Abstract
Purpose
The classic periacetabular osteotomy (PAO) approach can result in hip flexor weakness in adolescents. The rectus-sparing approach (PAO-RS) preserves the origin of the rectus femoris tendon which may prevent hip flexor weakness and improve functional outcome.
Methods
This is a prospective analysis of adolescents treated with a PAO or PAO-RS. The PAO group included 24 hips/21 patients (18 female, meanage 16 years (sd 4)); the PAO-RS group included ten hips (eight female, mean age 16 years (sd 1)). Preoperatively, the PAO group had decreased hip flexion strength compared with the PAO-RS group (83 Nm/kg versus 102 Nm/kg). A subset of PAO patients (n = 13 hips/12 patients, nine female, mean age 15 years (sd 3)) were matched for preoperative flexion strength to the PAO-RS group. Radiographic parameters, modified Harris hip score (mHHS), isokinetic hip strength and instrumented motion analysis preoperatively, six months and one-year postoperatively were compared.
Results
There were no differences in preoperative deformity, postoperative correction or degree of correction between groups. Hip flexor strength decreased significantly at six months in the PAO group compared with the PAO-RS group (-35 Nm/kg versus -7 Nm/kg; p = 0.012), as did hip flexion pull-off power (1.33 W/kg PAO versus 1.76 W/kg PAO-RS; p = 0.010). Hip flexion strength improved from six months to one year in the PAO group, with no significant differences in strength at one year between groups (80 Nm/kg versus 90 Nm/kg). There were no differences between groups in mHHS any time point; both groups improved significantly postoperatively.
Conclusion
Preserving the rectus femoris may lead to improved short-term hip flexor strength and pull-off power. Further assessment at long-term follow-up is needed to determine if this strength leads to improved functional outcomes.
Level of Evidence
II
Keywords: Rectus-sparing, periacetabular osteotomy, developmental dysplasia of the hip, flexion strength
Introduction
The Bernese periacetabular osteotomy (PAO) as described by Ganz et al1 has proven to be a reliable surgical technique for treating symptomatic acetabular dysplasia in skeletally mature patients. Multiple studies have demonstrated that the PAO can reproducibly restore anatomical acetabular orientation with patients reporting significant decrease in pain and improved function postoperatively and relatively few reported complications.2-14
The original description of the PAO includes a modified Smith-Peterson exposure with release of the direct and indirect heads of the rectus femoris tendon for complete visualization of the anterior hip capsule (with repair of the rectus tendon through bone at the end of the procedure).1 We have observed prolonged rehabilitation and delayed return to activities associated with the slow return of rectus strength. In a report from our institution, including 21 adolescent patients with symptomatic acetabular dysplasia evaluated at short-term (one year) follow-up after a PAO, we demonstrated that hip flexion strength was decreased at the six-month postoperative evaluation when compared with preoperatively and improved at the one-year postoperative evaluation, but it had not returned to the preoperative level.11 A similar trend was also observed with hip flexor pull-off power.11 Therefore, presented with these results, we adopted a rectus-sparing approach to the PAO.
Recent studies have evaluated a rectus-sparing approach to the PAO (no release of the indirect or direct head of the rectus tendons) with the goal of demonstrating improved postoperative pain control, quicker mobilization postoperatively, decreased length of stay, shorter surgical times and improved patient reported outcomes without compromising reorientation of the acetabulum.5,15 Both studies demonstrated that the rectus-sparing approach is safe and as effective as the original approach in achieving appropriate orientation of the acetabulum but with decreased surgical times. However, neither study included any strength testing.5,15
The purpose of the present study was to determine whether the use of the rectus-sparing approach was associated with return of preoperative hip flexion strength and hip pull-off power and improved self-reported patient outcomes at six months and/or 12 months postoperatively when compared with those undergoing a classic PAO approach.
