Supplemental Digital Content is Available in the Text.
Key Words: COVID-19, SARS-CoV-2, hip fracture, New York
Abstract
Objective:
To evaluate inpatient outcomes among patients with hip fracture treated during the COVID-19 pandemic in New York City.
Design:
Multicenter retrospective cohort study.
Setting:
One Level 1 trauma center and one orthopaedic specialty hospital in New York City.
Patients/Participants:
Fifty-nine consecutive patients (average age 85 years, range: 65–100 years) treated for a hip fracture (OTA/AO 31, 32.1) over a 5-week period, March 20, 2020, to April 24, 2020, during the height of the COVID-19 crisis.
Main Outcome Measurements:
COVID-19 infection status was used to stratify patients. The primary outcome was inpatient mortality. Secondary outcomes were admission to the intensive care unit, unexpected intubation, pneumonia, deep vein thrombosis, pulmonary embolus, myocardial infarction, cerebrovascular accident, urinary tract infection, and transfusion. Baseline demographics, comorbidities, treatment characteristics, and COVID-related symptomatology were also evaluated.
Results:
Ten patients (15%) tested positive for COVID-19 (COVID+) (n = 9; 7 preoperatively and 2 postoperatively) or were presumed positive (n = 1), 40 (68%) patients tested negative, and 9 (15%) patients were not tested in the primary hospitalization. American Society of Anesthesiologists' scores were higher in the COVID+ group (d = −0.83; P = 0.04); however, the Charlson Comorbidity Index was similar between the study groups (d = −0.17; P = 0.63). Inpatient mortality was significantly increased in the COVID+ cohort (56% vs. 4%; odds ratio 30.0, 95% confidence interval 4.3–207; P = 0.001). Including the one presumed positive case in the COVID+ cohort increased this difference (60% vs. 2%; odds ratio 72.0, 95% confidence interval 7.9–754; P < 0.001).
Conclusions:
Hip fracture patients with concomitant COVID-19 infection had worse American Society of Anesthesiologists' scores but similar baseline comorbidities with significantly higher rates of inpatient mortality compared with those without concomitant COVID-19 infection.
Level of Evidence:
Prognostic Level III. See Instructions for Authors for a complete description of levels of evidence.
INTRODUCTION
Coronavirus disease 2019 (COVID-19), which is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) viral strain, spread rapidly in New York City starting in March of 2020. COVID-19 put unprecedented pressure on the health care system of New York because hospitals diverted substantial human and physical resources to meet rising critical care demands. In particular, many resources normally used to provide orthopaedic care were repurposed, including anesthesia providers, operative and nursing staff, operating rooms, and postanesthesia care units. These reallocations limited the capacity of many hospitals to continue providing urgent orthopaedic care. Therefore, nonessential orthopaedic care was deferred, and essential care required new pathways established to transfer patients with essential urgent orthopaedic conditions to specific centers that were equipped to continue providing orthopaedic care during the pandemic.
Elderly patients with hip fractures were considered to have essential orthopaedic needs and represented a particularly challenging patient population in this context. Patients with hip fractures typically have a high comorbidity burden, thereby increasing their risk of morbidity and mortality due to COVID-19.1,2 Furthermore, patients with hip fractures are at increased risk of developing nosocomial pulmonary infection because of the need for hospitalization and limited ambulatory capacity.3,4 Several unique considerations arose in the context of caring for patients with hip fracture in New York City during the pandemic. These included regular transfer of patients between hospitals, minimizing the risk of SARS-CoV-2 exposure in patients who did not present with COVID-19 infection, stabilizing patients preoperatively who were acutely ill due to COVID-19, and intervening promptly to minimize mortality and potentially improve the respiratory capacity of affected patients.
Two recent studies from China5 and Italy6 described the clinical characteristics of fracture patients with COVID-19 infection. These studies highlighted the high comorbidity burden and poor prognosis of this group. However, these studies were descriptive case series that did not compare patients with COVID-19 to those without COVID-19. A more recent study from Spain found a mortality rate of 30.4% in patients with hip fractures who tested positive for SARS-CoV-2 compared with 5.3% in those testing negative or not tested.7 In light of these recent studies, the purpose of this study was to provide further assessment of hip fracture outcomes during the COVID-19 pandemic in the United States, with a focus on identifying differences in mortality and complications among COVID-positive (COVID+) patients relative to those who were not COVID-positive.
