Abstract
Purpose
Since the state of alarm was decreed in Spain on 14 March 2020, the coronavirus disease 2019 (COVID-19) pandemic has had an extraordinary impact in paediatric hospitals. This study shows the effect of the pandemic on our practice in paediatric orthopaedics in a referral third level paediatric hospital.
Methods
We performed a single-centre retrospective review of the official census from a third level paediatric hospital from 14 March to 14 April for the years 2018, 2019 and 2020.
Results
The patients seen in our clinic during this period in 2020 decreased in by 82% (p < 0.001) compared with 2018 and 2019, however, the number of telemedicine consultations increased by 90.21% (p < 0.001). The total number of patients attending the clinic (including onsite and virtual) was reduced by 54.25% (p < 0.001). The total surgeries performed plummeted by 81% in this period in 2020 (p < 0.001) due to a reduction in elective cases of 94.6% (p < 0.001). No significant decrease was found in the number of urgent surgical cases per day in 2020 (p = 0.34). Finally, the number of orthopaedic patients admitted to our emergency department dropped by 78.6% during the state of alarm (p < 0.001).
Conclusion
According to our results, the pandemic has significantly affected our daily practice by decreasing elective surgeries and onsite clinics, but other activities have increased. As we have implemented telemedicine and new technologies to adapt to this setback, we should take advantage of the situation to change our practice in the future to better allocate our health resources and to anticipate outbreaks.
Published without peer review.
Level of Evidence
IV
Keywords: COVID-19, pandemics, paediatric orthopaedics, telemedicine, emergencies
Introduction
Since December 2019, a novel coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has emerged from Wuhan, Hubei Province, China.1,2
Paediatric clinical manifestations are not typical, and relatively milder, compared with adult patients.3 As COVID-19 is having a major impact on all aspects of healthcare delivery worldwide, this has created unique challenge for children’s hospitals regarding patients’ and health workers’ safety and their role in containing the spread of COVID-19 through the community.4 In this context, paediatric hospitals around the world are not on the ‘frontline’, and as a consequence, these hospitals have become centres for the whole paediatric pathology in other health areas since adult and general hospitals needed to allocate all their health resources for the assistance of adults with the COVID-19 infection.
Besides, changes to orthopaedic clinical practice have been largely guided by three main, overarching principles: a) clinical urgency; b) patient and healthcare worker protection; and c) extraordinary increase of healthcare resources. Patients requiring urgent or early orthopaedic care are still being attended to at the earliest possible opportunity without any difference in routine workflows. Other elective surgical cases have been postponed allowing hospitals to free up beds and respirators for the treatment of patients with confirmed or suspected COVID-19.
On the other hand, outpatients have been individually screened by clinicians and separated into three levels: Level 1: must be seen in person, clinical issue is urgent and physical exam essential; level 2: appropriate for a telephone or telemedicine consultation; level 3: visit should be rescheduled. Other considerations taken into account have been to divide teams to avoid contact between the members of the team to decrease the risk of infection.
Finally, COVID-19 infection is having an extraordinary impact on national health systems around the world, and specifically in monographic paediatric hospitals due to the considerations mentioned above. Since the state of alarm was decreed in Spain on 14 March 2020, a significant modification of our daily practice has been necessary. Likewise, the level of patient flow to external outpatient clinics and the demand for care has changed considerably. This has been previously observed in major televised sport events5-13 To the best of our knowledge, this is the first European study in a national and international referral paediatric centre evaluating the effect of the COVID-19 pandemic on paediatric trauma and orthopaedic pathology.
Materials and methods
Daily patient census figures from a third level paediatric hospital (Hospital Sant Joan de Deu Barcelona) were reviewed retrospectively. Census data from 14 March 2018 to 14 April 2020, including our paediatric orthopaedics outpatient clinic, paediatric trauma emergency department (ED) and paediatric orthopaedic and trauma surgical cases were reviewed to compare the effects of the COVID-19 outbreak. We reviewed both 2018 and 2019 to avoid the effect of Easter holidays during this period in 2018.
For the main outcome, the total mean number of cases per day of the three years and three tiers were compared. As secondary outcomes, we also included timeframe of patient visits to the ED, level of triage, type of surgery (elective or urgent) and type of consultation (onsite or telemedicine (telephone or video call depending on patient requirements)).
