Abstract
Purpose
Proximal tibial metaphyseal fractures can be complicated by a late valgus deformity, referred to as Cozen’s phenomenon. We studied children with such fractures to determine whether the child’s age at the time of injury influenced the development of Cozen’s as well as the occurrence of elongation. In addition, we explored whether the deformity resolved at long-term follow-up.
Methods
We conducted a retrospective study of 33 patients (six months to 14 years old). Mean follow-up was 8.8 years (3 to 25). We measured angulation of the fractured limb post-treatment, at maximum deformity and final follow-up, as well as elongation and compared them with the uninjured limb.
Results
Three of the fractures were treated surgically whereas the rest, nonoperatively. In all, 15 out of 33 fractures developed late valgus deformity between eight and 19 months (mean time 12.5 months). A total of 24 fractures developed elongation. We found no association of either of these with age. Angulation increased to a statistically significant level, from post-treatment to maximum deformity, and then decreased at final follow-up, leaving no statistically significant difference from the initial measurement. The difference in valgus between fractured and uninjured limb increased to a statistically significant level from post-treatment to maximum deformity and then decreased, leaving an excess from the initial measurement.
Conclusion
In almost half the patients, late valgus deformity developed within two years post-fracture and corrected to the initial post-treatment angles. Patients should be warned of this possibility and reassured of its natural resolution.
Level of evidence
IV
Keywords: proximal tibial metaphyseal fractures, Cozen’s phenomenon, valgus deformity, elongation, children, age
Introduction
In paediatric orthopaedics it is common practice to advise long-term follow-up for certain fractures with known late onset complications. This is for the sake of identifying them upon their occurrence and subsequently treating them, in cases where we do not expect correction to ensue.
The incidence of all proximal tibial fractures in children is 5 to 6/100 000.1 They can be followed by numerous complications, such as angular deformity and leg-length discrepancy and in certain cases, can even lead to compartment syndrome and Volkmann’s ischaemia.2 In particular, proximal tibial metaphyseal fractures are known to result in late valgus deformity. Dr Cozen, in his article published in 1953,3 was the first to describe a valgus deformity of the tibia that occurs after a patient sustains a proximal tibial metaphyseal fracture. We tend to refer to the complication of late valgus deformity which may occur as ‘Cozen’s phenomenon’.
In this study we reviewed 33 patients treated for proximal tibial fractures in order to determine if the child’s age at the time of the fracture influences the development of Cozen’s phenomenon as well as the occurrence of elongation. In addition, given the fact that the literature is unclear as to whether the deformity resolves or whether it needs to be addressed surgically, we recorded residual deformity at long-term follow-up.
Patients and methods
We conducted a retrospective study of patients with proximal tibial fractures (± fibula) treated at our institution by reviewing patients’ records. We did not include patients with physeal injuries or underlying metabolic disorders. A total of 34 patients with 35 proximal metaphyseal fractures (one child had a bilateral fracture) who were treated between January 1990 and 2015, were available for follow-up. We excluded the child with bilateral tibial fractures because we assessed angular deformity as well as elongation in comparison with the unaffected side. Informed consent was obtained from all patients included.
There were 20 boys and 13 girls. Out of the 33 fractures, 21 involved the left limb and 12 the right. In all, 12 children had sustained a pedestrian injury, having been hit by bicycle, motorcycle or car. Six children had suffered a fall. Five children had sustained a bicycle injury. Four children were injured during sports. Three were injured in a road traffic accident. Two sustained stress fractures. One child was injured when its leg was caught in a swing. The age of the children at the time of injury ranged from six months to 14 years, with a mean age of 6.8 years (sd 3.96). Two of our patients were younger than 18 months and, therefore, child abuse had to be ruled out. In one of these cases the child fell from a couch and in the other, the child fell from the parent’s grip. No case for abuse was established in either of the cases.
As far as fracture type is concerned, there were 11 greenstick fractures, nine complete displaced fractures, seven undisplaced hairline fractures, four torus fractures and two stress fractures. There were no open fractures.