PATIENTS AND METHODS
Study Design and Setting
A multicenter retrospective cohort study was conducted to evaluate outcomes in patients older than 65 years of age with hip fractures (OTA/AO 31, 32.1) treated during the COVID-19 pandemic. A descriptive case series was also performed to evaluate trends in the inflammatory response among patients with hip fracture during the perioperative phase of care. Findings were reported in accordance with the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) checklist for retrospective cohort studies.8
All patients with hip fractures (OTA/AO 31, 32.1) admitted to 1 of 2 hospitals in New York City over a 5-week period from March 20, 2020, to April 25, 2020, were identified retrospectively. March 20, 2020, was chosen as the start date because this was the first date an orthopaedic patient was tested for SARS-CoV-2 at one of the hospitals. One of the hospitals is a Level 1 trauma center, and one of the hospitals is an orthopaedic specialty hospital without an emergency department. In the setting of the pandemic, the Level I trauma center became overburdened with the management of patients with COVID-19, as their operating rooms were largely converted to intensive care units (ICUs) and their anesthesia providers and operative staff were diverted to critical care roles. In this context, the roles of the 2 hospitals changed substantially with regard to managing acute orthopaedic trauma, with operative injuries being routinely transferred from the emergency department at the trauma center (as well as other hospitals throughout New York) directly to the orthopaedic specialty hospital, which was equipped to provide essential orthopaedic care during the pandemic. Therefore, patients presenting with hip fractures to both hospitals were included in this study.
Excluded from the study were patients with high-energy trauma, periprosthetic fracture, pathologic fracture, age less than 65 years, or revision surgery for prior hip fracture.
Patients were stratified into COVID+ and non-COVID cohorts based on SARS-CoV-2 testing status (positive, negative, or not tested). Patients in the COVID+ and non-COVID groups were compared in the primary analysis. Patients who tested negative for SARS-CoV-2 but were “presumptive positive” as documented by hospitalist evaluation were incorporated into a secondary analysis, which included “presumptive positive” patients in the COVID+ group. This was performed to account for the limited sensitivity of the real-time reverse transcriptase polymerase chain reaction (rRT-PCR) test for SARS-CoV-2 virus in patients with a high pretest probability of COVID infection.9
Outcomes
The primary outcome was inpatient mortality. Secondary outcomes were complications and unexpected pulmonary conditions and included documented neurovascular injury, hematoma, superficial or deep infection, wound dehiscence, deep vein thrombosis, pulmonary embolus, pneumonia from any cause, cerebral vascular accident, myocardial infarction, cardiac arrhythmia, urinary tract infection, blood transfusion, decubitus ulcer, admission to the ICU, and respiratory distress requiring intubation.
Covariates
Demographic, clinical, and functional variables were extracted from the electronic medical record, including age at presentation, sex, body mass index, baseline domicile, ambulatory status, comorbidities, smoking status, American Society of Anesthesiologists (ASA) score,10 and the calculated Charlson Comorbidity Index.11 Variables related to the timing of care were also collected, including presentation delay (number of days from injury to the first presentation to any hospital), treatment delay (number of hours from the first presentation to any hospital to the time of surgery), and whether the patient required a transfer from a hospital or outpatient/urgent care center. Variables related to the injury and surgery were collected, including fracture type, mechanism of injury, laterality, fixation method, surgical duration, and anesthesia type. Postoperative ambulation, length of stay, and discharge disposition were also assessed.
For all patients, COVID-related data points were collected, including SARS-CoV-2 testing status, preoperative and postoperative COVID-related symptomatology, laboratory test results, and imaging results. COVID-related symptoms included new-onset cough, dyspnea, anosmia, fever (>38°C), and new oxygen requirement. Preoperative and postoperative laboratory test results were also compared between COVID-positive and non-COVID groups.
