Abstract
Introduction
Injection drug use (IDU) remains a significant public health problem. IDU has been associated closely with the opioid crisis; driving overdose, HIV, and Hepatitis C (HCV) infection nationwide. Syringe services programs (SSPs) remain pivotal evidence-based interventions to reduce harm and engage subgroups of people who inject drugs (PWID). This study aims to provide policy considerations from the IDEA SSP, the first legal SSP in the state of Florida.
Methods
We performed a latent class analysis on patterns of substance use among participants (N = 982) newly enrolled in a syringe services program (SSP). Associations between classes of substance use and sociodemographic variables, risky injection and sex behaviors, HIV/HCV status and syringe coverage were analyzed using the R3STEP and BCH 3-step procedures in latent class regression.
Results
We found a three-class solution: Heroin-Dominant class (73.9%), Methamphetamine-Dominant class (9.5%) and Heroin/Cocaine class (16.6%). Compared to Heroin-Dominant class, the Heroin/Cocaine class were more likely to report homelessness, sharing works, unprotected sex, public injection, and to be HCV positive. Compared to both Heroin-Dominant and Heroin/Cocaine classes, the Methamphetamine-Dominant class were more likely to be male, Hispanic, gay or bisexual orientation, HIV positive, to report unprotected sex and sex with PWID. In addition, the lowest and highest syringe coverage were among those in the Heroin/Cocaine and Methamphetamine-Dominant classes, respectively.
Conclusion
Existing interventions among this population to mitigate infectious disease risk, such as SSPs, can be a used to engage differing PWID populations. However, multi-component, targeted preventive interventions and need-based syringe distribution policies are required to further reduce HIV and HCV risk among various PWID populations.
Keywords: Substance Use, Syringe Services Program, HIV prevention, HCV, Drug Policy
1. Introduction
People who inject drugs (PWID) experience increased morbidity and mortality, including drug-related overdose, blood-borne viral infections and bacterial infections. In 2018, the State of Florida recorded the highest number of new HIV cases and new AIDS diagnoses in the United States (U.S.)(CDC, 2019). Three metropolitan areas in Florida were among the top ten areas across the U.S. for HIV incidence, with Miami-Fort Lauderdale-West Palm Beach recording the most diagnoses (CDC, 2019). The Florida Department of Health has reported that injection drug use was a dominant risk factor in approximately 6% of new HIV diagnoses in 2017 (Florida Department of Health Surveillance Report, 2018). However, PWID accounted for 9% of HIV diagnoses and 13% of AIDS diagnoses nationally in 2018 (CDC, 2019). Increases in injection drug use have the potential to be a catalyst in rapidly spreading HIV among PWID, as demonstrated recently in outbreaks in Indiana, Massachusetts, Washington, and Miami (Alpren et al., 2020; Cranston et al., 2019; Golden et al., 2019; Peters et al., 2016; Tookes et al., 2019). In addition to injection-related risk, prevalence of sex work to generate income has increased, posing additional risk for HIV infection (Baral et al., 2014; Kerr et al., 2016). With the lifetime treatment cost of one HIV infection estimated to be $379,668, HIV acquisition among PWID continues to be a significant public health concern (Schackman et al., 2015).
In addition to the risk of HIV transmission, IDU is currently the most common means of hepatitis C (HCV) transmission in the U.S., with an estimated 80% of all new infections attributable to injection drug use (Zibbell et al., 2018; Zibbell et al., 2015). In addition, there has been a 350% national increase in acute HCV from 2010–2016, seen in part due to the nation’s opioid crisis (Zibbell et al., 2018). Currently, there are an estimated 151,000 individuals living with HCV in the State of Florida (Rosenberg et al., 2018). Although the current state of new HCV infections has been linked to opioid injection, non-opioid related substance use has also been implicated in HCV transmission, specifically injection of methamphetamine (Cunningham et al., 2015).
Prior studies have suggested that the potential risks associated with injection drug use may differ by type of drug injected. A study in Eastern Europe determined that people who primarily use stimulants, including amphetamines, had a lower association of HIV infection compared to people who inject opioids within the two cities sampled (Tavitian-Exley, Maheu-Giroux, et al., 2018). People who inject multiple substances engage in more injection and sexual risk behaviors, and are at higher risk for HIV compared to mono-substance using PWID (Meacham et al., 2018; Tavitian-Exley, Boily, et al., 2018). Prior data from our syringe services program (SSP) in Miami, Florida has illustrated that participants use many different substances, including heroin, cocaine, and methamphetamine (Iyengar, Kravietz, Bartholomew, Forrest, & Tookes, 2019).
In 2019, Florida passed the Infectious Disease Elimination Act (IDEA), which authorizes individual counties to opt into establishing SSPs. Over 30 years of research have supported the effectiveness of SSPs for HIV prevention (Fernandes et al., 2017), engagement for substance use treatment (Bluthenthal, 2001), and overdose prevention (Barocas, Baker, Hull, Stokes, & Westergaard, 2015). With this expansion policy, it is imperative to analyze existing programs in the state to better understand how to improve SSP implementation and policies that impact SSP operation and effectiveness. Currently, the only legal SSP in Florida is the IDEA SSP, formerly a pilot program at the University of Miami authorized under the 2016 Infectious Disease Elimination Act. Under past and current legislation, SSPs must follow a strict one-for-one syringe exchange distribution method—a method that has demonstrated reduced effectiveness in decreasing risk for HIV/HCV infection (Bluthenthal, Anderson, Flynn, & Kral, 2007). Participants must provide a used syringe for enrollment into the program where each participant is given a base set of 10 syringes in return. After this baseline enrollment visit, participants are only given the number of syringes disposed of at that exchange visit. Given the high incidence of new HIV diagnoses in Miami-Dade County, the diversity of substances reportedly being injected (Iyengar et al., 2019), and the change in policy landscape, the population of PWID at the Miami SSP provides a unique opportunity to examine risk and syringe coverage under the restrictive one-for-one exchange policy.