Statistical analysis
All data were analyzed using IBM SPSS 26 software (IBM SPSS Inc., Armonk, New York). Univariate statistical analysis consisted of a Student two-tailed t-test to compare the outcomes of mean number of consultations (including onsite and telemedicine), mean number of surgical procedures (including elective and urgent) and emergencies between 2018 and 2019 and 2020 (including triage level). A p-value of < 0.05 was considered statistically significant. In all, 95% confidence intervals were compared to determine significant differences between both years.
Results
The number of patients who attended our orthopaedic clinic onsite, per day, has been reduced from a mean of 66.45 (sd 44.315/151) patients in this period from 2018 to 2019 to 12.0 (sd 16.351/71) patients in the same period of 2020. This means a decrease of 82% (mean difference 54.5 patients). However, the number of virtual consultations such as phone calls, video conferences and meetings on a virtual platform increased substantially, from a mean of 1.88 (1.773/7.0) patients per day in 2018 to 2019 to 19.3 patients per day. This change represents an increase in telephone/online consultations of 90.21% (p < 0.001) (Table 1). If we consider these phone and onsite consultations, the mean number of patients attending per day in the 2020 period was 31.3 (SD 32.389/116) patients compared with 68.3 (sd 46.653/155) patients, resulting in a reduction of 54.25% (p < 0.001). Data referring to patients who attended the clinic are represented in Figures 1 and 2. As seen in Figure 1, the number of clinics in the third week of 2018 was decreased due to the Easter holidays. No patients appear in the fifth week of 2020 because there was only one day with clinics held (13 April). In Figure 2, we can see how the number of telemedicine consultations decreases after the first three weeks in 2020 because the Easter holidays were in the fourth week (01 April to 06 April) and some of the clinics were previously rescheduled as during this period some doctors take vacation for Easter holidays.
Table 1.
Differences between 2018 and 2019, and 2020
| N | Year | Mean (95% confidence interval) | Mean (95% confidence interval) of change | p-value* | |
|---|---|---|---|---|---|
| Onsite clinic | 31 | 2018/2019 | 66.5 (50.2 to 82.7) | 54.5 (37.3 to 71.7) | 0.000 |
| 2020 | 12.0 (6.0 to 18.0) | ||||
| Telemedicine clinics | 2018/2019 | 1.9 (1.2 to 2.5) | 17.4 (10.1 to 24.8) | 0.000 | |
| 2020 | 19.3 (12.0 to 26.6) | ||||
| Total clinics | 2018/2019 | 68.34 (51.6 to 85.1) | 37.0 (16.9 to 57.2) | 0.000 | |
| 2020 | 31.3 (19.4 to 43.1) | ||||
| Surgical procedures | 2018/2019 | 4.9 (4.0 to 5.9) | 3.0 (3.0 to 5.0) | 0.000 | |
| 2020 | 0.9 (0.5 to 1.3) | ||||
| Elective surgeries | 2018/2019 | 3.5 (2.5 to 4.5) | 3.3 (2.3 to 4.3) | 0.000 | |
| 2020 | 0.2 (0.01 to 0.4) | ||||
| Urgent surgeries | 2018/2019 | 1.2 (0.9 to 1.5) | 0.5 (0.04 to 0.9) | 0.034 | |
| 2020 | 0.7 (0.4 to 1.1) | ||||
| Emergencies | 2018/2019 | 39.4 (37.5 to 41.1) | 31.0 (28.8 to 33.1) | 0.000 | |
| 2020 | 8.4 (7.1 to 9.6) | ||||
| Triage | 2018/2019 | 4.0 (3.6 to 4.5) | 0.1 (0.01 to 0.2) | 0.062 | |
| 2020 | 3.9 (3.7 to 4.1) |
Univariate statistical analysis consisted of a student two-tailed t-test to compare the outcomes of mean number of consultations (including onsite and telemedicine), mean number of surgical procedures (including elective and urgent) and emergencies between 2018, 2019 and 2020 (including triage level). A p-value of < 0.05 was considered statistically significant.
Fig. 1.
