COVID-19 has manifested as twin public health and economic crises. In mid-Missouri, after shelter-in-place orders during the first wave, social and physical distancing appears to have worked well so far. The risks associated with reopening remain uncertain, but we have had the opportunity to learn best practices from other communities and health systems.
To date, approximately 10% of symptomatic (since early March) and also preoperative (since late April) patients statewide have tested positive for COVID-19. In Boone County, that number is reportedly closer to 2–3%.1,2 The good news is that the first wave of COVID-19 was less severe in mid-Missouri than we had feared; the bad news is that we remain quite vulnerable to future waves of infection coming from either coast. Amid the tragedy, we have also been inspired by the innovations of our local community.
MU Emergency Department Response and Experience
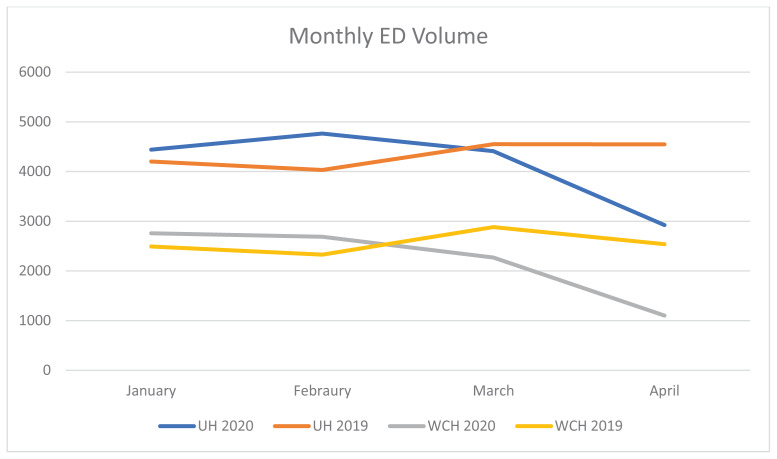
Emergency Departments (ED) have seen plummeting patient volumes, both nationally and in mid-Missouri. When comparing to the pre-COVID admission rate, the University of Missouri (MU) EDs saw a 43% drop in overall ED volume in April 2020 compared to 2019 (Figure 1). The initial approach to the COVID-19 pandemic at the MU EDs was multi-faceted and encompassed three main areas: safety, clinical care, and education.
Figure 1.
Monthly ED volume at University Hospital and Women & Children’s Hospital.
For emergency medicine (EM) physicians, the response is a natural outgrowth of our training. EM physicians are trained to be flexible and think “outside the box” in order to rapidly adapt to new situations. Learning from our Italian colleagues, we quickly divided our ED into two main areas: a “clean” and a “dirty” section. Patients were screened prior to physical entry into the ED for fevers and respiratory symptoms. Those who screened positive for these symptoms were separately admitted to the “dirty” side, in an effort to cohort possible COVID+ patients. Initially, the ED entrance was a tent; over time, this was upgraded to a shipping container-type building for our screening staff. This upgrade was necessary after accounting for staff needs of heating, air conditioning, and protection from the elements.
In another effort to keep potentially infectious patients away from the ED, we initiated telemedicine visits across the system for general health as well as for COVID screening. A remote drive-through COVID testing center was opened, and the timing was coordinated with similar efforts at Boone Hospital Center. Patients were given the option of a virtual screening visit, or to come to the drive-through site, and to be questioned using a nursing protocol. At our peak, over 200 patients were utilizing drive-through testing daily.
