Summary
Background
Rapid population growth, urbanisation, and economic development have led to an unprecedented number of waste sites in developing countries. This challenge has become a contentious international relations issue, with an unsustainable amount of waste and its health consequences often being borne by developing countries. However, little national-level evidence is available in sub-Saharan Africa to quantify the association between exposure to waste sites and health.
Methods
We used panel data from the South African National Income Dynamics Study (SA-NIDS) to investigate the association between exposure to waste sites and asthma, tuberculosis, diabetes, and depression. The SA-NIDS is a panel survey of a nationally representative sample in South Africa, which includes data reporting the health status of 32 255 individuals between 2008 and 2015. The study exposure was distance of households, in km, to the nearest waste site, derived from waste site geospatial locations from the South Africa Waste Information System.
Findings
We observed a substantial increase in exposure of households to waste sites between 2008 and 2015. The median distance between study households and waste sites decreased from 68·3 km (IQR 31·1–111·7) to 8·5 km (3·0–23·7). Residing within 5 km of a waste site was significantly associated with asthma (adjusted relative risk 1·41; 95% CI 1·20–1·64), tuberculosis (1·18; 1·02–1·36), diabetes (1·25; 1·05–1·49), and depression (1·08; 1·03–1·14). The association persisted even after controlling for multiple socioeconomic factors.
Interpretation
We identified multiple adverse health outcomes in individuals living close to waste sites at a national level in South Africa, suggesting the need to reduce the number and size of waste sites to diminish harmful effects on health and wellbeing for communities living in close proximity to such sites.
Funding
South African Medical Research Council, South African National Treasury, and Wellcome Trust.
Introduction
Considerable public attention is being paid to the challenges of waste management encountered by developing countries. Although high-income countries constitute only 16% of the global population, they disproportionately generate a third of the world's waste, estimated to be 683 million tonnes each year.1 In addition to this inequity in waste generation, developing countries are often recipients of waste that originates from developed countries. Although some of the waste generated, such as scrap, can potentially be advantageous for importing countries to gain access to cheaper raw materials and goods for manufacturing purposes, importing and hosting waste can also place them in a vulnerable position, if their health, safety, and environmental policies are weak or poorly implemented.2 In addition to the possible health and environment costs of importing waste in these countries, an estimated 11–19% of their municipal budgets are allocated towards their own waste management—a stark contrast to the average 4% in high-income countries.1
The challenges associated with the waste management across developing countries are expected to intensify, particularly in sub-Saharan Africa. The volume of waste, driven by unprecedented population growth and economic development in the region, is expected to place an additional burden on top of the existing challenges of addressing locally generated waste. By 2050, the volume of waste is projected to triple from 174 million tonnes per year in 2016 to 516 million tonnes per year across sub-Saharan Africa.1 Without waste minimisation or recovery implementation strategies in place, waste is either incinerated or deposited in landfill as the final resort, with approximately 69% of all waste being deposited in landfill across sub-Saharan Africa.1 South Africa is in the midst of a waste crisis, with the 2018 report by the South Africa Department of Environmental Affairs indicating that only 10% of waste is recycled, while the remaining estimated 98 million tonnes are deposited into landfills each year.3 The volume of waste is expected to reach unsustainable levels in the near future, with landfills for the country's large municipalities being projected to be full before 2025.4
Research in context.
Evidence before this study
We searched PubMed, MEDLINE, EBSCO, Sabinet Online, and Google and Google Scholar databases for studies and reports published before August, 2019, with a combination of search terms, including “waste” or “landfill” for exposure. For health outcomes, search terms included “respiratory”, “asthma”, “tuberculosis”, “diabetes”, “mental health”, “depression”, “depressive”, or “depressive symptoms”. We also expanded the search to include non-English publications. The growing population, urbanisation, and economic development in sub-Saharan Africa means production of more waste, with a greater number of people being at risk of exposure. Despite the potential health risks associated with waste exposure, evidence supporting this association is limited by the absence of panel population-based data that are generalisable at a national level in sub-Saharan Africa. Such evidence would contribute meaningfully to the sustainable development debate, and to national-level policy on the health benefits of waste reduction.
Added value of this study
Our study was based on data (2008–15) from the South African National Income Dynamics Study (SA-NIDS), with access to global positioning system (GPS) coordinates of study households from the DataFirst Secure Research Data Centre. The SA-NIDS is a panel survey of a nationally representative sample of households. We also obtained GPS coordinates of registered waste sites from the South Africa Waste Information System. Overlays of SA-NIDS households and GPS locations of waste sites permitted the use of spatial methods to investigate the association between exposure to waste sites and health at a national level in sub-Saharan Africa. Even after controlling for multiple socioeconomic factors, living in close proximity to waste sites (5 km distance) was significantly associated with asthma, tuberculosis, diabetes, and depression. Our results can inform national sustainable development policy in South Africa, and also highlight the need to reduce waste on a global level, and to reduce the transfer of waste to developing countries, to improve health and wellbeing.
Implications of all the available evidence
Our results have important implications for achieving multiple Sustainable Development Goal (SDG) targets by 2030, including managing and reducing the production of waste (SDG targets 12.4 and 12.5) and improving health by reducing the burden of asthma, tuberculosis, diabetes, and depression (SDG targets 3.3 and 3.4), in countries in sub-Saharan Africa that are undergoing rapid economic development and urbanisation (SDG target 11.6). Section 24 of the Constitution of South Africa guarantees the right to a healthy environment, and our results emphasise the importance of waste management to minimise adverse effects on human health and wellbeing more generally.
With the increasing projected level of waste in South Africa, exposure to waste sites, particularly poorly managed ones, has raised serious health concerns, particularly for individuals residing in the vicinity of such waste sites. A systematic review from Brazil shows various adverse health effects, such as physical and mental challenges, due to work exposure5 to so-called closed waste sites.6 The health issues associated with exposure to waste sites are not restricted to onsite exposure. Landfill sites, as one form of waste site, are a potential reservoir for rodents (eg, rats and mice), which can contribute to human respiratory diseases in nearby communities, such as asthma7 and hantavirus pulmonary syndrome,8 in addition to other diseases that can be caused indirectly by an intermediate vector.9 Air pollutants from waste sites, such as hydrogen sulfide emissions, can harm the respiratory system, which can not only lead to lung disease, such as asthma10 but also cause less obvious non-respiratory illnesses, such as diabetes,11 through exposure to polychlorinated biphenyls originating from hazardous waste sites.12 Groundwater contamination by landfill sites13 can also affect health outcomes.14
The link between exposure to waste sites and adverse health outcomes should not be limited to the abovementioned biomedical mechanisms with a narrow focus on individual agents. The structural and social determinants of health linked to waste exposure15 also need acknowledgment. Polluting facilities, from a neoclassical economic perspective, are often spatially located in areas near socioeconomically vulnerable communities16 because of the lower property values (ie, lower cost of housing), and business costs.17 Another perspective, the political ecology of environmental inequity, which contends that unequal social power relationships are a cause of environmental injustice,18 should also be acknowledged. In South Africa, before the democratic transition in 1994, non-white people were dispossessed of their land and forcibly moved to sites that were racially designated, often at urban outskirts, which were near areas with industrial activities, such as factories, airports, and landfill sites (due to the 1913 Natives Land Act19). The spatial planning policies extended to environmental racism, where non-white communities were situated adjacent to waste sites.20 To date, rectifying forced migration from, and struggle for tenure on, what was once productive land is an economic and psychological issue that speaks to the dignity of dispossessed communities, as noted in Section 10 of the 1996 Constitution of South Africa21 on Human Dignity: “Everyone has inherent dignity and the right to have their dignity respected and protected.” Despite the diversity of waste products, the danger posed by certain landfill gases lasts for decades,22 specifically for those living in close proximity to such sites and who had little choice as to where they could live in pre-democratic South Africa. The enduring effects of racist environmental policies, inherited from the apartheid regime, cannot be dismissed. Although tuberculosis is not exclusively a respiratory disease, and might seem unrelated to air pollution from waste sites from a biomedical perspective, the disease is often driven by poverty and poor living conditions (eg, overcrowding, poorly ventilated housing, stress, and malnutrition),23 which occur in impoverished, peri-urban communities.24 Furthermore, a review of perceptions and attitudes towards waste treatment facilities suggests that concerns related to waste treatment sites included odour, traffic, pollution, and property devaluation, which can have a psychological impact on communities living near such sites.25
South Africa is challenged by persistent poverty coupled with one of the highest inequality rates in the world.26 The cost of pollution27 from poorly managed waste sites that affect the health of nearby inhabitants, who have no control over their circumstances, is a typical example of the negative environmental externalities that further undermine the dignity and equitable aspirations of sustainable development in South Africa, including redress for past discrimination. Many diseases, such as asthma, diabetes, and depression, can have deadly consequences when left untreated, yet are often neglected when compared with other public health problems in South Africa, such as the HIV and tuberculosis epidemic. Although reliable nationwide data are scarce, estimates suggest that one in 20 adults have asthma, and age-adjusted asthma death rates are among the highest in the world, according to the 2018 Global Asthma Report.28 Despite being treatable, tuberculosis remains the top cause of death (6·5% of all deaths in 2016) in South Africa, followed by diabetes (5·5% of all deaths in 2016), according to the latest data from Statistics South Africa.29 Lastly, depression, a serious health condition that affects 9·8% of South Africans in their lifetime,30 and is a leading cause of disability globally,31 is understood to have the highest negative impact on productivity among all medical conditions.32 It is also a major impediment to development, with workplace-related economic loss from depression being estimated to be 4·9% of gross domestic product (GDP).33 More importantly, the impact of an unhealthy environment, such as exposure to waste sites, on depression, also has to be placed in the context of human rights, as prescribed in the Constitution of South Africa and many other nations. Section 24 of the Constitution of South Africa states: “Everyone has the right—(a) to an environment that is not harmful to their health or wellbeing; (b) to have the environment protected, for the benefit of present and future generations, through reasonable legislative and other measures that—(i) prevent pollution and ecological degradation…”21 The 1996 Constitution of South Africa also places human dignity and equality at the centre of national founding values. Although we acknowledge that human dignity and mental wellness are not equivalent, it is plausible that the dignity of people, and subsequently mental wellbeing, can be diminished when the constitutional right to a healthy environment is not achieved.