Patients and methods
Study design and setting
This was an institutional review board approved analysis of a consecutive series of adolescents who were enrolled in a prospective outcomes registry for hip preservation at our institution between January 1999 and December 2014. Only patients treated with a standard Bernese PAO using a modified Smith-Peterson approach for symptomatic idiopathic acetabular dysplasia were included. The indications for surgery were hip pain with radiographic evidence of dysplasia. All patients had a minimum of one-year follow-up.
Participants/study subjects
There were 67 PAO-RS procedures performed at our institution between 2011 through 2014. Of these, 49 procedures were performed in patients with idiopathic hip dysplasia while the remaining were performed in patients with other associated conditions, such as cerebral palsy, Perthes disease, Charcot-Marie-Tooth disease and slipped capital femoral epiphysis. In all, 29 of the 49 hips were eligible for one-year follow-up at the time of analysis. Subsequently, two patients were excluded, one had a revision PAO performed on the ipsilateral side and the other had a surgical hip dislocation prior to the PAO to address intra-articular pathology. Of the remaining 27 hips, ten underwent instrumented gait analysis and strength testing preoperatively, at six months and one-year postoperatively and are the cohort of interest in this study. In all, 13 of the other 17 hips underwent testing preoperatively and at six months or one-year postoperatively. Four hips were not tested. An unpublished comparison of clinical results (preoperative radiographic measures, intraoperative findings and postoperative correction) in the ten included hips demonstrated no significant differences from the 17 hips that were not seen for gait analysis at appropriate time points.
The outcomes of the ten patients with pre- and postoperative gait analysis and strength testing and treated with the rectus-sparing approach (PAO-RS) were compared with 13 patients, also with pre- and postoperative gait analysis and strength testing, who were matched for preoperative hip strength and from the initial cohort of PAO patients (PAO), who have been previously reported.11 Based on the standard of care surgical procedures at the time of enrollment, both the PAO (prior to 2011) and PAO-RS (subsequent to 2011) represent a convenience sample of patients treated at a single institution.
Radiographic evaluation
Standard radiographic measurements, including the lateral centre-edge angle of Wiberg (LCEA)16 and acetabular index of the weight-bearing zone (AI) on the anteroposterior pelvis view and the ventral centre-edge angle (VCEA)17 on the false-profile on the affected hip, were analyzed at the preoperative and one-year postoperative evaluations to quantify the initial acetabular dysplasia and the correction achieved.
Gait analysis, strength testing, and self-reported functional scores
Hip flexion and abductor strength were measured using the Biodex System 3 isokinetic dynamometer (Biodex Medical Systems, Inc., Shirley, New York, USA) at 60 °/sec. Peak torque was a primary outcome measure of overall maximal strength and was normalized to body weight. Kinematic (Vicon Motion Systems Ltd, Centennial, Colorado, USA) and kinetic (Advanced Mechanical Technology Inc., Watertown, Massachusetts, USA) data were processed using the Plug-in-Gait model in Vicon Nexus. The primary gait analysis outcome was the peak hip flexion pull-off power near the transition from stance to swing, as this is a measure of functional strength during a main activity of daily living. Other secondary variables of interest included hip range of movement in the sagittal plane across the gait cycle. Patients were asked to complete the modified Harris hip score (mHHS). Hip strength and instrumented movement analysis preoperatively and at six months and one-year postoperatively.
Statistical analysis
Demographics and clinical variables were summarized with counts/percentages and means/sd where appropriate. Differences between the radiographic and gait parameters and the functional hip scores at the preoperative and follow-up evaluations were analyzed using a paired t-test and analysis of variance. Comparisons between groups were determined by independent samples t-tests. Data were checked for normality and equal variances.
