Abstract
Background
The clinical course of schizophrenia varies among patients and is difficult to predict. Some patient populations present persistent negative symptoms, referred to as the deficit syndrome. Compared to relatives of non-deficit schizophrenia patients, family members of this patient population are at an increased risk of developing schizophrenia. Therefore, the aim of this study was to search for genetic underpinnings of the deficit syndrome in schizophrenia.
Methods
Three SNPs, i.e., rs1799732 and rs6276 located within DRD2, and rs1800497 within ANKK1, were identified in the DNA samples of 198 schizophrenia probands, including 103 patients with deficit (DS) and 95 patients with non-deficit schizophrenia (NDS). Results: No significant differences concerning any of the analyzed polymorphisms were found between DS and NDS patients. However, significant links were observed between family history of schizophrenia and the deficit syndrome, G/G genotype and rs6276 G allele. In a separate analysis, we identified significant differences in frequencies of rs6276 G allele between DS and NDS patients with family history of schizophrenia. No significant associations were found between DRD2 and ANKK1 SNPs and the age of onset or schizophrenia symptom severity.
Conclusions
The results of our preliminary study fail to provide evidence of associations between DRD2 and ANKK1 polymorphisms with the deficit syndrome or schizophrenia symptom severity, but suggest potential links between rs6276 in DRD2 and the deficit syndrome in patients with hereditary susceptibility to schizophrenia. However, further studies are necessary to confirm this observation.
Keywords: Schizophrenia, Deficit syndrome, Family history of schizophrenia, Gene polymorphisms, DRD2, ANKK1
Background
Schizophrenia is a common mental disorder with a multifactorial background, and a lifetime prevalence of about 0.5–1% [1]. Its course is varied and difficult to predict. Some patients experience a single psychotic episode, while others report alternating periods of exacerbation and remission, or gradual functional deterioration from the very onset, with permanent negative symptoms. Early and precise recognition and prognosis, especially regarding disease progression enables timely implementation of appropriate preventive measures [2, 3]. Based on observations of Carpenter et al. [4], it was proposed that enduring negative symptoms, which are present during or in-between episodes of exacerbation of positive symptoms, and independently of social isolation, antipsychotic treatment, or depressive symptoms, should be distinguished as another schizophrenia subtype and called the “deficit syndrome”. Although none of the available classifications of diseases include the term “deficit schizophrenia”, the ICD-11 and DSM-5 identify schizophrenia with dominant negative symptoms [5, 6]. The deficit syndrome is linked with a stable progression of negative symptoms, observed from illness onset throughout the course of the disease [7–10], and its incidence in patients with chronic schizophrenia is estimated at 25–30% [11]. Evidence from family, twin and adoption studies highlights the key role of genetic factors in the development of schizophrenia [12] and its heritability of up to 80% [13]. Associations with family history were also found for the deficit syndrome [11].
Despite years of research, pathogenesis of schizophrenia is yet to be fully understood, but dysregulation of dopaminergic neurotransmission seems to be somehow implicated in its development. Positive symptoms are hypothesized to result from excessive dopamine activity in the mesolimbic pathway, while the negative symptoms and cognitive impairment to stem from reduced dopamine activity in the mesocortical pathway [14]. Findings suggest elevated density of dopamine D2 receptor (DRD2) in the brains of schizophrenic patients and most antipsychotic agents act as DRD2 antagonists [15–17]. However, studies on the effect of antipsychotic drugs on negative symptoms yield inconsistent results. According to some, antipsychotic medication may trigger or worsen negative symptoms in both clinical [18] and non-clinical samples [19–21], while others suggest no clinically meaningful effect on negative symptoms [22]. According to de Haan et al. [23], negative symptoms may be related to striatal dopamine D(2) receptor occupancy, but other studies fail to replicate such findings [24, 25]. Brito-Melo et al. [26] showed an association between increased expression of DRD2 in peripheral blood T-cells, higher scores in the Brief Psychiatric Rating Scale (BPRS) and the Positive and Negative Syndrome Scale (PANSS). Liu et al. [27] also found a relationship between DRD2 expression and negative symptoms, observing a positive correlation between the deficit syndrome severity and DRD2 expression in peripheral blood leukocytes of chronic schizophrenia patients receiving clozapine treatment.
Although a linkage was reported between the DRD2 genomic location (11q22–11q23) and schizophrenia [28], the results of association studies of particular polymorphisms remain inconsistent, due possibly to relatively small sample sizes, multifactorial underpinnings of schizophrenia and heterogeneous study groups [29]. In this study, we decided to investigate whether common functional single nucleotide polymorphisms (SNPs) located within DRD2 (rs1799732, rs6276) and ankyrin repeat and kinase domain containing 1 (ANKK1; rs1800497) are associated with the deficit syndrome or symptom severity in schizophrenic patients.
Rs1799732 (-141C Ins/Del) is a functional SNP located in the 5′-promoter region of DRD2, affecting striatal dopamine receptor density [30] and likely associated with schizophrenia [31–37], although not all studies confirm this association [38–40]. Himei et al. report a link between rs1799732 and PANSS-positive symptom score in schizophrenic patients [41]. In turn, according to Ohara et al. [31], it is associated with the age of onset, but not the PANSS scores in this patient population. Lencer et al. [42] demonstrate a link between rs1799732 and motor and cognitive function in first-episode psychosis. On top of that, it is also associated with antipsychotic efficacy [43, 44], antipsychotic-induced weight gain [45], neuroleptic-induced extrapyramidal adverse effects [46], personality traits [47, 48], sexual dysfunction in male schizophrenia [49], suicide attempts [50, 51] and alcoholism [52].
Rs6276 is a putative functional polymorphism located in 3′UTR region of DRD2 gene. To date, there seems to be a paucity of research examining its links with schizophrenia, but it has been associated with total and spatial insight problem solving [53], creative potential determined by verbal and figural divergent thinking tests [54], susceptibility to delirium [55], alcohol consumption [56], acute pain severity [57] and human longevity [58].
Rs1800497, previously known as DRD2 Taq 1A, is a functional polymorphism in adjacent ankyrin repeat and kinase domain containing 1 (ANKK1) gene, affecting dopamine D2 receptor binding [59]. Findings concerning its links with schizophrenia are somewhat inconsistent [29, 36, 60–63]. There is evidence of its associations with the age of schizophrenia onset [64], antipsychotic-induced weight gain [65], antipsychotic treatment response [66] and mood disorders [67, 68]. Takeuchi et al. [69] demonstrated its effect on emotional intelligence, which is, albeit indirectly, believed to also affect divergent thinking and motivation. Interestingly, haplotypes of rs1079597-rs1800497 were found to be associated with improvements in negative symptoms after amisulpride treatment, but there was no significant finding concerning the polymorphism itself [70].
Despite many studies linking dopamine receptors and their genetic polymorphisms with schizophrenia and its clinical manifestation, including the age of onset, cognitive functions, positive and negative symptom severity, treatment response and adverse effects, there is still a relative paucity of research investigating direct associations between DRD2 polymorphisms and the deficit syndrome. Therefore, the aim of this study is to fill this gap and examine the effect of DRD2 and ANKK1 polymorphisms on the deficit syndrome.