Achieving the targets of the UN Sustainable Development Goals34 (SDGs) by 2030, which include ending the tuberculosis epidemic and reducing the global burden of asthma, diabetes, and depression (targets 3.3 and 3.4), is unlikely in South Africa, and elsewhere in sub-Saharan Africa, without addressing the considerable challenges of waste production and management (SDG targets 12.4 and 12.5) that are fuelled by urbanisation (SDG targets 11.6), population growth, and economic development.9, 35, 36, 37 Despite these global goals, to the best of our knowledge there are no national-level evidence-based studies in sub-Saharan Africa, including in South Africa, that have explored the health effects of living near waste sites. The available evidence is controversial, with systematic reviews often showing detrimental health effects of living near waste sites.38, 39 At least one systematic review also highlighted the role of pollution-mitigating technology for waste management and disposal that contributes to inconsistencies in the association between the health effects associated with, and the disposal of solid waste in, landfills and incinerators.40 Furthermore, studies included in the systematic review by Mattiello and colleagues40 were mainly from developing countries (with the exception of Brazil and Colombia), indicating a gap in knowledge about any association between health and waste site exposure in sub-Saharan Africa. In the current study, this gap was addressed by investigating the various health risks associated with proximity to waste sites, primarily (but not exclusively) focusing on respiratory and respiratory-related diseases, and mental health outcomes. The study is based on the South African National Income Dynamics Study (SA-NIDS), a unique and nationally representative panel data set designed to enable the monitoring of socioeconomic factors and the health of households or individuals over time, with the geographical coordinates of each household. This dataset permits the use of spatial methods to quantify the association between exposure to waste sites and respiratory diseases, and other non-communicable diseases, at a national level.
Methods
Study design
For this geospatial analysis we used data from SA-NIDS from wave 1 (2008), wave 2 (2010), wave 3 (2012), and wave 4 (2015). The SA-NIDS is the first panel survey of a nationally representative sample of households and provides unique insights into population trends in health and wellbeing on a scale that is seldom investigated in sub-Saharan Africa. The detailed SA-NIDS study design is described in a published report.41 Briefly, SA-NIDS uses a stratified, two-stage cluster sample design to obtain a nationally representative sample of households. Of the 3000 primary sampling units (PSUs), 400 were selected from Statistics South Africa's master sample for inclusion, and were proportionally allocated on the basis of 53 district councils in the first stage of the study. In the next stage, clusters of dwelling units were systematically sampled within each PSU, with two clusters of 12 dwelling units being selected from each. All consenting resident household adult members at the selected dwelling units were administered the SA-NIDS Adult questionnaire once written informed consent had been obtained. The use of SA-NIDS data was approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee (BE 111/14).
Outcomes
The main study outcomes were self-reported asthma, tuberculosis, diabetes, and depression. With the exception of depression, study participants were asked whether they were informed by doctors, nurses, or health-care professionals, to have any of the abovementioned diseases. Information about depression was obtained from the ten-item abridged version of the Center for Epidemiologic Studies Depression Scale (CES-D), which was included in the SA-NIDS Adult questionnaire. As a commonly used valid and reliable psychometric instrument,42, 43 the CES-D captures self-reported depression-associated symptoms during the past week. Each of the items in the CES-D has four possible responses in a Likert format, that ranges from 0 (rarely or none of the time; less than 1 day) to 3 (almost or all of the time; 5–7 days). A total score of 10 or greater, based on the composite score of the ten items (Cronbach's α=0·75), was the cutoff to signify significant depressive symptoms, consistent with a previous study.43
Exposures
Distance to the nearest waste site was the main exposure variable of the study. To ensure broad policy implications about the health consequences associated with waste, we included wide-ranging types of facilities deemed waste sites. These included waste disposal or storage (both general and hazardous), treatment (including incineration), recovery and composting, transfer stations, remediation of contaminated land, and other facilities involved in extraction and flaring of landfill gas. We calculated the exact ellipsoid distance between each study participant's household and their nearest waste site.44 Household geographic position system (GPS) coordinates were accessed from the DataFirst's Secure Data Centre at University of Cape Town, whereas the publicly available GPS coordinates of waste sites were obtained from the South Africa Waste Information System (SAWIS),45 provided by the South Africa Department of Environmental Affairs. Any person conducting any waste activity (both general and hazard) listed in the Annex 1 of the National Waste Information Regulations46 (generation, recovery or recycling, treatment, disposal, and exportation of waste) is required to register on the SAWIS. The nearest waste site and the ellipsoidal distance from the households were identified and calculated by use of ArcGIS software by Esri, version 10.3. Distance to the waste site from the SA-NIDS households was subsequently analysed in three different ways, with one continuous and two categorical approaches that assessed threshold distances for those living near waste sites: natural logarithm of distance, residing inside and outside 10 km of waste sites, and residing inside and outside 5 km of waste sites (5 km was chosen on the basis of previous work47).
Statistical analysis
First, we summarised participants' baseline sociodemographic and clinical details using a descriptive analysis. Second, we quantified the household distance to waste sites from 2008 to 2015. Third, we investigated the relationship between distance to waste site and disease outcomes. For each of the disease outcomes of asthma, tuberculosis, diabetes, and depression, we fitted three separate generalised estimating equation (GEE) regression models, given the repeated measurements of the SA-NIDS panel data structure. Distance to waste sites from the SA-NIDS households was analysed in three different ways as mentioned above. We therefore fitted three regression models (models 1–3) against each disease status outcome. Each regression model was further adjusted for sociodemographic variables available in SA-NIDS (eg, sex, race or ethnicity, age category, marital status, educational attainment, employment status, household income, and residence). Analyses involving proportions and regressions were adjusted by post-stratification weight to allow the results to better represent the contemporary South African population. Further details about the construction of post-stratification weights by the SA-NIDS have been published elsewhere.48
Role of the funding source
The funders of the study were not involved in data collection, data analysis, data interpretation, study design, participant recruitment, or any aspect pertinent to the study. The funders had no role in the writing of the manuscript or in the decision to submit it for publication. The corresponding author had the final responsibility for the decision to submit for publication.
Results
32 255 individuals participated in the SA-NIDS study at least once between 2008 and 2015; of these, 15 630 participated in 2008 (table 1). 9338 (56·0%) were female, 12 272 (78·8%) were Black African, and 7723 (52·4%) were aged younger than 35 years. The prevalence at baseline of the investigated diseases was 3·5% for asthma, 3·6% for tuberculosis, 3·5% for diabetes, and 21·7% for depression.
