Supplemental Digital Content is Available in the Text.
Key Words: hip fracture, COVID-19, coronavirus
Abstract
Objectives:
To examine one health system's response to the essential care of its hip fracture population during the COVID-19 pandemic and report on its effect on patient outcomes.
Design:
Prospective cohort study.
Setting:
Seven musculoskeletal care centers within New York City and Long Island.
Patients/Participants:
One hundred thirty-eight recent and 115 historical hip fracture patients.
Intervention:
Patients with hip fractures occurring between February 1, 2020, and April 15, 2020, or between February 1, 2019, and April 15, 2019, were prospectively enrolled in an orthopaedic trauma registry and chart reviewed for demographic and hospital quality measures. Patients with recent hip fractures were identified as COVID positive (C+), COVID suspected (Cs), or COVID negative (C−).
Main Outcome Measurements:
Hospital quality measures, inpatient complications, and mortality rates.
Results:
Seventeen (12.2%) patients were confirmed C+ by testing, and another 14 (10.1%) were suspected (Cs) of having had the virus but were never tested. The C+ cohort, when compared with Cs and C− cohorts, had an increased mortality rate (35.3% vs. 7.1% vs. 0.9%), increased length of hospital stay, a greater major complication rate, and a greater incidence of ventilator need postoperatively.
Conclusions:
COVID-19 had a devastating effect on the care of patients with hip fracture during the pandemic. Although practice patterns generally remained unchanged, treating physicians need to understand the increased morbidity and mortality in patients with hip fracture complicated by COVID-19.
Level of Evidence:
Prognostic Level III. See Instructions for Authors for a complete description of Levels of Evidence.
INTRODUCTION
Given the reality of today's aging population, hip fractures are a significant concern for our health care system.1 The general principles regarding hip fracture care include careful assessment, prompt medical optimization, and early surgery to provide patients the best chance at recovery while minimizing the incidence of postoperative complications, morbidity, and mortality. In recent years, the population has been aging, and the incidence of hip fractures continues to increase.2–4 Often, older patients have a number of medical comorbidities that place them at increased risk when undergoing repair of hip fractures. Regardless of conditions, there continues to be a steady rate of elderly patients presenting to the emergency department (ED) with a hip fracture.
The emergence of severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2; provisionally named 2019 novel coronavirus or 2019-nCoV disease (COVID-19)] in China at the end of 2019 has caused a large global pandemic and is a major public health issue.5 The virus is spread through droplet transmission and results in a flu-like upper respiratory illness with the symptoms of coughing, fever, and dyspnea in severe cases. The rate of spread throughout the world has been immense, and the lack of therapeutics for this new virus has led to a high mortality rate. In New York City, hospitals and EDs have been overwhelmed with cases.6 Health system resources have been redeployed to manage the crisis. Despite the reallocation of resources, patients with hip fractures have continued to present to the ED and require medical care.7,8
The need for urgent orthopaedic surgical care in the setting of a global or regional epidemic or pandemic has not been studied in detail. The NYU Langone Orthopedic Department is responsible for the musculoskeletal care at 7 different hospitals within the New York City area and services a range of health care delivery systems. Our faculty and residents provide orthopaedic services at 1 tertiary care university hospital (NYU Langone Tisch/Kimmel); an orthopaedic specialty hospital (Langone Orthopedic Hospital); a New York City public hospital (Bellevue Hospital Center); a Veterans' Administration Medical Center (Manhattan VA); 2 safety net and level 1 trauma centers in the boroughs of Queens and Brooklyn (Jamaica Hospital Medical Center and NYU Brooklyn); and a large tertiary care, level 1 center in the suburbs of the city (NYU Winthrop). Each of these centers has restructured their medical operations to tackle the vast number of patients with COVID-19 who presented in the spring of 2020. Despite this fact, the department's orthopaedic trauma service has continued to provide care to all patients presenting with the diagnosis of a hip fracture.
The purpose of this report is to analyze the perioperative complication rate and inpatient hospitalization issues associated with hip fracture patients who presented during the global COVID-19 pandemic. We compared the results with a cohort of similar patients treated during the same seasonal period 1 year ago with respect to management and care of patients who presented to our EDs with a hip fracture.