Methods
The sample
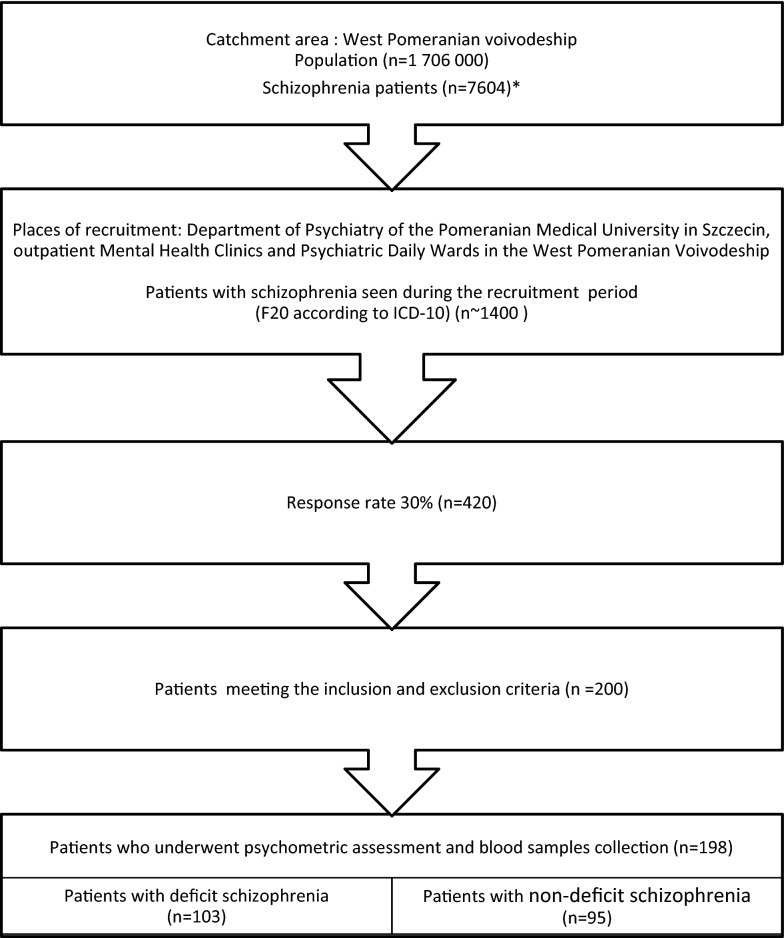
Our sample consisted of 198 Caucasian patients with schizophrenia, recruited in the Department of Psychiatry of the Pomeranian Medical University in Szczecin, Outpatient Mental Health Clinics and Psychiatric Day Wards in West Pomeranian voivodeship in the years 2011–2015 (Fig. 1).
Fig. 1.
Strobe flowchart of the recruitment process
Inclusion criteria were: age of 18–60 years, diagnosis of schizophrenia (F20 according to the ICD-10 [71–73]), disease duration of > 18 months, comprehension of test procedures and an informed consent to participate in the study. Exclusion criteria comprised: psychiatric comorbidity (including affective disorders), dementia or significant brain damage, epilepsy, addiction to alcohol or other psychoactive substances (excluding nicotine) and somatic conditions (cancer, chronic cardiovascular, respiratory, digestive, excretory or hormonal disorders). All recruitment procedures were carried out by two specialist psychiatrists. All participating clinicians were trained in the use of psychometric scales and had valid Good Clinical Practice certifications. The necessary calibrations were performed before baseline—the research team practiced implementation of study procedures on a standard patient, commenting on the results and setting endpoint criteria. Diagnostic assessment was performed using standardized research tools—the Mini-international neuropsychiatric interview [74], Operational Criteria Checklist for Psychotic Illness and Affective Illness (OPCRIT) [75], and a self-designed questionnaire. Psychometric assessment included validated Polish versions of the Positive and Negative Syndrome Scale (PANSS) [76–79], the Clinical Global Impression-Schizophrenia scale (CGI-SCH) [80, 81] and the Mini-Mental State Examination (MMSE) [82, 83]. In the PANSS, the positive (P1–P7), negative (N1–N7) and general (G1–G16) symptoms were rated on a 0–6 scale, based on the severity of each symptom. The CGI-SCH was used to assess the severity of schizophrenia across overall, positive, negative, depressive, and cognitive subdomains. Each symptom was scored on a scale from 1 to 7 [(1) norm, lack of dysfunction, (2) minimally ill, (3) slightly ill, (4) moderately ill, (5)-clearly ill, (6) seriously ill, 7-extremely ill). The MMSE was used to screen for cognitive impairment. A score of 27–30 suggested no cognitive impairment, 24–26—cognitive impairment without dementia, 19–3—mild dementia, 11–18—moderate dementia, and ≤ 10 severe dementia. None of the patients scored < 24 points. All patients received typical or atypical antipsychotics and were treated according to the psychopharmacological guidelines for the treatment of schizophrenia [84–87].
Based on clinical symptoms, medical history of functional impairment, and the Schedule for the Deficit Syndrome (SDS) outcome, the sample was divided into two subgroups: (1) patients with deficit (DS), and (2) non-deficit schizophrenia (NDS) [88–92]. The SDS ratings were made on a five-point scale, based on the primary or secondary character, persistence and intensity of each of the following six negative symptoms: restricted affect, diminished emotional range, poverty of speech, curbing of interests, diminished sense of purpose, diminished social drive. Patients with SDS score of ≥ 2 and two or more primary and permanent (i.e., lasting at least 12 months) negative symptoms were qualified to the DS subgroup, while all others comprised the NDS subgroup. The two groups differed in gender proportions, family history of schizophrenia (in first or second degree relatives), duration of longest relapse, and their MMSE, PANSS, CGI-SCH and SDS scores (Table 1).
Table 1.
Demographic and clinical characteristics of the study subgroups
| Parameter | DS | NDS | X2 | Z | p |
|---|---|---|---|---|---|
| Women n (%) | 43 (42) | 58 (61) | 7.37 | 0.007 | |
| Age (years) mean ± SD (median) | 41 ± 11 (40) | 39 ± 11 (36) | − 1.46 | 0.143 | |
| Higher education n (%) | 18 (17) | 18 (19) | 0.07 | 0.788 | |
| Cohabitation n (%) | 32 (31) | 29 (31) | 0.01 | 0.934 | |
| Psychiatric illness in the family n (%) | 41 (40) | 33 (35) | 0.46 | 0.496 | |
| Neurological illness in the family n (%) | 17 (17) | 13 (14) | 0.27 | 0.603 | |
| Schizophrenia in the family n (%) | 30 (29) | 15 (16) | 4.83 | 0.028 | |
|
Duration of schizophrenia (years) mean ± SD (median) |
14 ± 9 (13) | 13 ± 10 (10) | − 1.73 | 0.084 | |
| Age of onset (years) mean ± SD (median) | 27 ± 8 (24) | 26 ± 8 (24) | − 0.30 | 0.761 | |
| Time delay from onset to diagnosis n (%) | |||||
| < 1 month | 49 (48) | 48 (51) | |||
| 1–6 months | 23 (22) | 21 (22) | 0.22 | 0.897 | |
| > 6 months | 31 (30) | 26 (27) | |||
| Withdrawal of symptoms after neuroleptics n (%) | 97 (94) | 93 (98) | 1.76 | 0.184 | |
| Number of psychiatric hospitalizations mean ± SD (median) | 6.7 ± 5.8 (5) | 6.4 ± 6.8 (4) | − 1.14 | 0.253 | |
| Longest episode (weeks) mean ± SD (median) | 33 ± 62 (14) | 19 ± 27 (12) | − 2.31 | 0.021 | |
| Clinical course n (%) | 0.31 | 0.855 | |||
| Episodes of relapses and remissions | 78 (76) | 82 (86) | |||
| Chronic course | 10 (10) | 8 (8) | |||
| Chronic course with social withdrawal | 14 (14) | 5 (5) | |||
| MMSE mean ± SD (median) | 28 ± 2 (28) | 28 ± 2 (29) | 2.29 | 0.022 | |
| PANSS mean ± SD (median) | |||||
| Total | 42 ± 18 (41) | 22 ± 19 (17) | − 7.08 | < 0.001 | |
| Positive | 6 ± 5 (6) | 5 ± 5 (3) | − 2.72 | 0.006 | |
| Negative | 16 ± 6 (15) | 7 ± 6 (5) | − 9.01 | < 0.001 | |
| General | 19 ± 10 (18) | 10 ± 9 (8) | − 6.37 | < 0.001 | |
| CGI-SCH mean ± SD (median) | |||||
| Total | 14 ± 5 (14) | 9 ± 4 (8) | − 7.79 | < 0.001 | |
| Positive | 2.3 ± 1.3 (2) | 1.8 ± 1.0 (1) | − 2.23 | 0.026 | |
| Negative | 3.8 ± 1.3 (4) | 2.1 ± 1.2 (2) | − 8.10 | < 0.001 | |
| Depressive | 2.3 ± 1.1 (2) | 1.4 ± 0.6 (1) | − 6.73 | < 0.001 | |
| Cognitive | 2.8 ± 1.1 (3) | 1.8 ± 0.9 (2) | − 6.10 | < 0.001 | |
| Total severity of schizophrenia | 3.2 ± 1.1 (3) | 2.0 ± 1.0 (2) | − 7.35 | < 0.001 | |
| SDS mean ± SD (median) | 15 ± 5 (15) | 6 ± 6 (6) | − 8.99 | < 0.001 | |
Genetic tests
DNA was extracted from leukocytes using a salting out procedure [93]. In thus obtained genetic material, we identified three SNPs: rs1799732 and rs6276 located within DRD2 and rs1800497 within ANKK1. The tests were carried out using the real-time polymerase chain reaction (real-time PCR) technique, with the use of LightSNiP probes (TIB MOLBIOL GmbH) and melting curve analysis on the LightCycler 2.0 instrument (Roche Diagnostics). All assays were carried out in the Psychiatrics Genetic Laboratory at the Department of Psychiatry of the Pomeranian Medical University in Szczecin. Genotyping was performed blind to study group assignment (DS/NDS).