One methodology commonly used to assess subpopulations of substance use and risk is an extension of finite mixture modeling called latent class analysis (LCA). LCA allows for the identification of not directly observable classes of individuals based upon multiple observed characteristics that members of a heterogenous group share in common (McCutcheon, 1987). LCA has been employed to examine how individuals with different patterns of substance use differ in sexual risk behavior (Trenz et al., 2013); to classify people who use substances into low, middle, and high risk classes for HIV infection based on drug use and sexual behaviors (Feaster et al., 2016; Noor, Ross, Lai, & Risser, 2014); and to elucidate drug network composition based on type and route of administration of cocaine and heroin (Kuramoto, Bohnert, & Latkin, 2011). LCA also has been applied to uncover patterns of drug use differing in co-morbid pathologies (Monga et al., 2007); identify subgroups of people who use substances to identify more specific interventions to reduce harm (Meacham et al., 2015), and determine subpopulations of people with non-injection use of heroin and cocaine and identified risks related to acquiring HIV and HCV (Harrell, Mancha, Petras, Trenz, & Latimer, 2012). Recent studies have explored drug use typologies and the role of polysubstance use as it pertains to overdose and take-home naloxone (Gicquelais et al., 2019; Schneider et al., 2020). Polysubstance use has also been associated with increase in injection frequency (Leri, Stewart, Tremblay, & Bruneau, 2004) and syringe lending (Voon et al., 2015), suggesting an increased need for access to SSP services among those using multiple substances. This study aims to use LCA to identify specific injection drug use patterns among SSP participants and assess how these classes relate to risk behaviors, HIV/HCV status, and, most importantly, syringe coverage. We hypothesized that different risk profiles for the acquisition of HIV and HCV exist depending on which substances are primarily injected (Tavitian-Exley, Vickerman, Bastos, & Boily, 2015), and that these classes would differ in ability to maintain sufficient syringe coverage through SSP utilization.
2. METHODS
2.1. Human Subjects
This study was determined not to be human subjects research by the Institutional Review Board of the University of Miami (IRB #20190740) due to the use of anonymous program data as part of routine pilot program evaluation.
2.2. Setting
The Miami SSP was established December 2016 as the first legal SSP in the State of Florida, authorized as a five-year pilot program. It operates primarily from a fixed site but also has a mobile outreach unit. Participants are provided with new syringes and injection equipment, as well as naloxone and an array of wraparound services.
2.3. Study Sample
We studied participants (N = 982) who enrolled in the Miami SSP fixed site between December 2016 and July 2019. Data from the mobile SSP site was not used in this analysis due to incomplete data. At initial enrollment into the program, participants received rapid HIV and HCV testing, along with a 15-minute behavioral interview performed by SSP staff. This baseline assessment included sociodemographics, injection-related risk behaviors, drug use and sexual risk. All study data were collected and managed using REDCap (Harris et al., 2009) electronic data capture tools hosted at the University of Miami Department of Public Health Sciences.
Measures
2.4. Latent Class Indicators
As part of the assessment of drug use at baseline, participants were asked by the interviewer “In the past 30 days, what drugs have you injected?” Participants were asked to choose as many drugs as were applicable from the following list: heroin, prescription painkillers, cocaine, methamphetamine, crack-cocaine, speedball (a mixture of heroin and cocaine), and fentanyl/carfentanil. These seven drug indicators were used in the LCA to determine class membership.
2.5. Socio-Demographics
Socio-demographic measures included age (continuous), gender (male vs. female), race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic), education level (high school education or less vs. higher education degree beyond high school), income (less than $15,000/year vs. more than $15,000/year), health insurance (Medicaid, Medicare, Private), housing status (currently homeless vs. not homeless) and sexual orientation (gay or bisexual vs. heterosexual).
2.6. Risk Behaviors
Risky injection-related practices included overdose (“Have you ever overdosed due to injection drug use” and dichotomized to ever overdosed while injecting vs. never overdosed while injecting), frequency of injection in the previous 30 days (more than 7 times/day vs. less than 7 times/day), reusing syringes in the previous 30 days (any vs. no reusing), receptive or distributive sharing of works (i.e., needles, syringes, cottons, cookers) in the previous 30 days (any vs. no sharing), private (i.e., in home) injection in the previous 30 days and public (i.e., street, park, sidewalk) injection in the previous 30 days.
Risky sexual practices included self-reported unprotected sex in the previous 30 days (yes/no) and having sex with a person who injects drugs in the previous 30 days (yes/no).
2.7. HIV/HCV status
At initial enrollment into the SSP, participants were offered a rapid HIV test via fingerstick using OraQuick Advance® Rapid HIV-1/2 Antibody test or Chembio SURE CHECK® HIV 1/2 Assay and a rapid HCV test via fingerstick using OraQuick® HCV Rapid Antibody Test. Participants also were asked to self-report current HIV and HCV status. Both self-reported and biological test data for HIV and HCV were used in the analysis.
2.8. Syringe Coverage Estimates
Using the methods for calculating syringe coverage estimates presented in Bluthental et al., 2007, we developed an adapted methodology to determine syringe coverage. Currently, by statute, the IDEA SSP must provide strict one-for-one exchange of syringes. Syringe coverage would ideally be measured as the percentage of injections in which a new syringe was used, with a score of 100 implying that a participant has a new, unused needle for each injection. To estimate this percentage, the number of days between each participant’s visits was calculated and multiplied by the participant’s self-reported average injections per day in the previous 30 days at baseline to create the expected number of injections between visits. Because responses for average injections in a day were in binned categories, less then daily, 1–2 times, 3–4 times, 5–7 times, 8–10 times, 11–15, and >15 times a day, both the lower and upper cut points of the client’s bin were used to make a lower and upper bound for number of injections between exchange visits. The number of syringes given during that specific time was divided by the estimated number of injections during that same time period and multiplied by 100% to produce a syringe coverage estimate between visits per participant (100% coverage equals one syringe received for each estimated injection). The equation for syringe coverage can be seen below:
The median syringe coverage based on both the lower and upper cut point for each participant over the time using the program was calculated and used in the analysis. In addition, the average number of syringe exchange visits (specifically to exchange syringes) was calculated.
2.9. Statistical Analysis
Latent Class Analysis (LCA) was used to explore and define the injection drug use profiles of SSP participants engaging in program services for the first time (i.e., initial enrollment). These observed variables tend to be correlated; however, LCA uses this correlation to identify different latent classes, assuming that indicator variables are uncorrelated, conditional on class membership.
Class enumeration was done without covariates by estimating models with increasing numbers of classes until the sample size in each latent class was considered to be too small for practical interpretation (less than 5% of the total sample size) and/or information criteria showed worse model fit. To ensure the models converged to the global maximum, 500 random starts and 100 replicated likelihoods were used for each model. Model fit statistics for each of the models were used to determine the model that best fit the data, including entropy (Celeux & Soromenho, 1996) and penalized information criteria (i.e., Bayesian Information Criteria (BIC), Akaike’s Information Criteria (AIC) (Vrieze, 2012)) and bootstrapped likelihood ratio tests (BLRT)(Asparouhov & Muthén, 2012; Feng & McCulloch, 1996).
