return for follow‐up after surgery at 6 months and 1 year were enrolled. Participants were to be operated on by two experienced surgeons and were admitted to the hospital 1 or 2 days before the surgery. The study protocol was approved by the institutional review boards of All Indian Institute of Medical Sciences‐New Delhi (IEC‐351/01 .07.2016, RP‐15/2016), Indian Institute of Public Health‐Delhi (IIPHD‐IEC‐03‐2016), and Deakin University (2016‐252). This cohort study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline (24). The data sets analyzed during the current study are available from ND on reasonable request.
Data collection
Following written informed consent, information on sociodemography (age, sex, literacy, employment, and living situation with extended family) and clinical characteristics (duration of symptoms, comorbidity, other bodily pain, and use of pain medication and other alternative therapies) were collected from study participants. Impairment measures included pain, ROM, and knee extensor strength of both limbs. Activity limitation was measured using self‐reported and objective performance‐based assessments as recommended by the Osteoarthritis Research Society (25). Participation restriction was measured using a self‐reported tool. Questionnaires were administered and assessments were made by a trained physical therapist independently of the operating surgeons.
Impairment measures
Knee pain and symptoms
The pain (nine items) and symptom (seven items) subdomains of the Hindi version of the validated knee injury and osteoarthritis outcome score (KOOS) questionnaire (26) was administered, and the normalized scores for pain and symptom ranged from 0 to 100, with 0 meaning worst health state.
Range of motion
Active flexion of both knees were measured using a digital goniometer (Therapy Plus Digital Goniometer 360°, Scientific Solutions) in supine position (27). Considering that at least 100⁰ flexion ROM is required for walking, stair climbing, and standing from a seated position, participants with flexion ROM of less than 100⁰ in either of the limbs were categorized as having restricted ROM.
Knee extensor muscle strength
The maximum voluntary isometric contraction (MVIC) of the knee extensor was measured in N using a handheld dynamometer (model 01165, Lafayette Instrument Company), with the participant in a supine position (28). The knee joint was maintained at flexion of 30⁰ using a firm bolster placed under the knee, and the less affected limb was measured first. Three measurements were taken, and the higher of the last two was considered for analysis. MVIC was normalized for body mass index (BMI). Because all participants were diagnosed with bilateral OA, the average normalized muscle strength of both limbs was calculated.
Activity limitation
Self‐reported activity limitation
The activities of daily living (ADLs) domain of the KOOS (26) questionnaire, consisting of 17 items, was used to measure limitations to self‐care. The level of lower extremity–related physical activity was measured using lower extremity activity scale (LEAS), which is a single item questionnaire with 18 options (1 indicates the patient is restricted to bed all day; 18 = indicates the patient participates in relaxed physical activity every day or in competitive‐level sports). Participants were asked to choose one item that described their current activity level. This is a validated tool for assessing activity level in patients undergoing joint replacement (29) (ICC = 0.91 and a correlation (r) = 0.79 against a pedometer) (30). Although we discuss LEAS under the activity limitation domain, this is a hybrid tool that overlaps with participation restriction.
Performance‐based objective measures
The minimum core set of physical functional assessments as recommended by the OA Research Society International (25) were conducted as per standardized procedures (31), in the following order: 30‐s chair stand test (CST), timed up and go (TUG), 40‐m fast‐paced walk test, and stair climb test (SCT). The CST is a test of lower‐body strength and dynamic balance. We counted the number of repetitions the participant was able to perform in 30 s using a chair of 44‐cm height. The same chair was used to measure TUG, which is a transition test for ambulatory activity. Here, the participant was asked to rise from the chair, walk 3 m at their regular pace, turn around, return to the chair, and sit back in it. The use of arm rests or placement of hands on thighs for support were recorded. The 40‐m fast‐paced walk test was conducted by asking participants to walk as fast as possible for 20 m and to turn around to walk back to the starting position. Timing was paused while the participant turned around. The SCT is a test of lower‐body strength and balance. Time taken to climb up and down 11 steps of 16‐cm height was recorded. Use of an assistive device or handrails while ascending and descending was also documented.
Participation restriction
The late‐life disability instrument (LLDI) (32) is a recommended tool for measuring level of participation restriction in this patient population (22). The LLDI has two dimensions: the frequency of performing socially defined life tasks and the limitation in capability of performing various social, community, and personal tasks. Scaled scores of each dimension ranged between 0 and 100 (100 indicates the highest participation level).
Confounders
The variables that could act as confounders (12, 13, 33, 34, 35, 36, 37, 38) were sociodemographic characteristics, namely age (in years), literacy (no formal education, schooling, and graduation and above), current employment status (working/retired or never worked), living in a nuclear or extended family, and socioeconomic scale (SES). SES was an unweighted total of six parameters (possession of a cellphone, possession of a personal computer, possession of a car, possession of air conditioning, house ownership, and possession of patient's own separate room in the household) (39). Clinical characteristics were BMI (in kg/m2), comorbidity, presence of other chronic musculoskeletal pain (self‐reported), history of TKA for the other limb, and current analgesic intake. Medical history, including diagnosed hypertension, diabetes mellitus, chronic respiratory illness, and hypothyroidism at the time of surgery, was obtained from medical records and recoded as none, one, or more than one comorbidity. Information on any non–knee‐related chronic self‐reported musculoskeletal ailments or bodily pain and analgesic intake was collected during the interview with the participant.
