Estimators of glomerular filtration rate (GFR) have been shown to be flawed in critically ill patients, especially for augmented renal clearance (ARC), commonly defined as a measured urinary creatinine clearance (CrCl) ≥ 130 ml/min/1.73 m2 [1]. Therefore, measuring CrCl should be performed in daily practice on the intensive care unit (ICU). However, many ICUs still rely on estimating formulae to monitor GFR [1, 2]. As estimators underestimate measured CrCl in ARC patients, ARC might remain unrecognized and lead to subtherapeutic plasma levels of drugs with predominant renal clearance [3]. Therefore, the aim of this study is to define the most precise GFR estimator, which can then be used to detect ARC when measured CrCl is unavailable.
We performed a multicenter retrospective registry-based [4] cohort study in adult ICUs from 3 tertiary university-affiliated hospitals in Belgium (Leuven, Ghent, Antwerp). All consecutive patients admitted between January 2013 and December 2015 were screened for eligibility. All patients ≥ 18 years old and having at least one measured 24-h urinary CrCl (CrCl24h) were included. Agreement between CrCl24h and formulae estimating renal function, i.e., Cockcroft–Gault (CG), Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI), and Modification of Diet in Renal Disease Study (MDRD), was evaluated on all included ICU days. For the estimator with the best precision, a cut-off for ARC with optimal specificity and sensitivity was identified, by calculating the Youden index [5]. Predictions for ARC using the cut-off value were compared to the actual presence of ARC based on the CrCl24h. Cut-off values with either very high sensitivity (> 95%) or specificity (> 95%) were also identified. Finally, the performance of these cut-offs was evaluated in an external single-center (Leuven, January 2016–December 2016) validation set by receiver-operating characteristics (ROC) curve analysis, using 2000 bootstrap replicates. The same inclusion and exclusion criteria as described above were applied.
A total of 51,604 ICU days were included to define a cut-off. Agreement analysis between CrCl24h, the clinical reference, and the formulae estimating renal function is shown in Table 1. None of the estimators were precise (i.e., standard deviation of the mean bias was large for all estimators), with the CKD-EPI formula performing best over the whole CrCl24h range, and for ARC specifically, as illustrated in Fig. 1a. Hence, the CKD-EPI formula was selected for further analysis. In the validation set, 10,503 ICU days were included. For the CKD-EPI formula, the optimal cut-off for ARC was 96.5 ml/min/1.73 m2. This cut-off showed a sensitivity of 86.6% [85;88.1] and a specificity of 71% [70;71.9]. The cut-off values with very high sensitivity and specificity were 87.3 ml/min/1.73 m2 (sens, 95.8% [95;96.7]; spec, 57.6% [56.6;58.7]) and 125.2 ml/min/1.73 m2 (sens, 31.4% [29.4;33.5]; spec, 95.2% [94.7;95.6]), respectively. The ROC curve analysis including the cut-off values is shown in Fig. 1b. Evaluating the optimal cut-off in the validation set, we found that the proportion of accurate predictions for ARC decreased during the first 2 weeks of ICU stay. The is due to an increased false positive rate (Day-1, 16%; Day-14, 49%).
Table 1.
Agreement analysis between CrCl24h and formulae estimating renal function
| All ICU days (n = 51,604) | CrCl24h < 130 ml/min/1.73 m2 (n = 41,290) | CrCl24h ≥ 130 ml/min/1.73 m2 (n = 10,314) | |
|---|---|---|---|
| Median (IQR) (ml/min/1.73 m2) | |||
| CrCl24h | 73 (37;118) | 58 (30;88) | 166 (145;200) |
| CrClCG | 83 (50;127) | 70 (43;103) | 145 (116;183) |
| eGFRMDRD | 87 (50;130) | 72 (42;109) | 143 (115;185) |
| eGFRCKD-EPI | 88 (51;108) | 75 (43;99) | 116 (104;130) |
| Correlation with CrCl24h = Spearman correlation coefficient | |||
| CrClCG | 0.63° | 0.62° | 0.18° |
| eGFRMDRD, | 0.59° | 0.60° | 0.15° |
| eGFRCKD-EPI | 0.69° | 0.72° | 0.19° |
| Mean bias (95% CI) = mean difference CrCl24h – estimator (ml/min/1.73 m2) | |||
| CrClCG | − 11 (− 11;-10) | − 20 (− 20;-19) | 25 (23;27) |
| eGFRMDRD | − 14 (− 15;− 14) | − 23 (− 23;− 23) | 21 (19;23) |
| eGFRCKD-EPI | 3 (3;4) | − 12 (− 13;− 12) | 66 (64;67) |
| Precision = SD of the bias (ml/min/1.73 m2) | |||
| CrClCG | 55 | 41 | 83 |
| eGFRMDRD | 61 | 46 | 94 |
| eGFRCKD-EPI | 48* | 26* | 62* |
| Accuracy = percentage within 30% of CrCl24h | |||
| CrClCG | 47 | 45 | 58 |
| eGFRMDRD | 45 | 43 | 56 |
| eGFRCKD-EPI | 50 | 51 | 45 |
n number of ICU days; CrCl24h creatinine clearance measured by 24-h urine collection, corrected for body surface area; IQR interquartile range; CrClCG estimated creatinine clearance by the Cockcroft – Gault formula, corrected for body surface area; eGFRMDRD estimated glomerular filtration rate by the 4-variable Modification of Diet in Renal Disease formula; eGFRCKD-EPI estimated glomerular filtration rate by the Chronic Kidney Disease Epidemiology Collaboration formula; SD standard deviation; CI confidence interval
°p < 0,001
*Best performing
Fig. 1.
