Existing American Heart Association cardiopulmonary resuscitation (CPR) guidelines do not address the challenges of providing resuscitation in the setting of the coronavirus disease 2019 (COVID-19) global pandemic, wherein rescuers must continuously balance the immediate needs of the patients with their own safety. To address this gap, the American Heart Association, in collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, The Society of Critical Care Anesthesiologists, and American Society of Anesthesiologists, and with the support of the American Association of Critical Care Nurses and National Association of EMS Physicians, has compiled interim guidance to help rescuers treat individuals with cardiac arrest with suspected or confirmed COVID-19.
Over the past 2 decades, there has been a steady improvement in survival after cardiac arrest occurring both inside and outside the hospital.1 That success has relied on initiating proven resuscitation interventions such as high-quality chest compressions and defibrillation within seconds to minutes. The evolving and expanding outbreak of severe acute respiratory syndrome coronavirus 2 infections has created important challenges to such resuscitation efforts and requires potential modifications of established processes and practices. The challenge is to ensure that patients with or without COVID-19 who experience cardiac arrest get the best possible chance of survival without compromising the safety of rescuers, who will be needed to care for future patients. Complicating the emergency response to both out-of-hospital and in-hospital cardiac arrest is that COVID-19 is highly transmissible, particularly during resuscitation, and carries a high morbidity and mortality.
Approximately 12% to 19% of COVID-positive patients require hospital admission, and 3% to 6% become critically ill.2–4 Hypoxemic respiratory failure secondary to acute respiratory distress syndrome, myocardial injury, ventricular arrhythmias, and shock are common among critically ill patients and predispose them to cardiac arrest,5–8 as do some of the proposed treatments such as hydroxychloroquine and azithromycin, which can prolong the QT.9 With infections currently growing exponentially in the United States and internationally, the percentage of patients with cardiac arrests and COVID-19 is likely to increase.
Healthcare workers are already the highest-risk profession for contracting the disease.10 This risk is compounded by worldwide shortages of personal protective equipment (PPE). Resuscitations carry added risk to healthcare workers for many reasons. First, the administration of CPR involves performing numerous aerosol-generating procedures, including chest compressions, positive-pressure ventilation, and establishment of an advanced airway. During those procedures, viral particles can remain suspended in the air with a half-life of ≈1 hour and be inhaled by those nearby.11 Second, resuscitation efforts require numerous providers to work in close proximity to one another and the patient. Finally, these are high-stress emergency events in which the immediate needs of the patient requiring resuscitation may result in lapses in infection-control practices.
In arriving at this interim guidance, we reviewed existing American Heart Association CPR recommendations in the context of the COVID-19 pandemic and considered the unique pathophysiology of COVID-19 with reversal of hypoxemia as a central goal. We sought to balance the competing interests of providing timely and high-quality resuscitation to patients and simultaneously protecting rescuers. This statement applies to all adult, pediatric, and neonatal resuscitations in patients with suspected or confirmed COVID-19 infection unless otherwise noted. The guidance contained herein is based on expert opinion and needs to be adapted locally on the basis of current disease burden and resource availability.
General Principles for Resuscitation in Patients with Suspected and Confirmed COVID-19
Reduce Provider Exposure to COVID-19
Rationale
It is essential that providers protect themselves and their colleagues from unnecessary exposure. Exposed providers who contract COVID-19 further decrease the already strained workforce available to respond and have the potential to add additional strain if they become critically ill.
Strategies
1. Before entering the scene, all rescuers should don PPE to guard against contact with both airborne and droplet particles. Consult individual health or emergency medical services (EMS) system standards because PPE recommendations may vary considerably on the basis of current epidemiological data and availability.
2. Limit personnel in the room or on the scene to only those essential for patient care.
3. In settings with protocols in place and expertise in their use, consider replacing manual chest compressions with mechanical CPR devices to reduce the number of rescuers required for adults and adolescents who meet the manufacturer’s height and weight criteria.
4. Clearly communicate COVID-19 status to any new providers before their arrival on the scene or receipt of the patient when transferring to a second setting.
Prioritize Oxygenation and Ventilation Strategies With Lower Aerosolization Risk
Rationale
Although the procedure of intubation carries a high risk of aerosolization, if the patient is intubated with a cuffed endotracheal tube and connected to a ventilator with a high-efficiency particulate air (HEPA) filter in the path of exhaled gas and an inline suction catheter, the resulting closed circuit carries a lower risk of aerosolization than any other form of positive-pressure ventilation.12
Strategies
5. Attach a HEPA filter securely, if available, to any manual or mechanical ventilation device in the path of exhaled gas before administering any breaths.
6. After healthcare providers assess the rhythm and defibrillate any ventricular arrhythmias, patients in cardiac arrest should be intubated with a cuffed tube at the earliest feasible opportunity. Connect the endotracheal tube to a ventilator with a HEPA filter when available.
