Abstract
Objective
To bring recent advances in pregnancy management in lupus to women nationwide, this multidimensional educational intervention sought to equip community rheumatologists with the needed skills, attitudes, and confidence to manage contraceptive decisions and pregnancy planning for women with lupus.
Methods
The program included an in‐person didactic, training in use of a comprehensive handout to guide contraception and pregnancy conversations, a simulated clinical experience, and access to an innovative website (www.lupuspregnancy.org). The program was analyzed using mixed methods, which included a quantitative survey by e‐mail before and after program completion and multiple qualitative interviews about attendees’ experiences integrating created resources into practice.
Results
The analysis included 68 preintervention surveys and 55 postintervention surveys. For qualitative analysis, eight interviews were completed until thematic saturation was achieved. After completion of the program, there was an increase in providers reporting a systematic approach to preparing a woman with lupus for pregnancy (from 45.6% to 94.6%; P < 0.0001). Confidence in choosing both appropriate contraception and pregnancy‐compatible medications improved significantly. As expected, change in knowledge about contraception was limited. Qualitative themes included the utility of the printable handouts, enthusiasm for the program, increased confidence and, importantly, increased empathy for the patients.
Conclusion
We created a valuable implementation tool that improves self‐reported provider skills and confidence in managing women with lupus who desire pregnancy. Providers now have access to a unique curriculum and resources that encourage providers to have open and accurate conversations about pregnancy, thus creating lasting clinical change.
Significance & Innovation.
We created an innovative, multifaceted educational program focused on enabling honest and accurate conversations between patients and their rheumatologists about pregnancy planning.
This curriculum targeted skills, attitudes, and building confidence through training to use easily accessible and navigable printouts to ensure that up‐to‐date medical advice is always available to patients.
In a mixed‐methods analysis, the program improved providers’ self‐reported skills and attitudes regarding pregnancy planning with patients, and there was high satisfaction with the program and continued use of provided tools and resources after program completion.
This is the first incorporation of the One Key Question into rheumatology care for pregnancy planning.
Introduction
When managed by lupus experts, pregnancies that start without nephritis in the setting of mild to moderate lupus activity can have outcomes comparable with those in the general population (Predictors of Pregnancy Outcomes in Systemic Lupus Erythematosus and Antiphospholipid Syndrome) (1). Lupus pregnancies in less than these ideal circumstances, however, continue to result in rates of preterm birth (20%‐60%) and preeclampsia (10%‐25%), several‐fold higher than that in the general population (2). Timing pregnancy to coincide with a period when lupus is quiet is associated with improved pregnancy outcomes. Unfortunately, we and others have identified barriers to pregnancy planning among both rheumatologists and patients. These include 1) gaps in clinician knowledge about medication compatibility with pregnancy and contraception, 2) deficits in communication about pregnancy planning between rheumatologists and patients and between rheumatologists and obstetricians, and 3) limits to patient‐provider trust and understanding that interfere with effective discussions and decisions (3, 4). Additionally, studies have shown that contraception counseling in women with systemic lupus erythematosus (SLE) is limited despite common use of teratogenic medications and a desire for these conversations by patients (5). It has been shown that these conversations are most successful and associated with better adherence when communication is focused on understanding the woman's needs, concerns, and plans rather than coercing the woman to use a specific contraceptive (6, 7).
In response to these needs, we created Healthy Outcomes in Pregnancy with SLE Through Education of Providers (HOP‐STEP) (www.lupuspregnancy.org). We designed this curriculum to provide rheumatology clinicians with the necessary skills, attitudes, and knowledge‐based resources to guide successful pregnancy planning to optimize outcomes. We designed the HOP‐STEP program to create transformative learning by grounding the intervention in participants’ previous experiences, changing providers’ attitudes about pregnancy in lupus to align with those of their patients, and providing process maps to be used in the clinic. The process maps bypass the need for clinicians to have in‐depth knowledge regarding contraception, teratogens, and pregnancy planning committed to memory at all times. Presented as an in‐person workshop, our program included ample time to practice new skills for honest and accurate conversations between rheumatology clinicians and women with lupus. The program used the One Key Question (OKQ) “Would you like to become pregnant in the next year?” a validated tool developed by the Oregon Foundation for Reproductive Health as an initiative for providers to routinely have intentional conversations about women's reproductive health (8). The OKQ was designed to provide a standardized framework to increase the frequency that open and honest conversations about pregnancy begin prior to conception. Doing so recognizes the importance of women's reproductive health prior to conception in an effort to optimize pregnancy outcomes (8, 9). The OKQ is used in primary care clinics across the United States and has been endorsed by the American Public Health Association and the American College of Obstetricians and Gynecologists as a simple and effective way to start pregnancy planning conversations (10). Implementation studies of the OKQ have demonstrated that two‐thirds of patients reported the tool as helpful in communicating their reproductive goals to their providers (11).