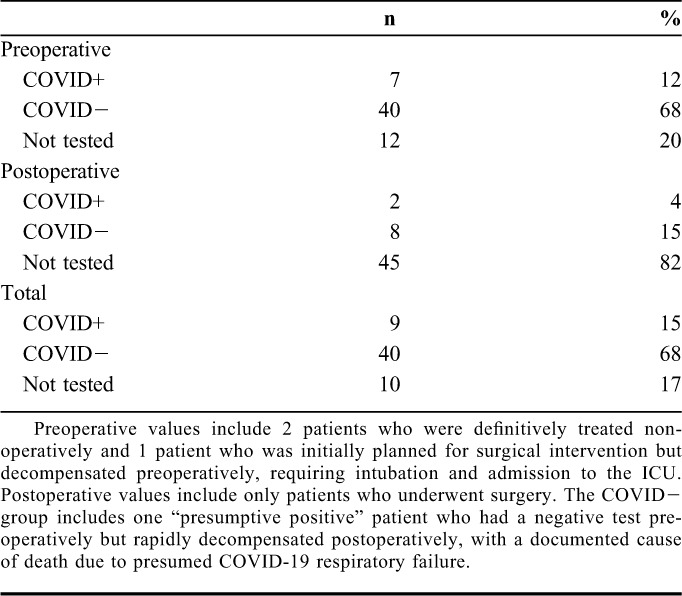
Patient Characteristics
Sixty-three patients with proximal femur fractures were initially screened, yielding 59 patients for inclusion in the study sample. Patients were excluded for the following reasons: periprosthetic fracture (n = 3) and revision surgery for prior hip fracture (n = 1). Nine of the 59 (15%) patients had a positive result on SARS-CoV-2 nasopharyngeal rRT-PCR. In most COVID+ patients, their status was known preoperatively (7 of 9, 78%). Forty patients tested negative and 16 were not tested. Details of the timing, preoperative or postoperative, are presented in Table 1. Of 40 patients who tested negative preoperatively, 7 underwent a second test postoperatively and 1 tested positive. This patient was considered positive for all analyses. Therefore, 9 patients were considered in the COVID+ group and 50 patients were considered in the non-COVID group for the primary analysis. One patient who tested negative postoperatively was considered in a secondary analysis as “presumptive positive” because of documentation in the electronic medical record of COVID-related death, despite a negative test earlier in his/her hospitalization.
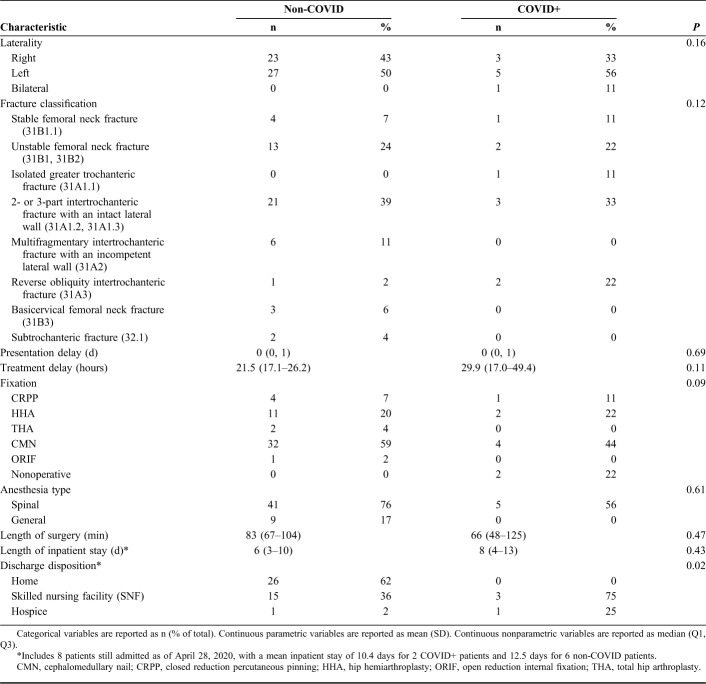
TABLE 1.
SARS-CoV-2 Nasopharyngeal RT-PCR Testing Results Among the Study Sample
Statistical Analysis
Patient characteristics between the 2 cohorts were compared using the Fisher exact test for categorical variables and the t test and Cohen's d or the Wilcoxon rank-sum test for continuous parametric or nonparametric variables, respectively. Normality was assessed with the Shapiro–Wilks test. Inpatient mortality and complications were analyzed through univariate logistic regression. Data are presented as mean (SD) if they are normally distributed, as median (first quartile, third quartile) if they are not normally distributed, and as a count (percentage) if they are categorical. Given that all covariates and outcomes assessed were documented as the standard of care in the electronic medical record, there were minimal missing data (<5%) for all demographic and clinical characteristics. Patients missing laboratory values were excluded from the analysis of the laboratory data. A 2-sided P value of <0.05 was used. R statistical software (Vienna, Austria) was used for statistical analysis.
Ethical Approval
The study was approved by the institutional review boards of both hospitals under study.