PATIENTS AND METHODS
This quality improvement IRB-approved study analyzed a consecutive series of patients with hip fracture who presented to the 7 EDs of 1 academic medical center between February 1, 2020, and April 15, 2020. Patients were included if they presented with a hip fracture (femoral neck (OTA/AO 31B), intertrochanteric (OTA/AO 31A), subtrochanteric, and periprosthetic (32(A,B,C).1)) and were treated during their index admission at one of our department's hospital sites (Fig. 1). Hip fracture diagnosis was confirmed on physical examination and with standard radiographs of the affected hip. During the pandemic period, each center had their own methodology and procedures for identifying and confirming COVID-positive patients, which changed over time. Hip fracture treatment was decided by the attending fracture surgeon and followed the general standard of care for patients with hip fracture. Hip fracture surgical care was performed according to standard techniques. Limiting room flow traffic and the use of negative pressure rooms and regional over general anesthetic techniques were implemented as available at each site as the breadth of the pandemic became clear. Personal protective equipment was available for all surgeons in all cases.
FIGURE 1.
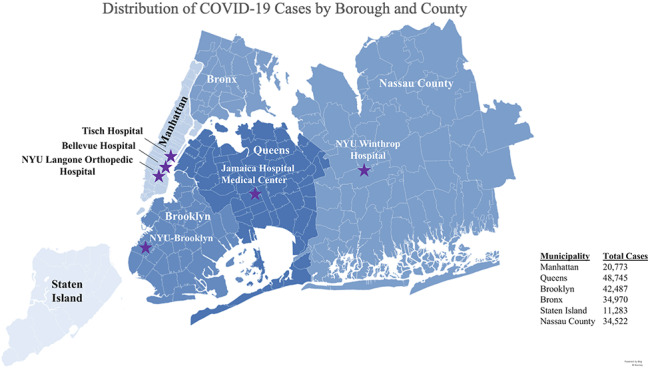
Cases in New York City and surrounding counties with NYU Langone Orthopedic treatment sites.
Patient demographics, mechanism of injury, comorbidities, Charlson Comorbidity Index (CCI), time between presentation and surgery, all laboratory values, oxygen requirements, and delivery methods (O2%, nasal cannula, continuous positive airway pressure, bilevel positive airway pressure, rebreather, and mechanical ventilation) were identified and recorded. We calculated the length of stay, recorded the operative procedure performed, and analyzed inpatient complications.
Patients were identified as COVID positive (C+), COVID suspected (Cs), or COVID negative (C−). Patients were identified as C+ if they had a positive COVID-19 RT-PCR test before, during, or after (at rehabilitation) hospitalization for their hip fracture. Patients were identified as Cs if they presented with symptoms or imaging consistent with COVID-19 infection but had a negative COVID-19 RT-PCR test or if they were not tested, having presented before the implementation of routine testing for symptomatic patients in our health system (March 15, 2020). Other medical comorbidities were analyzed using the CCI. Procedures were divided into nonoperative, closed reduction and internal fixation, open reduction and internal fixation, and arthroplasty procedures. Major complications included acute renal failure, surgical site infection, urinary tract infection, acute anemia, sepsis, pneumonia, deep vein thrombosis/pulmonary embolus (DVT/PE), acute myocardial infarction, stroke, acute postoperative infection, decubitus ulcer, acute respiratory failure, cardiac arrest, and death. In-hospital mortality data were obtained.
A second cohort of patients with hip fracture who presented to our EDs between February 1, 2019, and April 15, 2019 was recruited from another IRB-approved database.9–11 Similar data were obtained minus the laboratory values and oxygen requirements so that comparisons between the cohorts could be made based on the time periods in question. Analysis of descriptive statistics was performed to determine differences between expected and observed frequencies. Chi-square tests of association and independent-samples t tests were used to assess differences between the 2019 and 2020 cohorts and between C+, Cs, and C− cohorts. Factors associated with mortality and major complications were assessed using the bivariate regression Cox analysis. All analyses were completed with SPSS software, version 25.0 (IBM Corporation). All analyses were considered significant for P < 0.05.