Table 1.
Baseline sociodemographic andclinical characteristics of SA-NIDS study participants
| Number of participants | |
|---|---|
| Sex | |
| Male | 6292 (44·0%) |
| Female | 9338 (56·0%) |
| Race or ethnicity | |
| African | 12 272 (78·8%) |
| Coloured* | 2220 (8·2%) |
| Asian or Indian | 224 (2·4%) |
| White | 914 (10·6%) |
| Age category | |
| 15–19 years | 2725 (16·3%) |
| 20–24 years | 2062 (13·3%) |
| 25–29 years | 1573 (12·0%) |
| 30–34 years | 1363 (10·8%) |
| 35–64 years | 6342 (40·6%) |
| ≥65 years | 1547 (7·0%) |
| Marital status | |
| Married | 4365 (31·5%) |
| Living with partner | 1398 (9·2%) |
| Widow or widower | 1388 (6·9%) |
| Divorced or separated | 417 (3·3%) |
| Never married | 8002 (49·0%) |
| Education | |
| Less than high school | 2085 (8·7%) |
| Completed high school | 10 039 (61·7%) |
| Beyond high school | 3506 (29·6%) |
| Employment status | |
| Not employed | 2085 (56·8%) |
| Employed | 13 545 (43·2%) |
| Household income | |
| Lowest 20% | 3000 (17·5%) |
| Low and middle 20% | 3494 (17·9%) |
| Middle 20% | 3417 (19·0%) |
| Middle and high 20% | 3447 (22·6%) |
| Highest 20% | 2272 (23·1%) |
| Residence | |
| Rural | 8031 (37·7%) |
| Urban formal | 6662 (53·1%) |
| Urban informal | 937 (9·3%) |
| Asthma | |
| No | 14 965 (96·5%) |
| Yes | 561 (3·5%) |
| Tuberculosis | |
| No | 14 856 (96·4%) |
| Yes | 696 (3·6%) |
| Diabetes | |
| No | 14 920 (96·5%) |
| Yes | 607 (3·5%) |
| Depression | |
| No | 10 275 (78·3%) |
| Yes | 5288 (21·7%) |
SA-NIDS=South African National Income Dynamics Study.
The term “coloured” is used by Statistics South Africa,49 and is a South African ethnic label that includes children or descendants from Black-White, Black-Asian, Black-Coloured, and White-Asian unions.50 Percentages are adjusted on the basis of post-stratification weight to better match population estimates produced by Statistics South Africa.
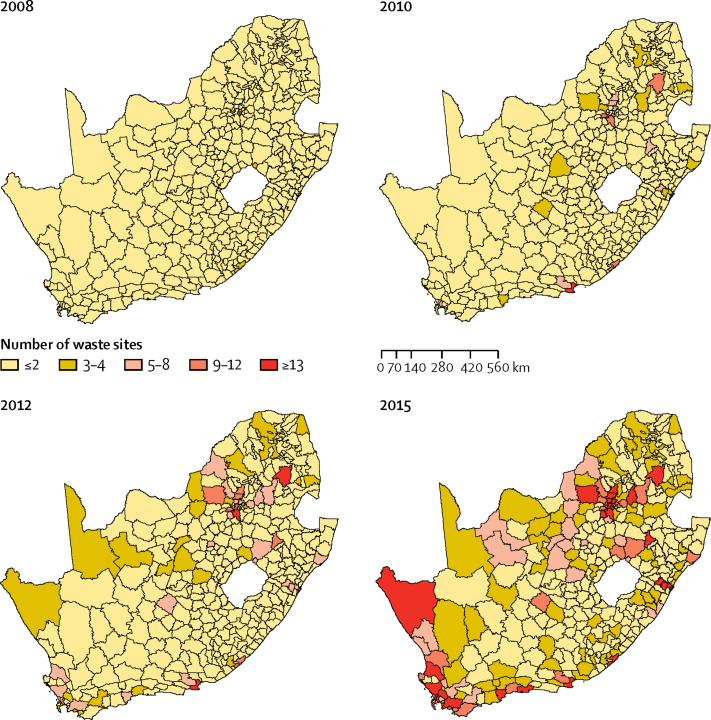
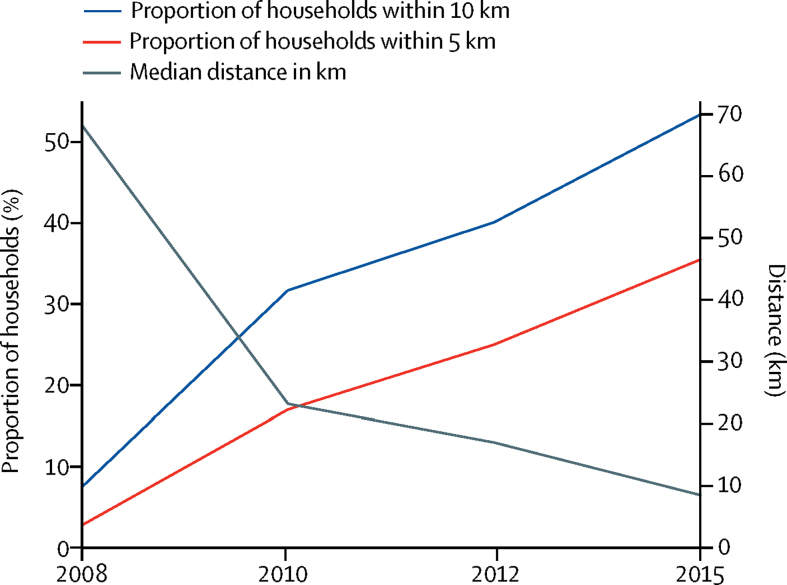
42 waste sites were observed in 2008, 280 in 2010, 519 in 2012, and 1086 in 2015. Figure 1 shows the density of waste sites, including the rapid increase in the density of waste sites in South Africa over time. With this growing waste site density, the distance between the SA-NIDS households and waste sites became shorter in each assessment period (figure 2). For example, the median distance in 2008, as a continuous measure, was 68·3 km (IQR 31·1–111·7), whereas by 2015 the median distance between SA-NIDS households and waste sites decreased to 8·5 km (3·0–23·7), signifying an 87·6% reduction in median distance. During the same period, the number of SA-NIDS households sampled grew by 32·4%, from 7274 in 2008 to 10 814 in 2015. The maximum distance between households and the nearest waste site was 488·9 km in 2008 and 201·9 km in 2015. In terms of finite distance, 2·8% of SA-NIDS households were within 5 km distance of a waste site in 2008, an estimate that rose to approximately 35·5% of all SA-NIDS households in 2015. More than half (53·4%) of SA-NIDS households were within 10 km of a waste site by 2015.
Figure 1.
Density of waste sites in South Africa (2008–15)
Maps were created using ArcGIS software by Esri, version 10.3.
Figure 2.
Exposure to waste sites between 2008 and 2015 in SA-NIDS households
SA-NIDS=South African National Income Dynamics Study.
The associations between distance to waste sites and disease outcomes (tuberculosis, diabetes, asthma, and depression), based on the GEE models, are summarised in Table 2, Table 3, Table 4, Table 5. The adjusted regression indicated that a greater distance, as a continuous measure (model 1 from Table 2, Table 3, Table 4, Table 5), between waste sites and SA-NIDS households, was significantly associated with lower asthma (adjusted relative risk [RR] 0·94; 95% CI 0·89–0·99), tuberculosis (0·95; 0·91–0·99), and diabetes (0·92; 0·87–0·98), but not with depression. When treated as a categorical measure (threshold distance), study participants residing within 10 km of waste sites had an increased risk of asthma (adjusted RR 1·28; 95% CI 1·08–1·51) and diabetes (1·19; 95% CI 1·02–1·40), as illustrated in model 2 from Table 2, Table 3, Table 4, Table 5. Study participants residing within a 5 km threshold distance from waste sites (model 3 from Table 2, Table 3, Table 4, Table 5) were at increased risk of asthma (adjusted RR 1·41; 95% CI 1·20–1·64), tuberculosis (1·18; 95% CI 1·02–1·36), diabetes (1·25; 1·05–1·49), and depression (1·08; 1·03–1·14).
Table 2.