Patients were examined clinically and radiologically with plain radiographs of both tibias, anteroposterior and lateral. Angulation was calculated on the anteroposterior radiograph by determining the angle between a line perpendicular to the upper epiphyseal plate and the axis of the tibial shaft below the fracture site according to Visser and Veldhuizen.4 Elongation was assessed clinically at final follow-up with patients standing, using the medial malleolus tip and the superior surface of the medial condyle as landmarks.
For all patients, post-treatment angulation was recorded as well as angulation of the unaffected limb (first measurement). In patients who developed valgus deformity within two years of follow-up, the maximum valgus value was recorded as well as the angulation at that time of the unaffected side (second measurement). In addition, residual valgus deformity at final follow-up and angulation of the unaffected side were calculated (third measurement). Values are recorded in degrees. We also chose to examine tibial elongation as a difference in centimetres compared with the uninjured side by clinical assessment at final follow-up (Table 1). Between initial fracture management and final follow-up, no further surgery was performed.
Table 1.
Results: patient demographics, angulation (°) post-treatment (first measurement), at maximum deformity (second measurement) and final follow-up (third measurement) of fractured and uninjured limb
| Count | Percentage (%) | Mean | Range | |
|---|---|---|---|---|
| Sex | ||||
| Male | 20 | 60 | ||
| Female | 13 | 39 | ||
| Age, years | 6.8 | 13.5 | ||
| Fractured limb (first measurement) | 3.0 | 16.0 | ||
| Fractured limb (second measurement) | 5.8 | 23.0 | ||
| Fractured limb (third measurement) | 3.1 | 16.0 | ||
| Uninjured limb (first measurement) | 2.5 | 12.0 | ||
| Uninjured limb (second measurement) | 2.2 | 12.0 | ||
| Uninjured limb (third measurement) | 1.2 | 11.0 | ||
| Elongation, cm | .6 | 1.5 | ||
The Linear Bivariate Correlation method was used to investigate the relationship between elongation with age. For normality testing, in order to select the appropriate correlation index (Pearson or Spearman) the Shapiro-Wilk test was used.5
For the study of the relationship between the three valgus values (post-treatment, at maximum deformity, at final follow-up) of the fractured limb and of the difference between the fractured and the uninjured limb with the age of the child, two-way analysis of variance repeated measures were applied.6,7
Statistical analysis was conducted using IBM SPSS Statistics, Version 25.0 (Armonk, New York). A p-value < 0.05 was considered statistically significant for all tests.
Results
A total of 30 fractures were treated nonoperatively. In cases with angulation, specifically six complete fractures and eight greenstick fractures, reduction was performed under general anaesthesia. In all cases treated conservatively, a long leg cast was applied for four to eight weeks depending on the child’s age.
The remaining three complete fractures were treated surgically. In particular, a nine-year-old boy who sustained a complete displaced fracture during a pedestrian injury, underwent open reduction and Kirschner-wire fixation. This boy was at risk for compartment syndrome and, therefore, fasciotomies were performed as well.
A six-year-old girl suffered a complete displaced fracture after falling from the first floor of an apartment block. She was treated by open reduction and Kirschner-wire fixation. She was at risk for compartment syndrome and, therefore, fasciotomies were performed as well. In addition, a seven-year-old boy who fell from his own height and was then squashed by an older child, sustained a complete fracture which was treated surgically with closed reduction and Kirschner-wire fixation.