Recognizing the complexity of lupus care and of preparing women with lupus for pregnancy, our goals were to create an educational program that would 1) help align attitudes of providers and patients with lupus regarding childbearing to help providers become better partners with their patients, 2) simplify and demystify the patient encounter by providing skills to use a comprehensive handout that includes the necessary knowledge to accurately counsel women, and 3) improve providers’ confidence in their ability to counsel patients through facilitated practice with real‐time feedback.
We hypothesized that our HOP‐STEP workshop would help create attitudes toward parenthood and childbearing among attendees that were more aligned with those of patients. We aimed to change attitudes to help providers understand that for most women, simply becoming a mother was their goal, and they were willing to accept changes in their own health and an “imperfect” child to experience motherhood.
We also hypothesized that providing instruction and practice using a highly accurate discussion guide would equip providers to have these challenging discussions with their patients and thereby partner with them more effectively to promote healthy childbearing. Because medical information that is learned but not frequently used is quickly forgotten, we created a handout with the needed facts to use during patient counseling and provided access to a comprehensive supplemental website.
Patients and Methods
Study setting and population
To design an educational intervention and tools for practice that would meet the needs of practicing rheumatologists, we sought input for program development from local leaders in the Association of Women in Rheumatology (AWIR) through several telephone conferences. In addition, the program was developed with patient input through the Duke Autoimmunity in Pregnancy Patient Advisors and Collaborators (DAPPAC). The DAPPAC is a group of women with lupus and related conditions at various stages in their reproductive life who met regularly with the authors to provide patient context and advice for program development. We piloted the HOP‐STEP educational program for rheumatology clinicians at the AWIR national conference in August 2018.
Educational intervention
Recognizing that our planned learners were practicing rheumatologists, we conceptualized and designed HOP‐STEP using assumptions from Knowles andragogy. Specifically, we aimed to show respect for the preexisting expertise of these rheumatology learners and to ground our interventions in their need to effectively manage female patients of childbearing age (12). These assumptions seek to understand adult learning in the context of being on a continuum consisting of acquisition of three main domains: knowledge, skills, and attitudes (13). We additionally decided to focus on creating transformative learning. Transformative learning occurs in adult learners when the educational program asks them to both challenge their current beliefs and connect the new knowledge with what they already know based on their previous experiences (13). Thus, we designed the HOP‐STEP intervention as an interactive workshop with role‐play to allow each participant to experience what it feels like to be in both the provider and the female patient role. In addition, we asked them to practice using the resources so that they were well prepared to use them in clinical practice. We also gave them the opportunity to be observed and get feedback on their use of new skills.
Didactic and role‐play
On arrival for the didactic session, each attendee received a copy of our handout, which included information on preparing for a pregnancy (Figure 1A) on one side and information on contraception (Figure 1B) on the other. The handout includes the OKQ “Would you like to become pregnant in the next year?” along with data about contraceptive efficacy and medication compatibility with pregnancy, although these knowledge topics were not a focus of the presentation. The 90‐minute workshop started with a 45‐minute oral presentation with the learning objectives that attendees become 1) equipped to begin honest and accurate conversations about pregnancy planning and management with women with lupus, 2) able to guide women with lupus to appropriate contraception options, and 3) able to guide a woman with lupus through pregnancy planning.
Figure 1.