Statistical analysis
Statistical analysis was performed using Statistica 13 software (StatSoft, Inc.). Sample size was calculated using Statistica software for sample size calculation (two-sample Z test). We assumed a power of 0.90 and α = 0.05 to detect a medium effect size for differences in allelic proportions between DS and NDS patients for all analyzed SNPs. As per proportion estimation, we considered minor allele frequency of particular SNPs in the European population (https://www.ncbi.nlm.nih.gov/projects/SNP/), and the expected difference between arcsine transformed proportions (h) of 0.5 in the investigated groups, which is considered a medium effect size [94]. According to our calculations, the minimum number of patients was 87 for each of the subgroups, 174 in total. Therefore, the collected material was sufficient to perform all planned analyses. The Hardy–Weinberg equilibrium was assessed using a calculator (http://www.dr-petrek.eu/documents/HWE.xls, access on 16.11.2018). Pearson’s Χ2 test was used to analyze differences in distribution of genotypes and alleles between the two groups. For small sample sizes (if frequency of one of the genotypes was < 10), significant differences were verified using the Yates correction. Most of the analyzed variables deviated from the normal distribution in the Shapiro–Wilk test, therefore the Mann–Whitney U test and Kruskal–Wallis test were performed to analyze associations between genotypes, patient subgroups and the quantitative variables. In all analyses, statistical significance was set at p > 0.05.
Results
For all analyzed SNPs, the observed genotype distributions in the study group were consistent with the Hardy–Weinberg equilibrium (χ2 < 0.16, p > 0.68).
Direct comparisons did not show any significant differences in genotype or allele distributions between patients with deficit and non-deficit schizophrenia for any of the studied polymorphisms (Table 2).
Table 2.
Comparison of genotype and allele distributions of DRD2/ANKK1 SNPs between schizophrenic patients with (DS) and without (NDS) the deficit syndrome
| Group | n | Genotypes N (%) | χ2 | p | Alleles N (%) | χ2 | p | |||
|---|---|---|---|---|---|---|---|---|---|---|
| rs1799732 | ||||||||||
| C/C | C/del | del/del | 3.86 | 0.145 | C | del | 1.73 | 0.188 | ||
| DS | 103 | 77 (75) | 25 (24) | 1 (1) | 179 (87) | 27 (13) | ||||
| NDS | 95 | 80 (84) | 13 (14) | 2 (2) | 173 (91) | 17 (9) | ||||
| rs6276 | ||||||||||
| A/A | A/G | G/G | 2.98 | 0.226 | A | G | 1.18 | 0.277 | ||
| DS | 103 | 42 (41) | 44 (43) | 17 (17) | 128 (62) | 78 (38) | ||||
| NDS | 95 | 41 (43) | 46 (48) | 8 (8) | 128 (67) | 62 (33) | ||||
| rs1800497 | ||||||||||
| C/C | C/T | T/T | 1.57 | 0.457 | C | T | 0.002 | 0.966 | ||
| DS | 102 | 68 (67) | 29 (28) | 5 (5) | 165 (81) | 39 (19) | ||||
| NDS | 95 | 61 (6)] | 32 (34) | 2 (2) | 154 (81) | 36 (19) | ||||
Due to significant differences in gender proportions between the DS and NDS groups, we decided to perform an additional separate subgroup analysis. However, we found no significant gender-related differences in genotype or allele frequencies between DS and NDS patients (p > 0.1). No differences in genotype or allele frequencies were found between women and men in the entire sample or the DS and NDS subgroups (p > 0.1).
In our sample, the G/G genotype and rs6276 G allele were significantly more frequent in patients with family history of schizophrenia than in those without schizophrenia in the family (Table 3). Likewise, a separate subgroup analysis of DS patients showed that the G/G genotype and rs6276 G allele were significantly more frequent in patients with schizophrenia in the family, compared to those with negative family history (30% vs 10%, χ2 = 5.44, p = 0.020 and 55% vs 31%, χ2 = 10.12, p = 0.0015, respectively). These associations proved significant even after the Yates correction for small sample sizes (χ2 = 4.14, p = 0.041 and χ2 = 9.14, p = 0.0025, respectively). In the NDS group, there were no significant associations between family history of schizophrenia and genotype or allele frequencies for any of the analyzed SNPs.
Table 3.
Comparison of genotype and allele distribution of DRD2/ANKK1 SNPs between schizophrenic patients with positive and negative family history of schizophrenia
| Family history of schizophrenia | n | Genotypes N (%) | χ2 | p | Alleles N (%) | χ2 | p | |||
|---|---|---|---|---|---|---|---|---|---|---|
| rs1799732 | ||||||||||
| C/C | C/del | del/del | 5.71 | 0.058 | C | del | 2.13 | 0.144 | ||
| Positive | 45 | 31 (69) | 14 (31) | 0 (0) | 76 (84) | 14 (16) | ||||
| Negative | 150 | 123 (82) | 24 (16) | 3 (2) | 270 (90) | 30 (10) | ||||
| rs6276 | ||||||||||
| A/A | A/G | G/G | 7.22 | 0.027 | A | G | 6.84 | 0.009 | ||
| Positive | 45 | 13 (29) | 22 (49) | 10 (22) | 48 (53) | 42 (47) | ||||
| Negative | 150 | 69 (46) | 67 (45) | 14 (9) | 205 (68) | 95 (32) | ||||
| rs1800497 | ||||||||||
| C/C | C/T | T/T | 0.94 | 0.625 | C | T | 0.94 | 0.333 | ||
| Positive | 45 | 32 (71) | 12 (27) | 1 (2) | 76 (84) | 14 (16) | ||||
| Negative | 149 | 95 (64) | 48 (32) | 6 (4) | 238 (80) | 60 (20) | ||||
The DS was more frequent in patients with family history of schizophrenia than in those with negative family history (67% vs 48%, χ2 = 4.83, p = 0.028). A separate analysis of patients with family history of schizophrenia showed significant differences in rs6276 G allele distributions between DS and NDS patients (55% vs 30%, χ2 = 5.02, p = 0.0025, after Yates correction χ2 = 4.07, p = 0.044). In addition, rs6276 was also associated with family history of mental illness (Table 4). We did not find any significant associations between DRD2 and ANKK1 SNPs and other analyzed clinical parameters (Table 4).
Table 4.