Power calculation
This was an exploratory analysis using baseline data from a prospective cohort study, and thus pre hoc sample size estimation was not calculated for this objective. However, a sample of 240 participants would have more than 90% power to detect an effect size (Cohen's f) as small as 0.05 (difference in disability outcomes between men and women) with a 5% α with at least 10 covariates in the regression model.
Statistical methods
Participant characteristics and outcome measures on a continuous scale are described using means and SD or median and interquartile range (IQR). Categorical variables are reported as frequencies and percentages. All continuous measures of impairments (KOOS‐Pain and KOOS‐Symptoms), activity limitation (KOOS‐ADL, LEAS, CST, SCT, and walking speed), and participation restriction (limitation and frequency dimension) were normally distributed. Average MVIC of knee extensors and TUG were right‐skewed and analyzed on a logarithmic scale. There were missing observations for SCT in 74 patients (31%), walk speed in 35 patients (15%) and TUG in 16 patients (7%). The reasons for missing were refusal (47 for SCT, 16 for walking, and 5 for TUG) and inability to perform (27 for SCT, 19 for walking, and 11 for TUG). Hence, these missing values were imputed using multiple chained imputations (multiple imputation Stata package, StataCorp). For CST, the missing data were only 2%; hence complete case analysis was performed. All analyses were performed using Stata 15.
Differences between men and women in impairments (pain, symptoms, and ROM and MVIC of knee extensors), activity limitation (KOOS‐ADL, LEAS, and four performance measures), and participation restriction as defined by the two dimensions of LLDI (limitation and frequency) were analyzed using univariable analysis followed by multivariable regression adjusting for all covariates. ROM (less than 100⁰ flexion ROM in either of the knees vs. 100⁰ or more flexion ROM) was analyzed using logistic regression. Departure from linearity was tested for all continuous independent variables. Presence of multicollinearity between covariates was checked, and model assumptions were tested by assessing the normality of the residuals. Adjusted β coefficients (mean differences [MDs] and adjusted odds ratios [aORs]) along with 95% confidence intervals (95% CIs) are reported. A P value of less than 0.05 was considered a statistically significant association, and no adjustments were done for multiple comparisons. Standardized mean differences adjusted for covariates were plotted to compare the group (men and women) differences across outcomes of varying units. A standardized MD of 0.2 is considered a small effect, an MD of 0.5 is considered a medium effect, and an MD of 0.8 is considered a large effect (40).
Regression analyses were undertaken to explore associations of the impairment measure (pain, average flexion ROM of both knees, average MVIC of the quadriceps of both knees) with the two dimensions of participation restriction. The same set of confounders as stated above were included in each of these models. The coefficients of determinants (R 2) are reported along with the unstandardized β coefficient to compare the proportions of variation in the outcome explained by each of the impairment measure. An interaction term was added between the impairment measure and sex to assess if the relationship between impairment and participation restriction was modified by sex. A P value of less than 0.05 was considered significant for the interaction test.
Results
Between January 2017 and April 2019, 556 consecutive patients assigned for knee arthroplasty were screened for eligibility. Of the total screened, 79% were eligible, with 54% of these enrolling into the cohort. Reasons for ineligibility and nonrecruitment of eligible participants are presented in Figure 1.
Figure 1.
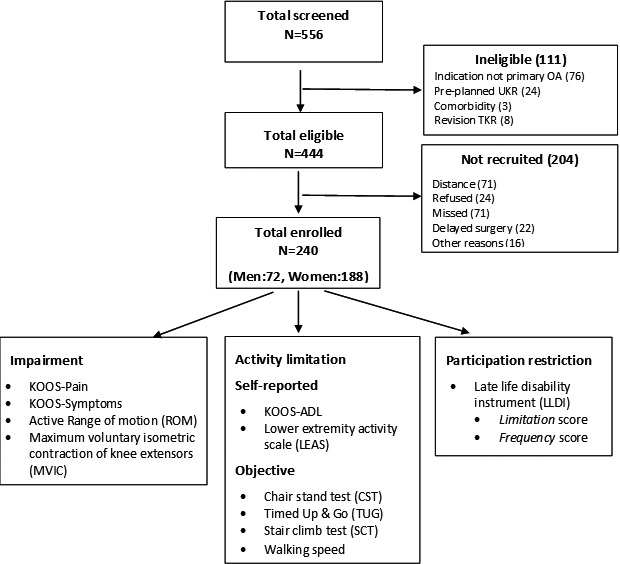
Participant recruitment and parameters measured. ADL, activities of daily living; KOOS, knee injury and osteoarthritis outcomes score; OA, osteoarthritis; TKR total knee replacement; UKR, Unicompartment knee replacement.
Descriptive characteristics
A total of 240 participants (70% women; mean BMI: 287 kg/m2; mean duration of symptom: 8.1 y) were enrolled. Sociodemographic and clinical characteristics of the overall sample and the separate sexes are reported in Table 1. Women were slightly younger, had higher BMIs, were less likely to have received formal education, and were less likely to have been formally employed when compared with men.
Table 1.