Once the best-fitting class structures were determined, a 3-step approach using the R3STEP procedure (Asparouhov & Muthén, 2014) was used to examine between-class differences among the covariates without changing class structure. Associations of between-class covariate predictor effects were assessed using unadjusted odds ratios. In addition, the BCH procedure (Asparouhov & Muthén, 2014) was used to determine the mean difference in upper and lower syringe coverage between latent classes. The BCH and R3Step methods avoid shifts in latent class and evaluate differences in the means across determined classes. All LCA data modeling was performed using Mplus version 8 (Muthén & Muthen, 2017), and significance was set at an alpha of 0.05.
3. RESULTS
3.1. Description of Overall Sample
The overall sample included in this analysis were 982 SSP participants that enrolled into the program between December 2016 and July 2019. Descriptive statistics of the sample can be found in Table 1. Majority of the participants were male (75.3%), non-Hispanic White (54.9%) and reported heroin use (75.9%). In addition, 37.8% had reported being currently homeless when enrolling into the SSP.
Table 1.
Descriptive Statistics of the Study Sample (N=982)
| Characteristic | N (%) |
|---|---|
| Age (mean, SD) | 37.5 (10.6) |
| Gender | |
| Male | 734 (75.3) |
| Female | 241 (24.7) |
| Race/Ethnicity | |
| Non-Hispanic White | 520 (54.9) |
| Non-Hispanic Black | 50 (5.3) |
| Hispanic | 376 (39.7) |
| Educational Attainment | |
| Less than High School | 478 (49.4) |
| Greater than High School | 489 (50.6) |
| Income (annual) | |
| <$14,999 | 478 (53.5) |
| >$15,000 | 415 (46.5) |
| Homeless | |
| Currently homeless | 350 (37.8) |
| Not currently homeless | 577 (62.2) |
| Drugs Injected | |
| Heroin | 746 (75.9) |
| Prescription Opioids | 70 (7.1) |
| Cocaine | 281 (28.6) |
| Methamphetamine | 157 (16.0) |
| Crack-Cocaine | 90 (9.2) |
| Speedball | 179 (18.2) |
| Fentanyl/Carfentanil | 153 (15.6) |
| Injection Frequency | |
| Less than Daily | 88 (9.3) |
| 1–2 times a day | 211 (22.2) |
| 3–4 times a day | 277 (29.2) |
| 5–7 times a day | 211 (22.2) |
| 8–10 times a day | 95 (10.0) |
| 11–15 times a day | 28 (3.0) |
| >15 times a day | 40 (4.2) |
| Disease Status | |
| HIV-positive | 98 (10.2) |
| HCV-positive | 419 (44.4) |
3.2. Class Membership
We selected a latent class model that identified 3 classes of PWID as the optimal model for our data. Comparisons among model fit indices are presented in Table 2. The 3-class model presented the lowest BIC score (BIC=5718.94). Although the 4-class model had a lower SA-BIC (5631.93vs. 5645.89) compared to the 3-class model, the 3-class model had the greatest entropy among all models (entropy = 0.82) and the 4-class solution had one class below 5% of the sample. This taken together (lowest BIC, sufficient entropy, and class sample size), a 3-class model was chosen.
Table 2.
Model Fit Statistics and Entropy for 1-Class through 4-Class models
| Information Criteria | 1-Class | 2-Class | 3-Class | 4-Class |
|---|---|---|---|---|
| N Free Parameters | 7 | 15 | 23 | 31 |
| N Classes | 1 | 2 | 3 | 4 |
| AICa | 6026.84 | 5789.06 | 5606.48 | 5578.81 |
| BICb | 6061.06 | 5862.40 | 5718.94 | 5730.39 |
| SABICc | 6038.83 | 5814.76 | 5645.89 | 5631.93 |
| Entropy | --- | 0.72 | 0.82 | 0.72 |
| LLd | −3006.42 | −2879.53 | −2780.24 | −2758.41 |
| BLRTe | --- | −3006.4 (p<0.001) | −2879.5 (p<0.001) | −2780.2 (p<0.001) |
| Chi-Square | 1866.74 | 436.73 | 198.48 | 123.33 |
| df | 120 | 112 | 104 | 96 |
| p value | <0.001 | <0.001 | <0.001 | 0.032 |
| Number in Each Class | ||||
| Class 1 | 982 (100%) | 157 (16%) | 93 (9.5%) | 42 (4.3%) |
| Class 2 | --- | 825 (84%) | 163 (16.6%) | 93 (9.5%) |
| Class 3 | --- | --- | 726 (73.9%) | 304 (30.9%) |
| Class 4 | --- | --- | --- | 543 (55.3%) |
Note. Bolded values indicate optimal fit among the four models.
AIC = Akaike Information Criteria
BIC = Bayesian Information Criteria
SaBIC = Sample-Adjusted Bayesian Information Criteria
LL = Log Likelihood
BLRT = Bootstrapped likelihood ratio test
In the 3-class model, the largest class contained 73.9% (n = 726) of the participants in the total sample. This class was comprised of individuals who had a high probability of reporting heroin injection (81%) but low (<20%) probability of reporting injection of any of the other drugs. This class was named the Heroin-Dominant Injection class. The smallest class consisted of 9.5% (n = 93) of the total sample size. This class was comprised of individuals who had a 100% probability of reporting methamphetamine injection and 0% probability of reporting prescription opioid, speedball, crack-cocaine and fentanyl injection. In addition, this class had very low levels of heroin (10%) and cocaine (8%) injection, so this class was determined to be the Methamphetamine-Dominant Injection class. The final class consisted of 16.6% (n = 163) of the total sample. This class was comprised of individuals who reported a high probability of heroin (91%), cocaine (82%), speedball (71%) and crack-cocaine (40%) injection. This class also had the highest probabilities compared to the other classes for prescription opioids (9%) and fentanyl (28%) injection. Based on these posterior probabilities, this class was determined to be the Heroin/Cocaine Injection class (see Figure 1).
Figure 1.