Associations between DRD2 and ANKK1 gene polymorphisms and selected clinical parameters in schizophrenic patients (N = 198)
| Parameter | rs1799732 | rs6276 | rs1800497 | |||
|---|---|---|---|---|---|---|
| χ2* H# | p | χ2* H# | p | χ2* H# | p | |
| Psychiatric illness in the family | 0.08 | 0.777 | 9.54 | 0.002 | 1.98 | 0.159 |
| Neurological illness in the family | 0.06 | 0.807 | 1.08 | 0.299 | 2.52 | 0.112 |
| Age of onset (years) | 0.85 | 0.653 | 1.01 | 0.603 | 0.98 | 0.611 |
| Time delay from onset to diagnosis | 4.75 | 0.093 | 0.03 | 0.987 | 2.41 | 0.299 |
| < 1 month | ||||||
| 1–6 months | ||||||
| > 6 months | ||||||
| Withdrawal of symptoms after neuroleptics | 0.99 | 0.321 | 1.57 | 0.211 | 1.61 | 0.204 |
| Number of psychiatric hospitalizations | 2.97 | 0.226 | 0.41 | 0.814 | 3.65 | 0.161 |
| Longest episode (weeks) | 1.25 | 0.535 | 3.90 | 0.142 | 0.52 | 0.770 |
| Clinical course | 0.01 | 0.996 | 2.00 | 0.368 | 1.04 | 0.596 |
| Episodes of relapses and remissions | ||||||
| Chronic course | ||||||
| Chronic course with social withdrawal | ||||||
| MMSE | 3.07 | 0.216 | 2.18 | 0.337 | 0.47 | 0.789 |
| PANSS | ||||||
| Total | 2.51 | 0.285 | 0.33 | 0.846 | 0.70 | 0.705 |
| Positive | 4.83 | 0.090 | 0.67 | 0.717 | 0.76 | 0.684 |
| Negative | 1.32 | 0.517 | 1.34 | 0.512 | 2.64 | 0.267 |
| General | 2.37 | 0.306 | 0.02 | 0.992 | 0.50 | 0.779 |
| CGI-SCH | ||||||
| Total | 0.70 | 0.703 | 0.38 | 0.828 | 0.62 | 0.734 |
| Positive | 0.62 | 0.734 | 1.54 | 0.462 | 1.80 | 0.406 |
| Negative | 0.40 | 0.819 | 0.97 | 0.615 | 0.83 | 0.66 |
| Depressive | 0.93 | 0.627 | 0.82 | 0.66 | 1.73 | 0.421 |
| Cognitive | 0.66 | 0.718 | 0.73 | 0.693 | 2.42 | 0.298 |
| Total severity of schizophrenia | 0.83 | 0.66 | 0.27 | 0.872 | 0.03 | 0.987 |
| SDS | 0.16 | 0.924 | 0.85 | 0.654 | 1.78 | 0.411 |
* χ2 coefficient for allele comparison in Pearson’s test (genotype comparisons were abandoned due to the small numbers expected for certain genotypes)
#H coefficient, Kruskal–Wallis test for genotype comparison
Discussion
In this study, we analyzed the influence of DRD2 and ANKK1 gene polymorphisms on the disease phenotype in schizophrenic patients. Given that most antipsychotic drugs act as DRD2 antagonists, and although the results of meta-analyses remain inconclusive [29, 36, 95–98], about 35% of case–control studies suggest that at least one SNP in DRD2 is significantly associated with schizophrenia [99], we assumed that its biological underpinnings are complex and that the differences in clinical phenotype may, at least in part, result from polymorphisms in DRD2 gene. It was demonstrated that the family members of DS patients have a 1.75 times greater risk of schizophrenia compared to family members of NDS patients, and that the presence of DS in the family increases the risk of the deficit syndrome in schizophrenia patients [11, 100, 101]. Therefore, we decided to check if the presence of the “deficit syndrome” in schizophrenic patients is associated with distinct genetic factors.
Overall, we found no associations between the presence of the deficit syndrome and any of the analyzed SNPs in the entire sample of schizophrenic patients. We also found no associations with any other analyzed clinical parameters, which suggests a lack of associations between DRD2 polymorphisms and the clinical course of schizophrenia.
The only positive result was the observation that DRD2 rs6276 was significantly more frequent in patients with family history of schizophrenia. In addition, a separate analysis of this patient subgroup showed that the DRD2 rs6276 G allele was significantly more frequent in patients with DS compared to NDS, which may suggest its associations with inherited susceptibility to schizophrenia and its DS phenotype. This observation, however, needs to be further confirmed in family studies.
To the best of our knowledge, no previous studies investigated associations between SNP rs6276 in DRD2 and the phenotype of schizophrenia, but Liu et al. showed that DRD2 mRNA expression levels in chronic schizophrenia patients on clozapine treatment were correlated with severity of the deficit syndrome [27]. Chien et al. demonstrated significant associations between some SNPs and haplotypes of DRD2 (not analyzed in our study), negative symptom severity and sustained attention deficits in Han Chinese, thus supporting the hypothesis that DRD2 gene may be associated with schizophrenia phenotype [102, 103].
We found no significant links between DRD2 polymorphisms and investigated clinical parameters, except for those between rs6276, family history of schizophrenia and psychiatric disorders in general, which may be accounted for by common genetic underpinnings of psychiatric diseases and/or the fact that schizophrenia is one thereof. There exists evidence of associations between rs 1799732 and rs1800497 and the age of schizophrenia onset [31, 64], but we failed to replicate such findings, potentially attributable to population differences, random nature of these single associations or their small effect size not detected in our research due to small sample size.
Neither of the analyzed SNPs was associated with the time delay from onset to diagnosis, number of psychiatric hospitalizations, duration of longest relapse, clinical course, MMSE, PANSS, CGI-SCH or SDS scores, or symptom withdrawal after neuroleptics. However, this may result from resistance to therapy and the use of various antipsychotics, which reduces the quality of the analysis. Kang et al. [70] did not find any associations between rs1800497 and improvement of the total, positive, negative and general scores on the PANSS and the CGI-S total score after 6 weeks of amisulpride treatment. According to Ohara et al. [31], rs1799732 is not associated with the PANSS scores, while Himei et al. [41] suggest its links with the PANSS-positive score. In our study, this association did not prove significant, but close to the significance level (p < 0.1), which may suggest the existence of an association with a small size effect. However, further studies are necessary to verify this association. To date, there were no studies investigating the links between rs 6276 and PANSS, CGI-SCH or SDS, which precluded comparisons with our results, but the lack of direct associations with PANSS negative, CGI-SCH negative and SDS scores and DS/NDS status in our sample indicates links with the deficit syndrome only in patients with hereditary susceptibility to schizophrenia.
The main limitation of our study is a small sample size, which substantially reduces the power of this study, especially in subgroup analysis. Thus, our results should be considered as preliminary reports in need of further verification. Observed associations may be random and therefore require replication in larger samples and family studies. Sample size estimation was based on a desired power of 0.90 and α = 0.05 to detect medium effect size, therefore we cannot exclude a small modifier effect of the analyzed SNPs on the observed characteristics. We also analyzed a limited number of SNPs associated with DRD2. It is therefore possible that other DRD2 SNPs may have a modifying effect on the clinical course of schizophrenia. We have made every effort to ensure that the psychometric analysis is as reliable as possible, including the use of standardized scales by well-trained psychiatrists. However, symptom severity measured by the psychometric scales could be affected by various environmental factors and pharmacological therapy, and therefore the results should be interpreted carefully.
A considerable difficulty in comparing our results with previous findings is a limited number of studies investigating the relationships between the analyzed polymorphisms with schizophrenia and the fact that most of them focused on associations with the disease itself, and not necessarily its clinical course. It seems that due to its complex etiopathogenesis and varied course, the analysis of SNPs’ effect on schizophrenia phenotype should be an integral part of research on the role of genetic factors in mental disorders. More importantly, we were the first to demonstrate that rs6276 in DRD2 may be associated with the deficit syndrome in schizophrenic patients. Our results thus indicate the need for a more in-depth analysis of this polymorphism and its associations with schizophrenia. Our study also shows that research on more homogeneous patient groups, like those with family history of schizophrenia, may be beneficial in searching for disease- or symptom-related polymorphisms. This type of research could help predict the course of schizophrenia in specific patient groups.
Conclusions
In conclusion, the results of our preliminary study do not support the hypothesis that DRD2 or ANKK1 gene polymorphisms are associated with the deficit syndrome or symptom severity in the entire population of schizophrenic patients. Analyzed polymorphisms were not associated with time delay from onset to diagnosis, number of psychiatric hospitalizations, duration of longest relapse, clinical course, MMSE, PANSS, CGI-SCH and SDS scores, or symptom withdrawal after neuroleptics. The results suggest that rs6276 in DRD2 may be associated with the deficit syndrome in patients with hereditary susceptibility to schizophrenia. Confirmation of the observed dependencies requires further research.
Acknowledgements
Not applicable.