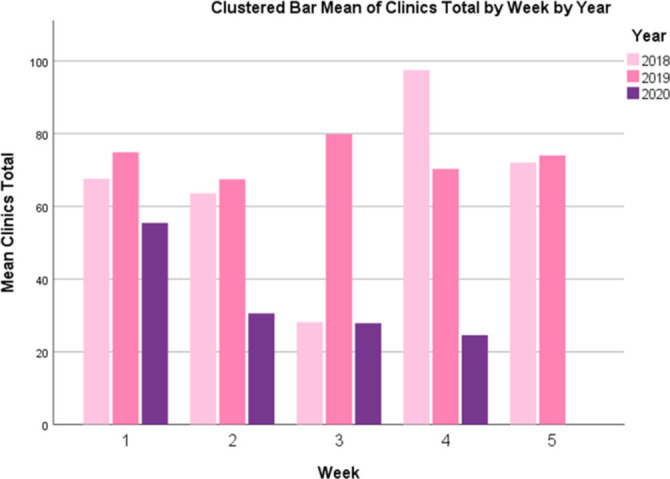
Mean total clinics.
Fig. 2.

Mean telemedicine clinics by year.
If we compare the number of surgical cases during this period in the last two years, in 2018 to 2019 we performed on mean 4.9 (sd 2.569/8.5) surgeries per day, including a mean of 3.5 (sd 2.689/9.0) elective cases and a mean of 1.2 (0.783/2.5) urgent cases; while during the state of alarm, the mean number of surgical cases per day was 0.9 (sd 1.093/4.0), including 0.2 (sd 0.477/2.0) elective cases per day and 0.7 (sd 0.965/3.0) urgent cases per day. This means a reduction of 81% of the surgical cases per day, mostly due to a reduction of the elective cases of 94.6% (p < 0.001). However, no significant decrease was found in the mean number of urgent surgical cases per day (p = 0.34) (Table 1). Among the elective cases, there were three oncological cases, one prominent hardware removal, one symptomatic high-grade spondylolisthesis and one patient with an external fixation for limb deformity who fell and had a loss of correction. All these patients tested negative for COVID-19. This data is represented in Figure 3. As seen in Figure 1, we found a decrease of cases in the third week of 2018 due to Easter holidays in our country in that year.
Fig. 3.
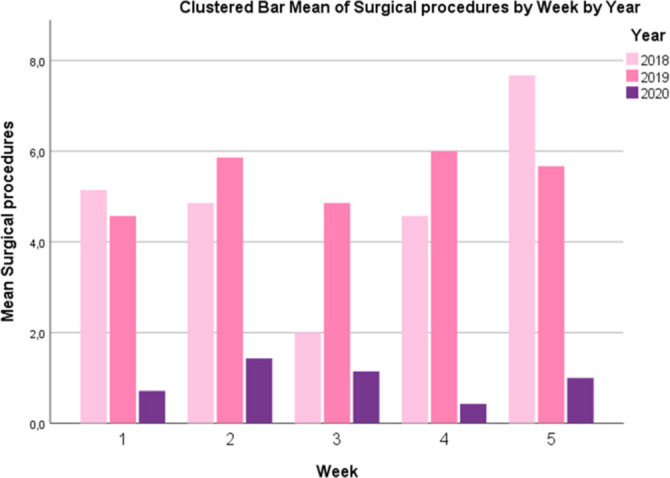
Mean surgical procedures by year.
The census also showed that the number of trauma and orthopaedic patients who attended our paediatric ED plummeted during the state of alarm. While between 14 March and 14 April 2018 and 2019 the mean number of cases per day was 39.2 (SD 4.907/21.0), in the same period of 2020 only 8.4 (sd 3.412/16.0) cases on mean per day attended (78.6% lower) (p < 0.001). According to the Emergency Severity Index (ESI) five-level triage scale,14 patients in 2018-2018-2019 were graded 4.0 (0.177/0.86), whilst in 2020 the mean grade was 3.9 (sd 0.233/1.0). This means that despite the reduction of patients of 78.6%, the severity of those patients was higher. However, this was not found to be significant (p = 0.62). As seen in the previous paragraph, from all the patients seen at the ED, 24 required surgery (8.45%), including five wounds, 18 fractures and one case of septic arthritis that required surgical debridement. Data from the emergencies attended are represented in Figure 4.
Fig. 4.