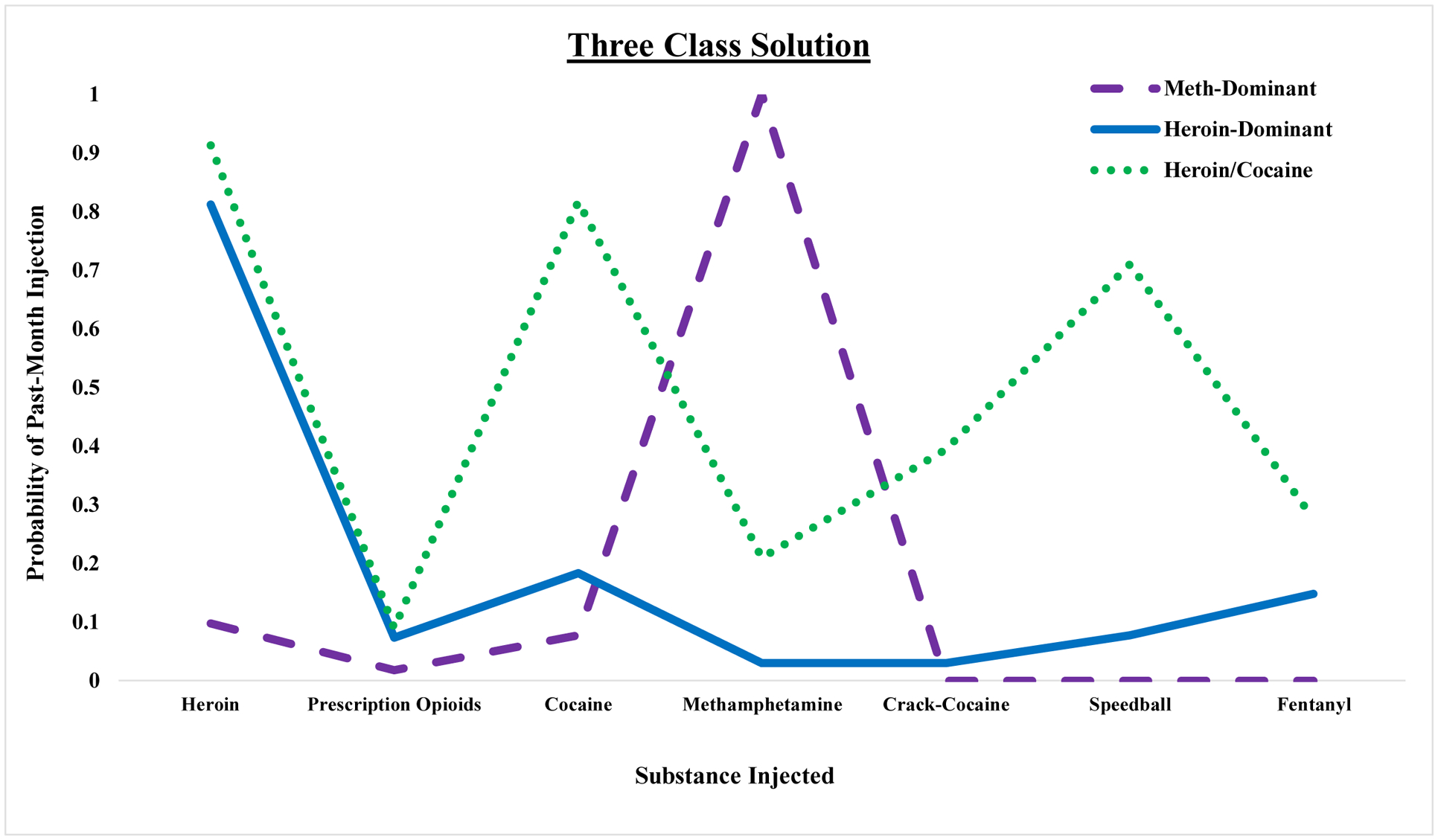
Three class solution for LCA of 982 syringe services program participants. Estimated probabilities for past-month substance injection are graphed on class membership.
Characteristics of the Latent Classes
3.3. Socio-Demographics
Table 3 provides the associations between membership in the three classes and sociodemographic characteristics. Compared to both the Heroin-Dominant (HD) Injection class and the Heroin/Cocaine (HC) Injection class, individuals in the Methamphetamine-Dominant (MD) Injection class were more likely to be male (ORMD/H=7.3 [2.4– 22.3], ORMD/HC=7.7 [2.4–25.0]), higher education (ORMD/HD=3.6 [2.0–6.3], ORMD/HC=5.1 [2.7–9.8]), higher income (ORMD/HD=1.9 [1.1–3.0], ORMD/HC=2.8 [1.6–5.1]), report gay or bisexual orientation (ORMD/HD=36.3 [19.4– 68.1], ORMD/HC=25.0 [12.5–50.0]) and less likely to be homeless (ORMD/HD=0.6 [0.3–0.96], ORMD/HC=0.19 [0.1–0.4]). The Methamphetamine-Dominant Injection class was more Hispanic (ORMD/HD=1.96 [1.2–3.2]) compared to the Heroin-Dominant Injection class and more likely to have private insurance (ORMD/HC=3.6 [1.5–8.3]) compared to the Heroin/Cocaine Injection class. Compared to the Heroin-Dominant Injection class, the Heroin/Cocaine Injection class was more likely to be homeless (ORHC/HD=2.9 [1.9–4.6]) and less likely to have private insurance (ORHC/HD=0.5 [0.2–0.98]).
Table 3.