RESULTS
2019 Versus 2020 Cohorts
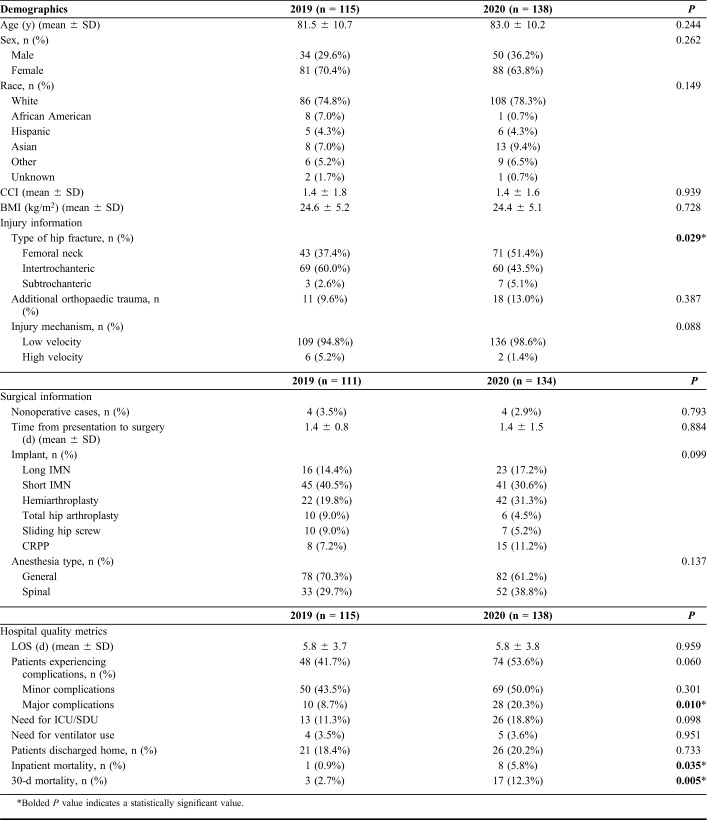
Between February 1, 2020, and April 15, 2020, 138 patients (63.8% women) with a mean age of 82.9 years (±10.1) presented to one of our EDs and were diagnosed with a hip fracture. To assess the pandemic era cohort, we compared them with a second group of 115 patients with hip fracture who presented to the same EDs between February 1, 2019, and April 15, 2019. There were no differences between the groups with regard to demographics (age, sex, and race), body mass index (BMI), CCI, or mechanism of injury. The only difference found was a preponderance of femoral neck fractures in 2020 as compared to 2019 (Table 1). In addition, there were no differences with regard to time to surgery, surgeries performed for each fracture, type of anesthesia, and postoperative ICU/SDU admission. However, the mortality rates (30-day mortality was 12.3% in 2020 vs. 3% in 2019), length of stay, and complication rates observed in the 2020 cohort were significantly greater than those in the 2019 cohort (Table 1).
TABLE 1.
Demographics, Injury Information, and Surgical Data for the 2019 Versus 2020 Cohort
With regard to operative treatment, 133 patients (96.4%) in the 2020 cohort underwent immediate operative treatment (Table 1). There were 5 patients (all C+) who initially did not undergo repair; 2 patients (1.4%) who were too sick to undergo surgery and died; 1 patient (0.7%) with a nondisplaced femoral neck fracture that displaced after 2 weeks and then underwent hemiarthroplasty; and 2 others (1.4%), 1 with a nondisplaced intertrochanteric fracture and 1 with a nondisplaced femoral neck fracture, who were successfully treated without surgery. No patients were treated without surgery in the 2019 cohort.