-
7. Minimize the likelihood of failed intubation attempts by the following:
a. Assigning the provider and approach with the best chance of first-pass success to intubate
b. Pausing chest compressions to intubate
8. Video laryngoscopy may reduce intubator exposure to aerosolized particles and should be considered if available.
9. Before intubation, use a bag-mask device (or T piece in neonates) with a HEPA filter and a tight seal, or, for adults, consider passive oxygenation with a nonrebreathing face mask covered by a surgical mask.
10. If intubation is delayed, consider manual ventilation with a supraglottic airway or bag-mask device with a HEPA filter.
11. Once on a closed circuit, minimize disconnections to reduce aerosolization.
Consider the Appropriateness of Starting and Continuing Resuscitation
Rationale
CPR is a high-intensity team effort that diverts rescuer attention away from other patients.13 In the context of COVID-19, the risk to the clinical team is increased and resources can be profoundly more limited, particularly in regions that are experiencing a high burden of disease. Although the outcomes for cardiac arrest in COVID-19 are still unknown, the mortality for critically ill patients with COVID-19 is high and rises with increasing age and comorbidities, particularly cardiovascular disease.2,5–8 Therefore, it is reasonable to consider age, comorbidities, and severity of illness in determining the appropriateness of resuscitation and to balance the likelihood of success against the risk to rescuers and patients from whom resources are being diverted.14
Strategies
12. Address goals of care with patients with COVID-19 (or proxy) in anticipation of the potential need for increased levels of care.
13. Healthcare systems and EMS agencies should institute policies to guide frontline providers in determining the appropriateness of starting and terminating CPR for patients with COVID-19, taking into account patient risk factors to estimate the likelihood of survival. Risk stratification and policies should be communicated to patients (or proxy) during discussions of goals of care.
14. There are insufficient data to support extracorporeal CPR for patients with COVID-19.
Algorithms with Key Changes
Figures 2 through 6 reflect COVID-19–specific updates to the current basic life support, advanced cardiovascular life support, pediatric basic life support, and pediatric cardiac arrest algorithms and are meant to replace the standard algorithms in patients with suspected or confirmed COVID-19 disease. In COVID-19–negative patients or when COVID-19 is not suspected, cardiac arrest resuscitations should proceed according to the standard algorithms. New boxes specific to COVID-19 are in yellow, and new guidance specific to COVID-19 is bolded and underlined.
Figure 2.
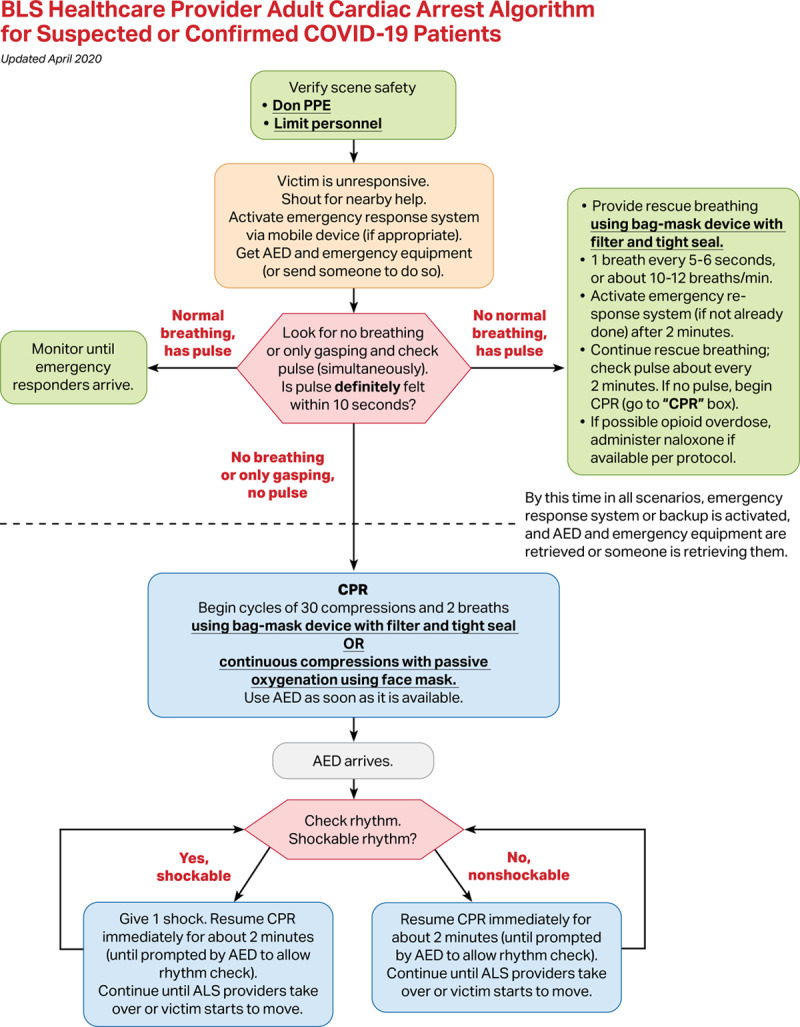
Basic life support healthcare provider adult cardiac arrest algorithm for patients with suspected or confirmed coronavirus disease 2019 (COVID-19). AED indicates automated external defibrillator; ALS, advanced life support; CPR, cardiopulmonary resuscitation; and PPE, personal protective equipment.