Socio-Demographic, Injection risk, Sexual risk and HIV/HCV infection associations among injection substance use classesa
| Characteristic | Heroin/Cocaine Use vs. Heroin- Dominant Use | Methamphetamine-Dominant Use vs. Heroin-Dominant Use | Methamphetamine-Dominant Use vs. Heroin/Cocaine Use |
|---|---|---|---|
| Demographics | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| Age | 0.99 (0.97–1.01) | 1.01 (0.99–1.03) | 1.02 (0.99–1.04) |
| Gender (male vs. female) | 0.94 (0.59–1.51) | 7.34 (2.41–22.34) | 7.69 (2.44–25.00) |
| Race/Ethnicity | |||
| (Non-Hispanic Black vs. Non-Hispanic White) | 1.32 (0.51–3.41) | 1.12 (0.35–3.49) | 0.83 (0.22–3.23) |
| (Hispanic vs. Non-Hispanic White) | 1.47 (0.94–2.29) | 1.96 (1.21–3.15) | 1.33 (0.75–2.38) |
| Educational Attainment | 0.69 (0.45–1.06) | 3.57 (2.04–6.25) | 5.12 (2.68–9.78) |
| Annual Income | 0.66 (0.42–1.03) | 1.85 (1.14–3.03) | 2.81 (1.56–5.08) |
| Health Insurance | |||
| No Insurance | 1.35 (0.88–2.09) | 0.37 (0.23–0.61) | 0.27 (0.15–0.50) |
| Medicaid | 0.53 (0.24–1.16) | 1.03 (0.53–1.99) | 1.96 (0.76–5.00) |
| Medicare | 1.80 (0.79–4.12) | 1.48 (0.57–3.84) | 0.82 (0.28–2.38) |
| Private | 0.46 (0.22–0.98) | 1.63 (0.96–2.80) | 3.57 (1.54–8.33) |
| Experiencing homelessness | 2.94 (1.90–4.56) | 0.56 (0.32–0.96) | 0.19 (0.10–0.36) |
| Sexual Orientation | 1.38 (0.72–2.64) | 36.31 (19.35–68.11) | 25.00 (12.50–50.00) |
| Risk Behaviors | |||
| Ever Overdose | 1.50 (0.96–2.33) | 0.61 (0.38–0.98) | 0.41 (0.23–0.72) |
| Amount Injecting per day | 1.26 (0.82–1.94) | 0.52 (0.31–0.89) | 0.42 (0.23–0.77) |
| Reused syringes | 1.30 (0.78–2.15) | 0.17 (0.10–0.28) | 0.13 (0.07–0.25) |
| Sharing works | 2.78 (1.80–4.28) | 0.41 (0.22–0.78) | 0.15 (0.07–0.30) |
| Private (in home) injection | 0.52 (0.34–0.80) | 5.95 (2.83–12.49) | 11.11 (5.00–25.00) |
| Public injection (street, park) | 5.75 (3.58–9.25) | 0.38 (0.19–0.75) | 0.07 (0.03–0.14) |
| Unprotected Sex | 1.58 (1.03–2.41) | 4.60 (2.70–7.85) | 2.94 (1.56–5.56) |
| Sex with PWID | 1.93 (1.23–3.01) | 7.52 (4.51–12.51) | 3.85 (2.13–7.14) |
| Disease Status | |||
| HIV-positive | 1.09 (0.42–2.85) | 22.71 (12.47–41.38) | 20.00 (8.33–50.00) |
| HCV-positive | 1.73 (1.12–2.67) | 0.18 (0.09–0.36) | 0.10 (0.05–0.22) |
Note.
Associations are presented as unadjusted odds ratios with 95% confidence intervals
Note. Bolded values indicate p <0.05.
3.4. Risk behaviors
Drug and injection-related risk behaviors varied across all three classes. Compared to both the Heroin-Dominant Injection class and the Heroin/Cocaine Injection class, individuals in the Methamphetamine-Dominant Injection class were more likely to report injecting in a private home (ORMD/HD=6.0 [2.8– 12.5], ORMD/HC=11.1 [5.0–25.0]), unprotected sex (ORMD/HD=4.6 [2.7– 7.9], ORMD/HC=2.9 [1.6–5.6]) and sex with a PWID (ORMD/HD=7.5 [4.5–12.5], ORMD/HC=3.9 [2.1–7.1]). In addition, those in the Methamphetamine-Dominant Injection class were less likely to report ever overdosing (ORMD/HD=0.6 [0.4–0.98], ORMD/HC=0.4 [0.2–0.7]), injecting more than 7 times a day (ORMD/HD=0.5 [0.3–0.9], ORMD/HC=0.4 [0.2–0.8]), reusing their syringes (ORMD/HD=0.2 [0.1–0.3], ORMD/HC=0.1 [0.1–0.3]), sharing works (ORMD/HD=0.4 [0.2–0.8], ORMD/HC=0.2 [0.1–0.3]) and injecting in public (ORMD/HD=0.4 [0.2–0.8], ORMD/HC=0.1 [0.03–0.1]). Compared to the Heroin-Dominant Injection class, individuals in the Heroin/Cocaine Injection class were more likely to report sharing works (ORHC/HD=2.8 [1.8–4.3]), public injection (ORHC/HD=5.8 [3.6–9.3]), unprotected sex (ORHC/HD=1.6 [1.0–2.4]) and sex with a PWID (ORHC/HD=1.9 [1.2–3.0]). In addition, those in the Heroin/Cocaine Injection class were less likely to report injection in a private home (ORHC/HD=0.5 [0.3–0.8]) compared to Heroin-Dominant Injection class.
3.5. HIV/HCV status
HIV and HCV infection statuses varied greatly between the three classes. Sensitivity analysis results for self-report, biological testing, and combined measures are presented in Supplemental Table 1. The Heroin-Dominant Injection class had a baseline HIV and HCV prevalence of 6% and 46%, respectively; the Methamphetamine-Dominant Injection class had a baseline HIV and HCV prevalence of 53% and 14%, respectively; and the Heroin/Cocaine Injection class had a baseline HIV and HCV prevalence of 6% and 57%, respectively. Compared to both the Heroin-Dominant Injection class and the Heroin/Cocaine Injection class, those in the Methamphetamine-Dominant Injection class were more likely to be HIV positive (ORMD/HD=22.7 [12.5–41.4], ORMD/HC=20.0 [8.3–50.0]), but less likely to HCV positive (ORMD/HD=0.2 [0.1–0.4], ORMD/HC=0.1 [0.1–0.2]). In addition, the Heroin/Cocaine Injection class were more likely to be HCV positive (ORHC/HD=1.7 [1.1–2.7]) than the Heroin-Dominant Injection class.
3.6. Syringe Coverage between Classes
Table 4 provides the mean SSP visits and syringe coverage estimates between the three latent classes. Overall, the Heroin-Dominant Injection class had an average of 12.2 visits, followed by the Heroin/Cocaine Injection class (10.0) and the Methamphetamine-Dominant class (7.1). The lower mean coverage for the Methamphetamine-Dominant Injection class was 93.2% (SE=15.1%) and the upper mean coverage was 185.5% (SE=30.4%). The lower mean coverage for the Heroin/Cocaine Injection class was 24.7% (SE=6.3%) and the upper mean coverage was 34.6% (SE=8.8%). For the Heroin-Dominant Injection class, the lower mean coverage was 40.4% (SE=3.9%) and the upper mean coverage was 67.8 (SE=7.6%). The Methamphetamine-Dominant Injection class had higher mean coverage in the lower (χ2=17.40, p <0.001) and upper (χ2=22.69, p <0.001) estimates compared to the Heroin/Cocaine Injection class and the Heroin-Dominant Injection class [lower (χ2=11.11, p =0.001) and upper (χ2=13.75, p <0.001)]. Furthermore, the Heroin/Cocaine Injection class had a lower mean coverage whether measured as the lower cut-off of cells (χ2=3.83, p =0.05) or the upper cut-off (χ2=6.84, p =0.009) estimates compared to the Heroin-Dominant Injection class.