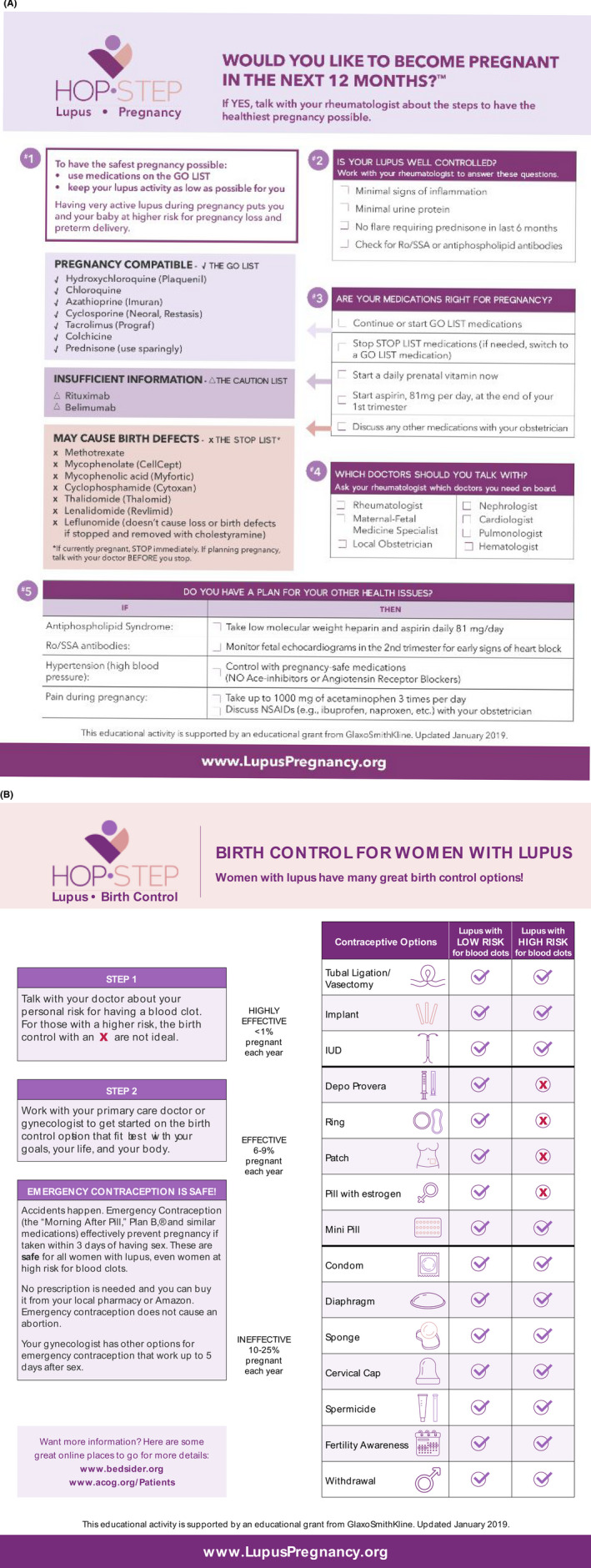
Healthy Outcomes in Pregnancy With Systemic Lupus Erythematosus Through Education of Providers (HOP‐STEP) handouts. A, HOP‐STEP pregnancy planning handout. B, HOP‐STEP contraception handout. IUD, intrauterine device; NSAID, nonsteroidal anti‐inflammatory drug.
After the 45‐minute presentation, we facilitated a 20‐minute case‐based role‐play experience to meet two objectives: 1) attitude change, in which attendees gain understanding of the patient experience through conversations about childbearing, and 2) attendees gaining confidence in using the provided contraception and preparing for pregnancy conversation guides through practice. Pairs of attendees role‐played the clinician or the patient in two conversations about pregnancy planning, in which the “clinicians” were instructed to use the handout provided to guide the conversation. After the role‐play, attendees participated in a facilitated group discussion of their attitudes about the patient experience regarding family building and how attitudes changed through role‐play participation. The workshop concluded with summary learning points from the didactic and the role‐play exercise.
Simulation exercise
To enhance retention and motivation for practice change, we invited clinicians to participate in a 20‐minute simulation exercise with standardized patients for additional practice. Simulations were designed by an author with expertise in designing simulated patient experiences (LGC‐S). In this simulation, participants individually provided preconception counseling to a young woman (actor) (RN and AE) who desired pregnancy but was taking a teratogenic medication for lupus nephritis. Facilitators (MEBC and LGC‐S) observed the counseling interactions and provided immediate feedback to participants, who then had an opportunity to navigate the situation again.
Website
We developed a website (www.lupuspregnancy.org) with resources to support implementation of practice changes after the in‐person workshop. Resources for patients and providers include printable contraception and pregnancy planning handouts to initiate and navigate pregnancy planning conversations, accurate phrases about medications and pregnancy with lupus for insertion into visit documentation and descriptions of medications and current usage recommendations. Video stories of DAPPAC members were created for inclusion on the website and the in‐person workshop to support attitude change among providers through understanding the patient perspective on lupus and pregnancy. Within the workshop, three short video clips were interspersed in the didactic session, illustrating the overwhelming desire for pregnancy experienced by some women, the hesitancy some women feel in bringing up pregnancy planning with their rheumatologists, and the fears many women have about taking medications during pregnancy. Longer video stories are also included on the website, and all participants had access to these following the in‐person workshop. Although website videos were available for viewing by all participants, we do not have data on who viewed which videos.