If one word were to describe our ED response to this pandemic, it would be “innovation.” We converted our decontamination room to use as a COVID code room. Having an entrance to the outside prevented the critical concern of having a possibly infectious patient from passing through a clean ED. We outfitted that room to the same standard as one of our resuscitation rooms. Another benefit to the use of this room was that it was equipped for negative pressure. One of our faculty, Adam Beckett, MD, and his Global First Responder colleagues, also designed a portable airway protection device to help keep his ED and EMS colleagues safe when performing high risk procedures like intubation. We have also been inspired by community efforts to #HackThePandemic, from a local high school student who 3D-printed face shields for distribution,3 to the collaborations between the Columbia STEM alliance and the MU College of Engineering, and across the University of Missouri campus, where a MU Textile and Apparel Management student innovated a way to use a laser cutter to cut 10,000 pieces of cloth daily, to address the shortage of masks.4
Personal protective equipment (PPE) has been a national concern as well as at our facility. Thankfully, we have never reached the point of inadequate PPE, but cleaning and reusing N-95 masks is definitely the new normal. Our institution also implemented UVC for decontamination.5 Who would have ever thought that a recommendation to use bandanas as face coverings would be featured on the CDC website? We also learned the side effects of long-term mask usage, previously used for only limited patient encounters, that we now wear for 8–12 hour shifts. Painful noses and facial abrasions were some of the new problems that our frontline healthcare workers have encountered.
The patient and family experience has also changed greatly. In conjunction with increased COVID-19 case numbers, stricter visitor rules were implemented. For most patients, this meant being in the ED without loved ones or advocates. Creative solutions such as video conferencing were used to help connect patients with their families. Perhaps the hardest times were with critically ill or dying patients. To not be able to spend your final moments with your family takes an emotional toll not just on families, but also on staff who sometimes feel that they have had to take on the role of supportive family members amid this pandemic. We certainly worry about burnout and compassion fatigue among all our caregivers.
Despite everything, morale has remained high in the ED over the past few months. Community support has been amazing, from uplifting messages to the meals provided for frontline workers. Hopefully, what we have learned in this first wave will enable us to work more safely and efficiently in future spikes.
Boone County Medical Society (BCMS) COVID-19 Outreach
Although there is undeniable tragedy that comes with a pandemic, there are also opportunities. This pandemic has highlighted the cracks in the structure of our health care delivery systems, economy, and social welfare systems. Now more than ever, there is a role for organized medicine to provide a voice for our physicians on the frontlines, as well as to connect our physician community and provide timely and helpful information.
Given that data on COVID-19 has been limited, preliminary, and rapidly evolving, our Boone County Medical Society (BCMS) began hosting weekly webinars on COVID-19 on March 24, 2020. These webinars have been an important source of information for all our community physicians, and we opened up attendance to members and nonmembers alike, as well as to residents, fellows, and medical students throughout Missouri. It has also provided a forum to ask questions of our local experts.1,2.5
We have had speakers from our state and local health departments as well as leaders and physicians from all three major local hospital systems. It has been reassuring and heartening to know that leaders from all three local hospital systems are meeting weekly to strategize and to craft consistent and organized messaging and local responses. Especially in light of recent reports of conflict between state and local health departments in other states, it is comforting to see and hear our state and local health departments working closely together. Early, consistent and cohesive communication is critically important during this global crisis.
Almost every week, we have had a speaker representing the public health perspective, represented by Ashley Millham, MD, Medical Director of Boone County Public Health & Human Services and Randall Williams, MD, Director of the Missouri Department of Health & Senior Services. We have had an infectious disease physician speaker on most weeks, in which Christian Rojas-Moreno, MD, and Taylor Nelson, MD, have shared the latest research and their invaluable clinical experience at the University of Missouri. Christopher Sampson, MD, and Jonathan Heidt, MD, have contributed their experiences from the ED at MU. Outside of our MU system, we have also had speakers from the other two major health systems in our community: Robin Blount, MD, Chief Medical Officer (CMO) of Boone Hospital, and Lana Zerrer, MD, CMO of Truman VA Hospital.
We are heartened to learn that we continue to have significant PCR testing capabilities here in mid-Missouri;1,2 testing in Boone County has been bolstered (both in volume and rapid turn-around times) in part because GeneTrait has a local lab facility in Columbia, MO. Our public health officials have a systematic and thoughtful strategy for identifying and containing outbreaks at long-term care facilities. We have learned of the challenges facing our private hospitals and academic and private physician practice practices. We are impressed with the preparedness and innovation at the VA, where they did not suffer as many concerns over PPE shortages due to a federal mandate for pandemic preparedness; they are also making regular contact with each of the 40,000 veterans in their catchment area, which is an important and large undertaking.