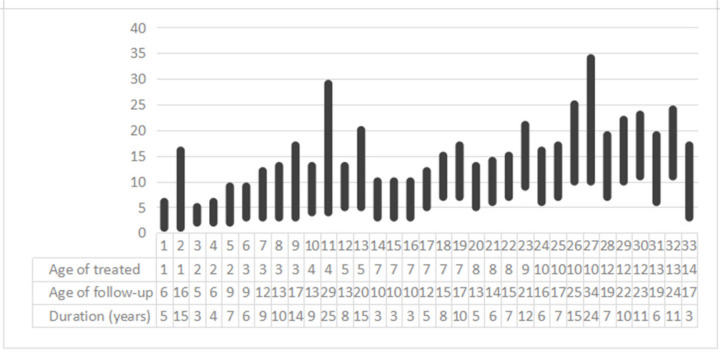
All children were followed up until healing of the fracture. They were then re-examined at six months, one year, 18 months and two years post-injury for the detection of late valgus deformity. Finally, all children were recalled for follow-up at the time the study was conducted. Final follow-up ranged from three years to 25 years with a mean time of 8.8 years (sd 5.42) (Fig. 1).
Fig. 1.
Age follow-up graph including: age of the children when treated; age of the patients at final follow-up; and years of follow-up. Children’s ages have been rounded to the nearest integer.
The patient with the longest follow-up of 25 years was four years old at the time of injury. He sustained a greenstick fracture due to a pedestrian injury. This was treated conservatively with reduction under general anaesthesia and cast wedging. There was an 8° angulation post-reduction similar to the uninjured side. He developed a maximum valgus deformity of 19° with a 13° difference from the uninjured side at 18 months. At final follow-up of 25 years, the left limb had a remaining 5° valgus angulation in comparison with the uninjured side. The elongation of the left limb was 1.5 cm when compared with the right uninjured side, assessed clinically (Figs 2 to 6).
Fig. 2.

Four-year-old patient, right uninjured limb at time of injury.
Fig. 6.
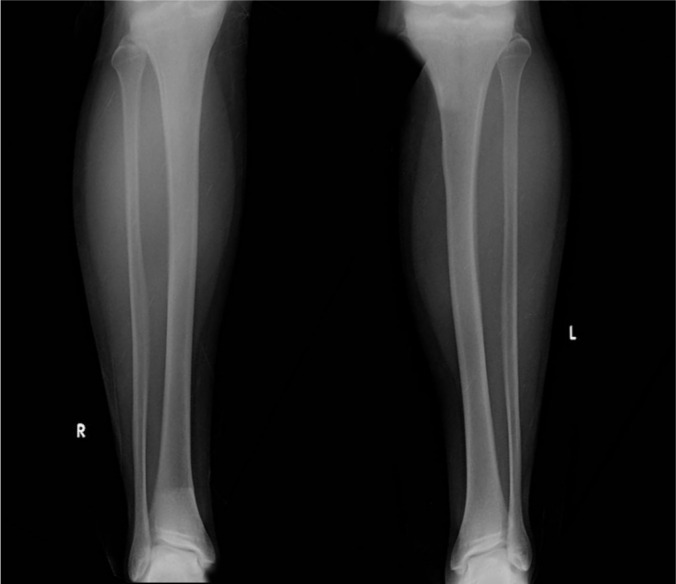
The 25-year follow-up X-rays of right and left limb. Left injured limb has a remaining angulation of 5° compared with the right uninjured side.
Fig. 3.

Four-year-old patient, left limb greenstick fracture.
Fig. 4.

Left limb after cast wedging.
Fig. 5.

Both limbs standing X-ray at 18 months post-injury where there is a 19° angulation of the left limb.
Out of the 33 patients, 15 developed late valgus deformity (Table 2). Maximum valgus deformity occurred between eight and 19 months post-fracture (mean 12.5 months, sd 4.17).
Table 2.