Program evaluation
We used a mixed‐methods approach to evaluate this program's efficacy, including pre–live session and post–live session surveys and qualitative interviews weeks after program completion. We e‐mailed surveys to the same 149 individuals before and after workshop completion. Surveys were designed to evaluate knowledge, skills, confidence, and attitudes surrounding lupus pregnancy planning. We assessed provider knowledge with focused survey questions about medications and contraception options. We assessed provider skills with focused questions about providers’ approach to having pregnancy planning and management conversations and availability of simulated clinical experience with real‐time feedback. We evaluated self‐reported confidence in recommending medications and contraception before and after the workshop. We assessed attitudes through questions about provider perception of patient priorities. Pre‐ and postintervention surveys were different to minimize test‐retest effect.
Qualitative program evaluation included telephone interviews conducted by a single interviewer (RN). All individuals who participated in the simulation exercise were invited to be interviewed about their experience with HOP‐STEP after the conference. Those who agreed voluntarily participated in a telephone conversation to discuss how they incorporated what they learned through the workshop and simulation into their clinical practice. Conversation guide questions were written to address the use of HOP‐STEP resources, provider confidence, barriers to application, and future directions. The Duke Institutional Review Board considered this protocol exempt (Pro00101649).
Statistical analysis
Quantitative
Primary comparisons of interest were differences between pre‐ and postsurvey data regarding having a systematic approach, contraception knowledge about teratogenicity and birth defects, and provider confidence. Categorical variables were analyzed via Fisher's exact test. Continuous variables, including questions about attitudes, were analyzed with t tests. Median values were analyzed via the Wilcoxon rank sum test. Assumptions were verified by ensuring normal distribution of data. If data were not normally distributed, then medians were compared.
Qualitative
Everyone who participated in the simulated clinical experience agreed to be contacted for a phone interview; we conducted interviews until we reached thematic saturation. A total of eight interviews for qualitative analysis were completed, at which point the authors unanimously agreed thematic saturation was accomplished. Rapid analysis of qualitative data consisted of categorizing questions into the following domains: use, provider confidence, barriers, medication knowledge, contraception knowledge, and general feedback. A summary template was created and was used to further assess for application and relevance by three authors (RN, AE, and MEBC). Once consistency was established using the summary template, each interview was independently reviewed by four members (RN, AE, AS, and MEBC) and compiled into a matrix to assess for thematic saturation.
Results
Workshop and participant characteristics
The workshop during the AWIR conference was attended by 149 individuals. All attendees participated in the table role‐play. Of these attendees, 16 participated in the individual patient counseling simulations. Of these 16 individuals, eight completed telephone interviews for qualitative analysis. All were women, including six practicing physician rheumatologists, one physician assistant, and one rheumatology fellow (time in practice: 1‐38 years). Preintervention surveys were completed by 68 individuals (45.6%), and 55 completed postintervention surveys (36.9%). Nearly all respondents were women and had an average of more than 10 years of experience (Table 1). Because surveys were anonymous, pre‐ and postintervention surveys could not be linked for analysis.
Table 1.
Provider and clinical practice characteristics
| Preintervention Survey (n = 68) | Postintervention Survey (n = 55) | |
|---|---|---|
| Response rate, % | 46 | 37 |
| Female sex, % | 93 | 96 |
| Medical role, % | ||
| Practicing rheumatologists | 66 | 64 |
| NP/PA | 12 | 20 |
| Rheumatology fellow | 6 | 9 |
| Other (eg, resident, industry) | 16 | 7 |
| Mean age, y | 46 | 44 |
| Mean years in practice | 13 | 10 |
Abbreviation: NP, nurse practitioner; PA, physician assistant.
Approach to patient conversations
In the preintervention survey, 45.6% of providers reported having a systematic approach to preparing a woman with lupus for pregnancy, 32.4% were not sure, and 22% reported having no approach. After the program, 94.6% reported having a systematic approach, 5.5% were not sure, and no respondents reported having no approach (P < 0.0001). We asked participants how they discovered a patient wanted to become a pregnant in a multiselect question. Before the intervention, 57% reported asking the patient, 44% reported that conversations were initiated by the patient, and 21% chose the response option “I don't know.” In the postintervention survey, 93% reported that they plan to ask the patient directly, and no providers chose the response option “I don't know” for how to find out if a patient with lupus wants to become pregnant (Figure 2). When asked to identify the key barrier to preparing women with lupus for pregnancy, 38.5% of providers identified patients already being pregnant, 21.5% identified patient trust, 21.5% identified time, and 18.5% identified medication knowledge as the key barriers (Figure 3).