The cancellations of schools, churches, and sports; the physical distancing; and the economic stressors associated with COVID-19 have also raised concern about physician wellness and worsened physician burnout during this pandemic, so we invited Steven Keithahn, MD Chief Wellness Officer at MU HealthCare and Craig Rooney, PhD, Program Director of the Office of Clinician Well-Being at MU School of Medicine to discuss physician autonomy, increased moral injury, and the defining point between burnout and depression. Dr. Keithahn also emphasized the importance of organized medicine in harnessing and amplifying our collective physician voices. To represent organized medicine, Jeff Howell, JD and Heidi Geisbuhler from the Missouri State Medical Association (MSMA) have also been regular speakers at our webinars, taking time out of their busy days to give us the latest updates2,6 on state legislative action in Jefferson City. We were dismayed that the PDMP still did not pass this spring, but we are encouraged by many of the public health and medicine-friendly measures that did.6
These webinars have also been very helpful for disseminating best practices and for a clinical discussion of the early evidence. For example, clinical experience with convalescent plasma; toclizumab; and hydroxycholoroquine +/− azithromycin; and remdesivir were reviewed in our webinars.1,2 We also had a wonderful discussion about how antibody testing is helpful for prevalence testing (from the publichealth perspective) but currently useless (despite being overly-marketed) to demonstrate durable immunity.7,8 This has empowered our physicians to better educate their patients and colleagues, and also provided an opportunity to discuss public health measures, like mask-wearing. While masks may have a role in source control, we are cognizant that not everyone can or even should wear a mask in public.1,9 Some reasons to not wear a mask include:
Concerns that mask-wearing may breed complacency in the wearer (such that wearers may want to attend a parade, rock concert, or Mardi Gras celebration), as masks are complementary to physical distancing and staying 6 feet apart;
Possible risks to the wearer if the cloth mask gets wet or soiled;
Possible risks to the wearer if the inside of the cloth mask gets dirty or contaminated;
If the wearer gets severely claustrophobic or anxious, has significant breathing difficulties, or otherwise cannot wear a mask safely (which, in turn, should be further evaluated as a concerning medical condition).1,
Finally, Boone County Medical Society leadership (together with Debra Howenstine, MD) has served as a source of mentors and advisors for an inspiring medical student and MPH student volunteer response to COVID-19. This spring, the rising fourth-year medical students have an unbelievable set of stressors. These stressors include removal from inpatient experiences in their recent clinical clerkships (in accordance with national AAMC guidance), a national cancellation of all upcoming “away” rotations, a national conversion of their upcoming fall interview season to an all-virtual format, and a lack of transparency and information about abrupt cancellations of high-stakes NBME exams. Indeed, in some cases, students have shown up at testing sites to take Step 1 or Step 2, only to find their Prometric testing center closed!10
Despite these colossal sources of stress and anxiety, a student leadership team at MU (including MS1 Ben VanAmberg, MS3 Eric Grisham, MS3 Natalie Miller, MS3 Zeke Kapusciak, MS3 Lucy Sheahan, MS3 Elizabeth Modde, MS3 Shelly D’Alessandro, MS3 Ramya Ramadas, and new graduates Abbi Berry, MD and Colbey Ricklefs, MD) has been organizing grocery delivery to individuals quarantined for COVID-19, sharing positive stories via social media, and raising funds for several local organizations (including our food bank, homeless shelters, and soup kitchens). Students have also been involved in outreach and advocacy. Under the leadership of Abbi Berry and MS2 Cynthia Tang, students have created a “COVID infographic” based on CDC guidance, translated it into 14 languages, and distributed it among community partners. Led by MS3 Nikki Kagan, MS3 Taylor Ross and new graduate Calli Morris, MD, a student group also successfully lobbied our Governor for the “Stay Home” order in March, and lobbied against proposed measures to strip local Public Health Agencies of enforcement authority. With MS2 Patricia DeCastro and MS3 Clarence Chu, another student team is writing letters to senior citizens at nursing homes, to help brighten their days amid the social isolation of this pandemic.
