Abstract
To examine the psychometric properties of a short form TSK-AV in Arabic-speaking patients with chronic low back pain (CLBP).
One hundred one CLBP patients recruited from Jordan University Hospital provided demographic information and completed the TSK-AV full version and measures of pain severity and disability. Explorative factor analysis was used to determine whether a generally accepted 2-factor model consisting of fewer TSK items applies to the TSK-AV and exhibits acceptable psychometric properties.
A 2-factor model provided an adequate-to-good fit to our data, explaining 46.54% of the variance. Factor 1 (labeled as “activity avoidance”) comprised items 1, 2, 7, 9, 14, 15, and 17. Factor 2 was labeled as “somatic focus” and comprised items 3, 6, 11, and 13. The 11-item TSK-AV comprised of the 2 factors (TSK-AV-11) as well as its subscales all remained independent significant (P < .001) predictors of pain disability in Jordanian patients with CLBP after accounting for factors such as age, gender, pain duration, and pain severity.
The short, 11-item TSK-AV (TSK-AV-11) appears to be an ideal clinical and research tool for measuring fear of movement/re (injury) in Arabic-speaking patients.
Keywords: arabic, chronic low back pain, psychometric properties, Tampa Scale of Kinesiophobia- version-11 (TSK-AV-11)
1. Introduction
Tampa Scale of Kinesiophobia (TSK) is one of the well-known tools for assessing fear of movement and (re)injury,[1] originally developed in English.[2] The TSK is a 17-item self-report questionnaire with a total score ranging from 17 to 68 with higher scores indicating higher level of fear of movement/(re)injury. High levels of kinesiophobia or fear of movement/(re)injury can predict future disability and pain in acute and healthy samples.[3–15] Importantly, interventions aimed at reduction of kinesiophobia have demonstrated improved functional status and activity tolerance among highly disabled patient samples.[4] Many reports could demonstrate replication of TSK in different types of chronic pain with ongoing testing of its contribution to improve outcomes.
Studying psychometric characteristics of TSK is of high importance for researchers to find out fitting model for studied samples. Both exploratory factor analysis and confirmatory factor analysis (CFA) were investigated, looking for possible factor structure or relation between components and specific factors, respectively.[16] Different models were proposed based on above mentioned methodology. the Dutch version[17] identified 4 factors:
harm
fear of (re)injury
importance of exercise
avoidance of activity
Geisser et al,[18] described a 2-factor structure for the TSK-13 in a sample of chronic back pain patients and French et al[19] also conducted a CFA of the TSK and confirmed the 13-item, 2-factors solution.
Moreover, looking for shorter, valid and replicable form was tempting. The TSK-11 was first described and recommended by Woby et al,[20] where 6 items found to have poor psychometric properties were omitted .This work was followed by a novel CFA by Roelofs et al,[21] who confirmed that an 11-item, 2-factor solution is a fitting model for different patients samples.
The first translation and validation in Arabic-speaking population was accomplished in Jordanian patients with chronic low back pain (CLBP) and reported in April 2017.[15] The original TSK-Arabic version consisted of all 17 items (TSK-AV-17) and was found to be an independent significant predictor of pain disability in these patients after accounting for factors such as age, gender, pain duration, and pain severity. In this current study we aimed to investigate whether the generally accepted 2-factor model of “activity avoidance” and “somatic focus” comprising fewer TSK items also applies to the TSK-AV, thereby potentially leading to a psychometrically sound short form TSK-AV for clinical and research use.
2. Patients & methods
2.1. Participants
One hundred one CLBP patients were recruited from the Department of Rehabilitation and Neurosurgery department at Jordan University Hospital in Amman, Jordan, all of whom gave their informed consent for participation in the study. The same set of patients used in our previous study[15] was used in this study to derive a new measure of kinesophobia in the Arabic population that has not been explored or published before. The study was approved by our local IRB committee and conducted in accordance with the Helsinki Declaration of 1975, as revised in 1983. Chronic pain was defined as pain of at least 3-month duration. Participants provided demographic information and completed measures of pain severity, disability and the TSK-AV.