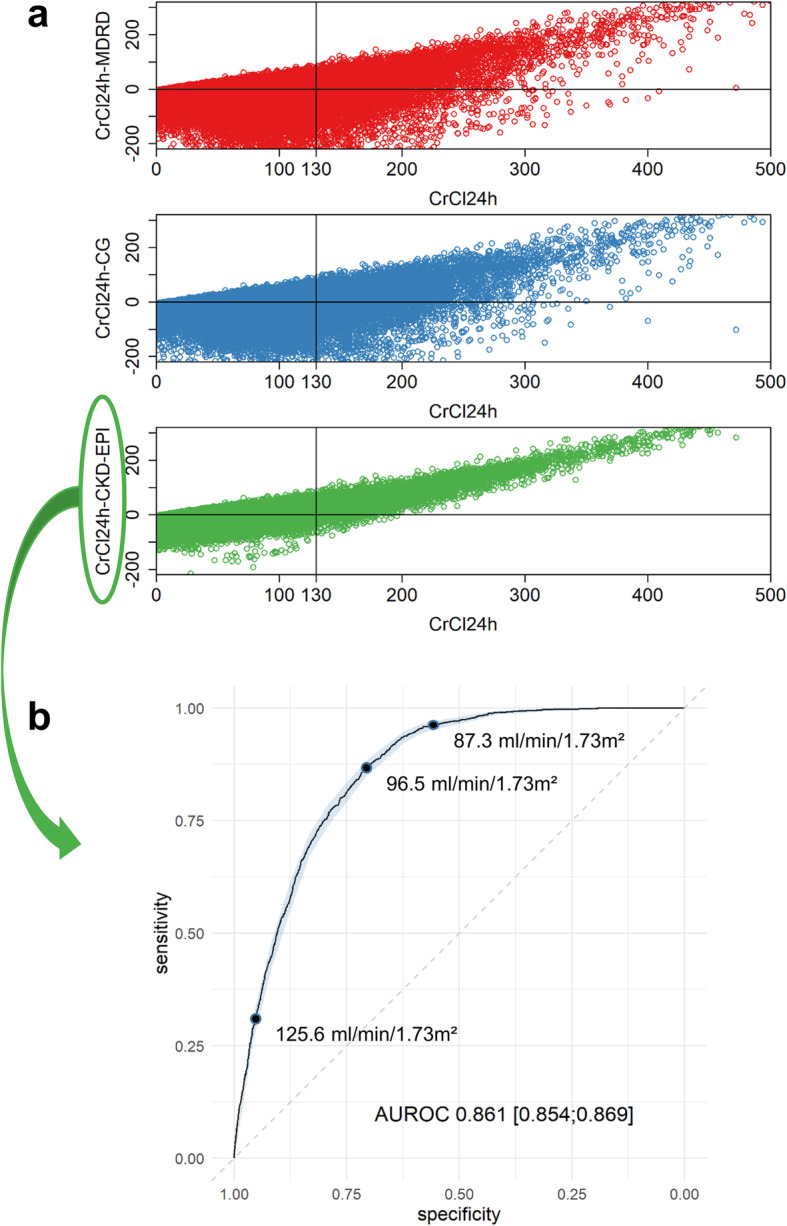
a Bias in function of CrCl24h for the three formulae estimating renal function. Top: MDRD (ml/min/1.73 m2); mid: CG corrected for a body surface area of 1.73 m2 (ml/min/1.73 m2); bottom: CKD-EPI (ml/min/1.73 m2). b Receiver operating characteristics curve analysis for the CKD-EPI formula. The shaded area represents the 95% confidence intervals. The dots represent the cut-off values for optimized sensitivity and specificity, very high (> 95%) sensitivity and very high (> 95%) specificity
Overall, there was poor agreement between CrCl24h and GFR estimators, confirming previous literature [1]. However, the CKD-EPI formula, which is the “least worse” alternative to CrCl24h, provided a cut-off with reasonable performance to detect ARC. Depending on the clinical context, this cut-off can be adapted to increase sensitivity or specificity. When applying this cut-off, the user should note that the accuracy decreases over time during the first 2 weeks of ICU stay. Hence, its largest benefit lies in the beginning of ICU stay. The presented CKP-EPI cut-off can be used to guide upfront increased antimicrobial dosing in patients presenting with ARC early upon ICU admission, when CrCl24h is not available.