Under the leadership of new graduate Toby Bradford, MD yet another student team wrote, directed, and produced five episodes of “Love is Viral,” a spoof of the “Love is Blind” Netflix show, about dating during COVID-19.11 These videos were designed to target 16–25 year-olds with messaging about the importance of social distancing and stay-home orders. 11 Medical students have also written articles about how a small craft distillery shifted production from spirits and cocktails to hand sanitizer,12 and about how one local homeless shelter and community resource had readjusted to “stay home” orders when community members have unstable housing.13
Summary
COVID-19 has been a tremendous ongoing global tragedy. Amid ever-evolving public health guidelines, COVID-19 places physicians and other health care providers in a climate of anxiety, uncertainty, feelings of helplessness, and worries about the future. For those who see things as “black-and-white” and may have previously been overly dependent on guidelines and algorithms, this may be a particularly difficult time. The need for social and physical distancing, and the rapid and massive expansion of telemedicine, is revolutionizing healthcare. In learning to live with uncertainty, we should learn that with every plan, we must be flexible, prepared to absorb new information, and ready to change direction with very little notice. Moving forward, our community is closer together than it was, pre-COVID. After all, we’re all in this together, and nobody is on the “side” of coronavirus. This is also a fine time to get involved in your local and state medical societies, to stay informed, to voice your concerns, and to advocate for our patients and profession. Together, we are stronger.
Acknowledgment
We appreciate the invaluable efforts of Sarah Luebbert, Gordon Casey, and Alan Hillard, MD, in making our BCMS webinars possible.
Footnotes
Christopher Sampson, MD, is an Emergency Physician at the University of Missouri-Columbia; Amy Zguta, MD, MSMA member since 2012, is a private practice Ophthalmologist; Albert Hsu, MD, MSMA member since 2017, (left), is an Ob/Gyn and Reproductive Endocrinologist at the University of Missouri - Columbia.
References
- 1.Boone County Medical Society (BCMS) COVID resources and BCMS webinars. at https://www.boonecountymedicalsociety.org/covid-19-resources.html.
- 2.Missouri State Medical Association conference calls with Dr. Randall Williams. https://www.msma.org/covid19-conf-calls.html.
- 3.High School Student 3D Prints face shields amidst PPE shortage. Apr 2, 2020. at < https://krcgtv.com/news/local/high-school-student-3d-prints-face-sheilds-amidst-ppe-shortage> versus https://engineering.missouri.edu/2020/05/mu-partners-with-community-to-produce-face-shields/
- 4.Cutting Cloth to Curb COVID: How one MU student lends her textile talents to fighting the COVID pandemic. Apr 21, 2020. at https://medium.com/@courageincovid/cutting-cloth-to-curb-covid-85597e330ced.
- 5.N95 decon. at https://www.n95decon.org/uvc.
- 6.Missouri State Medical Association legislative “big wins”. at https://www.msma.org/big-wins.html.
- 7.NYS DOH (4/22/20) “Dear Colleague” letter to physicians, about antibody tests being marketed inappropriately, as antibody testing does *not* indicate durable immunity. at https://www1.nyc.gov/assets/doh/downloads/pdf/han/alert/2020/covid-19-status-of-serologic-testing.pdf.
- 8.Yale statement (4/22/20) on serology testing. at https://bit.ly/YaleSerology.
- 9.2019-nCoV – What We Know So Far About … Wearing Masks in Public. at < https://www.publichealthontario.ca/-/media/documents/ncov/covid-wwksf/what-we-know-public-masks-apr-7-2020.pdf?la=en>.
- 10.Step 1 scramble: Test-center closures leave medical students in limbo. May 8, 2020. at < https://www.ama-assn.org/residents-students/usmle/step-1-scramble-test-center-closures-leave-medical-students-limbo>.
- 11.“’Love is Viral’: MU medical students bring social distancing to Instagram”. at < https://www.columbiamissourian.com/news/covid19/love-is-viral-mu-medical-students-bring-social-distancing-to-instagram/article_54766882-791c-11ea-af46-5b6094a8e73f.html>.
- 12.From Crafting Spirits to Crafting Hand Sanitizer. Apr 30, 2020. at < https://medium.com/@courageincovid/from-crafting-spirits-to-crafting-hand-sanitizer-cc92abf6140b>.
- 13.’Staying Home’ While Homeless. Apr 29, 2020. at < https://medium.com/@courageincovid/staying-home-while-homeless-55c76aa648b9>.