Cozen patients’ characteristics
| Age | Type of fracture | Treatment | Fracture angulation | F 1st M | U 1st M | F 2nd M | U 2nd M | F 3rd M | U 3rd M |
|---|---|---|---|---|---|---|---|---|---|
| 2 | Hairline | Cast | 5 | 5 | 5 | 13 | 5 | 4 | 0 |
| 2 | Torus | Cast | 0 | 0 | 0 | 4 | 0 | 2 | 1 |
| 3 | Greenstick | Cast | 10 | 10 | 8 | 16 | 8 | 4 | 0 |
| 3 | Greenstick | Reduction, cast wedging | 16 | 9 | 8 | 17 | 7 | 8 | 4 |
| 3 | Greenstick | Cast | 7 | 7 | 7 | 11 | 7 | 7 | 3 |
| 3 | Greenstick | Reduction, cast wedging | 8 | 4 | 4 | 18 | 5 | 9 | 3 |
| 4 | Greenstick | Reduction, cast wedging | 24 | 8 | 8 | 19 | 6 | 5 | 0 |
| 5 | Greenstick | Cast | 7 | 7 | 5 | 14 | 5 | 5 | 0 |
| 7 | Complete | Reduction, cast wedging | 14 | 0 | 5 | 6 | 4 | 4 | 0 |
| 7 | Greenstick | Reduction, cast | 12 | 0 | 0 | 12 | 2 | 8 | 4 |
| 7 | Complete | Cast | 4 | 4 | 4 | 6 | 2 | 3 | 3 |
| 7 | Complete | ORIF k-w | 25 | 12 | 0 | 15 | 0 | 10 | 6 |
| 9 | Complete | ORIF k-w | 10 | 0 | 0 | 7 | 0 | 3 | 0 |
| 10 | Greenstick | Reduction, cast wedging | 20 | 5 | 3 | 6 | 3 | 3 | 0 |
| 13 | Complete | Reduction, cast | −5* | −2* | 0 | 5 | 0 | 5 | 0 |
negative values refer to varus angulation, reduction was performed under general anesthetic
F, fractured limb; U, uninjured limb; 1st M, first measurement after treatment; 2nd M, second measurement at maximum deformity; 3rd M, third measurement at final follow-up; ORIF, Open Reduction Internal Fixation; k-w, Kirschner-wire.
Children’s ages have been rounded to the nearest integer.
Furthermore, 24 out of the 33 fractures developed elongation. Elongation occurred in all of the patients who developed Cozen’s phenomenon but also in nine more patients who did not. In the patients who developed elongation, the fractured tibia was between 0.3 cm and 1.5 cm longer at final follow-up in comparison with the uninjured (mean elongation 0.6 cm, sd 0.48). The association between elongation of the fractured limb and the children’s age at the time of fracture was studied, however, no statistically significant correlation (ρ Spearman = 0.141; p = 0.435)was identified.
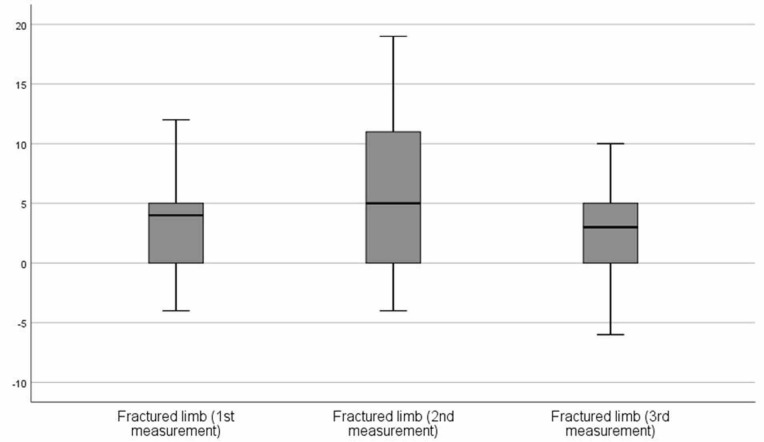
The angulation of the fractured limb was studied, beginning from post-treatment angulation, progressing to maximum deformity and reaching final follow-up. Mauchly’s test of sphericity indicated the assumption of sphericity was not violated (p = 0.091) and, therefore, a correction was not used. There was a significant difference in the total of participants among the three measurements (F = 7.232; p = 0.002).