RESULTS
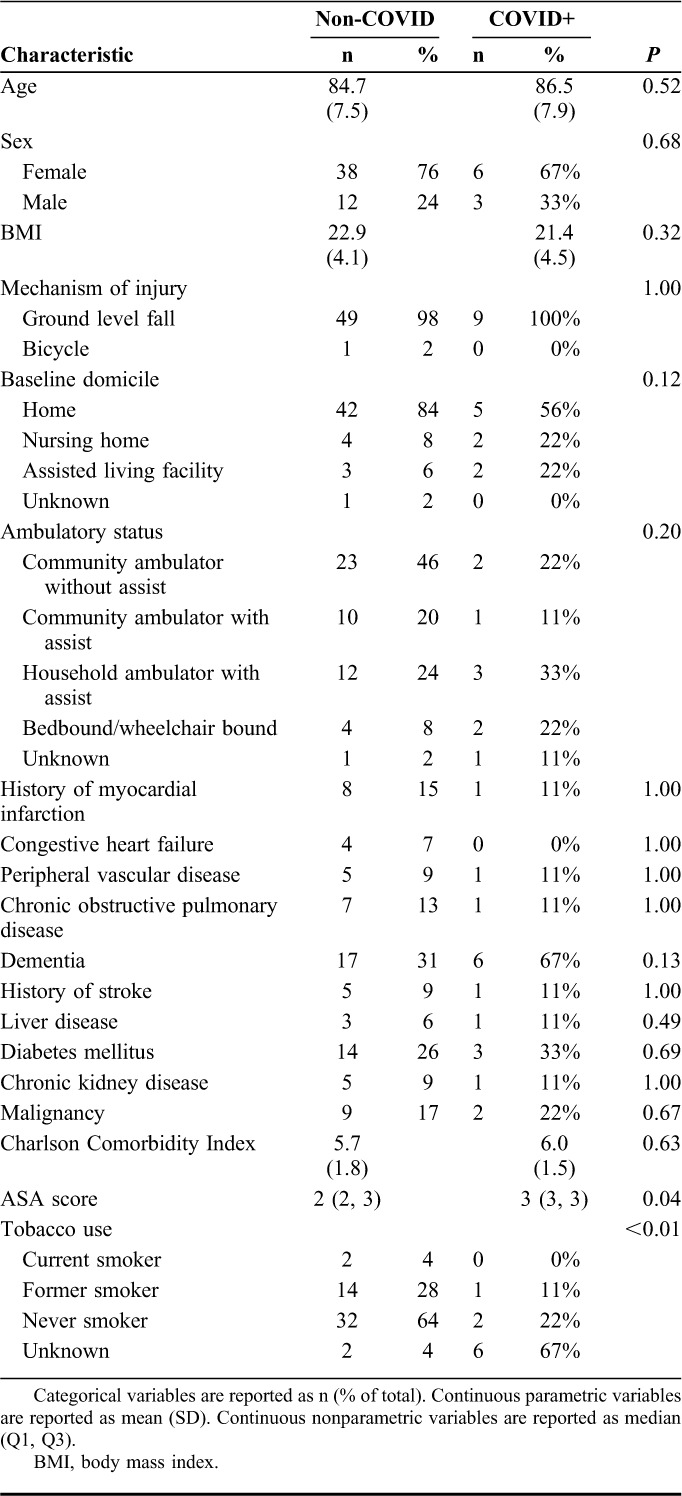
Comparison of Demographics and Fractures
Baseline demographic characteristics were similar between the study groups (Table 2). The majority of patients were women (n = 44; 75%), and the mean age was 85 years (range 65–100 years). ASA scores were worse in the COVID+ group (d = −0.83; P = 0.04); however, the Charlson Comorbidity Index was similar between the study groups (d = −0.17; P = 0.71).
TABLE 2.
Clinical and Demographic Characteristics of the Study Sample
Fracture and treatment characteristics were similar between the study groups (Table 3). The most common fracture type was a 2- or 3-part intertrochanteric fracture with an intact lateral wall (31A1.2 and 31A1.3) (n = 24; 41%). The most common surgical procedure was placement of a cephalomedullary nail (n = 36; 61%).
TABLE 3.