Sociodemographic and clinical characteristics of patients scheduled for TKA
| Participant characteristics | All (N = 240) | Men (n = 72) | Women (n = 188) | P a |
|---|---|---|---|---|
| Sociodemographic | ||||
| Age, mean (SD), y | 64 (8.0) | 66.8 (8) | 62.8 (7.7) | 0.003 |
| BMI, mean (SD), kg/m2 | 28.7 (5) | 26.9 (3.9) | 29.5 (5.2) | 0.003 |
| Education, n (%) | ||||
| No schooling | 34 (14.2) | 4 (5.6) | 30 (17.9) | <0.001 |
| Schooling (primary/high school) | 101 (42.1) | 23 (32) | 78 (46.4) | <0.001 |
| Graduation/postgraduation | 105 (43.8) | 45 (62.5) | 60 (35.7) | <0.001 |
| Socioeconomic scale (0‐6), mean (SD) | 4.03 (1.4) | 4.11 (1.5) | 4 (1.4) | 0.6 |
| Currently working, n (%) | 47 (19.6) | 33 (45.8) | 14 (8.3) | <0.001 |
| Living in nuclear family, n (%) | 101 (42.1) | 25 (34.7) | 76 (42.1) | 0.13 |
| Clinical | ||||
| Underwent TKA for other limb, n (%) | 26 (10.8) | 12 (16.7) | 14 (8.3) | 0.06 |
| Symptom duration, mean (SD), y | 8.1 (4.8) | 7.6 (5.3) | 8.3 (4.6) | 0.32 |
| Currently on, n (%) | ||||
| Pain medication | 170 (70.8) | 44 (62.1) | 126 (75.0) | 0.03 |
| Physiotherapy | 154 (64.2) | 45 (62.5) | 109 (62.5) | 0.72 |
| Alternative therapies b | 116 (48.3) | 33 (45.8) | 83 (49.4) | 0.61 |
| Comorbidities, n (%) | ||||
| 0 | 84 (35.0) | 32 (44.4) | 52 (31.0) | <0.001 |
| 1 | 93 (38.8) | 27 (37.5) | 66 (39.3) | <0.001 |
| 2‐4 | 63 (26.3) | 13 (18.1) | 50 (29.8) | <0.001 |
| Chronic musculoskeletal pain, c n (%) | 113 (47.1) | 32 (44.4) | 81 (48.2) | 0.50 |
| Primary reason for surgery, n (%) | ||||
| Cannot tolerate pain | 51 (21.3) | 17 (23.6) | 34 (20.2) | <0.001 |
| Walk without limping | 147 (61.3) | 42 (58.3) | 105 (62.5) | <0.001 |
| Want to perform daily activities | 39 (16.3) | 12 (16.7) | 27 (16.1) | <0.001 |
| Doctor recommended | 3 (1.3) | 1 (1.4) | 2 (1.2) | <0.001 |
| Bilateral TKA, n (%) | 108 (45.0) | 33 (45.8) | 75 (44.6) | 0.86 |
Abbreviation: BMI, body mass index; TKA, total knee arthroplasty.
P values were derived from unpaired t test for continuous variables and χ2 test for categorical variables.
Yoga, Ayurveda, homeopathy, Unani, Siddha, naturopathy, or acupuncture.
Chronic back pain (n = 68), shoulder pain (n = 19), spinal‐related pain (spondylolisthesis, radiculopathies, etc) (n = 22), other pain (n = 15), and pain in more than one site have been reported, so this will not add up to 113.
Most patients (65%) had at least one comorbidity, with hypertension being the most common (57.7%), followed by diabetes mellitus (21.7%). The main reason for undergoing surgery was wanting to walk without a limp (61%), followed by unbearable pain (21%); this did not vary with age (P = 0.60) or sex (P = 0.75).
Bilateral OA was diagnosed in all 240 participants, and 26 had undergone TKA of the other limb at least 6 months before enrollment. Forty‐five percent were scheduled for bilateral TKA. Most participants were on pain medication (71%), and 64% were advised to use some form of physical therapy. Complementary and alternative medicines/therapy for OA were used by half of the participants. Approximately 50% of the participants had chronic musculoskeletal‐related pain other than that in the knee joints.
Sex differences with impairment, activity limitation, and participation restriction
All unadjusted comparisons between men and women for impairment measures, self‐reported and objectively measured activity limitation, and participation restriction were statistically significant, with women faring worse than men. However, after adjusting for confounders, the effect was attenuated for most outcomes. Descriptive data of outcomes are presented in Table 2 The adjusted and unadjusted MDs and ORs along with 95% CIs are presented in Table 3.
Table 2.
Impairments, activity limitations, and participation in men and women scheduled for TKA
| Impairments | Men (n = 72), Mean (SD) | Women (n = 188), Mean (SD) | P a |
|---|---|---|---|
| KOOS‐Pain | 36.4 (21.1) | 24 (18) | 0.001 |
| KOOS‐Symptoms | 43.2(16.1) | 37 (16) | 0.007 |
| ROM <100⁰ in either of the knees, % | 4 (5.6) | 45 (26.8) | <0.0001 |
| Average quadriceps strength | 4.6 (1.9) | 2.9 (1.2) | <0.0001 |
| Activity limitations | |||
| Patient‐reported measures | |||
| KOOS‐ADL | 36.7 (21.1) | 27.5 (18) | 0.001 |
| Lower extremity activity score (1‐18) | 6.4 (1.4) | 5.7 (1.3) | 0.001 |
| Objective assessments | |||
| Chair‐raising test b | 7.6 (3.6) | 6.2 (3.2) | 0.004 |
| TUG, s c | 20.1 (11.4) | 25.7 (14.2) | 0.001 |
| 40‐m walk speed, m/s c | 0.80 (0.33) | 0.62 (0.26) | <0.0001 |
| Stair ascent and descent time, s c | 34.1 (23.6) | 48.3 (24.8) | 0.001 |
| Participation (late‐life disability instrument) | |||
| Overall frequency score (0‐100) | 44.8 (5.9) | 41.9 (5.1) | <0.0001 |
| Overall limitation score (0‐100) | 49 (7.0) | 45.9 (6.2) | 0.001 |
Abbreviation: ADL, activity of daily living; KOOS, knee injury and osteoarthritis outcome score; ROM, range of motion; TKA, total knee arthroplasty; TUG, timed up and go.