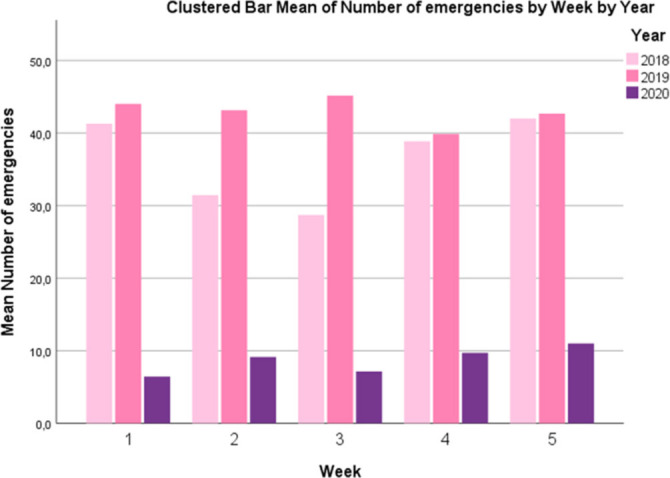
Mean patients attending emergency department by year.
Discussion
COVID-19 has been spreading all over the world during the last few months of 2020. In Spain, the first case reported was a tourist visiting La Gomera Island on 31 January. Since then, the number of cases has increased exponentially and nowadays the number of cases in our country overpass 200 000 with more than 23 000 deaths by April 2020 according to official data from the Spanish government. This is the first time since the Spanish flu pandemic in 1918 that a global pandemic is affecting our national health systems, and no previous studies have been reported. While most of the hospitals in Spain are overwhelmed and field hospitals have been built in major cities such as Madrid and Barcelona, paediatric hospitals and their EDs have seen a decrease in the number of children attending. Since the state of alarm was decreed in Spain on 14 March 2020, the fear of becoming infected during a visit to the hospital has considerably reduced the number of patients attending our hospital. Contrary to other third level adult hospitals where numbers of patients have surpassed capacity nationwide, paediatric hospitals have seen activity decreased. As previously mentioned, few cases of pneumonia in children with SARS-CoV-2 infection have been reported. Paediatric cases are mainly family cluster cases, and most of them have epidemiological links to adult patients. Paediatric clinical manifestations are not typical, and relatively milder, compared with that of adult patients.3 Lately, Dong et al15 reported a series of 2000 children with suspected or confirmed COVID-19. The authors found that 4% of virologically confirmed cases had asymptomatic infection, and this rate almost certainly underestimates the true rate of asymptomatic infection because many children who are asymptomatic are unlikely to be tested. Among children who were symptomatic, 5% had dyspnea or hypoxemia (a substantially lower percentage than the rate reported for adults16) and 0.6% progressed to acute respiratory distress syndrome or multi-organ system dysfunction (a rate that is also lower than that seen in adults). Preschool-aged children and infants were more likely than older children to have severe clinical manifestations.
According to Cruz and Zeichner,17 many infectious diseases affect children differently from adults, and understanding those differences can yield important insights into disease pathogenesis, informing management and the development of therapeutics. This will likely be true for COVID-19, just as it has been for other infectious diseases.
In this uncertain situation, there has been a rush by scientific journals to publish updated data. However, data in the children’s population is still scarce. Preliminary examination of characteristics of COVID-19 disease among children in the United States suggests that children do not always have a fever or cough as reported signs and symptoms. Although most cases reported among children to date have not been severe, clinicians should maintain a high index of suspicion for COVID-19 infection in children and monitor for progression of illness, particularly among infants and children with underlying conditions.18
From an orthopaedic point of view, we have developed a secondary role in this pandemic; nevertheless, COVID-19 is having a major impact on all aspects of our healthcare delivery. According to Chang Liang et al,19 clinicians have been advised to prolong the duration between non-urgent follow-ups to avoid patient overcrowding in hospitals. In their case, all patients are contacted the day before the surgical procedure and are checked for any respiratory symptoms and any risk factors or recent travel history (within 14 days) that might put them at risk for COVID-19. In place of conventional meetings, both faculty and residents can remotely log on for scheduled teaching sessions online using their laptops or handheld devices. In our practice and according to our hospital COVID-19 protocol, all our elective surgical procedure patients are tested 48 hours prior to the procedure. Patients who underwent a surgical procedure were managed according to the protocols and recommendations of the Journal of Bone & Joint Surgery 20 and the Journal of the American Academy of Orthopaedic Surgeons.21 Furthermore, all health workers in our hospital are tested every ten days even in absence of symptoms.