2020 Cohort: C+ Versus Cs Versus C−
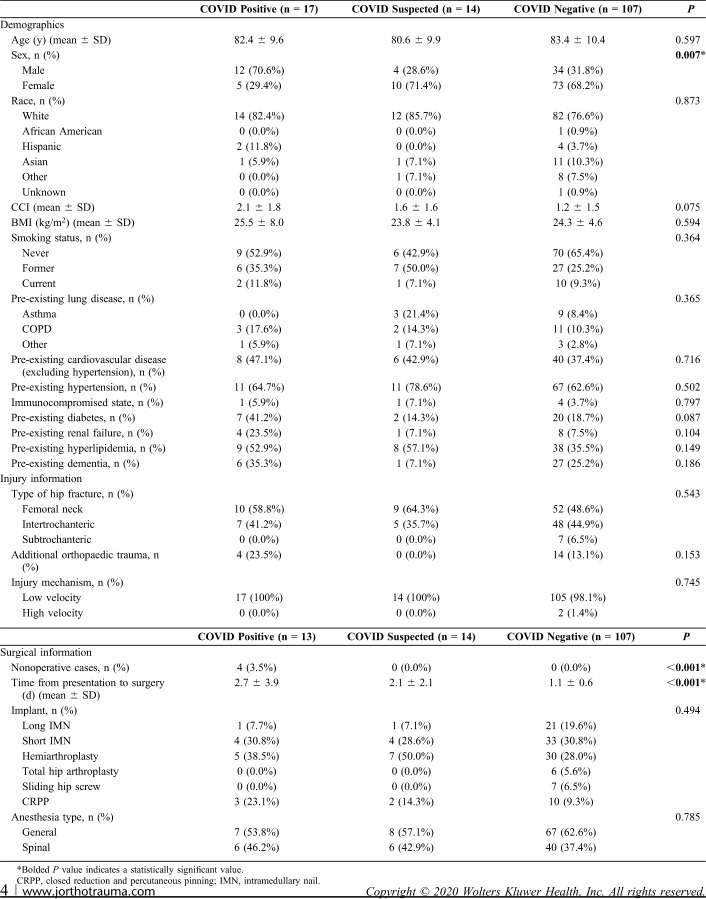
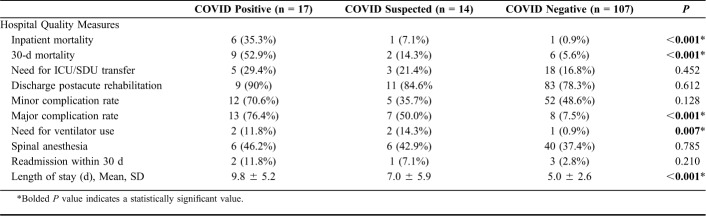
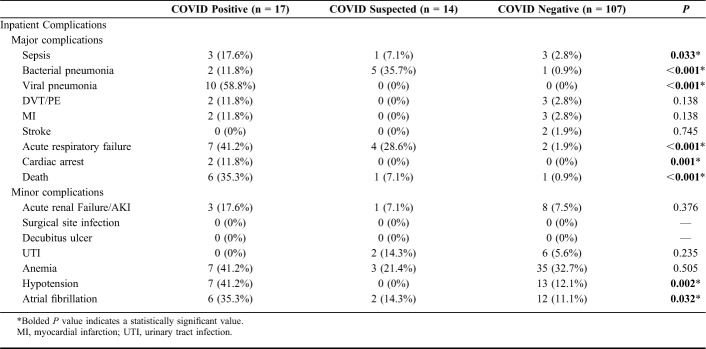
Of 2020 cohort patients, 17 (12.3%) were confirmed C+ by testing and another 14 (10.1%) were suspected (Cs) of having had the virus based on clinical presentation, chest computed tomography findings, or treatment but were never tested or had a negative test at some point. The length of time from presentation to surgery was 1.4 days (± 1.5 days); C+ patients did have a longer time to surgery than C− patients (Table 2). There were no demographic and injury characteristic differences between the C+, Cs, and C− groups (Table 2). When comparing the group of C+ and Cs with the C− hip fracture patients, we found greater in-hospital and 30-day mortality rates, a greater length of hospital stay, a greater major complication rate, and a greater incidence of ventilator need postoperatively (Table 3). In fact, 53% of C+ and 14% of Cs patients died by 30 days compared with 5.6% of C− patients. Complications were seen at a significantly higher rate in those with or suspected of having COVID than those not. The incidence of pneumonia (70.5% vs. 35.7% vs. 0.9%), respiratory failure (41.2% vs. 28.6% vs. 1.9%), sepsis (17.6% vs. 7.1% vs. 2.8%), and death (35.3% vs. 7.1% vs. 0.9%) was significantly elevated in the C+ group compared with the Cs and C− cohorts (Table 4).