Demographics and description of study population
The PAO group included 24 hips/21 patients (18 female) at an mean age at surgery of 16 years (sd 4); the PAO-RS group included ten hips (eight female) at an mean age at surgery of 16 years (sd 1). Preoperatively, the PAO group had decreased maximum hip flexion strength (83.1 (sd 33.9) Nm/kg versus 102.3 (sd 33.1) Nm/kg) compared with the PAO-RS group. Therefore, a subset of PAO patients (n = 13 hips/12 patients, nine female, mean age at surgery 15 years (sd 3)) was selected with matched preoperative maximum hip flexion strength to the PAO-RS group (100 (sd 26.3) Nm/kg versus 102.3 (sd 33.1) Nm/kg).
Results
There were no differences in preoperative deformity, postoperative correction or degree of correction between the matched-PAO and the PAO-RS groups (Table 1). Maximum hip flexor strength decreased significantly more at six months in the PAO group compared with the PAO-RS group (-34.7 (sd 27.3) Nm/kg versus -6.5 (sd 19.6) Nm/kg; p = 0.012). There was an improvement from six months to one year in the PAO group, resulting in no significant differences in maximum strength at one year between the PAO and PAO-RS groups (79.6 (sd 32.1) Nm/kg versus 90.1 (sd 41.2) Nm/kg; p = 0.495) (Table 2).
Table 1.
Comparison of variables and degree of correction between the matched periacetabular osteotomy (PAO) and rectus-sparing PAO (PAO-RS) cohorts. All values are given as mean (sd)
| Matched PAO (n = 13) | PAO-RS (n = 10) | p-value* | |
|---|---|---|---|
| Preoperative LCEA (°) | 7.7 (6.7) | 8.2 (5.5) | 0.847 |
| Preoperative AI (°) | 27.1 (5.5) | 24.9 (6.1) | 0.387 |
| Preoperative VCEA (°) | 2.2 (14.6) | 8.6 (10.6) | 0.280 |
| 1-yr LCEA(°) | 35.8 (9.4) | 30.8 (3.8) | 0.102 |
| 1-yr AI (°) | 8.8 (7.4) | 8.0 (3.3) | 0.742 |
| 1-yr VCEA (°) | 33.5 (11.5) | 28.4 (3.8) | 0.171 |
| Δ LCEA (°) | 28.1 (10.1) | 22.6 (2.9) | 0.084 |
| Δ AI (°) | −17.9 (5.9) | −16.9 (4.6) | 0.662 |
| Δ VCEA** (°) | 30.9 (12.1) | 20.1 (9.7) | 0.040 |
statistical analysis was performed using independent t-tests.
only 20 patients in the original cohort and 11 patients in the PAO-RS cohort had pre- to postoperative comparisons available for Δ VCEA.
LCEA, lateral centre-edge angle; AI, acetabular index; VCEA, ventral centre-edge angle.
Table 2.
Hip flexion strength. All values are given as mean (sd)
| Preoperative, Nm/kg | 6-mths postoperative, Nm/kg | 1-yr postoperative, Nm/kg | |
|---|---|---|---|
| PAO-RS | 102.3 (33.1) | 95.8 (42.9) | 90.1 (41.2) |
| PAO | 100.0 (26.3) | 65.3 (21.9) | 79.6 (32.1 |
| p-value* | ns | 0.037 | ns |
Statistical analysis was performed using independent t-tests.
PAO, periacetabular osteotomy; PAO-RS, periacetabular osteotomy with rectus-sparing approach; ns, not significant.
There were no differences between groups in sagittal hip range of movement during gait at any time point, and neither group demonstrated a significant change in range of movement pre- to postoperatively. Maximum hip flexion pull-off power (1.33 (sd 0.29) W/kg PAO versus 1.76 (sd 0.44) W/kg PAO-RS; p = 0.010) (Table 3; Fig. 1) and hip abductor moment-impulse (0.188 (sd 0.058) Nm/kg PAO versus 0.266 (sd 0.055) Nm/kg; p = 0.004) were significantly decreased at six months in the PAO group compared with the PAO-RS group. There were no differences between groups in mHHS (max 89) at any time point (matched PAO group: 67 (sd 9) to 79 (sd 8) to 75 (sd 12); RSA group: 63 (sd 11) to 71 (sd 13) to 79 (sd 8)) and both groups improved significantly pre- to postpostoperatively.