Abbreviations
- ANKK1
Ankyrin repeat and kinase domain containing 1
- CGI-SCH
Clinical Global Impression-Schizophrenia scale
- DRD2
Dopamine D2 receptor
- DS
Patients with deficit schizophrenia
- MMSE
Mini-Mental State Examination
- NDS
Patients with non-deficit schizophrenia
- PANSS
Positive and Negative Syndrome Scale
- SDS
Schedule for the Deficit Syndrome
- SNP
Single nucleotide polymorphism
Authors’ contributions
AM contributed to conceptualization, investigation and original draft preparation. JPW participated in conceptualization, investigation and original draft review and editing. JKM and MW participated in investigation (patient recruitment). BM improved the manuscript and added his remarks. JS supervised the study and participated in original draft review and editing. All authors read and approved the final manuscript.
Funding
The project was financed by the Polish Minister of Science and Higher Education under the program “Regional Initiative of Excellence” in 2019–2022, project number 002/RID/2018/19, amount of financing 12 000 000 PLN.
Availability of data and materials
The datasets analyzed/generated during this study are not publicly available due to patient confidentiality.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Pomeranian Medical University (KB-0080/169/09) and carried out in accordance with The Code of Ethics of The World Medical Association (Declaration of Helsinki). Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Simeone JC, Ward AJ, Rotella P, Collins J, Windisch R. An evaluation of variation in published estimates of schizophrenia prevalence from 1990 horizontal line 2013: a systematic literature review. BMC Psychiatry. 2015;15:193. doi: 10.1186/s12888-015-0578-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raballo A, Mechelli A, Menculini G, Tortorella A. Risk syndromes in psychiatry: a state-of-the-art overview. Arch Psychiatry Psychother. 2019;2:7–14. [Google Scholar]
- 3.Šumskiene EP, Donata KV. Biomedical and psychosocial interventions in the mental health care system in Lithuania: “Leaving the psychiatrist’s clinic—with at least a couple of prescriptions”. Arch Psychiatry Psychother. 2018;1:67–75. [Google Scholar]
- 4.Carpenter WT, Jr, Heinrichs DW, Wagman AM. Deficit and nondeficit forms of schizophrenia: the concept. Am J Psychiatry. 1988;145(5):578–583. doi: 10.1176/ajp.145.5.578. [DOI] [PubMed] [Google Scholar]
- 5.Keller WR, Fischer BA, Carpenter WT., Jr Revisiting the diagnosis of schizophrenia: where have we been and where are we going? CNS Neurosci Ther. 2011;17(2):83–88. doi: 10.1111/j.1755-5949.2010.00229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tandon R. The nosology of schizophrenia: toward DSM-5 and ICD-11. Psychiatr Clin North Am. 2012;35(3):557–569. doi: 10.1016/j.psc.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Fenton WS, McGlashan TH. Antecedents, symptom progression, and long-term outcome of the deficit syndrome in schizophrenia. Am J Psychiatry. 1994;151(3):351–356. doi: 10.1176/ajp.151.3.351. [DOI] [PubMed] [Google Scholar]
- 8.Tek C, Kirkpatrick B, Buchanan RW. A five-year followup study of deficit and nondeficit schizophrenia. Schizophr Res. 2001;49(3):253–260. doi: 10.1016/s0920-9964(00)00146-8. [DOI] [PubMed] [Google Scholar]
- 9.Strauss GP, Harrow M, Grossman LS, Rosen C. Periods of recovery in deficit syndrome schizophrenia: a 20-year multi-follow-up longitudinal study. Schizophr Bull. 2010;36(4):788–799. doi: 10.1093/schbul/sbn167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arango C, Bobes J, Kirkpatrick B, Garcia-Garcia M, Rejas J. Psychopathology, coronary heart disease and metabolic syndrome in schizophrenia spectrum patients with deficit versus non-deficit schizophrenia: findings from the CLAMORS study. Eur Neuropsychopharmacol. 2011;21(12):867–875. doi: 10.1016/j.euroneuro.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 11.Kirkpatrick B, Buchanan RW, Ross DE, Carpenter WT., Jr A separate disease within the syndrome of schizophrenia. Arch Gen Psychiatry. 2001;58(2):165–171. doi: 10.1001/archpsyc.58.2.165. [DOI] [PubMed] [Google Scholar]
- 12.Shih RA, Belmonte PL, Zandi PP. A review of the evidence from family, twin and adoption studies for a genetic contribution to adult psychiatric disorders. Int Rev Psychiatry. 2004;16(4):260–283. doi: 10.1080/09540260400014401. [DOI] [PubMed] [Google Scholar]
- 13.Sullivan PF, Kendler KS, Neale MC. Schizophrenia as a complex trait: evidence from a meta-analysis of twin studies. Arch Gen Psychiatry. 2003;60(12):1187–1192. doi: 10.1001/archpsyc.60.12.1187. [DOI] [PubMed] [Google Scholar]
- 14.Lieberman JA. Dopamine partial agonists: a new class of antipsychotic. CNS Drugs. 2004;18(4):251–267. doi: 10.2165/00023210-200418040-00005. [DOI] [PubMed] [Google Scholar]
- 15.Miyamoto S, Duncan GE, Marx CE, Lieberman JA. Treatments for schizophrenia: a critical review of pharmacology and mechanisms of action of antipsychotic drugs. Mol Psychiatry. 2005;10(1):79–104. doi: 10.1038/sj.mp.4001556. [DOI] [PubMed] [Google Scholar]
- 16.Stelzel C, Basten U, Montag C, Reuter M, Fiebach CJ. Frontostriatal involvement in task switching depends on genetic differences in d2 receptor density. J Neurosci. 2010;30(42):14205–14212. doi: 10.1523/JNEUROSCI.1062-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abi-Dargham A, Rodenhiser J, Printz D, Zea-Ponce Y, Gil R, Kegeles LS, et al. Increased baseline occupancy of D2 receptors by dopamine in schizophrenia. Proc Natl Acad Sci USA. 2000;97(14):8104–8109. doi: 10.1073/pnas.97.14.8104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schooler NR. Deficit symptoms in schizophrenia: negative symptoms versus neuroleptic-induced deficits. Acta Psychiatr Scand Suppl. 1994;380:21–26. doi: 10.1111/j.1600-0447.1994.tb05827.x. [DOI] [PubMed] [Google Scholar]
- 19.Saeedi H, Remington G, Christensen BK. Impact of haloperidol, a dopamine D2 antagonist, on cognition and mood. Schizophr Res. 2006;85(1–3):222–231. doi: 10.1016/j.schres.2006.03.033. [DOI] [PubMed] [Google Scholar]
- 20.Artaloytia JF, Arango C, Lahti A, Sanz J, Pascual A, Cubero P, et al. Negative signs and symptoms secondary to antipsychotics: a double-blind, randomized trial of a single dose of placebo, haloperidol, and risperidone in healthy volunteers. Am J Psychiatry. 2006;163(3):488–493. doi: 10.1176/appi.ajp.163.3.488. [DOI] [PubMed] [Google Scholar]
- 21.Mas S, Gasso P, de Bobadilla R, Arnaiz JA, Bernardo M, Lafuente A. Secondary nonmotor negative symptoms in healthy volunteers after single doses of haloperidol and risperidone: a double-blind, crossover, placebo-controlled trial. Hum Psychopharmacol. 2013;28(6):586–593. doi: 10.1002/hup.2350. [DOI] [PubMed] [Google Scholar]
- 22.Fusar-Poli P, Papanastasiou E, Stahl D, Rocchetti M, Carpenter W, Shergill S, et al. Treatments of Negative Symptoms in Schizophrenia: meta-Analysis of 168 Randomized Placebo-Controlled Trials. Schizophr Bull. 2015;41(4):892–899. doi: 10.1093/schbul/sbu170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de Haan L, Lavalaye J, Linszen D, Dingemans PM, Booij J. Subjective experience and striatal dopamine D(2) receptor occupancy in patients with schizophrenia stabilized by olanzapine or risperidone. Am J Psychiatry. 2000;157(6):1019–1020. doi: 10.1176/appi.ajp.157.6.1019. [DOI] [PubMed] [Google Scholar]
- 24.de Haan L, van Bruggen M, Lavalaye J, Booij J, Dingemans PM, Linszen D. Subjective experience and D2 receptor occupancy in patients with recent-onset schizophrenia treated with low-dose olanzapine or haloperidol: a randomized, double-blind study. Am J Psychiatry. 2003;160(2):303–309. doi: 10.1176/appi.ajp.160.2.303. [DOI] [PubMed] [Google Scholar]