P values were derived from unpaired t test for continuous variables and χ2 test for categorical variables.
Two observations in men and three in women were missing because of patient refusal.
Sixteen missing values for TUG, 35 missing values for walking speed, and 74 missing values for stair climb time were imputed using the chained multiple imputation method.
Table 3.
Adjusted differences in impairments, activity limitation, and participation restriction between women and men scheduled for TKA a
| Women vs. Men (Reference Category) | Unadjusted β Coefficient (95% CI) | Adjusted βCoefficient (95% CI) b | P c |
|---|---|---|---|
| Impairment measures | |||
| KOOS‐Pain, 0‐100 scale | −9.3 (−14.9 to −3.3) | −6.9 (−13.7 to −0.18) | 0.04 |
| KOOS‐Symptoms, 0‐100 scale | 6.2 (−10.6 to −1.7) | −4.1 (−9.5 to 1.3) | 0.14 |
| ROM <100⁰ in either of the knee | OR: 6.12 (2.11 to 17.8) | OR: 5.7 (1.6 to 20.3) d | 0.007 |
| Log MVIC of knee extensors e | −0.47 (−0.56 to −0.34) f | −0.36 (−0.49 to −0.24) f | <0.001 |
| Patient‐reported measures of functional limitations | |||
| Lower extremity activity score | −0.65 (−1 to −0.28) | −0.30 (−0.76 to 0.16) | 0.195 |
| KOOS‐ADL, 0‐100 scale | −9.2 (−14.5 to −3.9) | −6.2 (−12.5 to 0.14) | 0.055 |
| Objective assessments of functional limitations | |||
| Chair stand test (n = 62 men, 149 women) | −1.4 (−2.3 to −0.44) | −0.73 (−1.8 to 0.38) | 0.52 |
| TUG, log s | 0.23 (0.09 to 0.36) f , g | 0.15 (0.03 to 0.31) f , g | 0.046 |
| 40‐m walk speed, m/s | −0.19 (−0.27 to −0.11) | −0.13 (−0.23 to −0.03) f | 0.007 |
| SCT, s | 14.3 (7.5 to 21.0) g | 9.5 (1.5 to 17.5) g | 0.02 |
| Disability (late‐life disability score) | |||
| Overall frequency score, 0 to 100 scale) | −2.8 (−4.3 to −1.3) | −1.6 (−3.3 to 0.18) | 0.08 |
| Overall limitation score, 0 to 100 scale | −3.0 (−4.8 to −1.2) | −2.7 (−4.9 to −0.45) | 0.019 |
Abbreviation: ADL, activities of daily living; CI, confidence interval; KOOS, knee injury and osteoarthritis outcome score; MVIC, maximum voluntary isometric contraction; OR, odds ratio; ROM, range of motion; SCT, stair climb test; TKA, total knee arthroplasty; TUG, timed up and go.
KOOS and disability scores range from 0 (worst) to 100 (best). Hence, negative coefficients mean poorer function scores in women compared with the reference. For timed tests (SCT and TUG), positive scores mean poorer function. For chair stand test and walking speed, negative coefficients mean poorer function.
Linear regression adjusted for age, type of family (nuclear/extended), current employment (yes/no), literacy (no schooling, schooling, graduate level and above), body mass index (kg/m2), comorbidity (none, one, more than one), socioeconomic scale, other chronic musculoskeletal pain, pain medication (yes/no), and previous TKA of other limb.
P values are derived from maximum likelihood tests and bolded P values are statistically significant at 0.05 cut‐off.
ORs are obtained from logistic regression.
Average MVIC of both limbs divided by body mass index for obtaining normalized scores.
Effect estimates are ratios of geometric means interpreted as percentage increase/decrease.
Chained multiple imputation method to impute for 16, 35, and 74 missing values of TUG, walking speed, and SCT. Results of regression following multiple imputation and complete data set analyses were similar.
Impairments
Women reported more pain (aMD: −6.9 [95% CI −13.7 to −0.18]) compared with men (lower scores indicate higher pain severity). There were no sex‐related differences for symptom severity (KOOS‐Symptom related to stiffness, clicking, and inability to bend knees). The odds of having flexion of less than 100° in either knee was higher among women (aOR: 5.7 [95% CI 1.6‐20.3]). Women had 36% lower quadricep strength compared with men (geometric aMD: −0.36 [95% CI −0.49 to −0.24]).
Activity limitation
Higher limitation during ADLs (MD: −6.2 [95% CI −12.5 to 0.14]) was reported by women but was not statistically significant. There was no difference in activity levels (LEAS) (Table 3). Of the four objective assessments, a statistically significant difference was found in all except CST. Slower walking speeds (aMD: −0.13 m/s [95% CI −0.23 to −0.03]) and longer times to complete SCT (aMD: 9.5 s [95% CI 1.5‐17.5]) and TUG (aMD: 0.15 s [95% CI 0.03‐0.31]) were observed in women after adjusting for confounders.
Participation restriction
There was a small but statistically significant difference in the limitation domain (aMD: −2.7, [95% CI −4.9 to −0.45]) of LLDI and no difference between men and women in the frequency domain.