In the same vein, according to Farrell et al,22 the COVID-19 pandemic necessities have modified our paediatric orthopaedic practice to protect patients, families and healthcare workers to minimize viral transmission. General principles include limiting procedures to urgent cases such as traumatic injuries, and deferring outpatient visits during the acute phase of the pandemic. According to the authors, nonoperative methods should be considered where possible. For patients with developmental or chronic orthopaedic conditions, it may be possible to delay treatment for two to four months without substantial detrimental long-term impact.22 We have established this workflow in our daily practice and non-urgent patients have been rescheduled. As our data suggests, the number of virtual consultations (this includes patients for which no complementary exams or physical examination is required) have significantly increased, including telephone consultations, video conferences and virtual platform meetings. Despite the number of onsite patients who visited the outpatient clinic decreasing, if we include telemedicine, the total number of patients seen in this period of 2020 only decreased around 54% from the previous years (p < 0.001). This suggests that telemedicine is a helpful tool for monitoring patients in the clinic without any risk for the patients and caregivers or the staff. From an educational point of view, residents, fellows and consultants can continue their training with video conferences, webinars and online courses. As such, we have implemented video conferencing into our daily rounds and remote access to our computers has been allowed in order to work from home following local ethics and laws.
Despite our daily workflow having been substantially modified, data from our census showed that we are still efficient in our outpatient workflow with around 45% of the activity seen in previous years, meaning that our activity has not been completely stopped. Furthermore, other activities indirectly related to patients assistance have been reinforced during this period. These kind of activities include an increase in research activities, the establishment and improvement of different protocols and clinical pathways and other office management and administration tasks. During this time, we have had periodic video conferences to plan the work for the next weeks according to daily changes in the pandemic. This has included the management of surgical waiting lists and outpatient clinics lists.
Despite the fact that a pandemic is considered a health disaster and as previously mentioned, it has dramatically changed our daily work, it may establish a precedent on how we will work in the future, as the use of new technologies may be more convenient and more efficient for paediatric orthopaedic surgeons. In this context, telemedicine seems to be beneficial for patients from rural and distant areas by eliminating unnecessary travel to the hospital. As telemedicine decreases pressure on our outpatient clinics, this may help to allocate other onsite visits and reduce wait times.23-28
On the other hand, although elective surgical procedures have decreased dramatically, we have still operated for 24 urgent cases and no significant differences in the mean number of urgent surgeries were found compared with previous years. The psychological, emotional and educational consequences of the confinement (since 14 March 2020) are still unknown (school lessons have also switched to virtual education as recommended by the government) but it has also reduced the number of trauma cases derived from falls in the playground, sporting activities or school activities. The fact that the biggest percentage of trauma cases (48.9%) at our ED were registered in the second shift (from 3 pm to 11 pm) could also suggest that children have followed their daily educational tasks and falls have happened after the school time (distance learning at home in this case). Finally, despite the number of trauma cases reducing by 78.6% compared with 2018 and 2019, children triaged according to the ESI triage scale29 showed no significant differences in severity (4.01 in 2018 and 2019 versus 3.89 in 2020) (p = 0.62). From all of the trauma cases admitted to the ED in this period of 2020, 24 patients required surgery (8.45% of 284 cases), while in 2018 and 2019, only 33 patients from 1389 required surgery (2.4%). This suggests that despite the number of trauma and orthopaedic cases being lower in 2020, these were more severe cases. This may also suggest that the parents and caregivers are only bringing their children to the hospital in adverse times such as this pandemic for a major cause, while in our daily practice more seemingly banal trauma is attended.
Despite the fact that according to these results it may seem as if paediatric hospitals are not part of the fight against this pandemic, it must be said that all paediatric and obstetrics cases from the rest of the hospitals have been sent to our hospital to free beds for adult patients with COVID-19 related problems. It was established also that if necessary, adult trauma patients would be sent to our paediatric hospital as most of the adult third level hospitals were overcrowded and occupation of intensive care unit beds was around 100%. It is noteworthy to mention that countless administration and management tasks have been done as part of indirect clinical duties as well as research and education. Staff members were also offered the option to give assistance to other adult and field hospitals if necessary.