Fracture and Treatment Characteristics of the Study Sample
COVID-Related Presentation
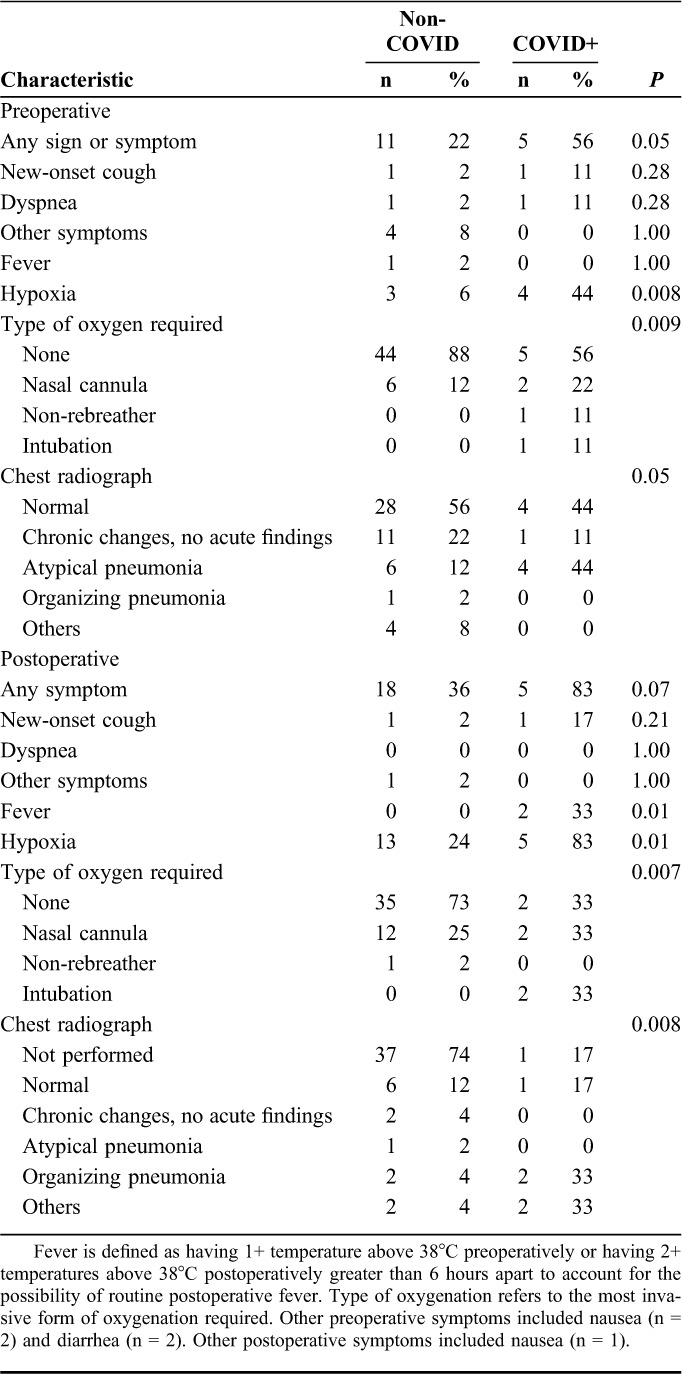
COVID+ patients were more likely to present with preoperative hypoxia requiring supplemental oxygen (44% vs. 6%; P = 0.008) (Table 4). Radiographic evidence of atypical pneumonia (eg, bilateral interstitial infiltrates) on presentation was seen in 4 (44%) of the COVID-positive patients, 1 of whom was asymptomatic. In addition, radiographic evidence of atypical pneumonia was seen in 4 asymptomatic individuals who tested negative and 2 asymptomatic individuals who were not tested.12
TABLE 4.