Acknowledgements
The authors would like to thank the members of the M@tric research group for helpfully providing the M@tric database. The authors would also like to thank Astrid Eggerickx for her contribution to the analysis of the multicenter cohort.
Abbreviations
- GFR
Glomerular filtration rate
- ARC
Augmented renal clearance
- CrCl
Creatinine clearance
- ICU
Intensive care unit
- CrCl24h
Measured 24-h urinary creatinine clearance
- CG
Cockcroft–Gault formula
- CKD-EPI
Chronic Kidney Disease Epidemiology Collaboration formula
- MDRD
Modification of Diet in Renal Disease Study formula
Authors’ contributions
MG, JW, and IS designed the study. GM and JW revised the study protocol. MG, AW, GM, and IS contributed to the data collection. MG, AW, JW, and IS were responsible for the analysis and interpretation of the data. MG and IS wrote the draft and all co-authors critically revised the manuscript and approved the final version for publication.
Funding
The Flemish Interuniversitary Intensive Care Database Project, later renamed M@tric, was funded by the Flemish government via the Hercules program of the Research Foundation, Flanders (FWO) (AUGE/09/022). GM receives funding from the FWO as senior clinical investigator (1843118 N), and project funding from the KU Leuven (C24/17/072). JW receives funding from FWO as senior clinical investigator (1833317 N). IS receives funding from the Clinical Research Fund of the University Hospitals Leuven, and project funding from the KU Leuven (C24/16/039).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics approval and consent to participate
M@tric data-collection has ethical committee approval from the University Hospitals Ghent, where the database is being hosted (PA 2009/006). Research on the M@tric database requires ethical committee approval of the ethical committee of one of the contributing centers which then independently acts as central ethical committee.
Approval for the present study was obtained from the ethical committee of the University Hospitals Leuven (S61364) for the use of the M@tric dataset, as well as the retrospective Leuven dataset. This research has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Trial registration: The study was registered at ClinicalTrials.gov, NCT03954275.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bilbao-Meseguer I, Rodriguez-Gascon A, Barrasa H, Isla A, Solinis MA. Augmented renal clearance in critically ill patients: a systematic review. Clin Pharmacokinet. 2018;57(9):1107–1121. doi: 10.1007/s40262-018-0636-7. [DOI] [PubMed] [Google Scholar]
- 2.Ruiz S, Minville V, Asehnoune K, Virtos M, Georges B, Fourcade O, et al. Screening of patients with augmented renal clearance in ICU: taking into account the CKD-EPI equation, the age, and the cause of admission. Ann Intensive Care. 2015;5(1):49. doi: 10.1186/s13613-015-0090-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Udy AA, Roberts JA, Lipman J. Clinical implications of antibiotic pharmacokinetic principles in the critically ill. Intensive Care Med. 2013;39(12):2070–2082. doi: 10.1007/s00134-013-3088-4. [DOI] [PubMed] [Google Scholar]
- 4.M@tric project [Available from: https://www.matric.be/]. Accessed 4 Nov 2019.
- 5.Fluss R, Faraggi D, Reiser B. Estimation of the Youden index and its associated cutoff point. Biom J. 2005;47(4):458–472. doi: 10.1002/bimj.200410135. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.