In order to investigate this, the linear contrast was used. From the first to the second measurement (post-treatment to maximum deformity) there was a statistically significant difference (F = 8.455; p = 0.007) and, in particular, an increase in the valgus angle. From the second to the third measurement (maximum deformity to final follow-up), there was a statistically significant difference (F = 9.779; p = 0.004) and, in particular, a decrease in the valgus angle. Among the first and third measurement there was no statistically significant difference (F = 0.055; p = 0.816) indicating that that valgus angle of the fractured limb had decreased to post-treatment values by final follow-up (Fig. 7).
Fig. 7.
Box plots of valgus angle of injured limb post-treatment, at maximum deformity, at final follow-up
Regarding the relationship between the valgus angle of the fractured limb with age, the probability value was not < 5% (F = 1.912; p = 0.156), meaning there is no interaction between the two variables.
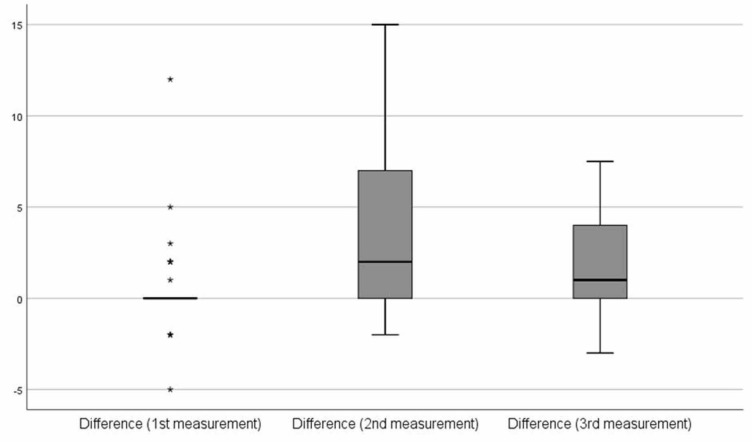
The difference in angulation between the limbs was studied, post-treatment, at maximum deformity and at final follow-up. Mauchly’s test of sphericity indicated that the assumption of sphericity was not violated (p = 0.051) and, therefore, a correction was not used. There was significant difference in the total of participants among the three measurements (F = 9.329; p< 0.001).
In order to investigate this, the linear contrast was used: from the first to the second measurement there was a statistically significant difference (F = 12.745; p = 0.00) and, in particular, an increase in the difference of valgus angle between the fractured and uninjured limb. From the second to the third measurement, there was a statistically significant difference (F = 9.670; p = 0.004) and, in particular, a decrease. Between the first and third measurement there was a statistically significant difference (F = 2.869; p = 0.010) and, in particular, an increase indicating that at final follow-up there remained an excess of valgus of the injured limb compared with the uninjured (mean 1.9°, sd 2.53) (Fig. 8).
Fig. 8.
Box plots of difference in the valgus angle between injured and uninjured limb post-treatment, at maximum deformity, at final follow-up
A clinical examination at final follow-up was conducted for all patients. The range of movement of the knee was compared with the uninjured side and no differences were identified. No patients had been adversely affected by the elongation of the injured side and none had needed to use a shoe insert. No patients complained of remaining pain. No patients mentioned restrictions in either movement or activities.
Discussion
Since the original paper by Cozen,3 several theories have been proposed to explain the phenomenon of valgus deformity. A recent article8 attempted to categorize the articles according to theory. One of the most popular theories suggests that increased vascular response to the fracture causes asymmetric stimulation of the medial proximal tibial growth plate.9-16 Another theory is that the soft-tissue interposition at the fracture site causes the valgus deformity.4,17-20 Some authors have attributed the deformity to loss of reduction or initial malreduction of the fracture.3,16,21,22 Other authors have argued that the tethering by the fibula or the iliotibial band causes the deformity.3,17,23,24 In addition, early weight-bearing after fracture and/or native valgus angulation has been blamed for the deformity before rigid callus formation.25,26
We postulated that the development of Cozen’s phenomenon could be influenced by the child’s age at the time of the fracture. This assumption was based on the known fact that there is a physiological genu valgum in children after the age of two years, which reaches its peak at the age of four years and usually resolves by the age of seven years, as is portrayed in the Salenius curve.27 However, we found no association between the valgus angulation of the fractured limb and the age of the child at the time of fracture.