Figure 2.
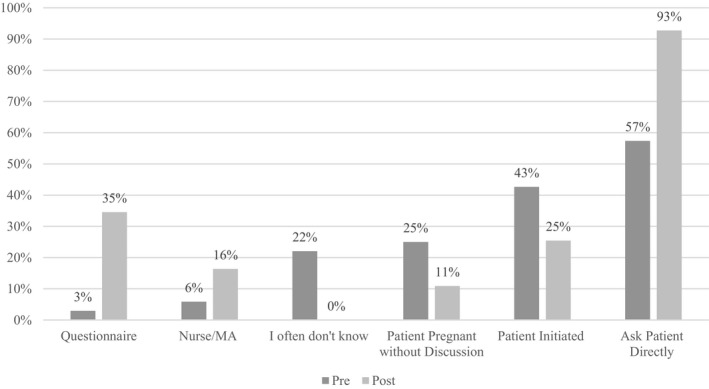
Provider responses to how they previously found out that a patient wanted to become pregnant compared with how they plan to after the conference (multiselect question). MA, Medical Assistant.
Figure 3.
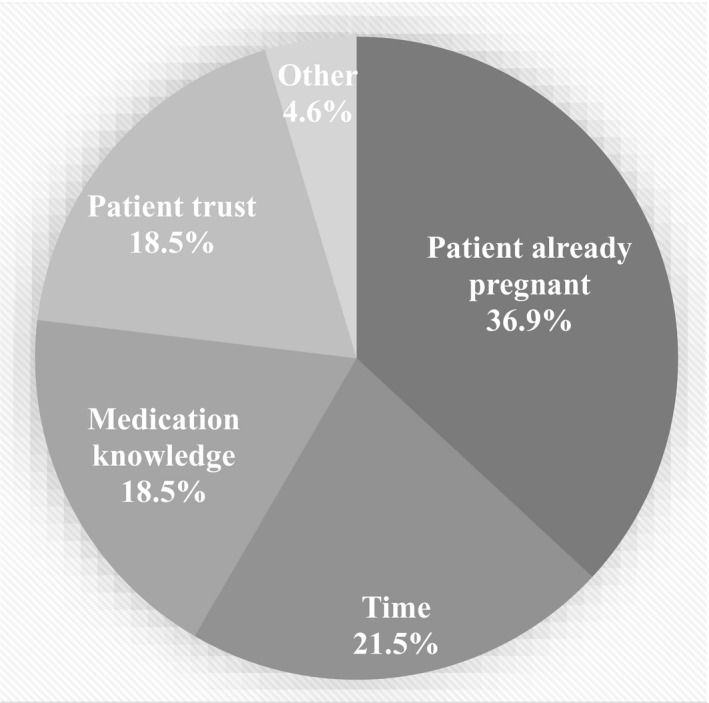
Provider‐identified barriers to preparing women with lupus for pregnancy.
The qualitative interviews demonstrated how the HOP‐STEP program improved the patient encounter. For example, using the handout with a patient was cited as an effective tool for communication:
Patients aren't good at remembering what you tell them because they are anxious…so having those handouts gives them something to refer back to and also gives them a little extra confidence…this [the handout] is the pathway that other people follow and this is the framework that is being used nationally.
Another provider reported that the HOP‐STEP handout made them more efficient because it streamlined the contraceptive and pregnancy planning discussion: “[I]t's a topic that we were going to be talking about anyway…it gives us a visual guide that may make some of the stuff easier.”
Knowledge
The knowledge assessment revealed minimal change in overall contraceptive knowledge, with the exception of improved knowledge about emergency contraception. At both time points participants seemed to understand the safety of intrauterine device use. There was no difference in correct responses regarding thrombotic risk or efficacy of specific contraceptives, which remained low at both time points. However, post intervention, providers reported using the contraception handout to alleviate this knowledge gap (Figure 3), with one provider stating, “I'm not really comfortable recommending birth control method[s], but it was interesting to see that whole [contraception] chart…it did increase my confidence because I could just cheat and look at it and show [patients] visually.” Another provider stated, “The contraception handout…I know which medicines you can and can't be on from a clot risk, but I think that is a helpful thing for providers who don't see lupus patients with antiphospholipids…I think that is a really helpful chart.”