2.2. Outcome measurements
Pain severity was measured by using a visual analog scale [VAS],[22] The Egyptian version of the Roland Morris disability questionnaire (RMDQ) was used as a measure of functional status/disability related to back pain.[23] The Arabic translation of the Tampa Scale of Kinesiophobia (TSK-AV) was used to assess the fear of (re)injury associated with physical movement.[15]
2.3. Statistical analysis
Means and standard deviations were calculated for participant socio-demographic characteristics, VAS, RMDQ, and TSK-A scores. Analyses of variance compared men and women on study variables.
Using the SPSS package for exploratory factor analysis, 13 TSK-AV items were subjected to a principle axis factoring with varimax rotation to determine whether the most recent 2-factor model proposed by Roelofs and colleagues[21] provided a good fit for the data. This analysis was performed with omission of reversed key items, an approach taken by nearly all proposed models to investigate the internal structure of TSK.[21,24,25] The scree plot (with all components after the elbow to be dropped) was used to determine appropriateness of the number of factors.[26] Items with loading below 0.32 on all factors were excluded based on the criteria of Comrey and Lee.[27] Items having high factor loading on more than 1 factor were assigned to a factor based on content. Internal consistency of subscales derived from the full version of TSK-AV was calculated using the Cronbach alpha coefficient, with values above 0.70 considered acceptable.[28]
A series of hierarchical regression analyses were then performed to assess the unique predictive validity of the various subscales of the TSK-AV obtained through exploratory factor analysis. For each regression, RMDQ score served as the dependent variable and initial blocks controlled for demographic variables and pain severity. Initial checks confirmed assumptions of normality, linearity, and hetero-scedasticity. Variance-inflation factors confirmed no problems of multi-collinearity.
3. Results
3.1. Sample characteristics
One hundred one patients with CLBP participated in the study. Fifty-three were female; 81 were married and 49 were employed. Their age ranged from 20 to 83 years with a mean age of 47.8 years (SD = 16.3). Mean pain duration was 5.1years (SD = 5.2) with a range of 0.25 to 25 years. In comparison to male participants, female participants were older (52.2 vs 43 years, P < .01), had higher VAS scores (pain severity), (60.7 vs 43.4, P < .001), RMDQ scores (disability) (15.5 vs 9.4, P < .001) and TSK-AV scores (47.7 vs 39.9, P < .001).
3.2. Factor analysis
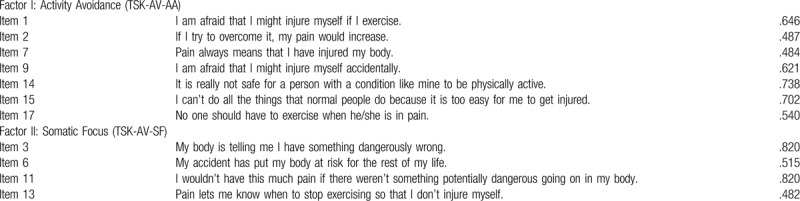
Scree test method indicated the relative suitability of 2 factors for the TSK-AV. A solution of 2 factors, similar to that proposed by Roelofs and colleagues[21] provided adequate fit for the data. Factors were labeled following the common procedure of giving the greatest consideration to items with high loadings on each factor. The following labels were assigned: activity avoidance (TSK-AV-AA) comprising items 1, 2, 7, 9, 14, 15, and 17 and somatic focus (TSK-AV-SF) comprising items 3, 6, 11, and 13. This 2-factor solution cumulatively accounted for 46.54% of the total variance (33.73% and 12.81% for each factor, respectively).
Table 1 shows the factor loadings of each of the TSK-AV items included in the 2-factor solution. Items 5 and 10 had no significant loadings on any factor. Item 6 was assigned to factor 2 (somatic focus) based on its content. The final TSK-AV consisted of 11 items (TSK-AV-11).