By reviewing the literature, we found that it was unclear whether Cozen’s phenomenon resolves on its own. Skak et al28 published a case series of 40 children aged from nine months to 12 years, with fractures of the proximal metaphysis, who were followed up between three and 14 years of the injury. He concluded that 15% of greenstick and complete fractures developed valgus deformity whereas it was not recorded either in buckle or in fissure fractures. Predisposing factors were young age and persistent valgus at the fracture site union. The authors recommended that the only indication for operative treatment was a persisting medial gap after closed manipulation.
Tuten et al29 re-evaluated seven patients aged 11 months to 6.3 years with proximal tibial metaphyseal fractures, who had developed a valgus deformity within 12 months after healing of the fracture. They were followed up for an average of 15 years and three months. In all patients, the affected tibia was longer than the uninjured tibia. The authors concluded there was spontaneous improvement of the deformity.
Zionts and MacEwan30 reviewed the cases of seven children aged 11 months to six years and four months with post-traumatic tibia valga. The children were followed up for an average of 39 months. All patients exhibited overgrowth of the injured tibia. Adequate correction occurred spontaneously in six of the patients and, therefore, the authors recommended a conservative approach of both the acute fracture and the valgus deformity.
Burton and Hennrikus8 reviewed 14 children with nondisplaced tibial fractures. They were aged one to six years and followed up for 16.2 months. They developed a valgus deformity at an average of 8.8 months. In all, 50% of patients developed a 5° valgus difference from the uninjured side. The authors recommended treatment in long leg cast with knee in extension and valgus mould.
Nenopoulos et al31 followed up 31 children (32 fractures) with proximal metaphyseal tibial fractures aged up to 14 years, for an average of 4.8 years. In all, 90.3% developed post-traumatic tibia valga. In addition, 27 patients developed lengthening. A total of 11 patients with a valgus angulation > 5° were re-evaluated at an average of 7.4 years from initial injury. Partial remodelling (2° to 3°) was observed in 54.5% of patients and total in 25%. The authors also noted that undisplaced fractures developed valgus deformity to a smaller degree compared with those affecting only the medial cortex and displaced fractures. They recommended against aggressive treatment and advised follow-up during skeletal development.
Our data analysis provided similar findings to those of Nenopoulos et al.31 The mean valgus angle of the fractured limb at maximum deformity was 5.8°. This reduced to 3.1° (mean value) at final follow-up. In comparison with the uninjured limb, there was as excess of 1.9° valgus (mean value) of the fractured limb. None of our patients were clinically affected by this.
However, not all authors suggest a wait and see approach. Müller at al32 published a case series of seven children aged from two years and ten months to ten years and two months who were followed up for an average of 34 months. They observed valgus deformity occurring in all cases and partial remodelling seen only in children up to the age of five years. Therefore, they recommended surgical correction and osteosynthesis as a preferred method of treatment.
In fact, in a most recent paper, Morin et al33 treated 19 patients with proximal tibial fractures who developed valgus deformity by guided growth at 18 months post-fracture. In this paper it is stated that the philosophy of “expectant management” was based upon the misguided hope for spontaneous remodelling.
Conclusion
We reached two interesting conclusions. In almost half of our patients, late valgus deformity of the fractured limb developed within two years post-fracture and corrected to the initial post-treatment angles until final follow-up (mean follow-up 8.8 years). However, when compared with the uninjured limb, there was an excess of valgus (mean 1.9°) of the fractured limb at final follow-up. This could explain the controversy in the literature as to whether the deformity resolves. In addition, about three-quarters of the patients developed elongation (mean 0.6 cm).
Neither valgus angulation nor elongation were influenced by the child’s age at the time of the fracture.