TABLE 2.
Demographics, Injury Information, and Surgical Data for the Three Cohorts of 2020 by COVID Status
TABLE 3.
Hospital Quality Measures in Three Cohorts From 2020
TABLE 4.
Inpatient Complications, Minor and Major
In an attempt to assess factors associated with a major complication in the C+/Cs group, we analyzed all laboratory values obtained on admission, postoperative day 1, and postoperative day 2 along with pre-existing medical conditions with those who sustained morbidity and mortality (see Table, Supplemental Digital Content 1, http://links.lww.com/JOT/B89, which describes the pre-existing medical conditions and laboratory values analyzed). Only one factor, postoperative day 1 white blood cell count, was associated with in-hospital major complications (IRR 5.586, CI 95% 1.21–25.786). None of these factors demonstrated an association with mortality; thus, the only predictor of death was C+ and Cs status. Furthermore, when we remove the C+ patients who were confirmed positive after discharge from analyses, the associations still hold (see Table, Supplemental Digital Content 2, http://links.lww.com/JOT/B90, which demonstrates analysis without C+ patients diagnosed after discharge).
DISCUSSION
We found a significantly elevated risk of death after hip fracture in those with confirmed or suspected COVID-19 infection. In addition, these patients treated for a hip fracture during the COVID-19 pandemic were at risk for major postoperative complications compared with those who were C−, the historical control group, and patients with hip fracture in general. Patients treated in each of our institutions were optimized, and the great majority was treated expeditiously when possible. As with most, surgeons in our department continually placed patient care as a top priority. None of the patients' pre-existing conditions or laboratory values during admission were predictive of major complication or death.
Orthopaedic surgeons are front-line health care providers. As first responders, orthopaedic trauma surgeons are called on to provide care for trauma patients and those subject to unanticipated fractures.12 Orthopaedic surgeons who take call do not have the luxury of being able to select their patients or being able to alter the present medical status of a patient in need of their care. In addition, they are susceptible to the contraction of contagious diseases. The risks to surgeons for blood-borne disease transmission are well known. Hepatitis and HIV transmission has always been of concern to orthopaedic surgeons involved in open, blood loss surgeries; however, the route of transmission of airborne or droplet-borne viruses poses considerable concern as well. Improperly protected surgeons are at risk for COVID transmission. Over a 1-month period, 26 orthopaedic surgeons tested positive for COVID-19 at 8 different hospitals in Wuhan, China. Eighty percent of exposures were felt to be on the wards and only 12.5% due to OR exposure, however.13
Because the COVID-19 pandemic has led to a global surge in critically ill patients, hospitals were forced to reallocate resources, potentially resulting in reduced health care access for patients requiring essential care.14 Untreated hip fractures are associated with a high mortality rate, and even slight delays (>72 hours) to operative fixation have been shown to increase morbidity and mortality. Therefore, patients presenting with fractures of the hip require timely surgical intervention regardless of their COVID status. Our cohort did not experience a delay to surgery when compared with accepted standards. However, the C+ group was delayed to surgery compared with the C− patients by 1 day. Whether this small delay to optimize these patients is the cause of the increased rates of postoperative mortality is unknown. It is generally accepted that the mortality rate after hip fractures is 9%–10% at 30 days and 25%–30% at 1 year.15–17 The exceedingly high mortality rate in the C+ patients warrants further investigation into ways to mitigate negative outcomes in this specific patient population. Male sex, older age, and higher CCI have all been associated with increased mortality after geriatric hip fracture.18–20 So, it was not surprising that our mortality rate was also male dominant. This may be related to the predominance of males affected by COVID-19.