Table 1.
Factor loadings of the 2-factor Tampa Scale of Kinesiophobia-Arabic Version model as obtained by principal axis factoring.
3.3. Internal consistency
The internal consistency (Cronbach coefficient) for the TSK-AV-11 was 0.80, indicating good internal consistency. Cronbach coefficients for the TSK-AV-AA and TSK-AV-SF factors were 0.74 and 0.68, respectively.
3.4. Predictive validity
Table 2 summarizes 3 separate hierarchical regression analyses conducted to examine the independent predictive value of the 2-factor TSK-AV-11and each discrete factor separately in accounting for variance in disability (RMDQ). For each analysis, socio-demographic variables (age, gender, pain duration) were entered into the first block. Pain severity (VAS) was entered into the second block. In Regression 1, the TSK-AV-11 was entered into the third block. Regressions 2 and 3 examined the unique contribution of TSK-AV-AA and TSK-AV-SF factors, respectively.
Table 2.
Stepwise hierarchical regression analyses.
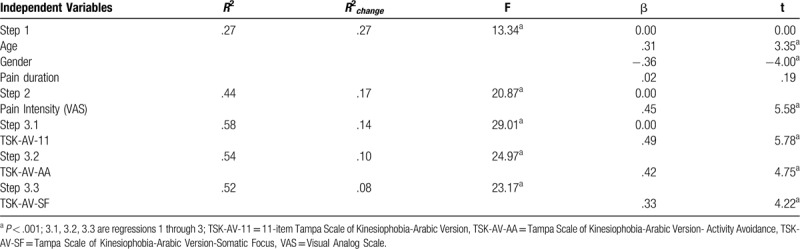
Of demographic characteristics, age and gender accounted for 27% of the variance in disability scores, FΔ = 13.34, P < .001, indicating that women and older patients reported greater disability. In the second block, pain severity accounted for an additional 17% of the variance, FΔ = 20.87, P < .001. When added to the third block, participants score on the 11-item TSK-AV accounted for an additional 14% of the variance in disability (Regression 1: FΔ = 29.01, P < .001), beyond that accounted for pain severity, duration, and socio-demographic variables. The factor TSK-AV-AA alone accounted for an additional 10% of the variance in disability scores when entered into the third block (Regression 2: FΔ = 24.97, P < .001). The factor TSK-AV-SF alone accounted for an additional 8% of the variance when entered in to the third block (Regression3: FΔ = 23.17, P < .001).
Finally, a regression model including age, gender, pain duration, pain severity (VAS), and TSK-AV-11 demonstrates that only TSK-AV-11 (beta = 0.489; P < .001), age (beta = 0.224; P = .0012), and VAS (beta = 0.2651; P = 0.001) are significant predictors of disability (RMDQ).
4. Discussion
Our group has previously reported the first translation and validation of the original TSK-AV in Arabic-speaking CLBP patients.[15] The 17-item TSK-Arabic version or TSK-AV-17 predicted pain disability in this population and was, deemed a suitable measure of kinesiophobia in Arab patients with CLBP. The objective of the current study is to investigate whether the generally accepted 2-factor model of “activity avoidance” and “somatic focus” comprising fewer TSK items also applies to the TSK-AV.