Advantages of our study are that all children’s ages were represented and that there was a long-term follow-up. Disadvantages include the limited number of patients (however, to our knowledge, no large case series exists in the literature), the fact that some patients were adults at the time of final follow-up and the lack of a patient questionnaire completion.
This study indicates that in cases of proximal tibial metaphyseal fractures, patients and their parents should be warned of the possibility of late valgus deformity and reassured of its natural resolution. Emphasis should be given at adequate initial management by achieving acceptable reduction, either by nonoperative means, or by surgical means when needed. Secondary surgery would be the exception in cases in which there remains a marked difference between the limbs, provided the patient is symptomatic.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: The study was approved by the institution’s Scientific Ethics Committee. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all of the participants.
ICMJE Conflict of interest statement
None declared.
Author Contributions
YMP: Data acquisition, Design of the study, Drafting the manuscript, Analyzing and interpreting the data, Recalling the patients for follow-up, Treating and following up the patients.
PT: Data acquisition, Design of the study, Drafting the manuscript, Analyzing and interpreting the data, Recalling the patients for follow-up, Treating and following up the patients.
GT: Data acquisition, Design of the study, Critical revision of the manuscript, Treating and following up the patients.
GC: Data acquisition, Design of the study, Critical revision of the manuscript, Treating and following up the patients.
References
- 1. Skak SV. Valgus deformity following proximal tibial metaphyseal fracture in children. Acta Orthop Scand 1982;53:141-147. [DOI] [PubMed] [Google Scholar]
- 2. Rang M. Childrens’ fractures. Philadelphia; Lippincott JB, 1983. [Google Scholar]
- 3. Cozen L. Fracture of the proximal portion of the tibia in children followed by valgus deformity. Surg Gynecol Obstet 1953;97:183-188. [PubMed] [Google Scholar]
- 4. Visser JD, Veldhuizen AG. Valgus deformity after fracture of the proximal tibial metaphysis in childhood. Acta Orthop Scand 1982;53:663-667. [DOI] [PubMed] [Google Scholar]
- 5. Yap BW, Sim CH. Power comparison of Shapiro-Wilk, Kolmogorov-Smirnov, Lilliefors and Anderson-Darling tests. J. Stat. Model. Analytics 2011;1:21-33. [Google Scholar]
- 6. Shuttleworth M. Repeated measures design. Experiment-resources.com (date last accessed 02 September 2013).
- 7. Bakeman R. Recommended effect size statistics for repeated measures designs. Behav Res Methods 2005;37:379-384. [DOI] [PubMed] [Google Scholar]
- 8. Burton A, Hennrikus W. Cozen’s phenomenon revisited. J Pediatr Orthop B 2016;25:551-555. [DOI] [PubMed] [Google Scholar]
- 9. Blount WP. Fractures in children. Baltimore, PA: Williams and Wilkins Co, 1954. [Google Scholar]
- 10. Griffin PP. The lower limb. In: Lovell WW, Winter RB, eds. Pediatric orthopaedics. Philadelphia, PA: J. B. Lippincott, 1978:884-886. [Google Scholar]
- 11. Houghton GR, Rooker GD. The role of the periosteum in the growth of long bones. An experimental study in the rabbit. J Bone Joint Surg [Br] 1979;61-B:218-220. [DOI] [PubMed] [Google Scholar]
- 12. Green NE. Tibia valga caused by asymmetrical overgrowth following a nondisplaced fracture of the proximal tibial metaphysis. J Pediatr Orthop 1983;3:235-237. [DOI] [PubMed] [Google Scholar]