Table 4.
SSP visits and Syringe Coverage Estimates between Substance Use Latent Classes
| Variable | Meth-Dominant Use | Heroin/Cocaine Use | Heroin-Dominant Use |
|---|---|---|---|
| Number of Visits (mean, SE) | 7.09 (SE=1.14) | 10.0 (SE=1.87) | 12.2 (SE=0.87) |
| Lower Coverage Estimate (%, SE) | 93.2% (SE=15.1%) | 24.7% (SE=6.3%) | 40.4% (SE=3.9%) |
| Upper Coverage Estimate (%, SE) | 185.5% (SE=30.4%) | 34.6% (SE=8.8%) | 67.8% (SE=7.6%) |
| Class Comparisons | Lower Coverage (mean) | Chi-squared (χ2) | Upper Coverage (mean) | Chi-squared (χ2) |
|---|---|---|---|---|
| Meth-Dominant vs. Heroin/Cocaine | 93.2% vs. 24.7% | 17.40 (p<0.001) | 185.5% vs. 34.6% | 22.69 (p<0.001) |
| Meth-Dominant vs. Heroin-Dominant | 93.2% vs. 40.4% | 11.11 (p=0.001) | 185.5% vs. 67.8% | 13.75 (p<0.001) |
| Heroin/Cocaine vs. Heroin-Dominant | 24.7% vs. 40.4% | 3.83 (p=0.05) | 34.6% vs. 67.8% | 6.84 (p=0.009) |
4. DISCUSSION
This study provides important comparative data on the differences in demographic characteristics, risk behaviors and syringe coverage among PWID with different patterns of substances injected. Demographics are similar to other reports on PWID in Miami, with the majority male in their 30s. However, black PWID are underrepresented at the IDEA fixed site (Levine et al., 2019). Our experience in Miami has shown that mobile strategies are more effective in reaching the black PWID community (Iyengar et al., 2019). The Heroin-Dominant Injection class contained the majority of the Miami SSP participants. Compared to the other two classes, the smaller Methamphetamine-Dominant Injection class was much more likely to be men who have sex with men and from higher socioeconomic status. Additionally, the Methamphetamine-Dominant Injection class was more likely to be HIV positive at baseline while less likely to be HCV positive and share syringes, suggesting high-risk sexual behavior may be the driver of baseline HIV infection among this class. This observation is consistent with the longer half-life of methamphetamine requiring less frequent injection, as well as disinhibited sexual behavior and condomless anal intercourse which has a significant association with methamphetamine use and HIV infection (Forrest et al., 2010).
The Heroin/Cocaine Injection class appeared to have the riskiest drug use behaviors, and higher risk sexual behaviors than the Heroin-Dominant Injection class. Most importantly, compared to the Methamphetamine-Dominant Injection and Heroin-Dominant Injection classes, those in the Heroin/Cocaine Injection class were more likely to report syringe sharing and public injection location. Higher rates of overdose, receptive syringe sharing, and arrest (Hunter et al., 2018; Marshall, Kerr, Qi, Montaner, & Wood, 2010; Small, Rhodes, Wood, & Kerr, 2007) have been observed among PWID who inject in public. In addition, recent research has demonstrated that experiencing homelessness is a risk factor for public injection (Trayner et al., 2019). These findings suggest that harm reduction efforts targeted at these high-risk activities are needed among PWID who inject multiple substances. In addition to higher rates of overdose in the Heroin/Cocaine Injection class, 28% reported injection of fentanyl. Introduction of fentanyl and analogues into the drug supply in Miami in 2016 led to a sharp increase in opioid overdose deaths by 88% (FDLE, 2019). These findings highlight the critical need for policies authorizing SSPs and targeted naloxone distribution for individuals at higher risk of overdose.
Additionally, the Heroin/Cocaine Injection class was more likely to have HCV than the Heroin-Dominant Injection and Methamphetamine- Dominant Injection classes. This result is concerning because HCV infection is a harbinger for HIV infection among PWID who report injection equipment sharing (Ramachandran et al., 2018), suggesting need for a targeted approach to members of the Heroin/Cocaine Injection class. Furthermore, results of the syringe coverage estimate reveal that the majority of clients served at the IDEA SSP do not maintain sufficient coverage, with the lowest coverage of syringes among the Heroin/Cocaine Injection class. In addition, the Methamphetamine-Dominant Injection class had, on average, the fewest number of visits; however, they maintained the highest syringe coverage. This finding highlights the shortcomings of the existing strict one-for-one policy that applies statewide, and suggests the importance of implementing need-based syringe distribution policies at new and existing SSPs in order to decrease HIV acquisition due to syringe sharing (Bluthenthal et al., 2007; Kerr et al., 2010).
In the context of the recent HIV outbreaks in Massachusetts, Washington, Miami and Indiana (Cranston et al., 2019; Golden et al., 2019; Peters et al., 2016), our findings suggest that members of the Heroin/Cocaine Injection class have the highest risk of HIV acquisition due to syringe sharing and might require additional, targeted interventions to prevent HIV infection. PWID in the Heroin/Cocaine Injection class had the highest odds of being currently homeless, a risk factor consistent with the Seattle and Lowell/Lawrence outbreaks (Cranston et al., 2019; Golden et al., 2019). At the Miami SSP in 2018, after implementation of routine HIV/HCV screening every three months, there were seven confirmed acute HIV seroconversions leading to an epidemiologic investigation with the Florida Department of Health. All of the acute cases investigated reported use of multiple substance, including speedball (Tookes et al., 2019). Cities that already have harm reduction programs such as SSPs could benefit from increased HIV testing, outreach and, importantly, need-based syringe distribution policies to people experiencing homelessness and people who inject multiple substances, and this multicomponent prevention strategy may help mitigate HIV outbreaks.