Table 3.
Hip flexion pull-off power. All values are given as mean (sd)
| Preoperative, W/kg | 6-mths postoperative, W/kg | 1-yr postoperative, W/kg | |
|---|---|---|---|
| PAO-RS | 1.39 (0.40) | 1.76 (0.44) | 1.91 (0.98) |
| PAO | 1.63 (0.60) | 1.33 (0.29) | 1.45 (0.49) |
| p-value* | ns | p = 0.010 | ns |
Statistical analysis was performed using independent t-tests.
PAO, periacetabular osteotomy; PAO-RS, periacetabular osteotomy with rectus-sparing approach; ns, not significant.
Fig. 1.
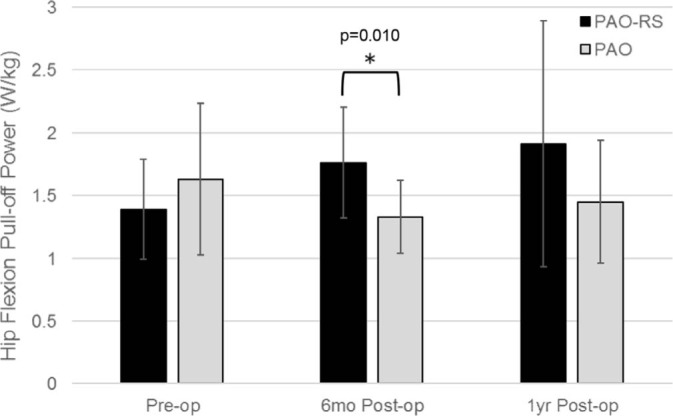
Hip flexion pull-off power was significantly decreased in the periacetabular osteotomy (PAO) group compared to the periacetabular osteotomy with rectus-sparing approach (PAO-RS) group (Pre-op, preoperative; Post-op, postoperative).
Discussion
Since the original description of the PAO,1 multiple modifications to the approach have been described in an attempt to decrease complications, decrease operative time, decrease length of stay postoperatively and increase patient function.7,18,19 Release of the indirect and direct heads of the rectus femoris tendon, as originally described, results in decreased hip flexion strength at six months and one year postoperatively when compared with preoperative strength.11 The rectus-sparing approach is safe and allows for unimpeded re-orientation of the acetabulum5,16 but there has been no previous study demonstrating the maintenance of hip flexion strength when using the approach. This study demonstrated that the rectus-sparing approach to the PAO preserves hip flexion strength in adolescents with hip dysplasia at six months postoperatively when compared with preoperatively and when compared with those who underwent the traditional approach.
This study does have several limitations. While all participants were enrolled into a single long-standing hip preservation registry, the two groups were recruited in series, not in parallel. The surgeries performed in the PAO group were earlier in our surgeons’ experience. Since the rectus-sparing approach was not introduced in our institution until 2011, our surgeons had approximately 10 to 12 years of PAO experience prior to implementing this change in technique. Clinical outcomes and intraoperative metrics, including operative time, blood loss and complications, have been shown to be similar between techniques by several other researchers.5,15 Unpublished analysis at our own institution revealed similar findings, and may suggest that surgeon experience is not a significant factor in this analysis.
The sample of the cohorts is small, however, this is due to the strict inclusion criteria that all patients needed to have appropriate clinical, radiographic and strength follow-up and no patient had a previous acetabular surgery or an underlying condition. A separate analysis, not included in the current report, found that the ten hips in the-PAO-RS group had similar radiographic and clinical outcomes as the 17 hips who were excluded for lack of gait analysis. In addition, a similar analysis indicated that the matched PAO group, selected from our previous published paper, was similar to those not included in the matched group, with the only difference being preoperative hip strength (how they were selected). Additionally, this report is limited to one-year follow-up, however, it is during this immediate postoperative period that the majority of the strength limitations/improvements are best assessed postoperatively.