Preoperative and Postoperative Signs, Symptoms, and Imaging Results
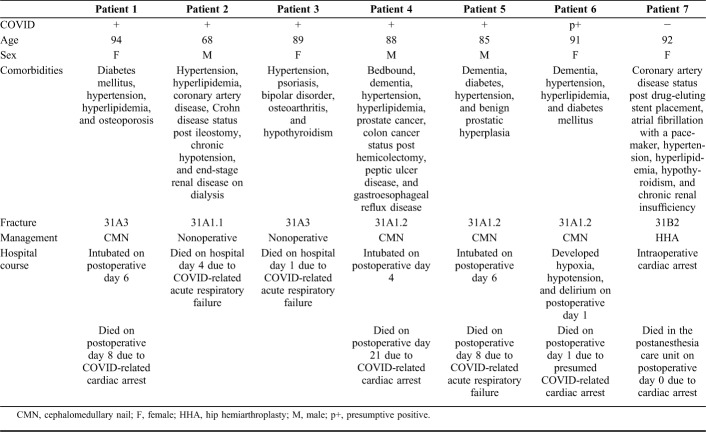
Mortality
Overall, inpatient mortality was 11.9%. Five of the 9 tested COVID+ patients died, all of COVID-related disease. Four of the 5 were 85 years of age or older, and all had multiple comorbid diseases known to affect survival in COVID-positive patients (Table 5). Two of the 5 died before operative intervention because of respiratory failure and were not intubated. Both patients had existing Do Not Resuscitate/Do Not Intubate orders. The 3 other deaths in the COVID+ group occurred between postoperative days 8 and 21. All 3 of these patients were intubated for COVID-related lung disease between postoperative days 4 and 6 and ultimately died (Table 5). The one presumed positive patient was 91 years old with dementia, hypertension, hyperlipidemia, and diabetes mellitus, became acutely hypotensive on postoperative day 1, and went into asystole later that day. Of the 4 surviving COVID+ patients, 2 were discharged on postoperative days 6 and 8 and 2 remained admitted. A comparison of baseline comorbidities between COVID+ patients who were alive versus died is provided in Supplemental Digital Content 1 (see Table, http://links.lww.com/JOT/B93).
TABLE 5.
Summary of Patients Who Died
One COVID-negative patient (not presumed positive), age 92 years, with comorbidities including coronary artery disease status post drug-eluting stent placement, atrial fibrillation with a pacemaker, hypertension, hyperlipidemia, hypothyroidism, and chronic renal insufficiency had a cardiac arrest intraoperatively during hip hemiarthroplasty treatment for his/her unstable femoral neck fracture under general anesthesia and died in the postanesthesia care unit.
Inpatient mortality was significantly increased among COVID+ patients (56% vs. 4%; odds ratio 30.0, 95% confidence interval 4.3–206.9; P = 0.001). This difference in mortality was accentuated by including the one “presumptive positive” patient in the COVID+ group (60% vs. 2%, odds ratio 72.0, 95% confidence interval 7.9–754; P < 0.001).
COVID-Related Complications
Postoperative hypoxia occurred in 18 patients and was more common in the COVID+ group (83% vs. 26%; P = 0.011). Three of 9 (33%) COVID+ patients required intubation and admission to the ICU on postoperative day 4 (n = 1) and postoperative day 6 (n = 2), and all 3 died (see Table, Supplemental Digital Content 2, http://links.lww.com/JOT/B94). Of the 4 surviving COVID+ patients, 3 had postoperative hypoxia that resolved during their admission, none were intubated, and none required ICU admission. By contrast, no patients in the non-COVID cohort required intubation and 1 patient required admission to the ICU for acute-on-chronic heart failure on postoperative day 1. COVID+ patients were more likely to be treated for pneumonia (67% vs. 10%, P = 0.001). There were no differences noted between the 2 groups in terms of deep vein thrombosis, myocardial infarction, arrhythmia, urinary tract infection, decubitus ulcer formation, and transfusion. No patients were found to have neurovascular injury, hematoma, superficial or deep infection, wound dehiscence, pulmonary embolus, or cerebrovascular accident. No patients were treated with COVID-19–specific modalities, including remdesivir, hydroxychloroquine, steroids, proning, or convalescent plasma.
Laboratory Analysis
Laboratory analysis (see Tables, Supplemental Digital Contents 3 and 4, http://links.lww.com/JOT/B95 and http://links.lww.com/JOT/B96) revealed changes in several values between specimens drawn on admission compared with those drawn on postoperative day 2. Preoperatively, COVID+ patients had lower absolute eosinophil (d = −0.66; P < 0.01) and basophil counts (d = −0.55; P = 0.02) compared with the non-COVID patients. Postoperatively, the COVID+ patients had a lower absolute monocyte count than the non-COVID patients (d = −1.05; P = 0.01), despite being similar preoperatively (P = 0.35).
DISCUSSION
This study raises several important concerns regarding hip fracture patients with concomitant COVID-19. First, despite having similar comorbidity profiles, COVID+ hip fracture patients were at a much greater risk of inpatient mortality than those without COVID-19. This difference was further emphasized after accounting for a “presumptive positive” patient whose death was attributed to sequelae of suspected COVID-19. It is important to note that although 5 of 9 COVID+ patients died, 4 of 9 only had mild postoperative hypoxia requiring supplemental oxygen through nasal cannula, which resolved during their admission. In addition, our study highlights characteristic presenting signs and symptoms of hip fracture patients with concomitant COVID-19, including hypoxia and bilateral interstitial infiltrates on chest radiography.