4.1. Limitations
There are several limitations to this study. First, the LCA focuses on a single SSP in one city and may not be directly generalizable to other settings. However, the identification of these classes may be helpful to other jurisdictions experiencing HIV outbreaks in similar patient populations. Second, the data is self-report and subject to social desirability and recall bias. In this case the data was anonymous and surveys were conducted by trusted SSP staff in confidential settings, limiting potential bias in our study. Additionally, although HIV and HCV status were determined by rapid test or by self-report, 67% of participants had a HIV rapid antibody test at baseline and 61% had an HCV rapid antibody test, and sensitivity analysis revealed measure stability. Importantly, HCV antibody testing only indicated exposure to HCV and chronic HCV infection was not confirmed, but exposure is indicative of risk as determined by this behavioral analysis. Finally, we only measured seven different drugs to generate the injection drug use classes, which may not capture all drugs being injected among this population. In addition, non-injection related drug use indicators were not collected by the SSP, which could provide more information regarding drug use. However, insufflation and smoking of substances has decreased risk of HCV compared to IDU and no risk of HIV transmission (Scheinmann et al., 2007). Nonetheless, taken together, this LCA suggests the potential importance of interventions tailored to different groups of PWID to effectively respond to the current substance use crisis.
5. CONCLUSIONS/IMPLICATIONS
The application of LCA and other advanced research techniques can help shed light on at-risk groups in order to inform syringe distribution policies and potential interventions. The injection risk profiles and syringe coverage varied between the classes, presenting a potential need for targeted prevention strategies and increased need for reform to the strict one-for-one syringe exchange policy at the state level. The overall goal for SSPs is to provide as close to 100% syringe coverage as possible to all clients served to protect against HIV and HCV infection. Other syringe transaction policies, such as needs-based syringe exchange, need to be implemented through policy reform in order to provide sufficient coverage to SSP clients.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Alpren C, Dawson EL, John B, Cranston K, Panneer N, Fukuda HD, …Peters PJ (2020). Opioid Use Fueling HIV Transmission in an Urban Setting: An Outbreak of HIV Infection Among People Who Inject Drugs—Massachusetts, 2015–2018. American journal of public health(0), e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asparouhov T, & Muthén B (2012). Using Mplus TECH11 and TECH14 to test the number of latent classes. Mplus Web Notes, 14, 22. [Google Scholar]
- Asparouhov T, & Muthén B (2014). Auxiliary variables in mixture modeling: Using the BCH method in Mplus to estimate a distal outcome model and an arbitrary secondary model. Mplus Web Notes, 21(2), 1–22. [Google Scholar]
- Baral S, Holland CE, Shannon K, Logie C, Semugoma P, Sithole B, … Beyrer C (2014). Enhancing benefits or increasing harms: community responses for HIV among men who have sex with men, transgender women, female sex workers, and people who inject drugs. JAIDS Journal of Acquired Immune Deficiency Syndromes, 66, S319–S328. [DOI] [PubMed] [Google Scholar]
- Barocas JA, Baker L, Hull SJ, Stokes S, & Westergaard RP (2015). High uptake of naloxone-based overdose prevention training among previously incarcerated syringe-exchange program participants. Drug and Alcohol Dependence, 154, 283–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluthenthal RN (2001). Factors associated with readiness to change drug use among needle-exchange users. Drug and Alcohol Dependence, 62(3), 225–230. [DOI] [PubMed] [Google Scholar]
- Bluthenthal RN, Anderson R, Flynn NM, & Kral AH (2007). Higher syringe coverage is associated with lower odds of HIV risk and does not increase unsafe syringe disposal among syringe exchange program clients. Drug and Alcohol Dependence, 89(2–3), 214–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. (2019). HIV Surveillance Report, 2018.
- Celeux G, & Soromenho G (1996). An entropy criterion for assessing the number of clusters in a mixture model. Journal of classification, 13(2), 195–212. [Google Scholar]
- Cranston K, Alpren C, John B, Dawson E, Roosevelt K, Burrage A, … Peters PJ (2019). Notes from the Field: HIV Diagnoses Among Persons Who Inject Drugs—Northeastern Massachusetts, 2015–2018. Morbidity and Mortality Weekly Report, 68(10), 253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham EB, Jacka B, DeBeck K, Applegate TL, Harrigan PR, Krajden M, … Olmstead AD (2015). Methamphetamine injecting is associated with phylogenetic clustering of hepatitis C virus infection among street-involved youth in Vancouver, Canada. Drug and Alcohol Dependence, 152, 272–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FDLE. (2019). Drugs Identified in Deceased Persons by Florida Medical Examiners.
- Feaster DJ, Parish CL, Gooden L, Matheson T, Castellon PC, Duan R, … Malotte CK (2016). Substance use and STI acquisition: Secondary analysis from the AWARE study. Drug and Alcohol Dependence, 169, 171–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng ZD, & McCulloch CE (1996). Using bootstrap likelihood ratios in finite mixture models. Journal of the Royal Statistical Society: Series B (Methodological), 58(3), 609–617. [Google Scholar]
- Fernandes RM, Cary M, Duarte G, Jesus G, Alarcão J, Torre C, … Carneiro AV (2017). Effectiveness of needle and syringe Programmes in people who inject drugs–An overview of systematic reviews. BMC public health, 17(1), 309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest DW, Metsch LR, LaLota M, Cardenas G, Beck DW, & Jeanty Y (2010). Crystal methamphetamine use and sexual risk behaviors among HIV-positive and HIV-negative men who have sex with men in South Florida. Journal of Urban Health, 87(3), 480–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gicquelais RE, Genberg BL, Astemborski J, Celentano DD, Kirk GD, & Mehta SH (2019). Association of Injection Practices and Overdose With Drug Use Typologies: A Latent Class Analysis Among People Who Inject Drugs in Baltimore, 2017. AIDS education and prevention, 31(4), 344–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden MR, Lechtenberg R, Glick SN, Dombrowski J, Duchin J, Reuer JR, … Buskin SE (2019). Outbreak of Human Immunodeficiency Virus Infection Among Heterosexual Persons Who Are Living Homeless and Inject Drugs—Seattle, Washington, 2018. Morbidity and Mortality Weekly Report, 68(15), 344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrell PT, Mancha BE, Petras