- 25.Fervaha G, Caravaggio F, Mamo DC, Mulsant BH, Pollock BG, Nakajima S, et al. Lack of association between dopaminergic antagonism and negative symptoms in schizophrenia: a positron emission tomography dopamine D2/3 receptor occupancy study. Psychopharmacology. 2016;233(21–22):3803–3813. doi: 10.1007/s00213-016-4415-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brito-Melo GE, Nicolato R, de Oliveira AC, Menezes GB, Lelis FJ, Avelar RS, et al. Increase in dopaminergic, but not serotoninergic, receptors in T-cells as a marker for schizophrenia severity. J Psychiatr Res. 2012;46(6):738–742. doi: 10.1016/j.jpsychires.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 27.Liu L, Luo Y, Zhang G, Jin C, Zhou Z, Cheng Z, et al. Correlation of DRD2 mRNA expression levels with deficit syndrome severity in chronic schizophrenia patients receiving clozapine treatment. Oncotarget. 2017;8(49):86515–86526. doi: 10.18632/oncotarget.21230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lewis CM, Levinson DF, Wise LH, DeLisi LE, Straub RE, Hovatta I, et al. Genome scan meta-analysis of schizophrenia and bipolar disorder, part II: schizophrenia. Am J Hum Genet. 2003;73(1):34–48. doi: 10.1086/376549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yao J, Pan YQ, Ding M, Pang H, Wang BJ. Association between DRD2 (rs1799732 and rs1801028) and ANKK1 (rs1800497) polymorphisms and schizophrenia: a meta-analysis. Am J Med Genet B Neuropsychiatr Genet. 2015;168b(1):1–13. doi: 10.1002/ajmg.b.32281. [DOI] [PubMed] [Google Scholar]
- 30.Jonsson EG, Nothen MM, Grunhage F, Farde L, Nakashima Y, Propping P, et al. Polymorphisms in the dopamine D2 receptor gene and their relationships to striatal dopamine receptor density of healthy volunteers. Mol Psychiatry. 1999;4(3):290–296. doi: 10.1038/sj.mp.4000532. [DOI] [PubMed] [Google Scholar]
- 31.Ohara K, Nagai M, Tani K, Nakamura Y, Ino A. Functional polymorphism of -141C Ins/Del in the dopamine D2 receptor gene promoter and schizophrenia. Psychiatry Res. 1998;81(2):117–123. doi: 10.1016/s0165-1781(98)00092-4. [DOI] [PubMed] [Google Scholar]
- 32.Arinami T, Gao M, Hamaguchi H, Toru M. A functional polymorphism in the promoter region of the dopamine D2 receptor gene is associated with schizophrenia. Hum Mol Genet. 1997;6(4):577–582. doi: 10.1093/hmg/6.4.577. [DOI] [PubMed] [Google Scholar]
- 33.Cordeiro Q, Siqueira-Roberto J, Zung S, Vallada H. Association between the DRD2-141C Insertion/Deletion polymorphism and schizophrenia. Arq Neuropsiquiatr. 2009;67(2a):191–194. doi: 10.1590/s0004-282x2009000200004. [DOI] [PubMed] [Google Scholar]
- 34.Saiz PA, Garcia-Portilla MP, Arango C, Morales B, Arias B, Corcoran P, et al. Genetic polymorphisms in the dopamine-2 receptor (DRD2), dopamine-3 receptor (DRD3), and dopamine transporter (SLC6A3) genes in schizophrenia: data from an association study. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34(1):26–31. doi: 10.1016/j.pnpbp.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 35.Lafuente A, Bernardo M, Mas S, Crescenti A, Aparici M, Gasso P, et al. 141C Ins/Del polymorphism of the dopamine D2 receptor gene is associated with schizophrenia in a Spanish population. Psychiatr Genet. 2008;18(3):122–127. doi: 10.1097/YPG.0b013e3282fb0019. [DOI] [PubMed] [Google Scholar]
- 36.He H, Wu H, Yang L, Gao F, Fan Y, Feng J, et al. Associations between dopamine D2 receptor gene polymorphisms and schizophrenia risk: a PRISMA compliant meta-analysis. Neuropsychiatr Dis Treat. 2016;12:3129–3144. doi: 10.2147/NDT.S118614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang Y, Liu L, Xin L, Fan D, Ding N, Hu Y, et al. The -141C Ins/Del and Taq1A polymorphism in the dopamine D2 receptor gene may confer susceptibility to schizophrenia in Asian populations. J Clin Neurosci. 2016;30:1–7. doi: 10.1016/j.jocn.2015.10.052. [DOI] [PubMed] [Google Scholar]
- 38.Kurt H, Dikmen M, Basaran A, Yenilmez C, Ozdemir F, Degirmenci I, et al. Dopamine D2 receptor gene -141C Insertion/Deletion polymorphism in Turkish schizophrenic patients. Mol Biol Rep. 2011;38(2):1407–1411. doi: 10.1007/s11033-010-0244-6. [DOI] [PubMed] [Google Scholar]
- 39.Zhang XC, Ding M, Adnan A, Liu Y, Liu YP, Xing JX, et al. No association between polymorphisms in the promoter region of dopamine receptor D2 gene and schizophrenia in the northern Chinese Han population: a case–control study. Brain Behav. 2019;9(2):e01193. doi: 10.1002/brb3.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hori H, Ohmori O, Shinkai T, Kojima H, Nakamura J. Association analysis between two functional dopamine D2 receptor gene polymorphisms and schizophrenia. Am J Med Genet. 2001;105(2):176–178. doi: 10.1002/ajmg.1196. [DOI] [PubMed] [Google Scholar]
- 41.Himei A, Koh J, Sakai J, Inada Y, Akabame K, Yoneda H. The influence on the schizophrenic symptoms by the DRD2Ser/Cys311 and -141C Ins/Del polymorphisms. Psychiatry Clin Neurosci. 2002;56(1):97–102. doi: 10.1046/j.1440-1819.2002.00935.x. [DOI] [PubMed] [Google Scholar]
- 42.Lencer R, Bishop JR, Harris MS, Reilly JL, Patel S, Kittles R, et al. Association of variants in DRD2 and GRM3 with motor and cognitive function in first-episode psychosis. Eur Arch Psychiatry Clin Neurosci. 2014;264(4):345–355. doi: 10.1007/s00406-013-0464-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lencz T, Robinson DG, Xu K, Ekholm J, Sevy S, Gunduz-Bruce H, et al. DRD2 promoter region variation as a predictor of sustained response to antipsychotic medication in first-episode schizophrenia patients. Am J Psychiatry. 2006;163(3):529–531. doi: 10.1176/appi.ajp.163.3.529. [DOI] [PubMed] [Google Scholar]
- 44.Zhang JP, Lencz T, Malhotra AK. D2 receptor genetic variation and clinical response to antipsychotic drug treatment: a meta-analysis. Am J Psychiatry. 2010;167(7):763–772. doi: 10.1176/appi.ajp.2009.09040598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lencz T, Robinson DG, Napolitano B, Sevy S, Kane JM, Goldman D, et al. DRD2 promoter region variation predicts antipsychotic-induced weight gain in first episode schizophrenia. Pharmacogenet Genomics. 2010;20(9):569–572. doi: 10.1097/FPC.0b013e32833ca24b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nakazono Y, Abe H, Murakami H, Koyabu N, Isaka Y, Nemoto Y, et al. Association between neuroleptic drug-induced extrapyramidal symptoms and dopamine D2-receptor polymorphisms in Japanese schizophrenic patients. Int J Clin Pharmacol Ther. 2005;43(4):163–171. doi: 10.5414/cpp43163. [DOI] [PubMed] [Google Scholar]
- 47.Tsuchimine S, Yasui-Furukori N, Sasaki K, Kaneda A, Sugawara N, Yoshida S, et al. Association between the dopamine D2 receptor (DRD2) polymorphism and the personality traits of healthy Japanese participants. Prog Neuropsychopharmacol Biol Psychiatry. 2012;38(2):190–193. doi: 10.1016/j.pnpbp.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 48.Jonsson EG, Cichon S, Gustavsson JP, Grunhage F, Forslund K, Mattila-Evenden M, et al. Association between a promoter dopamine D2 receptor gene variant and the personality trait detachment. Biol Psychiatry. 2003;53(7):577–584. doi: 10.1016/s0006-3223(02)01732-8. [DOI] [PubMed] [Google Scholar]
- 49.Zhang XR, Zhang ZJ, Zhu RX, Yuan YG, Jenkins TA, Reynolds GP. Sexual dysfunction in male schizophrenia: influence of antipsychotic drugs, prolactin and polymorphisms of the dopamine D2 receptor genes. Pharmacogenomics. 2011;12(8):1127–1136. doi: 10.2217/pgs.11.46. [DOI] [PubMed] [Google Scholar]
- 50.Suda A, Kawanishi C, Kishida I, Sato R, Yamada T, Nakagawa M, et al. Dopamine D2 receptor gene polymorphisms are associated with suicide attempt in the Japanese population. Neuropsychobiology. 2009;59(2):130–134. doi: 10.1159/000213566. [DOI] [PubMed] [Google Scholar]