Figure 2 illustrates the adjusted standardized mean differences between men and women across all domains of ICF. Knee extensor strength showed the maximum difference.
Figure 2.
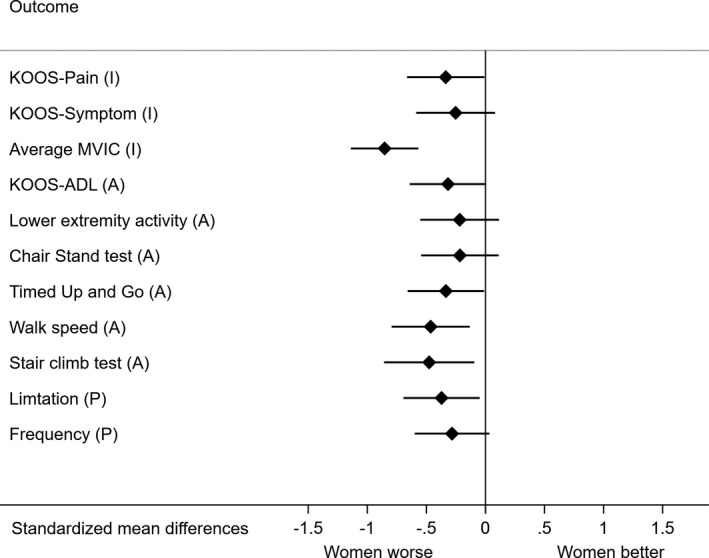
Difference between men and women across impairment (I), activity limitation (A), and participation (P) domains (as per international classification of functioning, disability, and health). The x‐axis shows standardized β coefficients, ie, mean differences between men and women, expressed in SDs. ADL, activities of daily living; KOOS, knee injury and osteoarthritis outcomes score; MVIC, maximum voluntary isometric contraction (average knee extensors of both limbs).
Association of impairments with participation restriction and interaction with sex
Higher levels of impairments had a negative effect on participation restriction. The limitation domain was affected more than the frequency of participation. Pain was more strongly associated with participation than other measures of impairment (R 2 = 12 and R 2 = 27 for frequency and limitation dimensions, respectively) (Table 4). However, the magnitude of association between knee pain, muscle strength, and ROM and participation restriction was similar in men and women (P ranged from 0.13‐0.75 for these interaction tests).
Table 4.
Association of impairment (independent variable) with participation restriction (dependent variable) a
| Impairment Measures | Frequency Score of LLDI (0‐100 Scale) | Limitation Score of LLDI (0‐100 Scale) | ||
|---|---|---|---|---|
| β Coefficient b (95% CI) | R 2 | β Coefficient b (95% CI) | R 2 | |
| KOOS‐Pain (0‐100 scale) | 0.10 (0.07 to 0.13) | 0.12 | 0.18 (0.15 to 0.21) | 0.27 |
| Average knee extensors MVIC | 0.94 (0.47 to 1.40) | 0.05 | 1.9 (1.35 to 2.41) | 0.15 |
| Average flexion ROM of both limbs per 5° | −0.007 (−0.23 to 0.25) | 0 | −2.5 (−4.7 to −0.25) | 1 |
Abbreviation: CI, confidence interval; KOOS, knee injury and osteoarthritis outcome score; LLDI, late‐life disability instrument; MVIC, maximum voluntary isometric contraction of both limbs; R 2, proportion of variance in participation restriction explained by the impairment measure; ROM, range of motion.
We have presented only overall results instead of by sex because no interactions were found between impairment measures and sex.
Linear regression is adjusted for age, sex, type of family (nuclear/extended), socioeconomic status, current employment (yes/no), literacy (no schooling, schooling, graduate level and above), body mass index (kg/.m2), comorbidity (none, one, more than one), duration of symptoms in years, other chronic musculoskeletal pain, analgesic intake (yes/no) and previous total knee arthroplasty of other limb.
Discussion
In this cross‐sectional analysis of individuals scheduled for TKA at a referral hospital in India, we aimed to explore differences between men and women across ICF constructs and assessed the effect of impairment measures on participation restriction. Women had significantly higher levels of impairments, activity limitation (stair climbing and walking speed), and limitation in participation compared with men, even after adjusting for potential confounding factors (small to medium size effects) (Figure 2). The contribution of knee pain on participation restriction was higher when compared with knee extensor muscle strength, and ROM was not associated (Table 4). This effect was similar in both men and women (Figure 3).
Figure 3.
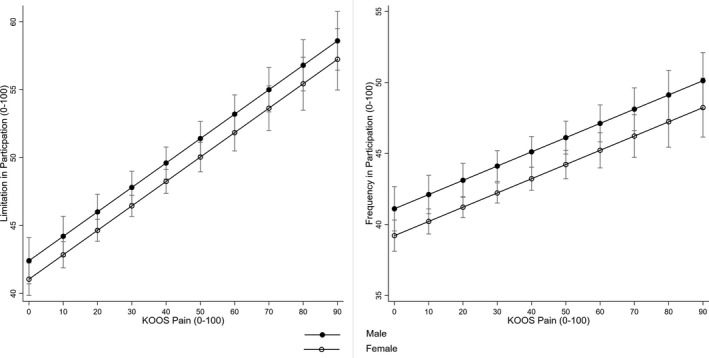
Association between knee pain and limitation in participation stratified by sex. KOOS, knee injury and osteoarthritis outcomes score.