Novais et al5 reported on 64 patients treated with a PAO, with half treated with the rectus-sparing approach. The authors noted that blood loss, haematocrit change and operative time were similar between the groups. The HHS also improved in both groups with no significant difference in the average change between the rectus-sparing and traditional PAO groups (25 versus 21). There was also no significant difference in the rate of complications (12.5% versus 25%) or improvement with respect to LCEA (19° versus 17°; p = 0.446), Tönnis angle (-14° versus -14°; p = 0.795) or the anterior centre edge angle (23° versus 17°; p = 0.093) between the rectus-sparing and the control group.5 Our study mirrors these results in that we were able to achieve the same radiographic correction in both groups and the mHHS were similar at follow-up.
In another report of young adult patients (age range 18 to 31 years), Peters et al15 compared the degree of acetabular orientation between patients who were treated with a standard PAO approach versus a modified rectus-sparing approach for acetabular dysplasia. They included 75 patients in the cohort, of which 44 were treated with a standard PAO and 31 patients were included in the rectus-sparing PAO group. The groups were similar in age and body mass index, although the rectus-sparing group had significantly higher percentage of male patients. The results indicated that patients who underwent a PAO with a rectus-sparing approach had less overall pain. The authors also reported that patients treated with the rectus-sparing approach ambulated similar distances during the hospital stay with a median 11 feet for the standard PAO group and 30 feet for the rectus-sparing group (p = 0.215). The patients in the standard PAO approach group did have a significantly greater postoperative hospital length of stay (median 4 days versus 3 days; p < 0.001), blood loss (median 500 mL versus 300 mL; p = 0.010) and surgical time (median 159.5 mins versus 103 mins; p < 0.001) than the patients in the rectus-sparing group. The percentage of patients to achieve desirable acetabular correction was not significantly different between the traditional PAO versus rectus-sparing PAO groups as defined by the AI (0°to 10°; 70% versus 81%; p = 0.321) or LCEA (20° to 35°; 82% versus 74%; p = 0.429). The percentage of patients achieving the desired anterior correction (VCEA 20° to 35°) was significantly higher in the rectus-sparing group compared with the traditional approach (77% versus 55%; p = 0.046). The authors concluded that the modified rectus-sparing approach did not compromise acetabular fragment mobilization or final positioning. Similar results were noted in our present study as patients in both the PAO-RS group and PAO group achieved similar radiographic correction and improvement in functional scores. However, our study is unique in that we are able to demonstrate improvement/maintenance of hip flexor strength at the six-month and one-year postoperative periods in the PAO-RS patients.
Conclusion
Preserving the rectus femoris when performing a PAO may be associated with an improved short-term conservation of hip flexor strength and hip flexion pull-off power. This may lead to greater return to activities in the early postoperative period and may provide for improved health-related quality of life and activity scores in the future. Further assessment at long-term follow-up is needed to determine if this strength leads to further improvement in functional outcomes.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
Ethical approval: Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research.
Informed consent: Informed consent for participation in the study was obtained.
ICMJE Conflict of interest statement
None declared.
Author Contributions
DAP: Study design, Data collection and analysis, Drafting and revision of manuscript.
KTF: Study design, Data collection and analysis, Drafting and revision of manuscript.
ADLR: Study design, Data collection and analysis, Drafting and revision of manuscript.
DC: Data collection and analysis.
DJS: Study design, Data collection and analysis, Drafting and revision of manuscript.