Our finding of elevated inpatient mortality among COVID+ hip fracture patients is consistent with the results from China and Italy, which demonstrated early mortality rates among fracture patients of 40% and 44%, respectively.5,6 Importantly, the former study included 10 patients in total, 6 of whom had hip fractures (50% died) and 6 of whom had RT-PCR evidence of confirmed COVID-19 infection, with the rest diagnosed by findings on CT scan consistent with possible COVID infection. Furthermore, our results corroborate recent data from Europe comparing patients who tested positive for COVID-19 with those testing negative or not tested.7 These data demonstrated a 30.3% 14-day mortality rate among COVID+ hip fracture patients compared with 10.3% among those who tested negative and 2.7% among those not tested.
Screening patients is important in ensuring that health care workers and patients are appropriately protected before, during, and after surgery.13 Published SARS-CoV-2 RT-PCR test metrics demonstrate a limited sensitivity of 32%–72%, suggesting a high false-negative risk.9 Furthermore, our study showed that patients who initially had negative RT-PCR tests for COVID infection later tested positive or developed severe symptoms in the acute postoperative period. Given these findings, care should be taken to protect the health care workforce and observe “COVID precautions” perioperatively for any patient with a high likelihood of infection regardless of preoperative test results, in line with previously described guidelines.13 It is also possible that patients may have been exposed to SARS-CoV-2 after surgery. To the extent possible, reducing inpatient hospital stays for all patients with hip fractures is critical to reduce the risk of spreading COVID-19 and reducing mortality in this vulnerable population. In our attempts to decrease hospital stay, we drastically changed our discharge practices early in the COVID-19 pandemic to discharge patients earlier in their hospital course (eg, postoperative day 0 or 1); however, we recognize that the effort to minimize SARS-CoV-2 exposure may have been at the expense of discharging too early and missing typical perioperative complications.
Although there are abundant data highlighting the importance of timely surgical intervention in patients with hip fractures, COVID-19 status should play a role in the decision making regarding timing of surgery.14,15 Recent studies suggest that mortality in COVID+ patients might be due to virally driven hyperinflammation, a “cytokine storm,” which corresponds to dramatic elevations in multiple inflammatory markers.16,17 A cytokine storm can lead to widespread organ failure, and the inflammation induced by an acute fracture or the surgery to repair the fracture could further exacerbate inflammation in acutely ill COVID+ patients.18–20 Thus, there may be a role for monitoring inflammatory markers and potentially delaying surgery until the inflammatory markers downtrend, although identifying a threshold level at which point it is “safe” to perform surgery may pose a secondary challenge. This approach would balance the need to stabilize the patient with the potential second-hit from surgery in the acute stage of COVID-19. Targeted immunotherapies or antiviral medications, which could directly reduce specific inflammatory factors induced by a fracture that can also exacerbate a cytokine storm, could be beneficial. Regional anesthesia and long-acting blocks may also play an important role in the temporization of hip fracture care during the acute inflammatory stage of COVID-19 before definitive fixation.21,22 Another important point related to surgical planning is how the informed consent discussion must be tailored to a patient with COVID-19. Acknowledging an elevated mortality rate during the informed consent process will likely influence the patient's and family's decisions regarding temporary or permanent comfort care and the possibility of delayed surgical intervention. Overall, further study will need to better elucidate the optimal surgical timing for COVID+ hip fracture patients and whether medical interventions can be administered before surgery to reduce mortality.
We acknowledge the limitations of this study. First, despite the multicenter nature of this study, the number of COVID+ patients was low. Therefore, the degree to which analyses can elucidate clinical factors associated with poor outcomes is limited. Second, the current study uses patients treated during the pandemic as a comparison group. This group represents an estimate of the baseline of care during the pandemic but does not represent the true baseline of care before the pandemic. Third, we limited our analysis to patients who tested positive for COVID-19. Other studies have highlighted the limited sensitivity of the SARS-CoV-2 rRT-PCR test9 and the need to evaluate potential missed cases in individuals with clinical and/or radiologic evidence of COVID-19.5 Given the high likelihood of asymptomatic COVID-19,23 it is possible that some patients in the sample had asymptomatic COVID-19 and were not tested or developed COVID-19 after a negative test and were not tested.