Our study has several strengths. First, we captured outcomes that represent important elements of the disablement model (41). This differentiates our study from previous studies that reported only impairment and functional limitations (12, 13). Second, in addition to age and BMI, we adjusted for other important demographic and clinical characteristics that could potentially confound the relationship between sex and outcomes. This is evident by the attenuation of differences in the adjusted analyses (Table 3). Third, we used standardized tools to measure both subjective and objective measurements, making it possible to compare our results with the existing literature. Finally, to our knowledge, this is the first study from India to specifically address sex differences in severity of OA among those scheduled for TKA.
Our findings need to be interpreted in the context of the following limitations: This was a single‐center study conducted at a referral academic hospital, which potentially limits generalizability of the findings. However, this hospital caters to patients from several neighboring states, making the results fairly representative of Northern India. In this study, we did not have healthy age‐matched controls for comparison, which could have enabled us to assess the difference over and above the normal difference between men and women. However, previously published studies (12, 13) have demonstrated larger differences in functional ability between men and women with OA when compared with the age‐matched controls. The differences we report between males and females in time taken for TUG, SCT, and walking speed were similar in magnitude to those reported in previous studies (12, 13).
Our results are concordant with previous literature (12, 13) in terms of impairment and activity limitation. There are several plausible explanations for the observed differences between men and women. Biologically, men have higher muscle strength than women and that in turn can lead to differences in performance‐based measures. Differences observed for self‐reported pain may be a function of women over‐reporting their pain relative to men (or men under‐reporting). But the same logic did not apply to symptom score, which was not statistically different between the two groups. We found that women had significantly higher restriction in ROM, emphasizing that the difference was more than a physiological difference, and higher restriction in ROM among women correlates with greater severity and longer duration of OA. Further consistency of direction of effect across outcomes (Figure 2) also supports our case. Delayed care‐seeking behavior (42) could be one of the reasons for the differences we see in this sample.
There were no previous reports comparing participation restriction between men and women. A previous report from the Multicenter Osteoarthritis Study (MOST) longitudinal cohort (43) from the United States that the same tool for LLDI for participation restriction reported that 37% of those scheduled for TKA had limitation in participation (mean 74 (SD 14), and the cutoff for defining restriction of participation was less than 67.6/100 (44). In our sample, 99% of participants were found to have participation restriction using this cutoff. However, another study from Canada reported (45) severe limitation and frequency scores (38 and 39 on the scale of 1‐100) among those scheduled for TKA. We do not have non‐OA age matched controls to compare with, that could dilineate the effect of age on low particpation levels, but a great extent can be attributed to the social structure in the context of India. Most (60%) of our study participants were living in extended families, and none were living alone; hence, the need to be independent within and outside household may be less of a requirement. The key message here is that participation restriction scores need to be interpreted keeping the contextual factors in mind.
The disability pathway of impairments leading to activity limitation and further affecting participation directly or indirectly applies to many disabling diseases. However, the extent and pathways can vary. Pollard et al (46) explored this basic relationship using multivariate techniques and could not find a strong relationship between impairment and participation but found a strong correlation between the impairment and activity and activity and participation. This difference could be due to the variation in the tool used for measuring the constructs. Of the three impairment measures, pain seemed to be the most important contributor to participation restriction, highlighting the importance of pain relief for improving quality of life. Surprisingly, restricted ROM was not associated with participation restriction, likely due to modification of lifestyle according to the existing disabilities.
Even if women had higher levels of pain, it affected their everyday activities as much it affected men. This finding could be interpreted as a higher level of tolerance or the continuation of everyday activities despite pain. This is shown in other illnesses (17, 18), and this is the first time this has been demonstrated in OA; the implications of this could be delayed care‐seeking and reduced quality of life.
Reasons for delayed care‐seeking behavior and delay in decision‐making when advised for surgery should be explored further in countries in which OA is prevalent and TKA utilization is increasing such as in India.
Our findings are important for future patient management because baseline severity of symptoms (34) and activity limitations (47) are important predictors of postoperative outcomes. Cohort studies have shown the rate of recovery to be slower in women than in men (48), with women having have poorer post‐TKA functional outcomes at 12 months (49, 50). Follow‐up data from this cohort would give us insight into whether higher disability before surgery also delays the rate and extent of recovery.
Women scheduled for TKA had higher levels of impairments, activity limitations, and participation restriction even after accounting for potential confounders. In both sexes, knee pain contributed the most toward participation restriction. It is important to consider the sex differences when counseling individuals to undergo TKA for severe OA.
Author Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Devasenapathy had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Devasenapathy, Malhotra, Mittal, Zodpey, Maddison, Belavy.
Acquisition of data
Malhotra, Mittal, Garg, Kumar, Dogra.
Analysis and interpretation of data
Devasenapathy, Maddison, Belavy.
Acknowledgments
The authors thank Dr. Patrick Owen for proofreading the final version of the manuscript and making English language corrections.
The Public Health Research Initiative and the government of India did not have any role in design, conduct, and analysis of this study or in the interpretation of the results.
Dr. Devasenapathy's work is supported by an intramural Public Health Research Initiative research grant from the Public Health Foundation of India with the financial support of the Department of Science and Technology of the government of India.
Niveditha Devasenapathy, MBBS, MSc: Indian Institute of Public Health‐Delhi, Gurgaon, Haryana, Public Health Foundation of India, New Delhi, India, and Deakin University, Geelong, Victoria, Australia; 2Rajesh Malhotra, MS, Kanchan Mittal, MPT, Bhavuk Garg, MS, Vijay Kumar, MS: All India Institute of Medical Sciences, New Delhi, India; 3Sanjay Zodpey, MD, PhD, Hardik Dogra, MPT, Ralph Maddison, PhD, Daniel L. Belavy, PhD: Deakin University, Victoria, Geelong, Australia.