Explorative factor analysis of our data supported the widely accepted 2-factor model, explaining approximately 46.54% of the variance. As in Roelofs et al,[21] our model contained 11 items; however, these items are not identical to the Roelofs study. Similar to Roelofs study, our “somatic focus” factor included items 3, 6, and 11; these items consistently reflect the somatic focus factor in previously reported models,[5,18,24,29,30] However, item 5 (labeled “somatic focus” by Roelofs et al) did not load on any factor in our investigation. Likewise, item 7 (also labeled “somatic focus” by Roelofs et al) loaded on the TSK-AV-AA factor in the current study. Conversely, item 13 emerged as part of the TSK-AV-SF factor within our study but were identified as part of the “activity avoidance” factor by Roelofs et al. Careful content inspection of items 7 and 13 suggests that they may be assigned to either the TSK-AV-AA or TSK-AV-SF factor. In particular, item 7 loaded onto “activity avoidance” in studies by Swinkels-Meewisse et al, Geisser et al[18] and in the 2-factor model of the TSK Persian version.[13]
In comparing our model with other studies, it is notable that our model showed good internal consistency for the 11-item TSK-AV (α=0.80) and acceptable internal consistency for the TSK-AV-AA and TSK-AV-SF factors (α=0.74 and 0.68, respectively). These values are in line with those previously reported for 2-factor models.[13,19] Moreover, the 11-item TSK-AV, the TSK-AV-AA, and the TSK-AV-SF each accounted for independent variance in disability after controlling for demographic and pain variables.
When examined separately, the factor TSK-AV-AA explained somewhat greater variance in disability than TSK-AV-SF. This finding is consistent with emphasis on avoidance behavior in development/maintenance of disability as articulated by the fear-avoidance model[30] as well as exposure-based interventions stemming from this model.[31] However, the predictive value of TSK-AV-SF attests to the importance of attention and interpretation of bodily sensations as part of the fear-avoidance cycle.[31] Finally, the variance explained by the combined factors was less than the sum of the variance of each factor, suggesting conceptual overlap between activity avoidance and somatic focus that has been noted in previous psychometric studies.[19]
When compared to the 17-item TSK-AV (TSK-AV-17) examined in our previous report,[15] the short form TSK-11 shows similar or superior psychometric properties. The 2-factor model explains 46.54% of the variance versus 45.2% explained by a 3-factor model comprising all 17 items. In multivariate regression analysis both the TSK-AV-11 and TSK-AV-17 accounted for an additional 14% of the variance in disability beyond that accounted for pain severity, duration, and socio-demographic variables. While the Cronbach coefficient for the TSK-AV-11was identical to the TSK-AV-17 (both 0.80), the Cronbach coefficients for the TSK-AV-AA and TSK-AV-SF factors in the current 2-factor model were 0.74 and 0.68, respectively versus 0.75, 0.64, and 0.6 for the TSK-AV-AA, TSK-AV-EP, and TSK-AV-SF factors, respectively in the 3-factor model encompassing all 17 TSK items, indicating superior internal consistency for the 2-factor model. Given the advantage of brevity and the similar or superior psychometric properties compared with the TSK-AV-17, the TSK-AV-11 is a preferred tool for measuring kinesiophobia in patients with CLBP with potential application in other pain conditions, such as acute LBP and work-related upper extremity disorders. This brevity allows the TSK-AV-11 to increase the response rate, item completion rate,[32] reduces response burden,[33] and puts the TSK-AV-11 at better preference from time required for administration compared to TSK-AV-17. However, prospective studies are needed to determine the performance of this new measure in the clinical and research settings.
5. Conclusion
The current study of TSK-AV in Jordanian patients with CLBP replicated the 2-factor structure of activity avoidance and somatic focus identified in previous literature. The 11-item TSK-AV (comprising the 2-factor model), the TSK-AV-AA, and the TSK-AV-SF each accounted for significant variance in disability above and beyond demographic and pain factors. Overall, the findings support the utility of the short TSK-AV-11 instrument in assessing kinesiophobia among Arabic individuals with CLBP.
Author contributions
AAL-S and MEJ conceived the study and its design; KF and ZMH collected the data; AAL-S, MEJ, KF, ZMH and AA managed, analyzed, and interpreted the data. AAL-S and MEJ wrote the original manuscript. All authors have read, edited and approved the final manuscript.
Footnotes
Abbreviations: CFA = confirmatory factor analysis, CLBP = chronic low back pain, RMDQ = Roland Morris disability questionnaire, TSK-AV = Tampa Scale of Kinesiophobia-Arabic version, VAS = visual analog scale.