Among study limitations, it should be noted that this is only a retrospective observational study obtained from a third level paediatric hospital, comparing only one month since the state of alarm was established in Spain. The objective is to give a general view of what we are finding and how we are changing our practice in the paediatric orthopaedic field. Another limitation is that we still are uncertain as to how this situation will affect our practice in the future, the effects on wait times or if it comes with hefty health resource utilization. For example, in scoliosis patients, time is crucial as a patient’s deformities increase over time. Previous data suggest that surgical procedures to address larger spinal deformities are associated with increased health resource utilization, such as increased operative times and blood loss.30,31 Another limitation is that our staff team formed of 15 senior surgeons was affected by COVID-19; four members were put in quarantine. In the same vein, despite our hospital being a university hospital and receiving residents and fellows from other hospitals, these were required by law to return to their home hospitals to assist with COVID-19 patients. This meant a reduction of 13 residents and three fellows, who added to four consultants in quarantine, meant that we went from 31 members to only 11. Furthermore, these 11 consultants were divided into teams as previously mentioned. This may also have affected the significant decrease in some clinical activities. From the authors’ point of view, we have to take advantage of this difficult situation to change and improve our practice in the future by adopting telemedicine as part of our practice in order to better allocate our health resources as this situation may be repeated infuture years.
Conclusion
As the COVID-19 pandemic has interfered in our daily practice, we have found a decrease in the number of paediatric trauma patients admitted to our ED, the number of patients visiting onsite to our paediatric orthopaedic clinic and the number of elective cases compared with other years. However, the percentage of urgent cases requiring surgery has increased. We also have found an important increase in the number of patients attending by virtual means. This could support a change in our practice in the future by implementing telemedicine as part of our daily work. To the best of our knowledge, this study shows the effect of the COVID-19 pandemic on paediatric orthopaedics practice.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: No human participants and/or animals are involved in this work. Institutional Review Board/Ethics committee approval was not required as this is an official census review. No data or information was reviewed from the patient´s charts.
Informed consent: Informed consent was not required for this study.
Acknowledgement
The authors wish to acknowledge MBA Institute for their contribution during the COVID outbreak.
ICMJE Conflict of interest statement
AP-G reports royalties from Spineart, outside the submitted work.
The other authors declare no conflict of interest.
Author Contributions
AP-G: Data collection, Manuscript preparation.
LC: Manuscript preparation.
AC: Data collection.
LDD: Data collection.
FT-R: Manuscript preparation and design.
CGF: Statistical analysis, Supervision.
References
- 1. No authors listed World Health Organization: Novel coronavirus (2019-nCoV), situation report – 11. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200131-sitrep-11-ncov.pdf?sfvrsn=de7c0f7_4 (date last accessed 31 January 2020).
- 2. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054-1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Weiss P, Murdoch DR. Clinical course and mortality risk of severe COVID-19. Lancet 2020;395:1014-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Parikh SR, Avansino JR, Dick AA, et al. Collaborative multidisciplinary incident command at Seattle Children’s Hospital for rapid preparatory pediatric surgery countermeasures to the COVID-19 pandemic. J Am Coll Surg 2020. April 11 (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Reich NT, Moscati R, Jehle D, Ciotoli M. The impact of a major televised sporting event on emergency department census. J Emerg Med 1994;12:15-17. [DOI] [PubMed] [Google Scholar]
- 6. Murphy SM, Myers E, Kingston R, Connolly P, McElwain JP. Ireland in the World Cup: trauma orthopaedic workloads. Ir Med J 2003;96:119-120. [PubMed] [Google Scholar]
- 7. Moody WE, Hendry RG, Muscatello D. Were attendances to accident and emergency departments in England and Australia influenced by the Rugby World Cup Final 2003? Eur J Emerg Med 2007;14:68-71. [DOI] [PubMed] [Google Scholar]
- 8. Miró O, Sánchez M, Borrás A, Millá J. Football, television and emergency services. Med Clin (Barc) 2000;114:538-539. [DOI] [PubMed] [Google Scholar]