Figure 6.
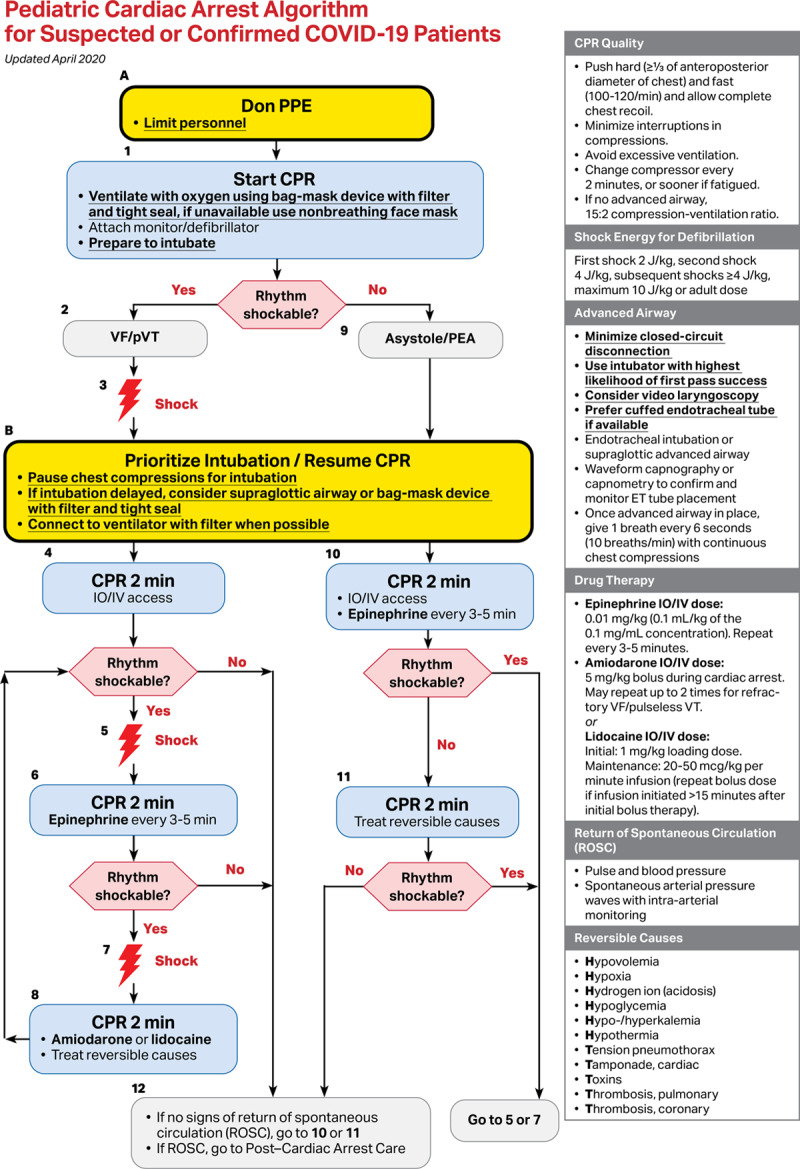
Pediatric cardiac arrest algorithm for patients with suspected or confirmed coronavirus disease 2019 (COVID-19). CPR indicates cardiopulmonary resuscitation; ET, endotracheal; PEA, pulseless electric activity; PPE, personal protective equipment; pVT, pulseless ventricular tachycardia; ROSC, return of spontaneous circulation; and VF, ventricular fibrillation.
Figure 1.
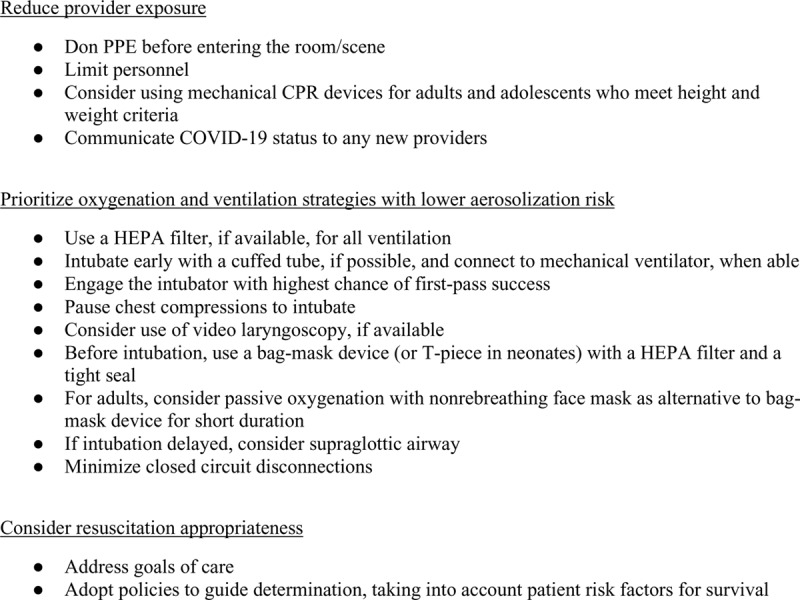
Summary of adjustments to cardiopulmonary resuscitation (CPR) algorithms in patients with suspected or confirmed coronavirus disease 2019 (COVID-19). HEPA indicates high-efficiency particulate air; and PPE, personal protective equipment.