Adjusted regression models on asthma outcome
|
Model 1: log km |
Model 2: within or outside 10 km |
Model 3: within or outside 5 km |
|||||
|---|---|---|---|---|---|---|---|
| Adjusted RR (95% CI) | p value | Adjusted RR (95% CI) | p value | Adjusted RR (95% CI) | p value | ||
| Distance | 0·94 (0·89–0·99) | 0·020 | 1·28 (1·08–1·51) | 0·0045 | 1·41 (1·20–1·64) | <0·0001 | |
| Sex | |||||||
| Male | .. | .. | .. | .. | .. | ||
| Female | 1·51 (1·21–1·89) | 0·0003 | 1·51 (1·21–1·89) | 0·0003 | 1·51 (1·21–1·89) | 0·0003 | |
| Population group | |||||||
| White | .. | .. | .. | .. | .. | .. | |
| African | 0·38 (0·25–0·56) | <0·0001 | 0·34 (0·23–0·51) | <0·0001 | 0·34 (0·23–0·50) | <0·0001 | |
| Coloured | 0·66 (0·42–1·03) | 0·064 | 0·59 (0·38–0·91) | 0·017 | 0·57 (0·37–0·88) | 0·011 | |
| Asian or Indian | 1·01 (0·54–1·89) | 0·98 | 0·93 (0·50–1·74) | 0·83 | 0·93 (0·50–1·71) | 0·81 | |
| Age category | |||||||
| 15–19 years | .. | .. | .. | .. | .. | .. | |
| 20–24 years | 1·47 (1·12–1·92) | 0·0049 | 1·57 (1·19–2·08) | 0·0014 | 1·58 (1·20–2·09) | 0·0012 | |
| 25–29 years | 1·07 (0·76–1·49) | 0·71 | 1·11 (0·79–1·55) | 0·54 | 1·10 (0·79–1·53) | 0·59 | |
| 30–34 years | 1·09 (0·77–1·55) | 0·62 | 1·10 (0·77–1·56) | 0·60 | 1·09 (0·77–1·55) | 0·63 | |
| 35–64 years | 1·47 (1·04–2·06) | 0·028 | 1·54 (1·09–2·16) | 0·014 | 1·52 (1·08–2·13) | 0·017 | |
| ≥65 years | 1·30 (0·85–2·00) | 0·23 | 1·45 (0·95–2·22) | 0·085 | 1·45 (0·95–2·20) | 0·084 | |
| Marital status | |||||||
| Single | .. | .. | .. | .. | .. | .. | |
| Living with partner | 1·16 (0·86–1·57) | 0·34 | 1·14 (0·84–1·55) | 0·39 | 1·13 (0·83–1·52) | 0·44 | |
| Widow or widower | 1·17 (0·89–1·54) | 0·27 | 1·15 (0·87–1·53) | 0·32 | 1·16 (0·88–1·53) | 0·28 | |
| Divorced or separated | 1·22 (0·75–1·99) | 0·42 | 1·15 (0·71–1·89) | 0·57 | 1·18 (0·72–1·92) | 0·51 | |
| Never married | 1·14 (0·89–1·47) | 0·31 | 1·15 (0·88–1·48) | 0·30 | 1·14 (0·89–1·48) | 0·30 | |
| Highest educational attainment | |||||||
| High school not completed | .. | .. | .. | .. | .. | .. | |
| Completed high school | 0·78 (0·58–1·04) | 0·089 | 0·81 (0·60–1·08) | 0·15 | 0·81 (0·61–1·08) | 0·15 | |
| Beyond high school | 0·54 (0·39–0·76) | 0·0004 | 0·53 (0·38–0·75) | 0·0003 | 0·53 (0·38–0·75) | 0·0002 | |
| Employment status | |||||||
| Unemployed | .. | .. | .. | .. | .. | .. | |
| Employed | 0·94 (0·78–1·12) | 0·48 | 0·91 (0·76–1·08) | 0·28 | 0·91 (0·76–1·09) | 0·29 | |
| Household income quintile | |||||||
| 1 (lowest) | .. | .. | .. | .. | .. | .. | |
| 2 | 1·02 (0·85–1·23) | 0·82 | 0·97 (0·80–1·19) | 0·79 | 0·98 (0·81–1·20) | 0·86 | |
| 3 | 1·17 (0·97–1·41) | 0·10 | 1·11 (0·94–1·31) | 0·22 | 1·12 (0·95–1·33) | 0·19 | |
| 4 | 1·11 (0·91–1·34) | 0·32 | 1·04 (0·83–1·31) | 0·71 | 1·06 (0·85–1·33) | 0·58 | |
| 5 (highest) | 1·10 (0·86–1·41) | 0·44 | 1·06 (0·78–1·43) | 0·73 | 1·07 (0·80–1·43) | 0·63 | |
| Residential area | |||||||
| Rural | .. | .. | .. | .. | .. | .. | |
| Urban formal | 1·51 (1·26–1·80) | <0·0001 | 1·46 (1·22–1·75) | <0·0001 | 1·44 (1·20–1·73) | 0·0001 | |
| Urban informal | 0·99 (0·74–1·32) | 0·93 | 0·93 (0·69–1·26) | 0·66 | 0·95 (0·71–1·27) | 0·73 | |
The term “coloured” is used by Statistics South Africa,49 a South African ethnic label that includes children and descendants from black-white, black-Asian, black-coloured, and white-Asian unions.50 The regression model adjusted based on post-stratification weight (from final observation of the individual panel) to reflect more recent population estimates produced by Statistics South Africa. RR=relative risk.
Table 3.
Adjusted regression models on tuberculosis outcome
|
Model 1: log km |
Model 2: within or outside 10 km |
Model 3: within or outside 5 km |
|||||
|---|---|---|---|---|---|---|---|
| Adjusted RR (95% CI) | p value | Adjusted RR (95% CI) | p value | Adjusted RR (95% CI) | p value | ||
| Distance | 0·95 (0·91–0·99) | 0·026 | 1·28 (0·90–1·19) | 0·61 | 1·18 (1·02–1·36) | 0·024 | |
| Sex | |||||||
| Male | .. | .. | .. | .. | .. | .. | |
| Female | 0·78 (0·67–0·90) | 0·0007 | 0·77 (0·67–0·89) | 0·0004 | 0·77 (0·67–0·89) | 0·0005 | |
| Population group | |||||||
| White | .. | .. | .. | .. | .. | .. | |
| African | 12·62 (5·71–27·89) | <0·0001 | 13·38 (6·06–29·55) | <0·0001 | 13·37 (6·05–29·54) | <0·0001 | |
| Coloured | 14·56 (6·53–32·47) | <0·0001 | 15·70 (7·05–34·97) | <0·0001 | 15·63 (7·02–34·81) | <0·0001 | |
| Asian or Indian | 1·44 (0·36–5·76) | 0·60 | 1·55 (0·39–6·18) | 0·54 | 1·55 (0·39–6·20) | 0·53 | |
| Age category | |||||||
| 15–19 years | .. | .. | .. | .. | .. | .. | |
| 20–24 years | 2·03 (1·44–2·87) | 0·0001 | 2·09 (1·47–2·96) | <0·0001 | 2·07 (1·46–2·94) | <0·0001 | |
| 25–29 years | 4·77 (3·42–6·66) | <0·0001 | 4·95 (3·54–6·92) | <0·0001 | 4·90 (3·50–6·85) | <0·0001 | |
| 30–34 years | 8·03 (5·65–11·39) | <0·0001 | 8·18 (5·75–11·63) | <0·0001 | 8·07 (5·68–11·48) | <0·0001 | |
| 35–64 years | 9·84 (7·09–13·66) | <0·0001 | 10·15 (7·30–14·12) | <0·0001 | 10·03 (7·22–13·94) | <0·0001 | |
| ≥65 years | 6·25 (4·27–9·16) | <0·0001 | 6·46 (4·40–9·48) | <0·0001 | 6·39 (4·35–9·38) | <0·0001 | |
| Marital status | |||||||
| Single | .. | .. | .. | .. | .. | .. | |
| Living with partner | 1·40 (1·13–1·74) | 0·0023 | 1·40 (1·12–1·74) | 0·0026 | 1·40 (1·13–1·74) | 0·0023 | |
| Widow or widower | 1·16 (0·93–1·45) | 0·19 | 1·17 (0·93–1·46) | 0·18 | 1·16 (0·93–1·45) | 0·19 | |
| Divorced or separated | 1·32 (0·97–1·80) | 0·078 | 1·32 (0·97–1·80) | 0·075 | 1·32 (0·97–1·80) | 0·080 | |