In this cohort of patients, C+ and Cs patients experienced a greater overall major complication rate, including an increase in complications such as sepsis, pneumonia, acute respiratory failure, cardiac arrest, and inpatient mortality. They additionally experienced the minor complications of hypotension and atrial fibrillation at a greater rate than C− patients, but the overall minor complication rate was comparable between groups (Tables 3 & 4). The increased frequency and types of perioperative complications observed in this cohort mirrors reports from other specialties.21,22 Lei et al describe a cohort of postoperatively diagnosed COVID-19 positive that underwent both orthopaedic and nonorthopaedic surgeries of various risk categories (low, mild, moderate, and high risk). All of these patients developed COVID-19–related pneumonia and experienced a 20.5% inpatient mortality rate. This mortality rate is lower than that described in our cohort, although patients underwent a variety of orthopaedic and nonorthopaedic procedures of varying risk, unlike our group who were all patients with hip fracture. Aminian et al report on 4 patients who underwent general and obstetric surgery (1 cholecystectomy, 1 hernia repair, 1 gastric bypass, and 1 hysterectomy) during the COVID-19 pandemic and developed perioperative complications; all 4 patients developed pulmonary compromise, which resulted in 3 deaths. While one can question why a hernia repair and gastric bypass were performed on patients with COVID-19, these previous reports enlightened us to the fact that perioperative patients are at heightened risk for complications due to COVID-19. A currently developing explanation for the damage caused by COVID-19 infection is a dysfunctional immune response accompanied by pulmonary and systemic inflammation.23,24 This, compounded with the secondary insult of anesthetic use and operative intervention, may have primed these patients for the pulmonary, vascular, and cardiac complications observed in this cohort.
The disease caused by the novel coronavirus (SARS-CoV-2) results in acute respiratory failure accompanied by a severe hypercoagulability rather than consumptive coagulopathy. This hypercoagulability poses challenges for the postoperative hip fracture patients. DVT and venous thromboembolism are common in patients with hip fracture, and recent treatment algorithms have been instituted to both limit blood loss while preventing thrombotic events.25 One alteration of practice has been the discontinuation of tranexamic acid during arthroplasty in patients during the pandemic. In our current study, we observed no difference in the rate of venous thromboembolism in the C+ cohort compared with C− and historical controls. This could be due to the fact that all patients with hip fracture receive chemical prophylaxis that continues throughout hospitalization and for at least 1 month after injury, as opposed to the general population of patients presenting to the hospital.
Limitations of this study include its retrospective design. Despite this, we have had a very active prospective trauma registry to capture all data prospectively. The data set is robust, but it is possible that some data are incomplete or missing. There were at least 12 different treating surgeons involved in the care of these patients. Patients were not treated as part of any protocol but rather individualized care provided, based on the clinical situation on the ground and the best care practices as decided by each surgeon. Guidelines and recommendations changed quickly as time went on over the 10 weeks studied. Although use of a Cs group of patients may be a limitation because we cannot definitively comment on their COVID-19 status, our purpose was to present the reader with all available data and allow them to make conclusions. Because the outcomes in the C+ group stand alone, we feel confident in reporting in this manner. Finally, long-term outcomes are not available at this time. It is possible that our mortality and major complication rate will continue to increase or that the numbers could change if C− patients converted to C+ postoperatively and were missed, thus lessening the differences between the 2 cohorts.
In conclusion, geriatric hip fractures continued to present to EDs throughout the COVID-19 pandemic period in New York City. Despite the incredible resource reallocation experienced by our hospital system, our treating orthopaedic surgeons continued to care for the elderly in need of essential surgery. Although there was some alteration in treatment algorithms, most patients were treated expeditiously and with great care. Despite this, we experienced an exorbitant rate of early mortality and major complications related to the pulmonary consequences of the virus in this population of patients. Physicians treating these COVID+ patients should counsel families of the significantly increased risks after hip fracture.
Footnotes
All authors declare that they have no conflicts of interest related to the content of this manuscript. Authorship has been granted only to those individuals who have contributed substantially to the research or manuscript. No sources of funding have been granted for this study.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jorthotrauma.com).