Most providers were already knowledgeable about the safety of hydroxychloroquine in pregnancy (98% preintervention to 97% post intervention; P = 1.0). However, there was a statistically significant increase in providers who correctly identified azathioprine (AZA) (74%‐98%; P < 0.0001) and tacrolimus (46%‐91%; P < 0.0001) as pregnancy compatible. Most providers were previously knowledgeable on the teratogenicity of both cyclophosphamide and methotrexate (MTX); however, there appeared to be an increase in providers who correctly identified mycophenolate mofetil (MMF) (84%‐96%; P = 0.04) as teratogenic. In response to any specific medication knowledge changes after the program, one provider stated, “That CellCept is as high as it is on the list of drugs that are very bad for fetuses…I didn't realize that quite as much as I should've, everybody knows about methotrexate, but the fact that CellCept is probably even worse than methotrexate I was not aware of.”
One survey question asked about appropriately managing a lupus pregnancy in which a woman with proteinuria conceived while taking MMF, a known teratogen with a US Food and Drug Administration–mandated Risk Evaluation and Mitigation Strategy (14). In the preintervention survey, 15% reported that they would continue MMF, and 34% answered they would start AZA; in the postintervention survey no providers would continue MMF (P = 0.002), and 78% would start AZA (P < 0.0001).
Provider confidence
Participants were asked to rate their confidence on a scale of 0 (not confident) to 100 (very confident) regarding choosing contraception and medications. Median provider confidence significantly increased for helping women with lupus choose appropriate contraception (59‐89; P < 0.0001) and medications compatible with pregnancy (66‐91; P < 0.0001). These data are consistent in qualitative analysis of provider confidence, in which a majority of interviewed providers report similar or increased confidence in recommending contraception and choosing appropriate pregnancy‐compatible medications. Median provider confidence increased in each domain when providers were asked to rank their confidence on a scale of 0 (not confident) to 10 (very confident) regarding skills such as broaching the topic in an open way (6‐8.5), discussing contraceptive options (6‐8.5), and discussing pregnancy planning (5.5‐8.25). Overall, after completion of the program, in the qualitative interviews, the majority of providers felt very confident in pregnancy planning and management of women with lupus, with one provider stating, “I've come a long way.”
Program application
Many providers were able to incorporate their skills and HOP‐STEP resources into their clinical practice. One provider described an encounter with a young woman newly diagnosed with SLE whom she discovered had discontinued her birth control. This finding prompted contraception counseling and emphasis on pregnancy planning. In discussing her interaction with the patient, she went on to say, “[The nurse practitioner (NP)] never knows what is going to come into the office, so it is important that she, as an NP, have extensive training in things like this to be ready to have challenging conversations.” Another provider described a patient who conceived when lupus was uncontrolled and delivered with preeclampsia at 24 weeks, who she thinks would have benefited from the HOP‐STEP program: “[It] will help women understand we are on their side–they want a family but there is a right time and place for everything. If you say your baby will do better if you do X, Y, and Z, then maybe they will listen.” Regarding the need for shared decision‐making tools in pregnancy planning, one provider stated, “[W]omen who want to start a family…and if physicians don't talk about it, they are going to do it anyway. So I think…having some shared medical decision‐making is very important.”
Qualitative analysis
Our qualitative analysis revealed several key themes: 1) great enthusiasm for and appreciation of the program, 2) time as the key barrier to use, 3) knowledge improvement regarding teratogenicity of MMF versus MTX, 4) use and practicality of the handout, 5) increased self‐reported confidence, 6) increased empathy for the patient after “playing the patient” in the role‐play, and 7) desire for the program to expand beyond lupus.
Discussion
We created the HOP‐STEP program to provide clinical practitioners with the necessary attitudes, skills, resources, and confidence to guide pregnancy planning and management. The curriculum was designed based on a needs assessment of practicing rheumatologists that revealed gaps in knowledge about contraception, teratogens, and pregnancy complications (3). Based on the patient perspectives gained from our patient advisors, the program was grounded in the need for rheumatologists to develop skills to establish therapeutic relationships. Our findings are consistent with previous studies demonstrating that shared decision‐making tools are effective in assisting health professionals to provide information and counseling surrounding choices during pregnancy (15). Our qualitative analysis showed that the educational program and distribution of printable resources gave providers the needed tools and information to effectively manage this patient population.