| Never married | 1·62 (1·35–1·95) | <0·0001 | 1·65 (1·37–1·98) | <0·0001 | 1·65 (1·37–1·98) | <0·0001 | |
| Highest educational attainment | |||||||
| High school not completed | .. | .. | .. | .. | .. | .. | |
| Completed high school | 0·96 (0·79–1·16) | 0·65 | 0·97 (0·80–1·17) | 0·75 | 0·96 (0·80–1·17) | 0·70 | |
| Beyond high school | 0·57 (0·43–0·76) | 0·0001 | 0·59 (0·44–0·78) | 0·0002 | 0·58 (0·44–0·77) | 0·0002 | |
| Employment status | |||||||
| Unemployed | .. | .. | .. | .. | .. | .. | |
| Employed | 0·82 (0·72–0·93) | 0·0024 | 0·83 (0·73–0·94) | 0·0035 | 0·83 (0·73–0·94) | 0·0029 | |
| Household income quintile | |||||||
| 1 (lowest) | .. | .. | .. | .. | .. | .. | |
| 2 | 0·87 (0·75–1·00) | 0·049 | 0·86 (0·75–0·99) | 0·036 | 0·86 (0·75–0·99) | 0·041 | |
| 3 | 0·82 (0·70–0·97) | 0·017 | 0·82 (0·70–0·97) | 0·019 | 0·83 (0·70–0·97) | 0·021 | |
| 4 | 0·80 (0·68–0·94) | 0·0064 | 0·79 (0·67–0·92) | 0·0035 | 0·79 (0·67–0·93) | 0·0044 | |
| 5 (highest) | 0·64 (0·52–0·78) | <0·0001 | 0·63 (0·52–0·77) | <0·0001 | 0·63 (0·52–0·77) | <0·0001 | |
| Residential area | |||||||
| Rural | .. | .. | .. | .. | .. | .. | |
| Urban formal | 0·95 (0·82–1·11) | 0·52 | 1·00 (0·86–1·17) | 0·97 | 0·96 (0·82–1·12) | 0·62 | |
| Urban informal | 1·09 (0·87–1·38) | 0·45 | 1·15 (0·91–1·46) | 0·25 | 1·10 (0·87–1·39) | 0·43 | |
The term “coloured” is used by Statistics South Africa,49 a South African ethnic label that includes children and descendants from black-white, black-Asian, black-coloured, and white-Asian unions.50 The regression model is adjusted on the basis of post-stratification weight (from final observation of the individual panel) to reflect more recent population estimates produced by Statistics South Africa. RR=relative risk.
Table 4.
Adjusted regression models on diabetes outcome
|
Model 1: log km |
Model 2: within or outside 10 km |
Model 3: within or outside 5 km |
|||||
|---|---|---|---|---|---|---|---|
| Adjusted RR (95% CI) | p value | Adjusted RR (95% CI) | p value | Adjusted RR (95% CI) | p value | ||
| Distance | 0·92 (0·87–0·98) | 0·0047 | 1·19 (1·02–1·40) | 0·032 | 1·25 (1·05–1·49) | 0·013 | |
| Sex | |||||||
| Male | .. | .. | .. | .. | .. | .. | |
| Female | 1·20 (0·97–1·47) | 0·088 | 1·19 (0·97–1·46) | 0·10 | 1·19 (0·97–1·47) | 0·093 | |
| Population group | |||||||
| White | .. | .. | .. | .. | .. | .. | |
| African | 0·98 (0·62–1·57) | 0·95 | 0·96 (0·61–1·50) | 0·85 | 0·94 (0·60–1·46) | 0·77 | |
| Coloured | 1·08 (0·63–1·85) | 0·77 | 1·03 (0·62–1·73) | 0·90 | 1·01 (0·61–1·69) | 0·96 | |
| Asian or Indian | 1·82 (1·06–3·15) | 0·031 | 1·80 (1·05–3·07) | 0·031 | 1·76 (1·03–3·00) | 0·038 | |
| Age category | |||||||
| 15–19 years | .. | .. | .. | .. | .. | .. | |
| 20–24 years | 1·15 (0·49–2·66) | 0·75 | 1·53 (0·58–4·05) | 0·39 | 1·52 (0·58–4·01) | 0·40 | |
| 25–29 years | 2·20 (0·80–6·07) | 0·13 | 2·39 (0·85–6·74) | 0·10 | 2·40 (0·86–6·73) | 0·096 | |
| 30–34 years | 4·13 (1·37–12·43) | 0·012 | 4·35 (1·42–13·31) | 0·010 | 4·33 (1·42–13·17) | 0·0098 | |
| 35–64 years | 12·30 (4·65–32·50) | <0·0001 | 13·02 (4·80–35·32) | <0·0001 | 12·85 (4·75–34·74) | <0·0001 | |
| ≥65 years | 19·28 (7·11–52·33) | <0·0001 | 19·97 (7·19–55·50) | <0·0001 | 19·62 (7·08–54·39) | <0·0001 | |
| Marital status | |||||||
| Single | .. | .. | .. | .. | .. | .. | |
| Living with partner | 0·53 (0·35–0·81) | 0·0028 | 0·53 (0·35–0·80) | 0·0023 | 0·53 (0·36–0·80) | 0·0022 | |
| Widow or widower | 1·01 (0·84–1·22) | 0·90 | 1·02 (0·84–1·23) | 0·87 | 1·01 (0·84–1·22) | 0·88 | |
| Divorced or separated | 0·91 (0·49–1·68) | 0·76 | 0·91 (0·49–1·67) | 0·75 | 0·92 (0·50–1·68) | 0·78 | |
| Never married | 0·60 (0·48–0·75) | <0·0001 | 0·61 (0·48–0·76) | <0·0001 | 0·61 (0·48–0·76) | <0·0001 | |
| Highest educational attainment | |||||||
| High school not completed | .. | .. | .. | .. | .. | .. | |
| Completed high school | 0·93 (0·77–1·12) | 0·47 | 0·95 (0·79–1·14) | 0·56 | 0·95 (0·79–1·14) | 0·56 | |
| Beyond high school | 0·60 (0·42–0·85) | 0·0047 | 0·60 (0·42–0·85) | 0·0044 | 0·60 (0·42–0·85) | 0·0043 | |
| Employment status | |||||||
| Unemployed | .. | .. | .. | .. | .. | .. | |
| Employed | 0·86 (0·73–1·01) | 0·061 | 0·84 (0·72–0·98) | 0·030 | 0·84 (0·72–0·98) | 0·032 | |
| Household income quintile | |||||||
| 1 (lowest) | .. | .. | .. | .. | .. | .. | |
| 2 | 1·10 (0·93–1·29) | 0·27 | 1·10 (0·94–1·29) | 0·25 | 1·11 (0·94–1·30) | 0·21 | |
| 3 | 1·37 (1·14–1·63) | 0·0006 | 1·39 (1·16–1·65) | 0·0003 | 1·40 (1·17–1·67) | 0·0002 | |
| 4 | 1·45 (1·21–1·73) | <0·0001 | 1·46 (1·22–1·75) | <0·0001 | 1·48 (1·24–1·76) | <0·0001 | |
| 5 (highest) | 1·36 (1·09–1·70) | 0·0063 | 1·41 (1·12–1·77) | 0·0034 | 1·42 (1·13–1·77) | 0·0023 | |
| Residential area | |||||||
| Rural | .. | .. | .. | .. | .. | .. | |
| Urban formal | 1·35 (1·13–1·63) | 0·0012 | 1·36 (1·13–1·64) | 0·0013 | 1·36 (1·14–1·63) | 0·0008 | |
| Urban informal | 0·98 (0·65–1·46) | 0·91 | 0·98 (0·66–1·47) | 0·92 | 0·99 (0·66–1·49) | 0·97 | |
The term “coloured” is used by Statistics South Africa,49 a South African ethnic label that includes children and descendants from black-white, black-Asian, black-coloured, and white-Asian unions.50 The regression model is adjusted on the basis of post-stratification weight (from final observation of the individual panel) to reflect more recent population estimates produced by Statistics South Africa. RR=relative risk.
Table 5.