- 9. Galvin GM, Jelinek GA. The impact of the America’s Cup on Fremantle Hospital. Arch Emerg Med 1989;6:262-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cheng D, Yakobi-shvili R, Fernandez J. Major sport championship influence on ED sex census. Am J Emerg Med 2005;23:408-409. [DOI] [PubMed] [Google Scholar]
- 11. Cooke MW, Allan TF, Wilson S. A major sporting event does not necessarily mean an increased workload for accident and emergency departments. Euro96 Group of Accident and Emergency Departments. Br J Sports Med 1999;33:333-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McGreevy A, Millar L, Murphy B, et al. The effect of sporting events on emergency department attendance rates in a district general hospital in Northern Ireland. Int J Clin Pract 2010;64:1563-1569. [DOI] [PubMed] [Google Scholar]
- 13. Farrell S, Doherty GM, McCallion WA, Shields MD. Do major televised events affect pediatric emergency department attendances or delay presentation of surgical conditions? Pediatr Emerg Care 2005;21:306-308. [DOI] [PubMed] [Google Scholar]
- 14. Gilboy N, Tanabe P, Travers D, Eitel D, Wuerz R. Emergency Nurses Association. The Emergency Severity Index. Des Plaines; 2003. https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/systems/hospital/esi/esihandbk.pdf (date last accessed 27 May 2020). [Google Scholar]
- 15. Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 among children in China. Pediatrics 2020;145:e20200702. [DOI] [PubMed] [Google Scholar]
- 16. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus- infected pneumonia in Wuhan, China. JAMA 2020;323:1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cruz AT, Zeichner SL. COVID-19 in children: initial characterization of the pediatric disease. Pediatrics 2020. March 16 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 18. Bialek S, Gierke R, Hughes M, et al. Coronavirus disease 2019 in children - United States, February 12-April 2, 2020. MMWR Morb Mortal Wkly Rep 2020;69:422-426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chang Liang Z, Wang W, Murphy D, Po Hui JH. Novel coronavirus and orthopaedic surgery: early experiences from Singapore. J Bone Joint Surg [Am] 2020;102:745-749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rodrigues-Pinto R, Sousa R, Oliveira A. Preparing to perform trauma and orthopaedic surgery on patients with COVID-19. J Bone Joint Surg [Am] 2020. April 10 (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Awad ME, Rumley JCL, Vazquez JA, Devine JG. Peri-operative considerations in urgent surgical care of suspected and confirmed COVID-19 orthopedic patients: operating rooms protocols and recommendations in the current COVID-19 pandemic. J Am Acad Orthop Surg 2020. April 10 (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Farrell S, Schaeffer EK, Mulpuri K. Recommendations for the care of pediatric orthopedic patients during the COVID pandemic. J Am Acad Orthop Surg 2020. April 14 (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Piqueras M, Marco E, Coll M, et al. Effectiveness of an interactive virtual telerehabilitation system in patients after total knee arthoplasty: a randomized controlled trial. J Rehabil Med 2013;45:392-396. [DOI] [PubMed] [Google Scholar]
- 24. Russell TG, Buttrum P, Wootton R, Jull GA. Internet-based outpatient telerehabilitation for patients following total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg [Am] 2011;93-A:113-120. [DOI] [PubMed] [Google Scholar]
- 25. Koo KI, Park DK, Youm YS, Cho SD, Hwang CH. Enhanced reality showing long- lasting analgesia after total knee arthroplasty: prospective, randomized clinical trial. Sci Rep 2018;8:2343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chen M, Li P, Lin F. Influence of structured telephone follow-up on patient compliance with rehabilitation after total knee arthroplasty. Patient Prefer Adherence 2016;10:257-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kim S. The future of E-Learning in medical education: current trend and future opportunity. J Educ Eval Health Prof 2006;3:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lamba P. Teleconferencing in medical education: a useful tool. Australas Med J 2011;4:442-447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gilboy N, Tanabe T, Travers D, Rosenau AM. Emergency Severity Index (ESI): A triage tool for emergency department care, Version 4. Implementation Handbook 2012 Edition. AHRQ Publication No. 12-0014 Rockville, MD: Agency for Healthcare Research and Quality; November 2011. [Google Scholar]
- 30. Miyanji F, Slobogean GP, Samdani AF, et al. Is larger scoliosis curve magnitude associated with increased perioperative health-care resource utilization?: a multicenter analysis of 325 adolescent idiopathic scoliosis curves. J Bone Joint Surg [Am] 2012;94-A:809-813. [DOI] [PubMed] [Google Scholar]
- 31. Ahn H, Kreder H, Mahomed N, Beaton D, Wright JG. Empirically derived maximal acceptable wait time for surgery to treat adolescent idiopathic scoliosis. CMAJ 2011;183:E565-E570. [DOI] [PMC free article] [PubMed] [Google Scholar]