Prior to the program, few of the rheumatologists surveyed reported having an approach to initiating a conversation surrounding pregnancy, mainly approaching this conversation by focusing on contraceptive adherence. An important goal of the program was to encourage rheumatologists to incorporate the OKQ into clinical practice as a valuable avenue to encourage patients to express their reproductive goals. After the workshop, the majority of providers reported directly asking the patient as the primary means to finding out if a patient with lupus desires pregnancy. Another program objective was to create attitude change to enable providers to better understand patient priorities, thus allowing the patient and provider team to be proactive when establishing optimal pregnancy timing to achieve outcomes similar to those in the general population. The program resulted in a significant increase in provider confidence in both recommending contraception and prescribing pregnancy‐compatible medications.
Preconception counseling is often overshadowed by the many tasks that must be accomplished in a lupus clinic visit. However, patients desire to receive contraception counseling from providers (16). Our in‐person program did not significantly increase contraception knowledge; these data are similar to those in studies conducted in other medicine subspecialties. One study regarding contraception use in the human immunodeficiency virus (HIV) population demonstrated that providers did not routinely discuss reproductive goals with patients with HIV and/or had limited or inaccurate knowledge (17). Limited knowledge and confidence may explain why conversations surrounding contraceptive options in patients with lupus are not occurring as frequently as they should be (5). Decision aids have proven to be effective at offering a framework for providers and patients to evaluate options and select treatments consistent with their individual needs (16). We designed the HOP‐STEP program and materials to overcome continued knowledge gaps through easy‐to‐find printable information to allow accurate patient counseling. Thus, despite limited change in knowledge among program participants, providers reported improved skills and confidence for appropriate patient management, enhanced by use of the printable decision aids provided. We expect that equipping more providers with the ability to use decision aids to counsel women with lupus and engage in shared decision‐making will lead to more pregnancies being optimally timed to allow for better outcomes.
A strength of the HOP‐STEP program is the use of multiple learning modalities, including a live program with peer‐to‐peer practice, incorporation of the validated OKQ, and a supplemental website with printable decision aids. In addition, we designed the educational program according to accepted premises of transformational and adult learning. We included patients as advisors to the program to ensure relevance and consistency with their priorities to strengthen the program. Finally, the mixed‐methods curriculum assessment gives a full picture of its impact and opportunities for improvement.
We acknowledge several limitations to our study, including the sample size for this initial program, with preintervention and postintervention survey response rates of 46% and 38%, respectively. Program participants were primarily female which may limit generalizability to all rheumatologists. The women members of AWIR who participated in the simulated clinical experience with individualized feedback sessions were self‐selected and might have had higher motivation to engage with this topic and, therefore, rate it as more impactful than a less interested group of learners would. Furthermore, the increase in confidence, but not knowledge, could be problematic if providers provide incorrect information about contraceptives and medications in pregnancy. This is why the program strongly emphasized the value and use of the handout to guide these conversations because the handout contains the accurate information that rheumatologists and patients need to make informed choices about contraception and pregnancy planning. Finally, we might have underestimated the efficacy of the program because the accompanying website was still under development during the live workshop, so participants did not have access to all the currently available resources.
In summary, we developed a multimodal educational and decision‐support program, HOP‐STEP, with the ultimate goal of improving lupus pregnancy planning and management, and ultimately pregnancy outcomes, in this high‐risk group. We demonstrated that participants of this program self‐reported improved confidence and skills for managing women with lupus who desired contraception or pregnancy. The website augments the in‐person program and handout by providing easy access to up‐to‐date information about contraception and pregnancy management and providing videos demonstrating the patient perspective. The use of the validated OKQ encourages providers and patients to have open and accurate conversations. Future work will include making adaptations to the HOP‐STEP program and handouts based on feedback from clinicians who have used it in clinical practice and distributing the program more broadly by training additional partners to deliver the HOP‐STEP workshops. Ultimately, we look forward to testing the effectiveness of the program in changing care and improving pregnancy outcomes. The HOP‐STEP program is being updated to correspond to the inaugural American College of Rheumatology reproductive health guidelines (18) and will be an important tool in allowing the implementation of these guidelines into practice.
Author Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Criscione‐Schreiber had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Criscione‐Schreiber, Eudy, Snyderman, Clowse.
Acquisition of data
Njagu, Criscione‐Schreiber, Eudy, Snyderman, Clowse.