CONCLUSIONS
This multicenter retrospective cohort study demonstrated that hip fracture patients with concomitant COVID-19 infection had similar comorbidity profiles with significantly increased rates of inpatient mortality compared with those who tested negative or were not tested. Further studies are necessary to identify modifiable factors in patient care that can potentially lead to better outcomes in this high-risk population.
ACKNOWLEDGMENTS
The authors acknowledge Craig Klinger and Daniel Edon for their support in completing this study.
Footnotes
The authors report no conflict of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jorthotrauma.com).
REFERENCES
- 1.Vestergaard P, Rejnmark L, Mosekilde L. Increased mortality in patients with a hip fracture-effect of pre-morbid conditions and post-fracture complications. Osteoporos Int. 2007;18:1583–1593. [DOI] [PubMed] [Google Scholar]
- 2.Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198. [DOI] [PubMed] [Google Scholar]
- 3.Liu Y, Ning Z, Chen Y, et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020. doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- 4.Roche JJW, Wenn RT, Sahota O, et al. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331:1374–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MI B, Chen L, Xiong Y, et al. Characteristics and early prognosis of COVID-19 infection in fracture patients. J Bone Joint Surg Am. 2020;102:750–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Catellani F, Coscione A, Ambrosi RD, et al. Treatment of proximal femoral fragility fractures in patients with COVID-19 during the SARS-CoV-2 outbreak in Northern Italy. J Bone Joint Surg Am. 2020:1–12. doi: 10.2106/JBJS.20.00617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vives J, Jornet-Gibert M, Camara-Cabrera J, et al. Mortality rates of patients with proximal femoral fracture in a Worldwide pandemic. J Bone Joint Surg Am. 2020:1–13. doi: 10.2106/JBJS.20.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:1623–1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323:1843–1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayhew D, Mendonca V, Murthy BVS. A review of ASA physical status—historical perspectives and modern developments. Anaesthesia. 2019;74:373–379. [DOI] [PubMed] [Google Scholar]
- 11.Charlson M, Szatrowski T, Peterson J, et al. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–1251. [DOI] [PubMed] [Google Scholar]
- 12.Yoon SH, Lee KH, Kim JY, et al. Chest radiographic and CT findings of the 2019 novel coronavirus disease (Covid-19): analysis of nine patients treated in Korea. Korean J Radiol. 2020;21:498–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rodrigues-Pinto R, Sousa R, Oliveira A. Preparing to perform trauma and orthopaedic surgery on patients with COVID-19. J Bone Joint Surg Am. 2020;e1:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nyholm AM, Gromov K, Palm H, et al. Time to surgery is associated with thirty-day and ninety-day mortality after proximal femoral fracture. J Bone Joint Surg Am. 2015;97:1333–1339. [DOI] [PubMed] [Google Scholar]
- 15.Sheehan KJ, Sobolev B, Guy P. Mortality by timing of hip fracture surgery: factors and relationships at play. J Bone Joint Surg Am. 2017;99:e106. [DOI] [PubMed] [Google Scholar]
- 16.Ruan Q, Yang K, Wang W, et al. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Behrens EM, Koretzky GA. Cytokine storm syndrome: looking toward the precision medicine era. Arthritis Rheumatol. 2017;69:1135–1143. [DOI] [PubMed] [Google Scholar]
- 19.Loi F, Cordova L, Pajarinen J, et al. Inflammation, fracture, and bone repair. Bone. 2016;86:119–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cruz FF, Rocco PRM, Pelosi P. Anti-inflammatory properties of anesthetic agents. Crit Care. 2017;21:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Debbi EM, Garlich JM, Yalamanchili DR, et al. Fascia Iliaca regional anesthesia in hip fracture patients revisited: which fractures and surgical procedures benefit most? J Orthop Trauma. 2020:1. doi: 10.1097/BOT.0000000000001774. [DOI] [PubMed] [Google Scholar]
- 22.Stephan SR, Garlich JM, Debbi EM, et al. A comparison in outcomes of preoperative single-shot versus continuous catheter fascia Iliaca regional anesthesia in Geriatric hip fracture patients. Injury. 2020;S0020–1383:30355–30357. [DOI] [PubMed] [Google Scholar]
- 23.Sutton D, Fuchs K, D'Alton M, et al. Universal screening for SARS-CoV-2 in Women admitted for delivery. N Engl J Med. 2020:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]