How to cite this article: AL-Shudifat A, Farah K, Hawamdeh ZM, Alqudah A, Juweid ME. Psychometric testing of a short form, 11-item Tampa Scale of Kinesiophobia–Arabic version: TSK-AV-11. Medicine. 2020;99:24(e20292).
The authors have no funding and conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain 2000;85:317–32. [DOI] [PubMed] [Google Scholar]
- [2].Miller RP, Kori S, Todd D. The Tampa Scale: a measure of kinesiophobia. Clin J Pain 1991;7:51–2. [Google Scholar]
- [3].Crombez G, Vlaeyen JW, Heuts PH, et al. Pain-related fear is more disabling than pain itself: evidence on the role of pain-related fear in chronic back pain disability. Pain 1999;80:329–39. [DOI] [PubMed] [Google Scholar]
- [4].Vlaeyen JWS, de Jong J, Geilen M, et al. The treatment of fear of movement/(re)injury in chronic low back pain: further evidence on the effectiveness of exposure in vivo. Clin J Pain 2002;18:251–61. [DOI] [PubMed] [Google Scholar]
- [5].Vlaeyen JW, Kole-Snijders AM, Boeren RG, et al. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain 1995;62:363–72. [DOI] [PubMed] [Google Scholar]
- [6].Boersma K, Linton SJ. How does persistent pain develop? An analysis of the relationship between psychological variables, pain and function across stages of chronicity. Behav Res Ther 2005;43:1495–507. [DOI] [PubMed] [Google Scholar]
- [7].Lundberg MKE, Styf J, Carlsson SG. A psychometric evaluation of the Tampa Scale for Kinesiophobia—from a physiotherapeutic perspective. Physiother Theory Pract 2004;20:121–33. [Google Scholar]
- [8].De Souza FS, Marinho C da S, Siqueira FB, et al. Psychometric testing confirms that the Brazilian-Portuguese adaptations, the original versions of the fear-avoidance beliefs questionnaire, and the Tampa Scale of Kinesiophobia have similar measurement properties. Spine 2008;33:1028–33. [DOI] [PubMed] [Google Scholar]
- [9].Haugen AJ, Grøvle L, Keller A, et al. Cross-cultural adaptation and validation of the Norwegian version of the Tampa scale for Kinesiophobia. Spine 2008;33:595–601. [DOI] [PubMed] [Google Scholar]
- [10].Monticone M, Giorgi I, Baiardi P, et al. Development of the Italian version of the Tampa Scale of Kinesiophobia (TSK-I): cross-cultural adaptation, factor analysis, reliability, and validity. Spine 2010;35:1241–6. [DOI] [PubMed] [Google Scholar]
- [11].Wong WS, Kwok HY, Luk KDK, et al. Fear of movement/(re)injury in Chinese patients with chronic pain: factorial validity of the Chinese version of the Tampa Scale for Kinesiophobia. J Rehabil Med 2010;42:620–9. [DOI] [PubMed] [Google Scholar]
- [12].Gómez-Pérez L, López-Martínez AE, Ruiz-Párraga GT. Psychometric Properties of the Spanish version of the Tampa Scale for Kinesiophobia (TSK). J Pain 2011;12:425–35. [DOI] [PubMed] [Google Scholar]
- [13].Jafari H, Ebrahimi E, Salvati M, et al. Psychometric properties of Iranian version of Tampa Scale for Kinesiophobia in low back pain patients. J Rehabil 2010;11:15–22. [Google Scholar]
- [14].Koho P, Borodulin K, Kautiainen H, et al. Finnish version of the Tampa Scale of Kinesiophobia: reference values in the Finnish general population and associations with leisure-time physical activity. J Rehabil Med 2015;47:249–55. [DOI] [PubMed] [Google Scholar]
- [15].Juweid M, Farah K, Hawamdeh Z, et al. Fear of movement/[re]injury among Arabic low back pain patients: establishing the validity of the Tampa Scale of Kinesiophobia-Arabic version. Myopain 2017;23:134–42. [Google Scholar]