No potential conflicts of interest relevant to this article were reported.
References
- 1. Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd‐Allah F, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990‐2016: a systematic analysis for the Global Burden of Disease Study 2016 [published erratum appears in Lancet 2017;390:e38]. Lancet 2017;390:1211–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Institutes for Health Metrics and Evaluation . Global burden of disease: Study data. URL: https://vizhub.healthdata.org/gbd‐compare/.
- 3. Jones CA, Pohar S. Health‐related quality of life after total joint arthroplasty: a scoping review. Clin Geriatr Med 2012;28:395–429. [DOI] [PubMed] [Google Scholar]
- 4. Kane RL, Saleh KJ, Wilt TJ, Bershadsky B. The functional outcomes of total knee arthroplasty. J Bone Joint Surg Am 2005;87:1719–24. [DOI] [PubMed] [Google Scholar]
- 5. Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health‐related quality of life in total hip and total knee arthroplasty: a qualitative and systematic review of the literature. J Bone Joint Surg Am 2004;86:963–74. [DOI] [PubMed] [Google Scholar]
- 6. Shan L, Shan B, Suzuki A, Nouh F, Saxena A. Intermediate and long‐term quality of life after total knee replacement: a systematic review and meta‐analysis. J Bone Joint Surg Am 2015;97:156–68. [DOI] [PubMed] [Google Scholar]
- 7. Koh IJ, Kim TK, Chang CB, Cho HJ, In Y. Trends in use of total knee arthroplasty in Korea from 2001 to 2010. Clin Orthop Relat Res 2013;471:1441–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Singh JA. Epidemiology of knee and hip arthroplasty: a systematic review. Open Orthop J 2011;5:80–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Indian Society of Hip and Knee Surgeons Registry . 2018 report. URL: http://www.ishks.com/pdf/ISHKS‐Regitsry‐Update‐2018.pdf.
- 10. Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am 2012;94:201–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta‐analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage 2005;13:769–81. [DOI] [PubMed] [Google Scholar]
- 12. Kennedy D, Stratford PW, Pagura SM, Walsh M, Woodhouse LJ. Comparison of gender and group differences in self‐report and physical performance measures in total hip and knee arthroplasty candidates. J Arthroplasty 2002;17:70–7. [DOI] [PubMed] [Google Scholar]
- 13. Petterson SC, Raisis L, Bodenstab A, Snyder‐Mackler L. Disease‐specific gender differences among total knee arthroplasty candidates. J Bone Joint Surg Am 2007;89:2327–33. [DOI] [PubMed] [Google Scholar]
- 14. Lim JB, Chi CH, Lo LE, Lo WT, Chia SL, Yeo SJ, et al. Gender difference in outcome after total knee replacement. J Orthop Surg (Hong Kong) 2015;23:194–7. [DOI] [PubMed] [Google Scholar]
- 15. Parsley BS, Bertolusso R, Harrington M, Brekke A, Noble PC. Influence of gender on age of treatment with TKA and functional outcome. Clin Orthop Relat Res 2010;468:1759–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hawker GA, Wright JG, Coyte PC, Williams JI, Harvey B, Glazier R, et al. Differences between men and women in the rate of use of hip and knee arthroplasty. N Engl J Med 2000;342:1016–22. [DOI] [PubMed] [Google Scholar]
- 17. Kapoor M, Agrawal D, Ravi S, Roy A, Subramanian SV, Guleria R. Missing female patients: an observational analysis of sex ratio among outpatients in a referral tertiary care public hospital in India. BMJ Open 2019;9:e026850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nante N, Messina G, Cecchini M, Bertetto O, Moirano F, McKee M. Sex differences in use of interventional cardiology persist after risk adjustment. J Epidemiol Community Health 2009;63:203–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ramakrishnan S, Khera R, Jain S, Saxena A, Kailash S, Karthikeyan G, et al. Gender differences in the utilisation of surgery for congenital heart disease in India. Heart 2011;97:1920–5. [DOI] [PubMed] [Google Scholar]
- 20. Regitz‐Zagrosek V. Sex and gender differences in health: Science & Society series on sex and science. EMBO Rep 2012;13:596–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bora JK, Saikia N. Gender differentials in self‐rated health and self‐reported disability among adults in India. PLoS One 2015;10:e0141953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Alnahdi AH. Outcome measures capturing ICF domains in patient with total knee arthroplasty. Int J Rehabil Res 2014;37:281–9. [DOI] [PubMed] [Google Scholar]
- 23. World Health Organization . International Classification of Functioning, Disability and Health (ICF). URL: https://www.who.int/classifications/icf/en/.
- 24. Von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335:806–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dobson F, Hinman RS, Roos EM, Abbott JH, Stratford P, Davis AM, et al. OARSI recommended performance‐based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthritis Cartilage 2013;21:1042–52. [DOI] [PubMed] [Google Scholar]
- 26. Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS): development of a self‐administered outcome measure. J Orthop Sports Phys Ther 1998;28:88–96. [DOI] [PubMed] [Google Scholar]
- 27. University of California, San Francisco . Knee range of motion. URL: http://most.ucsf.edu/docs/KneeROM_v1.0p_06.01.13.pdf.