Adjusted regression models on depression outcome
|
Model 1: log km |
Model 2: within or outside 10 km |
Model 3: within or outside 5 km |
|||||
|---|---|---|---|---|---|---|---|
| Adjusted RR (95% CI) | p value | Adjusted RR (95% CI) | p value | Adjusted RR (95% CI) | p value | ||
| Distance | 1·01 (1·00–1·03) | 0·097 | 1·03 (0·98–1·08) | 0·21 | 1·08 (1·03–1·14) | 0·0029 | |
| Sex | |||||||
| Male | .. | .. | .. | .. | .. | .. | |
| Female | 1·09 (1·04–1·14) | 0·0002 | 1·09 (1·04–1·14) | 0·0001 | 1·09 (1·04–1·14) | 0·0001 | |
| Population group | |||||||
| White | .. | .. | .. | .. | .. | .. | |
| African | 1·67 (1·38–2·02) | <0·0001 | 1·58 (1·30–1·91) | <0·0001 | 1·57 (1·30–1·90) | <0·0001 | |
| Coloured | 1·37 (1·12–1·68) | 0·0020 | 1·28 (1·05–1·56) | 0·017 | 1·27 (1·04–1·55) | 0·020 | |
| Asian or Indian | 1·15 (0·83–1·59) | 0·41 | 1·09 (0·79–1·51) | 0·60 | 1·09 (0·79–1·51) | 0·61 | |
| Age category | |||||||
| 15–19 years | .. | .. | .. | .. | .. | .. | |
| 20–24 years | 1·41 (1·30–1·53) | <0·0001 | 1·41 (1·30–1·53) | <0·0001 | 1·41 (1·30–1·53) | <0·0001 | |
| 25–29 years | 1·55 (1·43–1·69) | <0·0001 | 1·54 (1·42–1·68) | <0·0001 | 1·54 (1·42–1·68) | <0·0001 | |
| 30–34 years | 1·53 (1·39–1·68) | <0·0001 | 1·51 (1·38–1·66) | <0·0001 | 1·51 (1·38–1·66) | <0·0001 | |
| 35–64 years | 1·83 (1·70–1·98) | <0·0001 | 1·82 (1·69–1·97) | <0·0001 | 1·82 (1·68–1·96) | <0·0001 | |
| ≥65 years | 1·76 (1·59–1·96) | <0·0001 | 1·73 (1·56–1·93) | <0·0001 | 1·73 (1·55–1·92) | <0·0001 | |
| Martial status | |||||||
| Single | .. | .. | .. | .. | .. | .. | |
| Living with partner | 1·16 (1·06–1·26) | 0·0008 | 1·16 (1·06–1·26) | 0·0007 | 1·16 (1·06–1·26) | 0·0008 | |
| Widow or widower | 1·32 (1·22–1·43) | <0·0001 | 1·32 (1·22–1·43) | <0·0001 | 1·32 (1·22–1·43) | <0·0001 | |
| Divorced or separated | 1·31 (1·15–1·49) | 0·0001 | 1·29 (1·13–1·48) | 0·0002 | 1·29 (1·13–1·47) | 0·0002 | |
| Never married | 1·25 (1·18–1·32) | <0·0001 | 1·25 (1·18–1·33) | <0·0001 | 1·25 (1·18–1·33) | <0·0001 | |
| Highest educational attainment | |||||||
| High school not completed | .. | .. | .. | .. | .. | .. | |
| Completed high school | 0·89 (0·84–0·95) | 0·0004 | 0·89 (0·84–0·95) | 0·0002 | 0·89 (0·83–0·94) | 0·0001 | |
| Beyond high school | 0·72 (0·66–0·78) | <0·0001 | 0·71 (0·65–0·77) | <0·0001 | 0·71 (0·65–0·77) | <0·0001 | |
| Employment status | |||||||
| Unemployed | .. | .. | .. | .. | .. | .. | |
| Employed | 0·88 (0·84–0·93) | <0·0001 | 0·88 (0·84–0·92) | <0·0001 | 0·88 (0·84–0·92) | <0·0001 | |
| Household income quintile | |||||||
| 1 (lowest) | .. | .. | .. | .. | .. | .. | |
| 2 | 0·94 (0·90–1·00) | 0·036 | 0·95 (0·90–1·00) | 0·047 | 0·95 (0·90–1·00) | 0·051 | |
| 3 | 0·90 (0·85–0·95) | 0·0005 | 0·90 (0·85–0·95) | 0·0005 | 0·90 (0·85–0·96) | 0·0005 | |
| 4 | 0·85 (0·80–0·90) | <0·0001 | 0·85 (0·80–0·91) | <0·0001 | 0·85 (0·80–0·91) | <0·0001 | |
| 5 (highest) | 0·72 (0·66–0·78) | <0·0001 | 0·71 (0·65–0·77) | <0·0001 | 0·71 (0·65–0·77) | <0·0001 | |
| Residential area | |||||||
| Rural | .. | .. | .. | .. | .. | .. | |
| Urban formal | 1·20 (1·15–1·26) | <0·0001 | 1·17 (1·12–1·23) | <0·0001 | 1·16 (1·11–1·21) | <0·0001 | |
| Urban informal | 1·28 (1·19–1·37) | <0·0001 | 1·23 (1·15–1·32) | <0·0001 | 1·22 (1·13–1·30) | <0·0001 | |
The term “coloured” is used by Statistics South Africa,49 a South African ethnic label that includes children and descendants from black-white, black-Asian, black-coloured, and white-Asian unions.50 The regression model is adjusted on the basis of post-stratification weight (from final observation of the individual panel) to reflect more recent population estimates produced by Statistics South Africa. RR=relative risk.
Discussion
This study quantified the association between exposure to waste sites and health at a national level, and yielded three important findings. First, more households in South Africa have been exposed to, or are living closer to, waste sites over time. Second, we found a significantly greater likelihood of asthma, tuberculosis, diabetes, and depression in individuals residing within 5 km from waste sites. Third, the relationship between exposure to waste sites and health persisted even after controlling for socioeconomic factors. These findings highlight the challenges to the sustainable development agenda caused by waste, in terms of the risk of developing chronic and infectious diseases.
To the best of our knowledge, this is the first study to quantify the relationship between exposure to waste sites and multiple health outcomes at a national level. Although systematic reviews often point to the difficulty of drawing a causal relationship between exposure to waste sites and adverse health outcomes, a recent cohort study from Italy found that exposure to hydrogen sulfide emitted from landfill sites was associated with greater mortality and admissions to hospital caused by respiratory diseases for individuals living within 5 km of these waste sites.47 Compared to other measures of proximity to waste sites (eg, distance to a waste site as a continuous or fixed variable), we found that living within 5 km of a waste site was significantly associated with increased risk of asthma, tuberculosis, diabetes, and depression. Although South Africa is at the forefront of strict environmental regulations in sub-Saharan Africa, legal compliance among documented waste site operators is believed to be remarkably low in South Africa,51 which might explain our findings of close proximity to waste sites showing an association with adverse health outcomes.
Interpretation of our findings is subject to three limitations, the first being that we relied on self-reporting of health status, which lacked clinical diagnosis data. Although this is a concern, self-reported health status is likely to be under-reported, and, subsequently, to bias the results towards the null about the potential effect of proximity to waste sites. A study from India indicates that self-reported measures substantially understate true disease prevalence.52 Additionally, long-term effects of exposure to waste sites on various health outcomes (eg, cancer, low birthweight, and congenital abnormalities) beyond 2008–15 are areas of further research. Second, we did not measure land, water, or airborne contamination exposure at the national-level waste sites, nor did we control for general air pollution in the community, so we were unable to establish any causation between the observed health outcomes and living in close proximity to waste sites. High concentrations of hydrogen sulfide and polychlorinated biphenyls near waste sites might be one explanation for the significant association we observed between living within 10 km of a waste site and development of asthma and diabetes.10, 11, 12 Furthermore, we did not account for wind speed and direction, and geography, which could affect migration or dispersal of chemical substances from waste sites. Although the objective of this study was to quantify the health effects of broadly categorised waste and waste sites from a sustainable development perspective, the absence of direct environmental measurements also precludes quantification of different health effects due to varying types of waste sites, given possible variations in compliance with waste management standards.53 Further studies are needed to quantify the health effects of exposure to waste sites, with controls for direct environmental and exposure measurements, as well as dispersal of chemicals adjusted for wind speed and direction, and geography, as well as studies of potential bio-accumulation of risk factors into informal food production systems that undermine the basic livelihood of individuals residing in communities near waste sites. Lastly, our studies did not take illegal waste sites into consideration; we focused solely on publicly available licensed sites. Although environmental pollution from illegal waste disposal does affect health,54 the location and extent of such illegal waste sites in South Africa is unknown. Scarcity of specific occupation data (ie, living near and working in illegal or legally operated waste sites) is another limitation that should be taken into consideration in future studies.