- 51.Johann M, Putzhammer A, Eichhammer P, Wodarz N. Association of the -141C Del variant of the dopamine D2 receptor (DRD2) with positive family history and suicidality in German alcoholics. Am J Med Genet B Neuropsychiatr Genet. 2005;132(1):46–49. doi: 10.1002/ajmg.b.30085. [DOI] [PubMed] [Google Scholar]
- 52.Konishi T, Luo HR, Calvillo M, Mayo MS, Lin KM, Wan YJ. ADH1B*1, ADH1C*2, DRD2 (-141C Ins), and 5-HTTLPR are associated with alcoholism in Mexican American men living in Los Angeles. Alcohol Clin Exp Res. 2004;28(8):1145–1152. doi: 10.1097/01.alc.0000134231.48395.42. [DOI] [PubMed] [Google Scholar]
- 53.Zhang S, Zhang J. The Association of DRD2 with Insight Problem Solving. Front Psychol. 2016;7:1865. doi: 10.3389/fpsyg.2016.01865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang S, Zhang M, Zhang J. An exploratory study on DRD2 and creative potential. Creat Res J. 2014;26(1):115–123. [Google Scholar]
- 55.van Munster BC, de Rooij S, Yazdanpanah M, Tienari PJ, Pitkala KH, Osse RJ, et al. The association of the dopamine transporter gene and the dopamine receptor 2 gene with delirium, a meta-analysis. Am J Med Genet B Neuropsychiatr Genet. 2010;153b(2):648–655. doi: 10.1002/ajmg.b.31034. [DOI] [PubMed] [Google Scholar]
- 56.Lucht M, Barnow S, Schroeder W, Grabe HJ, Rosskopf D, Brummer C, et al. Alcohol consumption is associated with an interaction between DRD2 exon 8 A/A genotype and self-directedness in males. Neuropsychobiology. 2007;56(1):24–31. doi: 10.1159/000109974. [DOI] [PubMed] [Google Scholar]
- 57.Qadri YJ, Bortsov AV, Orrey DC, Swor RA, Peak DA, Jones JS, et al. Genetic polymorphisms in the dopamine receptor 2 predict acute pain severity after motor vehicle collision. Clin J Pain. 2015;31(9):768–775. doi: 10.1097/AJP.0000000000000167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Crocco P, Montesanto A, Passarino G, Rose G. Polymorphisms falling within putative miRNA target sites in the 3′UTR region of SIRT2 and DRD2 genes are correlated with human longevity. J Gerontol A Biol Sci Med Sci. 2016;71(5):586–592. doi: 10.1093/gerona/glv058. [DOI] [PubMed] [Google Scholar]
- 59.Tunbridge EM, Narajos M, Harrison CH, Beresford C, Cipriani A, Harrison PJ. Which dopamine polymorphisms are functional? systematic review and meta-analysis of COMT, DAT, DBH, DDC, DRD1-5, MAOA, MAOB, TH, VMAT1, and VMAT2. Biol Psychiatry. 2019;86(8):608–620. doi: 10.1016/j.biopsych.2019.05.014. [DOI] [PubMed] [Google Scholar]
- 60.Cordeiro Q, Vallada H. Association study between the Taq1A (rs1800497) polymorphism and schizophrenia in a Brazilian sample. Arq Neuropsiquiatr. 2014;72(8):582–586. doi: 10.1590/0004-282x20140100. [DOI] [PubMed] [Google Scholar]
- 61.Dubertret C, Bardel C, Ramoz N, Martin PM, Deybach JC, Ades J, et al. A genetic schizophrenia-susceptibility region located between the ANKK1 and DRD2 genes. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34(3):492–499. doi: 10.1016/j.pnpbp.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 62.Arab AH, Elhawary NA. Association between ANKK1 (rs1800497) and LTA (rs909253) Genetic Variants and Risk of Schizophrenia. Biomed Res Int. 2015;2015:821827. doi: 10.1155/2015/821827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Aslan S, Karaoguz MY, Eser HY, Karaer DK, Taner E. Comparison of DRD2 rs1800497 (TaqIA) polymorphism between schizophrenic patients and healthy controls: lack of association in a Turkish sample. Int J Psychiatry Clin Pract. 2010;14(4):257–261. doi: 10.3109/13651501.2010.492913. [DOI] [PubMed] [Google Scholar]
- 64.Zhang C, Zhang J, Fan J, Cheng W, Du Y, Yu S, et al. Identification of ANKK1 rs1800497 variant in schizophrenia: new data and meta-analysis. Am J Med Genet B Neuropsychiatr Genet. 2014;165(7):564–571. doi: 10.1002/ajmg.b.32259. [DOI] [PubMed] [Google Scholar]
- 65.Muller DJ, Zai CC, Sicard M, Remington E, Souza RP, Tiwari AK, et al. Systematic analysis of dopamine receptor genes (DRD1-DRD5) in antipsychotic-induced weight gain. Pharmacogenomics J. 2012;12(2):156–164. doi: 10.1038/tpj.2010.65. [DOI] [PubMed] [Google Scholar]
- 66.Ikeda M, Yamanouchi Y, Kinoshita Y, Kitajima T, Yoshimura R, Hashimoto S, et al. Variants of dopamine and serotonin candidate genes as predictors of response to risperidone treatment in first-episode schizophrenia. Pharmacogenomics. 2008;9(10):1437–1443. doi: 10.2217/14622416.9.10.1437. [DOI] [PubMed] [Google Scholar]
- 67.Zou YF, Wang F, Feng XL, Li WF, Tian YH, Tao JH, et al. Association of DRD2 gene polymorphisms with mood disorders: a meta-analysis. J Affect Disord. 2012;136(3):229–237. doi: 10.1016/j.jad.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 68.Zhang L, Hu L, Li X, Zhang J, Chen B. The DRD2 rs1800497 polymorphism increase the risk of mood disorder: evidence from an update meta-analysis. J Affect Disord. 2014;158:71–77. doi: 10.1016/j.jad.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 69.Takeuchi H, Tomita H, Taki Y, Kikuchi Y, Ono C, Yu Z, et al. The associations among the dopamine D2 receptor Taq1, emotional intelligence, creative potential measured by divergent thinking, and motivational state and these associations’ sex differences. Front Psychol. 2015;6:912. doi: 10.3389/fpsyg.2015.00912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kang SG, Na KS, Lee HJ, Chee IS, Lee K, Lee J. DRD2 genotypic and haplotype variation is associated with improvements in negative symptoms after 6 weeks’ amisulpride treatment. J Clin Psychopharmacol. 2015;35(2):158–162. doi: 10.1097/JCP.0000000000000294. [DOI] [PubMed] [Google Scholar]
- 71.WHO . The ICD-10 Classification of Mental and Behavioural Disorders. Diagnostic criteria for research. Geneva: World Health Organization; 1993. [Google Scholar]
- 72.Pużyński S, Wciórka J. Klasyfikacja zaburzeń psychicznych i zaburzeń zachowania w ICD-10. Badawcze kryteria diagnostyczne. Kraków: Vesalius; 2000. [Google Scholar]
- 73.Gaebel W, Kerst A. ICD-11 Mental, behavioural or neurodevelopmental disorders: innovations and managing implementation. Arch Psychiatry Psychother. 2019;3:7–12. [Google Scholar]
- 74.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 75.McGuffin P, Farmer A, Harvey I. A polydiagnostic application of operational criteria in studies of psychotic illness. Development and reliability of the OPCRIT system. Arch Gen Psychiatry. 1991;48(8):764–770. doi: 10.1001/archpsyc.1991.01810320088015. [DOI] [PubMed] [Google Scholar]
- 76.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 77.Rzewuska M. Badanie zgodności i niezawodności polskiej wersji skali PANSS [Examination of compliance and reliability of the Polish version of the PANSS scale] Farmakoterapia w Psychiatrii i Neurologii. 2004;4:390–398. [Google Scholar]
- 78.Leucht S, Kissling W, Davis JM. The PANSS should be rescaled. Schizophr Bull. 2010;36(3):461–462. doi: 10.1093/schbul/sbq016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Obermeier M, Mayr A, Schennach-Wolff R, Seemuller F, Moller HJ, Riedel M. Should the PANSS be rescaled? Schizophr Bull. 2010;36(3):455–460. doi: 10.1093/schbul/sbp124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Haro JM, Kamath SA, Ochoa S, Novick D, Rele K, Fargas A, et al. The Clinical Global Impression-Schizophrenia scale: a simple instrument to measure the diversity of symptoms present in schizophrenia. Acta Psychiatr Scand Suppl. 2003;416:16–23. doi: 10.1034/j.1600-0447.107.s416.5.x. [DOI] [PubMed] [Google Scholar]
- 81.Pełka-Wysiecka J. [Genetic and physiologic markers of negative symptoms in schizophrenia: a search for the biologically founded deficit phenotype of the disease]. In: Kojder I, editor. Annales Academiae Medicae Stetinensis. supplement 175. Szczecin: Pomeranian Medical University in Szczecin; 2013.