Figure 3.
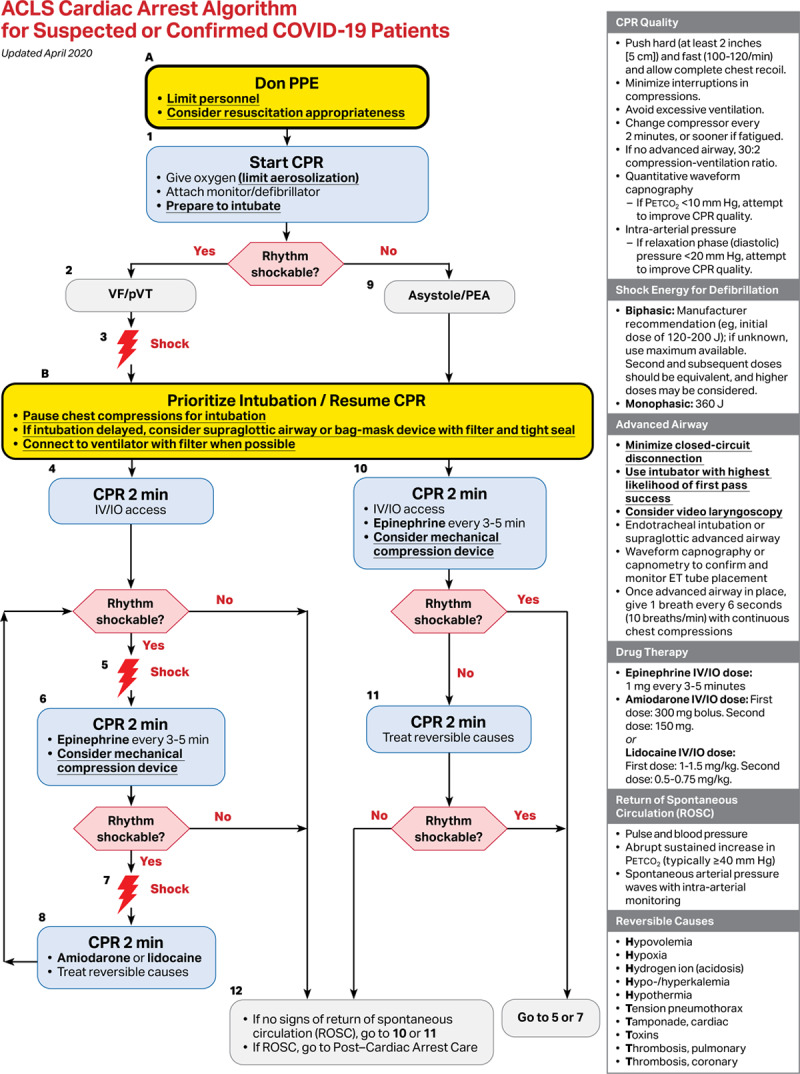
Advanced cardiac life support cardiac arrest algorithm for patients with suspected or confirmed coronavirus disease 2019 (COVID-19). CPR indicates cardiopulmonary resuscitation; ET, endotracheal; PEA, pulseless electric activity; Petco2, end-tidal carbon dioxide; PPE, personal protective equipment; pVT, pulseless ventricular tachycardia; ROSC, return of spontaneous circulation; and VF, ventricular fibrillation.