- 13. Jordan SE, Alonso JE, Cook FF. The etiology of valgus angulation after metaphyseal fractures of the tibia in children. J Pediatr Orthop 1987;7:450-457. [DOI] [PubMed] [Google Scholar]
- 14. Aronson DD, Stewart MC, Crissman JD. Experimental tibial fractures in rabbits simulating proximal tibial metaphyseal fractures in children. Clin Orthop Relat Res 1990;255:61-67. [PubMed] [Google Scholar]
- 15. Ogden JA. Skeletal injury in the child. New York, NY: Springer Verlag, 1999. [Google Scholar]
- 16. Lalonde F, Wenger D. Tibia. In: Rang M, Pring M, Ray D, eds. Rang’s children’s fractures. Philadephia, PA: Lippincott Williams & Wilkins, 2005. [Google Scholar]
- 17. Jackson DW, Cozen L. Genu valgum as a complication of proximal tibial metaphyseal fractures in children. J Bone Joint Surg [Am] 1971;53-A:1571-1578. [PubMed] [Google Scholar]
- 18. Weber BG. Fibrous interposition causing valgus deformity after fractures of the upper tibial metaphysis in children. J Bone Joint Surg [Br] 1977;59-B:290-292. [DOI] [PubMed] [Google Scholar]
- 19. Coates R. Knock knee deformity following upper tibial greenstick fractures. J Bone Joint Surg [Br] 1977;59-B:516. [Google Scholar]
- 20. Rooker GD, Coates RL. Deformity after greenstick fractures of the upper tibial metaphysis. In: Houghton GR, Thompson GH, eds. Orthopaedics 1. Problematic musculoskeletal injuries in children. London: Butterworths, 1983:1-13. [Google Scholar]
- 21. Salter RB, Best TN. Pathogenesis and prevention of valgus deformity following fractures of the proximal metaphyseal region of the tibia in children. J Bone and Joint Surg [Br] 1972;54-B:767. [PubMed] [Google Scholar]
- 22. Bahnson DH, Lovell WW. Genu valgum following fracture of the proximal tibial methaphysis in children. Orthop Trans 1980;4:306. [Google Scholar]
- 23. Goff CW. Surgical treatment of unequal extremities. Springfield: Thomas, 1960. [Google Scholar]
- 24. Taylor SL. Tibial overgrowth: a cause of genu valgum. J Bone Joint Surg [Am] 1963;45-A:659. [Google Scholar]
- 25. Lehner A, Dubas J. Secondary deformities after separation of epiphyses and after fractures close to epiphysial lines. Helv Chir Acta 1954;21:388-410. [PubMed] [Google Scholar]
- 26. Pollen AG. Fractures and dislocations in children Edinburgh. London: Churchill Livingstone, 1973. [Google Scholar]
- 27. Salenius P, Vankka E. The development of the tibiofemoral angle in children. J Bone Joint Surg [Am] 1975;57-A:259-261. [PubMed] [Google Scholar]
- 28. Skak SV, Jensen TT, Poulsen TD. Fracture of the proximal metaphysis of the tibia in children. Injury 1987;18:149-156. [DOI] [PubMed] [Google Scholar]
- 29. Tuten HR, Keeler KA, Gabos PG, Zionts LE, MacKenzie WG. Posttraumatic tibia valga in children. A long-term follow-up note. J Bone Joint Surg [Am] 1999;81-A:799-810. [DOI] [PubMed] [Google Scholar]
- 30. Zionts LE, MacEwen GD. Spontaneous improvement of post-traumatic tibia valga. J Bone Joint Surg [Am] 1986;68-A:680-687. [PubMed] [Google Scholar]
- 31. Nenopoulos S, Vrettakos A, Chaftikis N, Beslikas T, Dadoukis D. The effect of proximal tibial fractures on the limb axis in children. Acta Orthop Belg 2007;73:345-353. [PubMed] [Google Scholar]
- 32. Müller I, Muschol M, Mann M, Hassenpflug J. Results of proximal metaphyseal fractures in children. Arch Orthop Trauma Surg 2002;122:331-333. [DOI] [PubMed] [Google Scholar]
- 33. Morin M, Klatt J, Stevens PM. Cozen’s deformity: resolved by guided growth. Strategies Trauma Limb Reconstr 2018;13:87-93. [DOI] [PMC free article] [PubMed] [Google Scholar]