- 28. Mentiplay BF, Perraton LG, Bower KJ, Adair B, Pua YH, Williams GP, et al. Assessment of lower limb muscle strength and power using hand‐held and fixed dynamometry: a reliability and validity study. PLoS One 2015;10:e0140822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Saleh KJ, Mulhall KJ, Bershadsky B, Ghomrawi HM, White LE, Buyea CM, et al. Development and validation of a lower‐extremity activity scale: use for patients treated with revision total knee arthroplasty. J Bone Joint Surg Am 2005;87:1985–94. [DOI] [PubMed] [Google Scholar]
- 30. Terwee CB, Bouwmeester W, van Elsland SL, de Vet HC, Dekker J. Instruments to assess physical activity in patients with osteoarthritis of the hip or knee: a systematic review of measurement properties. Osteoarthritis Cartilage 2011;19:620–33. [DOI] [PubMed] [Google Scholar]
- 31. Osteoarthritis Research Society International . Recommended performance‐based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. URL: https://www.oarsi.org/sites/default/files/docs/2013/manual.pdf. [DOI] [PubMed]
- 32. Jette AM, Haley SM, Coster WJ, Kooyoomjian JT, Levenson S, Heeren T, et al. Late life function and disability instrument. I. Development and evaluation of the disability component. J Gerontol A Biol Sci Med Sci 2002;57:M209–16. [DOI] [PubMed] [Google Scholar]
- 33. Harmelink KE, Zeegers A, Hullegie W, Hoogeboom TJ, Nijhuis‐van der Sanden MW, Staal JB. Are there prognostic factors for one‐year outcome after total knee arthroplasty? A systematic review. J Arthroplasty 2017;32:3840–53. [DOI] [PubMed] [Google Scholar]
- 34. Hernandez C, Diaz‐Heredia J, Berraquero ML, Crespo P, Loza E, Ruiz Iban MA. Pre‐operative predictive factors of post‐operative pain in patients with hip or knee arthroplasty: a systematic review. Reumatol Clin 2015;11:361–80. [DOI] [PubMed] [Google Scholar]
- 35. Lungu E, Vendittoli PA, Desmeules F. Preoperative determinants of patient‐reported pain and physical function levels following total knee arthroplasty: a systematic review. Open Orthop J 2016;10:213–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Podmore B, Hutchings A, van der Meulen J, Aggarwal A, Konan S. Impact of comorbid conditions on outcomes of hip and knee replacement surgery: a systematic review and meta‐analysis. BMJ Open 2018;8:e021784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rosemann T, Laux G, Kuehlein T. Osteoarthritis and functional disability: results of a cross sectional study among primary care patients in Germany. BMC Musculoskelet Disord 2007;8:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Weiss E. Knee osteoarthritis, body mass index and pain: data from the Osteoarthritis Initiative. Rheumatology (Oxford) 2014;53:2095–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, et al. Socioeconomic status in health research: one size does not fit all. JAMA 2005;294:2879–88. [DOI] [PubMed] [Google Scholar]
- 40. Cohen J. A power primer. Psychol Bull 1992;112:155–9. [DOI] [PubMed] [Google Scholar]
- 41. McDonough CM, Jette AM. The contribution of osteoarthritis to functional limitations and disability. Clin Geriatr Med 2010;26:387–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Judge A, Welton NJ, Sandhu J, Ben‐Shlomo Y. Equity in access to total joint replacement of the hip and knee in England: cross sectional study. BMJ 2010;341:c4092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Maxwell JL, Keysor JJ, Niu J, Singh JA, Wise BL, Frey‐Law L, et al. Participation following knee replacement: the MOST cohort study. Phys Ther 2013;93:1467–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Keysor JJ, Jette AM, LaValley MP, Lewis CE, Torner JC, Nevitt MC, et al. Community environmental factors are associated with disability in older adults with functional limitations: the MOST study. J Gerontol A Biol Sci Med Sci 2010;65:393–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Davis AM, Perruccio AV, Ibrahim S, Hogg‐Johnson S, Wong R, Streiner DL, et al. The trajectory of recovery and the inter‐relationships of symptoms, activity and participation in the first year following total hip and knee replacement. Osteoarthritis Cartilage 2011;19:1413–21. [DOI] [PubMed] [Google Scholar]
- 46. Pollard B, Johnston M, Dieppe P. Exploring the relationships between International Classification of Functioning, Disability and Health (ICF) constructs of impairment, activity limitation and participation restriction in people with osteoarthritis prior to joint replacement. BMC Musculoskelet Disord 2011;12:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Devasenapathy N, Maddison R, Malhotra R, Zodepy S, Sharma S, Belavy DL. Preoperative quadriceps muscle strength and functional ability predict performance‐based outcomes 6 months after total knee. Phys Ther 2019;99:46–61. [DOI] [PubMed] [Google Scholar]
- 48. Kennedy DM, Stratford PW, Riddle DL, Hanna SE, Gollish JD. Assessing recovery and establishing prognosis following total knee arthroplasty. Phys Ther 2008;88:22–32. [DOI] [PubMed] [Google Scholar]
- 49. Pua YH, Seah FJ, Seet FJ, Tan JW, Liaw JS, Chong HC. Sex differences and impact of body mass index on the time course of knee range of motion, knee strength, and gait speed after total knee arthroplasty. Arthritis Care Res (Hoboken) 2015;67:1397–405. [DOI] [PubMed] [Google Scholar]
- 50. Ritter MA, Wing JT, Berend ME, Davis KE, Meding JB. The clinical effect of gender on outcome of total knee arthroplasty. J Arthroplasty 2008;23:331–6. [DOI] [PubMed] [Google Scholar]