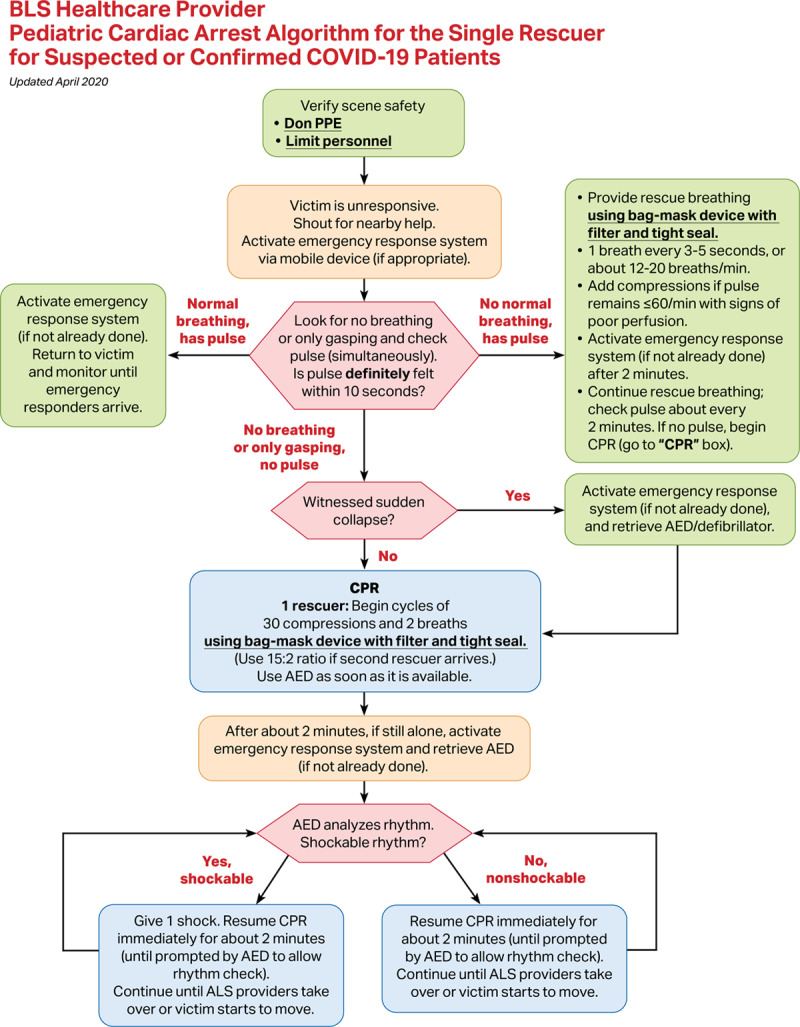
Figure 4.
Basic life support healthcare provider pediatric cardiac arrest algorithm for the single rescuer for patients with suspected or confirmed coronavirus disease 2019 (COVID-19). AED indicates automated external defibrillator; ALS, advanced life support; CPR, cardiopulmonary resuscitation; and PPE, personal protective equipment.
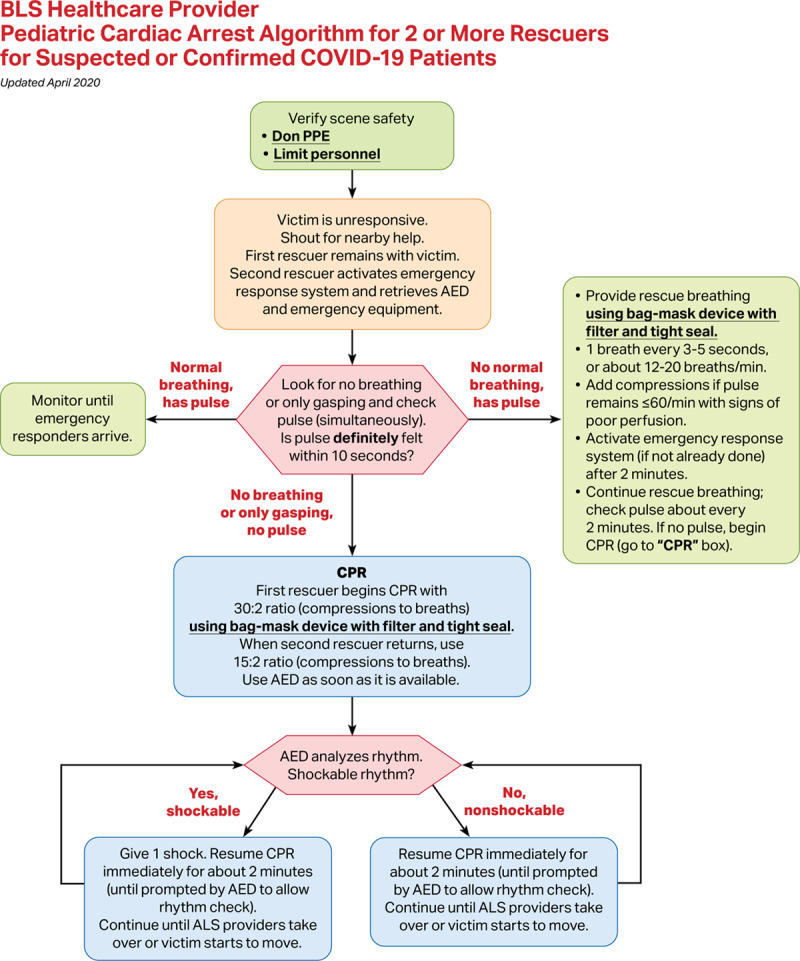
Figure 5.