Criticisms of similar previous studies point to an absence of data on potential confounders, such as socioeconomic status, that relate to both health outcomes and environmental exposure.55 Communities living near waste sites in South Africa are widely known to be socioeconomically vulnerable and among the most marginalised, as a result of the historical legacy of the apartheid system. Given the non-experimental nature of the study, we cannot rule out the possible role of residual confounding (although we controlled for multiple socioeconomic variables in the analysis), and caution is warranted in making any direct causal interpretations. Nevertheless, this was the first geospatially driven study, to our knowledge, based on a unique, nationally representative, household panel survey with robust socioeconomic data, that highlights the health risks of living in close proximity to waste sites in sub-Saharan Africa. Our findings have implications for and can inform national-level policies to reduce waste and promote sustainable management of waste. As South Africa undergoes rapid population growth, in a context where chronic poverty and income inequality need to be addressed, our study highlights some of the development challenges of increasing levels of waste (and waste sites); namely, waste production by one group diminishes the health and wellbeing of others, and is not compensated by the producer (ie, negative production externality). Contrary to popular belief, environmental protection and economic growth are not mutually exclusive; effectively functioning ecosystems are essential for economic development.56 Our study reaffirms the needs for a sustainable development approach to address and reduce the enormous rise in the number of waste sites in South Africa, in order to effectively improve health and wellbeing in line with the SDGs.
We identified multiple health problems in individuals living close to waste sites, which is contrary to the constitutional human rights of the population, as outlined in the Constitution of South Africa (ie, Section 24, the right of individuals to live in an environment that is not harmful to their health or wellbeing21). Furthermore, the association with mental health outcomes indicates a potential negative effect on the dignity of individuals living near waste sites, which is linked to both social justice and wellbeing.57 We believe that mental health indicators such as depression might be important for assessing the fulfilment of the constitutional right to dignity (Section 10 of the Constitution of South Africa21), which is also considered a fundamental human right globally (preamble of the Universal Declaration of Human Rights58 and Article 5 of the African Charter on Human and People's Rights59).
In developing countries, it is essential that due regard is given for fundamental human rights and is balanced against decisions relating to economic development; for example, the Constitution of South Africa provides clarity on the limitations on any rights in Section 36 (1), in that “The rights in the Bill of Rights may be limited only in terms of law of general application to the extent that the limitation is reasonable and justifiable in an open and democratic society based on human dignity…”21 The ability to assess the effects of economic development and growth on human dignity is an essential component of decision making in development. Furthermore, producers of waste (individual entities or countries) need to fully understand, quantify, and take responsibility for the complete costs of waste generation, particularly for the burden placed on communities that live near waste sites. This is a particular challenge for waste exporters, which might be contravening the Universal Declaration on Human Rights58 as well as other regional or national human rights provisions.
Our current work is timely in light of the adoption of the highly debated national health insurance programme60 in South Africa, which aims to ensure that all citizens and residents have access to quality health services irrespective of socioeconomic status. This government programme is in line with the Bill of Rights in Section 27 of the 1996 Constitution of South Africa,21 which unequivocally states that access to health care is a basic human right, although progressive in its implementation. We concur with the overarching principle of the national health insurance programme, and the need to prioritise universal health coverage of at-risk communities that are currently exposed to waste sites, in addition to minimising waste production to reduce adverse effects on human health and wellbeing.
Acknowledgments
Acknowledgments
Our study used data from SA-NIDS. Data from waves 1 to 4: Southern Africa Labour and Development Research Unit. National Income Dynamics Study 2008–2015, Cape Town: Southern Africa Labour and Development Research Unit (producer), 2016; Cape Town: DataFirst (distributor), 2016; Pretoria: Department of Planning Monitoring and Evaluation (commissioner), 2014. We thank Lynn Woolfrey at DataFirst (University of Cape Town, Cape Town, South Africa). AT was supported by the South African Medical Research Council (MRC-RFAUFSP-01–2013/UKZN HIVEPI) with funds from the South African National Treasury under its Economic Competitiveness and Support Package. This study forms part of the Sustainable and Healthy Food Systems (SHEFS) programme supported by the Wellcome Trust's Our Planet, Our Health programme (grant number: 205200/Z/16/Z). This content is solely the responsibility of the authors and does not necessarily represent the official views of the South Africa Medical Research Council, South African National Treasury, or the Wellcome Trust.
Contributors
AT, DFC, JKB, FT, and RS were responsible for the conception and design of the study, interpretation of the data, and drafting of the manuscript. AT and DFC analysed the data and generated figures. AT wrote the first draft of the report. All authors read and approved the final manuscript.
Declaration of interests
We declare no competing interests.
References
- 1.Kaza S, Yao L, Bhada-Tata P, Van Woerden F. World Bank; Washington, DC: 2018. What a waste 2.0: a global snapshot of solid waste management to 2050. [Google Scholar]
- 2.Mavropoulos A, Wilson DC, Appelqvist B, Velis CA, Cooper J. International Solid Waste Association; Vienna: 2014. Globalisation and waste management—final report from the ISWA Task Force. [Google Scholar]
- 3.Department of Environmental Affairs . Department of Environmental Affairs; Pretoria: 2018. A report on the state of the waste. Second draft report. [Google Scholar]
- 4.South African Cities Network . South African Cities Network; Braamfontein: 2014. State of waste management in cities – phase 2: modelling the effects of landfilling as a disposal method. [Google Scholar]
- 5.Tape ASB, Coulibaly A, Anoh PK, Aloko JN. Production des déchets et santé des travailleurs: Cas de la Mine d'or de Tongon (Côte d'Ivoire) Eur Sci J. 2019;15:104–118. [Google Scholar]
- 6.Zolnikov TR, da Silva RC, Tuesta AA, Marques CP, Cruvinel VRN. Ineffective waste site closures in Brazil: a systematic review on continuing health conditions and occupational hazards of waste collectors. Waste Manag. 2018;80:26–39. doi: 10.1016/j.wasman.2018.08.047. [DOI] [PubMed] [Google Scholar]
- 7.Jeal H, Jones M. Allergy to rodents: an update. Clin Exp Allergy. 2010;40:1593–1601. doi: 10.1111/j.1365-2222.2010.03609.x. [DOI] [PubMed] [Google Scholar]
- 8.Schountz T, Prescott J. Hantavirus immunology of rodent reservoirs: current status and future directions. Viruses. 2014;6:1317–1335. doi: 10.3390/v6031317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ziraba AK, Haregu TN, Mberu B. A review and framework for understanding the potential impact of poor solid waste management on health in developing countries. Arch Public Health. 2016;74:55. doi: 10.1186/s13690-016-0166-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bazhanov N, Ansar M, Ivanciuc T, Garofalo RP, Casola A. Hydrogen sulfide: a novel player in airway development, pathophysiology of respiratory diseases, and antiviral defenses. Am J Respir Cell Mol Biol. 2017;57:403–410. doi: 10.1165/rcmb.2017-0114TR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Silverstone AE, Rosenbaum PF, Weinstock RS. Polychlorinated biphenyl (PCB) exposure and diabetes: results from the Anniston Community Health Survey. Environ Health Perspect. 2012;120:727–732. doi: 10.1289/ehp.1104247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kouznetsova M, Huang X, Ma J, Lessner L, Carpenter DO. Increased rate of hospitalization for diabetes and residential proximity of hazardous waste sites. Environ Health Perspect. 2007;115:75–79. doi: 10.1289/ehp.9223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Przydatek G, Kanownik W. Impact of small municipal solid waste landfill on groundwater quality. Environ Monit Assess. 2019;191:169. doi: 10.1007/s10661-019-7279-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumari P, Gupta NC, Kaur A. A review of groundwater pollution potential threats from municipal solid waste landfill sites: assessing the impact on human health. Avicenna J Environ Health Eng. 2017;4 [Google Scholar]
- 15.Ma J, Hipel KW. Exploring social dimensions of municipal solid waste management around the globe—a systematic literature review. Waste Manag. 2016;56:3–12. doi: 10.1016/j.wasman.2016.06.041. [DOI] [PubMed] [Google Scholar]
- 16.Holifield R, Porter M, Walker G, editors. Spaces of environmental justice. Wiley-Blackwell; Malden: 2010. [Google Scholar]
- 17.Hussen AM. Routledge; London: 2012. Principles of environmental economics and sustainability: an integrated economic and ecological approach. [Google Scholar]
- 18.Holifield R. Actor-network theory as a critical approach to environmental justice: a case against synthesis with urban political ecology. Antipode. 2009;41:637–658. [Google Scholar]
- 19.Union of South Africa Natives Land Act. Act No. 27 of 1913. June 16, 1913. http://www.ruraldevelopment.gov.za/phocadownload/1913/nativelandact27of1913.pdf
- 20.Ruiters G. Environmental racism and justice in South Africa's transition. Politikon S Afr J Polit Stud. 2001;28:95–103. [Google Scholar]
- 21.Republic of South Africa. The Constitution of the Republic of South Africa. Government Gazette No. 17678. Pretoria: Republic of South Africa, 1996.