REFERENCES
- 1.Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018;49:1458–1460. [DOI] [PubMed] [Google Scholar]
- 2.Brauer CA, Coca-Perraillon M, Cutler DM, et al. Incidence and mortality of hip fractures in the United States. Jama. 2009;302:1573–1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–1767. [DOI] [PubMed] [Google Scholar]
- 4.Turesson E, Ivarsson K, Thorngren KG, et al. Hip fractures—treatment and functional outcome. The development over 25 years. Injury. 2018;49:2209–2215. [DOI] [PubMed] [Google Scholar]
- 5.Coronavirus Disease (COVID-19) Pandemic: World Health Organization; 2020. [Google Scholar]
- 6.Goyal P, Choi JJ, Pinheiro LC, et al. Clinical characteristics of covid-19 in New York city. N Engl J Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DePhillipo NN, Larson CM, O'Neill OR, et al. Guidelines for ambulatory surgery centers for the care of surgically necessary/time-sensitive orthopaedic cases during the COVID-19 pandemic. J Bone Joint Surg Am. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Awad ME, Rumley JCL, Vazquez JA, et al. Peri-operative considerations in urgent surgical care of suspected and confirmed COVID-19 orthopedic patients: operating rooms protocols and recommendations in the current COVID-19 pandemic. J Am Acad Orthop Surg. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Konda SR, Saleh H, Lott A, et al. Predicting discharge location among low-energy hip fracture patients using the score for trauma triage in the geriatric and middle-aged (STTGMA). Adv Orthop 2018;2018:9793435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Konda SR, Lott A, Egol KA. Development of a value-based algorithm for inpatient triage of elderly hip fracture patients. The J Am Acad Orthop Surg. 2019. doi: 10.5435/JAAOS-D-5418-00400. [DOI] [PubMed] [Google Scholar]
- 11.Konda SR, Lott A, Egol KA. The coming hip and femur fracture bundle: a new inpatient risk stratification tool for care providers. Geriatr Orthop Surg Rehabil. 2018;9:2151459318795311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moroz PJ, Spiegel DA. The World Health Organization's action plan on the road traffic injury pandemic: is there any action for orthopaedic trauma surgeons? J Orthop Trauma. 2014;28(suppl 1):S11–S14. [DOI] [PubMed] [Google Scholar]
- 13.Guo X, Wang J, Hu D, et al. Survey of COVID-19 disease among orthopaedic surgeons in Wuhan, People's Republic of China. J Bone Joint Surg Am. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Baker T, Schell CO, Petersen DB, et al. Essential care of critical illness must not be forgotten in the COVID-19 pandemic. Lancet. 2020;395:1253–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abrahamsen B, van Staa T, Ariely R, et al. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009;20:1633–1650. [DOI] [PubMed] [Google Scholar]
- 16.Guzon-Illescas O, Perez Fernandez E, Crespi Villarias N, et al. Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res. 2019;14:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mattisson L, Bojan A, Enocson A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: data from the Swedish fracture register. BMC Musculoskelet Disord. 2018;19:369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yong EL, Ganesan G, Kramer MS, et al. Risk factors and trends associated with mortality among adults with hip fracture in Singapore. JAMA Netw Open 2020;3:e1919706. [DOI] [PubMed] [Google Scholar]
- 19.Gundel O, Thygesen LC, Gögenur I, et al. Postoperative mortality after a hip fracture over a 15-year period in Denmark: a national register study. Acta Orthop. 2020;91:58–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schulz C, König HH, Rapp K, et al. Analysis of mortality after hip fracture on patient, hospital, and regional level in Germany. Osteoporos Int. 2020;31:897–904. [DOI] [PubMed] [Google Scholar]
- 21.Aminian A, Safari S, Razeghian-Jahromi A, et al. COVID-19 outbreak and surgical practice: unexpected fatality in perioperative period. Ann Surg. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020:100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tay MZ, Poh CM, Renia L, et al. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang W, Zhao Y, Zhang F, et al. The use of anti-inflammatory drugs in the treatment of people with severe coronavirus disease 2019 (COVID-19): the Perspectives of clinical immunologists from China. Clin Immunol. 2020;214:108393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Watts CD, Houdek MT, Sems SA, et al. Tranexamic acid safely reduced blood loss in hemi- and total hip arthroplasty for acute femoral neck fracture: a randomized clinical trial. J Orthop Trauma. 2017;31:345–351. [DOI] [PubMed] [Google Scholar]