Basic life support healthcare provider pediatric cardiac arrest algorithm for ≥2 rescuers for patients with suspected or confirmed coronavirus disease 2019 (COVID-19). AED indicates automated external defibrillator; ALS, advanced life support; CPR, cardiopulmonary resuscitation; and PPE, personal protective equipment.
Situation- and Setting-Specific Considerations
Out-of-Hospital Cardiac Arrest
Below are specific considerations for cardiac arrest in individuals with suspected or confirmed COVID-19 occurring outside of the hospital. Depending on local prevalence and evidence of community spread, COVID-19 may be suspected in some out-of-hospital cardiac arrests.
Lay Rescuers
Bystander CPR has consistently been shown to improve the likelihood of survival from out-of-hospital cardiac arrest, which decreases with every minute that CPR and defibrillation are delayed.15–17 Rescuers in the community are unlikely to have access to adequate PPE and therefore may be at increased risk of exposure to COVID-19 during CPR compared with healthcare providers with adequate PPE. Rescuers with increasing age and the presence of comorbid conditions such as heart disease, diabetes mellitus, hypertension, and chronic lung disease4 are at increased risk of becoming critically ill if infected with severe acute respiratory syndrome coronavirus 2. However, when the cardiac arrest occurs at home (as has been reported in 70% of out-of-hospital cardiac arrests17 before the recent widespread shelter-at-home ordinances), lay rescuers are likely to have already been exposed to COVID-19.
Chest Compressions
For adults: Lay rescuers should perform at least hands-only CPR after recognition of a cardiac arrest event, if willing and able, especially if they are household members who have been exposed to the patient at home. A face mask or cloth covering the mouth and nose of the rescuer and/or patient may reduce the risk of transmission to a nonhousehold bystander.
For children: Lay rescuers should perform chest compressions and consider mouth-to-mouth ventilation, if willing and able, given the higher incidence of respiratory arrest in children,17 especially if they are household members who have been exposed to the patient at home. A face mask or cloth covering the mouth and nose of the rescuer and/or patient may reduce the risk of transmission to a nonhousehold bystander if unable or unwilling to perform mouth-to-mouth ventilation.
Public-Access Defibrillation
Because defibrillation is not expected to be a highly aerosolizing procedure, lay rescuers should use an automated external defibrillator, if available, to assess and treat patients with out-of-hospital cardiac arrest.
EMS
Transport
Family members and other contacts of patients with suspected or confirmed COVID-19 should not ride in the transport vehicle.
If return of spontaneous circulation has not been achieved after appropriate resuscitation efforts in the field, consider not transferring to hospital given the low likelihood of survival for the patient,17 balanced against the added risk of additional exposure to prehospital and hospital providers.
In-Hospital Cardiac Arrest
Below are specific considerations for patients with suspected or confirmed COVID-19 in the hospital setting. These interim guidelines do not apply to patients who are known to be COVID-19 negative. Those patients should receive standard basic and advanced life support. However, it may be reasonable to reduce the number of personnel in the room for all resuscitations during the pandemic for social distancing purposes.
Prearrest
Address advanced care directives and goals of care with all patients with suspected or confirmed COVID-19 (or proxy) on hospital arrival and with any significant change in clinical status such as an increase in level of care.
Closely monitor for signs and symptoms of clinical deterioration to minimize the need for emergency intubations that put patients and providers at higher risk.
If the patient is at risk for cardiac arrest, consider proactively moving the patient to a negative-pressure room/unit, if available, to minimize risk of exposure to rescuers during a resuscitation.
Close the door when possible to prevent airborne contamination of adjacent indoor space.
Intubated Patients at the Time of Cardiac Arrest
Consider leaving the patient on a mechanical ventilator with a HEPA filter to maintain a closed circuit and to reduce aerosolization.
-
Adjust the ventilator settings to allow asynchronous ventilation (time chest compressions with ventilation in newborns). Consider the following suggestions:
– Increase the Fio2 to 1.0.
– Use either pressure or volume control ventilation and limit pressure or tidal volume to generate adequate chest rise (4-6 mL/kg ideal body weight is often targeted [6mL/kg for adults]).
– Adjust the trigger to “off” to prevent the ventilator from autotriggering with chest compressions and possibly prevent hyperventilation and air trapping.
– Adjust respiratory rate to 10 breaths/min for adults and pediatrics and 30 breaths/min for neonates.
– Assess the need to adjust the positive end-expiratory pressure level to balance lung volumes and venous return.
– Adjust alarms to deliver full breaths with asynchronous chest compressions.
– Ensure endotracheal tube/tracheostomy and ventilator circuit security to prevent unplanned extubation.
If return of spontaneous circulation is achieved, set ventilator settings as appropriate to patients’ clinical condition.
Prone Patients at the Time of Arrest
For patients with suspected or confirmed COVID-19 who are in a prone position without an advanced airway, attempt to place in the supine position for continued resuscitation.