Analysis and interpretation of data
Njagu, Criscione‐Schreiber, Eudy, Clowse.
Role of the Study Sponsor
GlaxoSmithKline had no role in the study design or in the collection, analysis, or interpretation of the data, the writing of the manuscript, or the decision to submit the manuscript for publication. Publication of this article was not contingent upon approval by GlaxoSmithKline.
GlaxoSmithKline provided an independent medical education grant to Duke University to support this program. The company did not contribute to the evaluation of this study or the content of www.lupuspregnancy.org.
Dr. Clowse has serves as a consultant for UCB and Astra‐Zeneca. No other disclosures relevant to this article were reported.
References
- 1. Buyon JP, Kim MY, Guerra MM, Laskin CA, Petri M, Lockshin MD, et al. Predictors of pregnancy outcomes in patients with lupus: a cohort study. Ann Intern Med 2015;163:153–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Clowse ME, Jamison M, Myers E, James AH. A national study of the complications of lupus in pregnancy. Am J Obstet Gynecol 2008;199:127.e1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Clowse ME, Eudy AM, Revels J, Sanders GD, Criscione‐Schreiber L. Rheumatologists’ knowledge of contraception, teratogens, and pregnancy risks. Obstet Med 2018;11:182–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Clowse ME, Eudy AM, Revels J, Neil L, Sanders GD. Provider perceptions on the management of lupus during pregnancy: barriers to improved care. Lupus 2019;28:86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yazdany J, Trupin L, Kaiser R, Schmajuk G, Gillis JZ, Chakravarty E, et al. Contraceptive counseling and use among women with systemic lupus erythematosus: a gap in health care quality? [Original article]. Arthritis Care Res (Hoboken) 2011;63:358–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Henderson JT, Raine T, Schalet A, Blum M, Harper CC. “I wouldn't be this firm if I didn't care”: preventive clinical counseling for reproductive health. Patient Educ Couns 2011;82:254–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Moskowitz E, Jennings B. Directive counseling on long‐acting contraception. Am J Public Health 1996;86:787–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Allen D, Hunter MS, Wood S, Beeson T. One key question®: first things first in reproductive health. Matern Child Health J 2017;21:387–92. [DOI] [PubMed] [Google Scholar]
- 9. Verbiest S, Malin CK, Drummonds M, Kotelchuck M. Catalyzing a reproductive health and social justice movement. Matern Child Health J 2016;20:741–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Power to Decide . Select360 consulting 2020. URL: https://powertodecide.org/select360-consulting#tab-1.
- 11. Baldwin MK, Overcarsh P, Patel A, Zimmerman L, Edelman A. Pregnancy intention screening tools: a randomized trial to assess perceived helpfulness with communication about reproductive goals. Contracept Reprod Med 2018;3:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Knowles MS. The modern practice of adult education: from pedagogy to andragogy. Englewood Cliffs, NJ: Cambridge Adult Education; 1970. [Google Scholar]
- 13. Taylor DC, Hamdy H. Adult learning theories: implications for learning and teaching in medical education: AMEE Guide No. 83. Med Teach 2013;35:e1561–72. [DOI] [PubMed] [Google Scholar]
- 14. Mycophenolate REMS . Welcome to the Mycophenolate REMS (Risk Evaluation and Mitigation Strategy). 2012. URL: https://www.mycophenolaterems.com/Default.aspx.
- 15. Dugas M, Shorten A, Dube E, Wassef M, Bujold E, Chaillet N. Decision aid tools to support women's decision making in pregnancy and birth: a systematic review and meta‐analysis. Soc Sci Med 2012;74:1968–78. [DOI] [PubMed] [Google Scholar]
- 16. Dehlendorf C, Fitzpatrick J, Steinauer J, Swiader L, Grumbach K, Hall C, et al. Development and field testing of a decision support tool to facilitate shared decision making in contraceptive counseling. Patient Educ Couns 2017;100:1374–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mindry DL, Milford C, Greener L, Greener RM, Maharaj P, Letsoalo T, et al. Client and provider knowledge and views on safer conception for people living with HIV (PLHIV). Sex Reprod Healthc 2016;10:35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sammaritano LR, Bermas BL, Chakravarty EE, Chambers C, Clowse ME, Lockshin MD, et al. 2020 American College of Rheumatology guideline for the management of reproductive health in rheumatic and musculoskeletal diseases. Arthritis Rheumatol 2020;72:529–56. [DOI] [PubMed] [Google Scholar]