- 82.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 83.Stańczak J. MMSE - polska normalizacja [MMSE - polish normalization]. Psychological Test Laboratory of Polish Psychological Association; 2010.
- 84.Jarema M, Kiejna A, Landowski J, Meder J, Jolanta RJ, Rybakowski J. Pharmacological standards in schizophrenia treatment. Psychiatr Pol. 2006;40(6):1171–1205. [PubMed] [Google Scholar]
- 85.Tybura P, Samochowiec A, Beszlej A, Grzywacz A, Mak M, Frydecka D, et al. Some dopaminergic genes polymorphisms are not associated with response to antipsychotic drugs in schizophrenic patients. Pharmacol Rep. 2012;64(3):528–535. doi: 10.1016/s1734-1140(12)70848-4. [DOI] [PubMed] [Google Scholar]
- 86.Jaracz J, Tetera-Rudnicka E, Kujath D, Raczynska A, Stoszek S, Czernas W, et al. The prevalence of antipsychotic polypharmacy in schizophrenic patients discharged from psychiatric units in Poland. Pharmacol Rep. 2014;66(4):613–617. doi: 10.1016/j.pharep.2014.02.024. [DOI] [PubMed] [Google Scholar]
- 87.Jarema M, Wichniak A, Dudek D, Samochowiec J, Bienkowski P, Rybakowski J. Guidelines for the use of second-generation long-acting antipsychotics. Psychiatr Pol. 2015;49(2):225–241. doi: 10.12740/PP/39370. [DOI] [PubMed] [Google Scholar]
- 88.Kirkpatrick B, Buchanan RW, McKenney PD, Alphs LD, Carpenter WT., Jr The Schedule for the Deficit syndrome: an instrument for research in schizophrenia. Psychiatry Res. 1989;30(2):119–123. doi: 10.1016/0165-1781(89)90153-4. [DOI] [PubMed] [Google Scholar]
- 89.Pelka-Wysiecka J, Wronski M, Jasiewicz A, Grzywacz A, Tybura P, Kucharska-Mazur J, et al. BDNF rs 6265 polymorphism and COMT rs 4680 polymorphism in deficit schizophrenia in Polish sample. Pharmacol Rep. 2013;65(5):1185–1193. doi: 10.1016/s1734-1140(13)71476-2. [DOI] [PubMed] [Google Scholar]
- 90.Pelka-Wysiecka J, Wronski M, Bienkowski P, Murawiec S, Samochowiec A, Samochowiec J. Odors identification differences in deficit and nondeficit schizophrenia. Pharmacol Rep. 2016;68(2):390–395. doi: 10.1016/j.pharep.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 91.Tyburski E, Pelka-Wysiecka J, Mak M, Samochowiec A, Bienkowski P, Samochowiec J. Neuropsychological Profile of Specific Executive Dysfunctions in Patients with Deficit and Non-deficit Schizophrenia. Front Psychol. 2017;8:1459. doi: 10.3389/fpsyg.2017.01459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bienkowski P, Samochowiec J, Pelka-Wysiecka J, Grzywacz A, Skibinska M, Jasiewicz A, et al. Functional polymorphism of matrix metalloproteinase-9 (MMP9) gene is not associated with schizophrenia and with its deficit subtype. Pharmacol Rep. 2015;67(3):442–445. doi: 10.1016/j.pharep.2014.11.007. [DOI] [PubMed] [Google Scholar]
- 93.Miller SA, Dykes DD, Polesky HF. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 1988;16(3):1215. doi: 10.1093/nar/16.3.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed: Lawrence Erlbaum Associates; 1988.
- 95.Gurling HMD, McQuillin A. The genetics of schizophrenia. In: Nurnberger JJ, Berrettini W, editors. Principles of Psychiatric Genetics. Cambridge: Cambridge University Press; 2012. pp. 230–261. [Google Scholar]
- 96.Allen NC, Bagade S, McQueen MB, Ioannidis JP, Kavvoura FK, Khoury MJ, et al. Systematic meta-analyses and field synopsis of genetic association studies in schizophrenia: the SzGene database. Nat Genet. 2008;40(7):827–834. doi: 10.1038/ng.171. [DOI] [PubMed] [Google Scholar]
- 97.Shi J, Gershon ES, Liu C. Genetic associations with schizophrenia: meta-analyses of 12 candidate genes. Schizophr Res. 2008;104(1–3):96–107. doi: 10.1016/j.schres.2008.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Glatt SJ, Faraone SV, Tsuang MT. DRD2 -141C insertion/deletion polymorphism is not associated with schizophrenia: results of a meta-analysis. Am J Med Genet B Neuropsychiatr Genet. 2004;128b(1):21–23. doi: 10.1002/ajmg.b.30007. [DOI] [PubMed] [Google Scholar]
- 99.Edwards AC, Bacanu SA, Bigdeli TB, Moscati A, Kendler KS. Evaluating the dopamine hypothesis of schizophrenia in a large-scale genome-wide association study. Schizophr Res. 2016;176(2–3):136–140. doi: 10.1016/j.schres.2016.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dollfus S, Ribeyre JM, Petit M. Family history and deficit form in schizophrenia. Eur Psychiatry. 1996;11(5):260–262. doi: 10.1016/0924-9338(96)82333-9. [DOI] [PubMed] [Google Scholar]
- 101.Ross DE, Kirkpatrick B, Karkowski LM, Straub RE, MacLean CJ, O’Neill FA, et al. Sibling correlation of deficit syndrome in the Irish study of high-density schizophrenia families. Am J Psychiatry. 2000;157(7):1071–1076. doi: 10.1176/appi.ajp.157.7.1071. [DOI] [PubMed] [Google Scholar]
- 102.Chien YL, Hwu HG, Fann CS, Chang CC, Tsuang MT, Liu CM. DRD2 haplotype associated with negative symptoms and sustained attention deficits in Han Chinese with schizophrenia in Taiwan. J Hum Genet. 2013;58(4):229–232. doi: 10.1038/jhg.2012.157. [DOI] [PubMed] [Google Scholar]
- 103.Wang YM. A commentary on DRD2 haplotype associated with negative symptoms and sustained attention deficits in Han Chinese with schizophrenia in Taiwan. J Hum Genet. 2013;58(4):182. doi: 10.1038/jhg.2013.13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed/generated during this study are not publicly available due to patient confidentiality.