Although the effectiveness of CPR in the prone position is not completely known, for those patients who are in the prone position with an advanced airway, it may be reasonable to avoid turning the patient to the supine position, unless able to do so without risk of equipment disconnections and aerosolization. If unable to safely transition the patient to a supine position, place the defibrillator pads in the anterior-posterior position and provide CPR with the patient remaining prone with hands in the standard position over the T7/10 vertebral bodies.18
Postarrest Patients
Consult local infection control practices concerning transport after resuscitation.
Maternal and Neonatal Considerations
Neonatal Resuscitation
Every newly born baby should have a skilled attendant prepared to resuscitate regardless of COVID-19 status. Although it remains unclear if newly born babies are infected or likely to be infectious when mothers have suspected or confirmed COVID-19, providers should don appropriate PPE. The mother is a potential source of aerosolization for the neonatal team.
Initial steps: Routine neonatal care and the initial steps of neonatal resuscitation are unlikely to be aerosol generating; they include drying, tactile stimulation, placement into a plastic bag or wrap, assessment of heart rate, and placement of pulse oximetry and electrocardiographic leads.
Suction: Suction of the airway after delivery should not be performed routinely for clear or meconium-stained amniotic fluid. Suctioning is an aerosol-generating procedure and is not indicated for uncomplicated deliveries.
Endotracheal medications: Endotracheal instillation of medications such as surfactant or epinephrine is an aerosol-generating procedure, especially via an uncuffed tube. Intravenous delivery of epinephrine via a low-lying umbilical venous catheter is the preferred route of administration during neonatal resuscitation.
Closed incubators: Closed incubator transfer and care (with appropriate distancing) should be used for neonatal intensive care patients when possible but do not protect against aerosolization of virus.
Maternal Cardiac Arrest
The tenets of maternal cardiac arrest are unchanged for women with suspected or confirmed COVID-19.
The cardiopulmonary physiological changes of pregnancy may increase the risk of acute decompensation in critically ill pregnant patients with COVID-19.
Preparation for perimortem delivery, to occur after 4 minutes of resuscitation, should be initiated early in the resuscitation algorithm to allow the assembly of obstetric and neonatal teams with PPE even if return of spontaneous circulation is achieved and perimortem delivery is not required.
Disclosures
De Edelson reports personal fees from AgileMD; grants and nonfinancial support from EarlySense; and grants, personal fees, and nonfinancial support from Philips Healthcare; in addition, Dr Edelson has a patent to ARCD.P0535US.P2 pending. Dr Chan reports grants from the National Heart, Lung, and Blood Institute and American Heart Association. Dr Aziz reports serving as past chair and member (academic role, without remuneration) of the Alberta coordinating committee for the Neonatal Resuscitation Program and ACoRN that oversees neonatal life support education for perinatal sites in Alberta. Dr Aziz just completed a term as a member of the International Liaison Committee on Resuscitation Neonatal Task Force. Dr Becker reports grants from Philips, National Institutes of Health, Zoll, Patient-Centered Outcomes Research Institute, and United Therapeutics; grants and other from Nihon Kohden; and other from BrainCool. In addition, Dr Becker has a patent for cooling technology issued and a patent fir reperfusion methodology issued. Dr Brooks reports nonfinancial support from Action First Aid and SaveStation; in addition, Dr Brooks has a patent for “A System and Method for an Emergency Communication and Remotely Activated Emergency Assistance Device” pending. Dr Kamath-Rayne reports that the American Heart Association and American Academy of Pediatrics have financial relationships related to the Neonatal Resuscitation Program and Pediatric Advanced Life Support, where these programs are cobranded, and her organizations pay each other royalties based on revenue from these programs. Dr Kamath-Rayne does not personally benefit from these relationships. Dr Mancini reports personal fees from Stryker. Dr Nadkarni reports grants from Zoll Medical Corp, American Heart Association/Resuscitation Quality Improvement Program, Nihon Kohden Corp, National Institutes of Health, and Agency for Healthcare Quality Improvement. Dr Zelop reports personal fees from UptoDate. The other authors report no conflicts.