- [16].Byrne BM. Structural equation modeling with EQS: basic concepts, applications, and programming. New York, NY: Psychology Press; 2006. [Google Scholar]
- [17].Vlaeyen JWS, Kole-Snijders AMJ, Rotteveel AM, et al. The role of fear of movement/(re)injury in pain disability. J Occup Rehabil 1995;5:235–52. [DOI] [PubMed] [Google Scholar]
- [18].Geisser ME, Haig AJ, Theisen ME. Activity avoidance and function in persons with chronic back pain. J Occup Rehabil 2000;10:215–27. [Google Scholar]
- [19].French DJ, France CR, Vigneau F, et al. Fear of movement/(re)injury in chronic pain: a psychometric assessment of the original English version of the Tampa Scale for Kinesiophobia (TSK). Pain 2007;127:42–51. [DOI] [PubMed] [Google Scholar]
- [20].Woby S.R., Roach N.K., Urmston M., et al. Psychomet-ric properties of the TSK-11: a shortened version of the Tampa Scale for Kinesiophobia. Pain. 2005;17: 137–144. [DOI] [PubMed] [Google Scholar]
- [21].Roelofs J, Sluiter JK, Frings-Dresen MHW, et al. Fear of movement and (re)injury in chronic musculoskeletal pain: evidence for an invariant two-factor model of the Tampa Scale for Kinesiophobia across pain diagnoses and Dutch, Swedish, and Canadian samples. Pain 2007;131:181–90. [DOI] [PubMed] [Google Scholar]
- [22].Hawker GA, Mian S, Kendzerska T, et al. Measures of adult pain visual analog scale for pain (VAS Pain), numeric rating scale for pain (NRS Pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res 2011;63:240–52. [DOI] [PubMed] [Google Scholar]
- [23].Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine 1983;8:141–4. [DOI] [PubMed] [Google Scholar]
- [24].Clark ME, Kori SH, Brockel J. Kinesiophobia and chronic pain: psychometric characteristics and factor analysis of the Tampa Scale. Am Pain Soc Abstr 1996;15:77–82. [Google Scholar]
- [25].Roelofs J, van Breukelen G, Sluiter J, et al. Norming of the Tampa Scale for Kinesiophobia across pain diagnoses and various countries. Pain 2011;152:1090–5. [DOI] [PubMed] [Google Scholar]
- [26].Colgan P. The scientific use of factor analysis in behavioral and life sciences. Behav Process 1981;6:385–6. [Google Scholar]
- [27].Psychology Press, Comrey AL, Lee HBA. A first course in factor analysis. 2013. [Google Scholar]
- [28].Allen & Unwin, Pallant J. SPSS survival manual: a step-by-step guide to data analysis using SPSS. 2007. [Google Scholar]
- [29].Goubert L, Crombez G, Van Damme S, et al. Confirmatory factor analysis of the Tampa Scale for Kinesiophobia: invariant two-factor model across low back pain patients and fibromyalgia patients. Clin J Pain 2004;20:103–11. [DOI] [PubMed] [Google Scholar]
- [30].Leeuw M, Goossens ME, Linton SJ, et al. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med 2007;30:77–94. [DOI] [PubMed] [Google Scholar]
- [31].Vlaeyen J, Morley S, Linton SJ. Pain-related fear: exposure based treatment for chronic pain. International Association for the Study of Pain 2012. [Google Scholar]
- [32].Salisbury C, Burgess A, Lattimer V, et al. Developing a standard short questionnaire for the assessment of patient satisfaction with out-of-hours primary care. Family Practice 2005;22:560–9. [DOI] [PubMed] [Google Scholar]
- [33].Mo C, Deane FP, Lyons GC, et al. Factor analysis and validity of a short six-item version of the Desires for Alcohol Questionnaire. Journal of Substance Abuse Treatment 2013;44:557–64. [DOI] [PubMed] [Google Scholar]