References
- 1. Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res 1988;232:26-36. [PubMed] [Google Scholar]
- 2. Thawrani D, Sucato DJ, Podeszwa DA, DeLaRocha A. Complications associated with the Bernese periacetabular osteotomy for hip dysplasia in adolescents. J Bone Joint Surg [Am] 2010;92-A:1707-1714. [DOI] [PubMed] [Google Scholar]
- 3. Czubak JB, Tyrakowski M, Pietrzk S. Periacetabular Ganz osteotomy in the treatment of hip dysplasia in adolescent and young adults with previous hip surgery in childhood. J Bone Joint Surg [Br] 2009;91-B:29. [Google Scholar]
- 4. Novais EN, Heyworth B, Murray K, et al. Physical activity level improves after periacetabular osteotomy for the treatment of symptomatic hip dysplasia. Clin Orthop Relat Res 2013;471:981-988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Novais EN, Kim YJ, Carry PM, Millis MB. The Bernese periacetabular osteotomy: is transection of the rectus femoris tendon essential? Clin Orthop Relat Res 2014;472:3142-3149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zaltz I, Baca G, Kim YJ, et al. Complications associated with the periacetabular osteotomy: a prospective multicenter study. J Bone Joint Surg [Am] 2014;96:1967-1974. [DOI] [PubMed] [Google Scholar]
- 7. Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy in the treatment of severe acetabular dysplasia. Surgical technique. J Bone Joint Surg [Am] 2006;88-A(suppl 1 Pt 1):65-83. [DOI] [PubMed] [Google Scholar]
- 8. De La Rocha A, Sucato DJ, Tulchin K, Podeszwa DA. Treatment of adolescents with a periacetabular osteotomy after previous pelvic surgery. Clin Orthop Relat Res 2012;470:2583-2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Murphy S, Deshmukh R. Periacetabular osteotomy: preoperative radiographic predictors of outcome. Clin Orthop Relat Res 2002;405:168-174. [PubMed] [Google Scholar]
- 10. Pedersen EN, Alkjaer T, Søballe K, Simonsen EB. Walking pattern in 9 women with hip dysplasia 18 months after periacetabular osteotomy. Acta Orthop 2006;77:203-208. [DOI] [PubMed] [Google Scholar]
- 11. Sucato DJ, Tulchin K, Shrader MW, et al. Gait, hip strength and functional outcomes after a Ganz periacetabular osteotomy for adolescent hip dysplasia. J Pediatr Orthop 2010;30:344-350. [DOI] [PubMed] [Google Scholar]
- 12. Trumble SJ, Mayo KA, Mast JW. The periacetabular osteotomy. Minimum 2 year followup in more than 100 hips. Clin Orthop Relat Res 1999;363:54-63. [PubMed] [Google Scholar]
- 13. Beaulé PE, Dowding C, Parker G, Ryu JJ. What factors predict improvements in outcomes scores and reoperations after the Bernese periacetabular osteotomy? Clin Orthop Relat Res 2015;473:615-622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zhu J, Chen X, Cui Y, Shen C, Cai G. Mid-term results of Bernese periacetabular osteotomy for developmental dysplasia of hip in middle aged patients. Int Orthop 2013;37:589-594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Peters CL, Erickson JA, Anderson MB, Anderson LA. Preservation of the rectus femoris origin during periacetabular osteotomy does not compromise acetabular reorientation. Clin Orthop Relat Res 2015;473:608-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wiberg G. Studies in dysplastic acetabulum and congenital subluxation of the hipjoint with special reference to the complication of osteoarthritis. Acta Chir Scand 1939;83:S58. [Google Scholar]
- 17. Lequesne M, Djian A. New radiographic angles for the study of the hip. The ‘false profile’ of the pelvis. Vie Med 1961;42:1629-1641. [PubMed] [Google Scholar]
- 18. Crockarell J Jr, Trousdale RT, Cabanela ME, Berry DJ. Early experience and results with the periacetabular osteotomy. The Mayo Clinic experience. Clin Orthop Relat Res 1999;363:45-53. [PubMed] [Google Scholar]
- 19. Hussell JG, Mast JW, Mayo KA, Howie DW, Ganz R. A comparison of different surgical approaches for the periacetabular osteotomy. Clin Orthop Relat Res 1999;363:64-72. [PubMed] [Google Scholar]