- 22.Speight JG. Unconventional gas. In: Speight JG, editor. Natural gas. 2nd edn. Gulf Professional Publishing; Boston, MA: 2019. pp. 59–98. [Google Scholar]
- 23.Figueroa-Munoz JI, Ramon-Pardo P. Tuberculosis control in vulnerable groups. Bull World Health Organ. 2008;86:733–735. doi: 10.2471/BLT.06.038737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tomita A, Smith CM, Lessells RJ. Space-time clustering of recently-diagnosed tuberculosis and impact of ART scale-up: evidence from an HIV hyper-endemic rural South African population. Sci Rep. 2019;9 doi: 10.1038/s41598-019-46455-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang L, Klenosky DB. Residents' perceptions and attitudes toward waste treatment facility sites and their possible conversion: a literature review. Urban For Urban Green. 2016;20:32–42. [Google Scholar]
- 26.Sulla V, Zikhali P. World Bank; Washington, DC: 2018. Overcoming poverty and inequality in South Africa: an assessment of drivers, constraints and opportunities. [Google Scholar]
- 27.Nahman A. Pricing landfill externalities: emissions and disamenity costs in Cape Town, South Africa. Waste Manag. 2011;31:2046–2056. doi: 10.1016/j.wasman.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 28.Global Asthma Network . Global Asthma Network; Auckland: 2018. The global asthma report 2018. [Google Scholar]
- 29.Statistics South Africa . Statistics South Africa; Pretoria: 2018. Mortality and causes of death in South Africa, 2016: findings from death notification. [Google Scholar]
- 30.Herman AA, Stein DJ, Seedat S, Heeringa SG, Moomal H, Williams DR. The South African Stress and Health (SASH) study: 12-month and lifetime prevalence of common mental disorders. S Afr Med J. 2009;99:339–344. [PMC free article] [PubMed] [Google Scholar]
- 31.Murray CJL, Vos T, Lozano R. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 32.Henderson M, Harvey SB, Overland S, Mykletun A, Hotopf M. Work and common psychiatric disorders. J R Soc Med. 2011;104:198–207. doi: 10.1258/jrsm.2011.100231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Evans-Lacko S, Knapp M. Global patterns of workplace productivity for people with depression: absenteeism and presenteeism costs across eight diverse countries. Soc Psychiatry Psychiatr Epidemiol. 2016;51:1525–1537. doi: 10.1007/s00127-016-1278-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.UN . United Nations; New York, NY: 2015. Transforming our world: the 2030 agenda for sustainable development. [Google Scholar]
- 35.Dyson B, Chang N-B. Forecasting municipal solid waste generation in a fast-growing urban region with system dynamics modeling. Waste Manag. 2005;25:669–679. doi: 10.1016/j.wasman.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 36.Hoornweg D, Bhada-Tata P, Kennedy C. Environment: waste production must peak this century. Nature. 2013;502:615. doi: 10.1038/502615a. [DOI] [PubMed] [Google Scholar]
- 37.Hoornweg D, Bhada-Tata P, Kennedy C. Peak waste: when is it likely to occur? J Ind Ecol. 2015;19:117–128. [Google Scholar]
- 38.Ncube F, Ncube EJ, Voyi K. A systematic critical review of epidemiological studies on public health concerns of municipal solid waste handling. Perspect Public Health. 2017;137:102–108. doi: 10.1177/1757913916639077. [DOI] [PubMed] [Google Scholar]
- 39.Fazzo L, Minichilli F, Santoro M. Hazardous waste and health impact: a systematic review of the scientific literature. Environ Health. 2017;16:107. doi: 10.1186/s12940-017-0311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mattiello A, Chiodini P, Bianco E. Health effects associated with the disposal of solid waste in landfills and incinerators in populations living in surrounding areas: a systematic review. Int J Public Health. 2013;58:725–735. doi: 10.1007/s00038-013-0496-8. [DOI] [PubMed] [Google Scholar]
- 41.Leibbrandt M, Woolard I, de Villiers L. University of Cape Town; Cape Town: 2009. Methodology: report on NIDS Wave 1. [Google Scholar]
- 42.Cole JC, Rabin AS, Smith TL, Kaufman AS. Development and validation of a Rasch-derived CES-D short form. Psychol Assess. 2004;16:360–372. doi: 10.1037/1040-3590.16.4.360. [DOI] [PubMed] [Google Scholar]
- 43.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 44.Vincenty T. Direct and inverse solutions of geodesics on the ellipsoid with application of nested equations. Surv Rev. 1975;23:88–93. [Google Scholar]
- 45.Department of Environmental Affairs. Republic of South Africa Licenses. 2019. http://sawic.environment.gov.za/?menu=88
- 46.Republic of South Africa National environmental management: Waste Act, 2008 (Act No. 59 of 2008). Government Gazette, Republic of South Africa. https://www.environment.gov.za/sites/default/files/legislations/nema_amendment_act59.pdf
- 47.Mataloni F, Badaloni C, Golini MN. Morbidity and mortality of people who live close to municipal waste landfills: a multisite cohort study. Int J Epidemiol. 2016;45:806–815. doi: 10.1093/ije/dyw052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wittenberg M. University of Cape Town; Cape Town: 2009. Weights: report on NIDS Wave 1. [Google Scholar]
- 49.Statistics South Africa . Statistics South Africa; Pretoria: 2004. Concept and definitions. [Google Scholar]
- 50.Brown K. Coloured and black relations in South Africa: the burden of racialized hierarchy. Macalester International. 2000;9:13. [Google Scholar]
- 51.GroundWork The Groundwork waste campaign. April, 2014. https://www.groundwork.org.za/waste.php
- 52.Onur I, Velamuri M. The gap between self-reported and objective measures of disease status in India. PLoS One. 2018;13 doi: 10.1371/journal.pone.0202786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Department of Environmental Affairs . Department of Environmental Affairs; Pretoria: 2012. 2nd South Africa environment outlook. A report on the state of the environment; p. 278. [Google Scholar]
- 54.Triassi M, Alfano R, Illario M, Nardone A, Caporale O, Montuori P. Environmental pollution from illegal waste disposal and health effects: a review on the “triangle of death”. Int J Environ Res Public Health. 2015;12:1216–1236. doi: 10.3390/ijerph120201216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rushton L. Health hazards and waste management. Br Med Bull. 2003;68:183–197. doi: 10.1093/bmb/ldg034. [DOI] [PubMed] [Google Scholar]
- 56.Hausmann A, Slotow ROB, Burns JK, Di Minin E. The ecosystem service of sense of place: benefits for human well-being and biodiversity conservation. Environ Conserv. 2016;43:117–127. [Google Scholar]
- 57.Saxena S, Hanna F. Dignity—a fundamental principle of mental health care. Indian J Med Res. 2015;142:355–358. doi: 10.4103/0971-5916.169184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.UNGA Universal declaration of human rights. Dec 10, 1948. https://www.un.org/en/universal-declaration-human-rights/
- 59.Organization of African Unity African (Banjul) Charter on Human and Peoples' Rights. June 27, 1981. https://www.achpr.org/legalinstruments/detail?id=49
- 60.Department of Health. Republic of South Africa National Health insurance for South Africa: towards universal health coverage. 2017. http://www.health.gov.za/index.php/nhi-documents?download=2257:white-paper-nhi-2017