Appendix
Collaborators: Monique Anderson Starks, MD, MHS, Duke University; Bentley J. Bobrow, MD, University of Texas Health System; Melissa Chan, MD, Stollery Children’s Hospital; Katherine Berg, MD, Beth Israel Deaconess Medical Center; Jonathan P. Duff, MD, MEd, University of Alberta; Benny L. Joyner Jr, MD, MPH, University of North Carolina at Chapel Hill; Javier J. Lasa, MD, Texas Children’s Hospital; Arielle Levy, MD, MEd, University of Montreal; Melissa Mahgoub, PhD, American Heart Association; Michael F. O’Connor, MD, University of Chicago; Amber V. Hoover, RN, MSN, American Heart Association; Amber J. Rodriguez, PhD, American Heart Association; Garth Meckler MD, MSHS, University of British Columbia, BC Children’s Hospital; Kathryn Roberts, MSN, RN, CCRN-K, CCNS; Nicholas M. Mohr, MD, MS, University of Iowa; Boulos Nassar, MD, MPH, University of Iowa; Lewis Rubinson, MD, PhD, Morristown Medical Center; Robert M. Sutton, MD, MSCE, the Children’s Hospital of Philadelphia, University of Pennsylvania; Stephen M. Schexnayder, MD, Arkansas Children’s Hospital; Monica Kleinman, MD, Boston Children’s Hospital; Allan de Caen, MD, Stollery Children’s Hospital, University of Alberta; Ryan Morgan, MD, the Children’s Hospital of Philadelphia, University of Pennsylvania Perelman School of Medicine; Farhan Bhanji, MD, McGill University; Susan Fuchs, MD, Ann & Robert H. Lurie Children’s Hospital; Mark Terry, MPA, National Registry of Emergency Medical Technicians; Mary McBride, MD, MD, MEd, Ann & Robert H Lurie Children’s Hospital of Chicago/Northwestern University; Michael Levy, MD, University of Alaska Anchorage; Jose G. Cabanas, MD, MPH, Wake County Department of Emergency Medical Services, University of North Carolina at Chapel Hill; David K. Tan, MD, EMT-T, Washington University School of Medicine; Vivek K. Moitra, MD, MHA, College of Physicians & Surgeons of Columbia University; Joseph W. Szokol, MD, American Society of Anesthesiologists.
Footnotes
References
- 1.Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, et al. on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–e596. doi: 10.1161/CIR.0000000000000757. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)–United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:343–346. doi: 10.15585/mmwr.mm6912e2. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 4.Guan W-j, Ni Z-y, Hu Y, Liang W-h, Ou C-q, He J-x, Liu L, Shan H, Lei C-l, Hui DSC, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, Greninger AL, Pipavath S, Wurfel MM, Evans L, et al. COVID-19 in critically ill patients in the Seattle region: case series. New Eng J Med. 2020;382:2012–2012. doi: 10.1056/NEJMoa2004500. doi: 10.1056/NEJMoa2004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) [published online March 27, 2020]. JAMA Cardiol. doi: 10.1001/jamacardio.2020.1017. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Information for clinicians on therapeutic options for COVID-19 patients. 2020. Apr 7, https://www.cdc.gov/coronavirus/2019-ncov/hcp/therapeutic-options.html/. Accessed April 8, 2020.
- 10.Gamio L. The workers who face the greatest coronavirus risk. New York Times. 2020 Mar 15; [Google Scholar]
- 11.van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.ECRI. Mechanical ventilation of SARS patients: lessons from the 2003 SARS outbreak. 2020. Feb 18, https://www.ecri.org/components/HDJournal/Pages/Mechanical-Ventilation-of-SARS-Patients-2003-SARS-Outbreak.aspx#. Accessed April 8, 2020.
- 13.Volchenboum SL, Mayampurath A, Göksu-Gürsoy G, Edelson DP, Howell MD, Churpek MM. Association between in-hospital critical illness events and outcomes in patients on the same ward. JAMA. 2016;316:2674–2675. doi: 10.1001/jama.2016.15505. doi: 10.1001/jama.2016.15505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Emanuel EJ, Persad G, Upshur R, Thome B, Parker M, Glickman A, Zhang C, Boyle C, Smith M, Phillips JP. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 15.Kragholm K, Wissenberg M, Mortensen RN, Hansen SM, Malta Hansen C, Thorsteinsson K, Rajan S, Lippert F, Folke F, Gislason G, et al. Bystander efforts and 1-year outcomes in out-of-hospital cardiac arrest. N Engl J Med. 2017;376:1737–1747. doi: 10.1056/NEJMoa1601891. doi: 10.1056/NEJMoa1601891. [DOI] [PubMed] [Google Scholar]
- 16.Pollack RA, Brown SP, Rea T, Aufderheide T, Barbic D, Buick JE, Christenson J, Idris AH, Jasti J, Kampp M, et al. ROC Investigators. Impact of bystander automated external defibrillator use on survival and functional outcomes in shockable observed public cardiac arrests. Circulation. 2018;137:2104–2113. doi: 10.1161/CIRCULATIONAHA.117.030700. doi: 10.1161/CIRCULATIONAHA.117.030700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.CARES: Cardiac Arrest Registry to Enhance Survival. 2018 Annual report. https://mycares.net/sitepages/uploads/2019/2018_flipbook/index.html?page=16. Accessed April 8, 2020. [DOI] [PubMed]
- 18.Mazer SP, Weisfeldt M, Bai D, Cardinale C, Arora R, Ma C, Sciacca RR, Chong D, Rabbani LE. Reverse CPR: a pilot study of CPR in the prone position. Resuscitation. 2003;57:279–285. doi: 10.1016/s0300-9572(03)00037-6. doi: 10.1016/s0300-9572(03)00037-6. [DOI] [PubMed] [Google Scholar]