H, Trenz RC, & Latimer WW (2012). Latent classes of heroin and cocaine users predict unique HIV/HCV risk factors. Drug and Alcohol Dependence, 122(3), 220–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics, 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter K, Park JN, Allen ST, Chaulk P, Frost T, Weir BW, & Sherman SG (2018). Safe and unsafe spaces: non-fatal overdose, arrest, and receptive syringe sharing among people who inject drugs in public and semi-public spaces in Baltimore City. International Journal of Drug Policy, 57, 25–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyengar S, Kravietz A, Bartholomew TS, Forrest D, & Tookes HE (2019). Baseline differences in characteristics and risk behaviors among people who inject drugs by syringe exchange program modality: an analysis of the Miami IDEA syringe exchange. Harm reduction journal, 16(1), 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr T, Shannon K, Ti L, Strathdee S, Hayashi K, Nguyen P, … Wood E (2016). Sex work and HIV incidence among people who inject drugs. AIDS (London, England), 30(4), 627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr T, Small W, Buchner C, Zhang R, Li K, Montaner J, & Wood E (2010). Syringe sharing and HIV incidence among injection drug users and increased access to sterile syringes. American journal of public health, 100(8), 1449–1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuramoto S, Bohnert A, & Latkin C (2011). Understanding subtypes of inner-city drug users with a latent class approach. Drug and Alcohol Dependence, 118(2–3), 237–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leri F, Stewart J, Tremblay A, & Bruneau J (2004). Heroin and cocaine co-use in a group of injection drug users in Montreal. Journal of Psychiatry and Neuroscience, 29(1), 40. [PMC free article] [PubMed] [Google Scholar]
- Levine H, Bartholomew TS, Rea-Wilson V, Onugha J, Arriola DJ, Cardenas G, … Spencer E (2019). Syringe disposal among people who inject drugs before and after the implementation of a syringe services program. Drug and Alcohol Dependence. [DOI] [PMC free article] [PubMed]
- Marshall BD, Kerr T, Qi J, Montaner JS, & Wood E (2010). Public injecting and HIV risk behaviour among street-involved youth. Drug and Alcohol Dependence, 110(3), 254–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCutcheon AL (1987). Latent class analysis: Sage. [Google Scholar]
- Meacham MC, Roesch SC, Strathdee SA, Lindsay S, Gonzalez-Zuniga P, & Gaines TL (2018). Latent classes of polydrug and polyroute use and associations with HIV risk behaviours and overdose among people who inject drugs in Tijuana, Baja California, Mexico. Drug and alcohol review, 37(1), 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meacham MC, Rudolph AE, Strathdee SA, Rusch ML, Brouwer KC, Patterson TL, … Roesch SC (2015). Polydrug use and HIV risk among people who inject heroin in Tijuana, Mexico: A latent class analysis. Substance use & misuse, 50(10), 1351–1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monga N, Rehm J, Fischer B, Brissette S, Bruneau J, El-Guebaly N, … Leri F (2007). Using latent class analysis (LCA) to analyze patterns of drug use in a population of illegal opioid users. Drug and Alcohol Dependence, 88(1), 1–8. [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthen B (2017). Mplus user’s guide: Statistical analysis with latent variables, user’s guide: Muthén & Muthén. [Google Scholar]
- Noor SW, Ross MW, Lai D, & Risser JM (2014). Use of latent class analysis approach to describe drug and sexual HIV risk patterns among injection drug users in Houston, Texas. AIDS and behavior, 18(3), 276–283. [DOI] [PubMed] [Google Scholar]
- Peters PJ, Pontones P, Hoover KW, Patel MR, Galang RR, Shields J, … Switzer WM (2016). HIV infection linked to injection use of oxymorphone in Indiana, 2014–2015. New England Journal of Medicine, 375(3), 229–239. [DOI] [PubMed] [Google Scholar]
- Ramachandran S, Thai H, Forbi JC, Galang RR, Dimitrova Z, Xia G. l., … Gentry J (2018). A large HCV transmission network enabled a fast-growing HIV outbreak in rural Indiana, 2015. EBioMedicine, 37, 374–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg ES, Rosenthal EM, Hall EW, Barker L, Hofmeister MG, Sullivan PS, … Ryerson AB (2018). Prevalence of hepatitis C virus infection in US states and the District of Columbia, 2013 to 2016. JAMA network open, 1(8), e186371–e186371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schackman BR, Fleishman JA, Su AE, Berkowitz BK, Moore RD, Walensky RP, … Weinstein MC (2015). The lifetime medical cost savings from preventing HIV in the United States. Medical care, 53(4), 293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheinmann R, Hagan H, Lelutiu-Weinberger C, Stern R, Des Jarlais DC, Flom PL, & Strauss S (2007). Non-injection drug use and hepatitis C virus: a systematic review. Drug and Alcohol Dependence, 89(1), 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider KE, O’Rourke A, White RH, Park JN, Musci RJ, Kilkenny ME, … Allen ST (2020). Polysubstance use in rural West Virginia: Associations between latent classes of drug use, overdose, and take-home naloxone. International Journal of Drug Policy, 76, 102642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Small W, Rhodes T, Wood E, & Kerr T (2007). Public injection settings in Vancouver: physical environment, social context and risk. International Journal of Drug Policy, 18(1), 27–36. [DOI] [PubMed] [Google Scholar]
- Tavitian-Exley I, Boily M-C, Heimer R, Uusküla A, Levina O, & Maheu-Giroux M (2018). Polydrug use and heterogeneity in HIV risk among people who inject drugs in Estonia and Russia: a latent class analysis. AIDS and behavior, 22(4), 1329–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavitian-Exley I, Maheu-Giroux M, Platt L, Heimer R, Uusküla A, Levina O, … Boily M-C (2018). Differences in risk behaviours and HIV status between primary amphetamines and opioid injectors in Estonia and Russia. International Journal of Drug Policy, 53, 96–105. [DOI] [PubMed] [Google Scholar]
- Tavitian-Exley I, Vickerman P, Bastos FI, & Boily MC (2015). Influence of different drugs on HIV risk in people who inject: systematic review and meta-analysis. Addiction, 110(4), 572–584. [DOI] [PubMed] [Google Scholar]
- Tookes H, Bartholomew TS, Geary S, Matthias J, Poschman K, Blackmore C, … Rodriguez AE (2019). Rapid Identification and Investigation of an HIV Risk Network Among People Who Inject Drugs–Miami, FL, 2018. AIDS and behavior, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trayner KM, McAuley A, Palmateer NE, Goldberg DJ, Shepherd SJ, Gunson RN, … Hutchinson SJ (2019). Increased risk of HIV and other drug-related harms associated with injecting in public places among people who inject drugs in Scotland: a national bio-behavioural survey. The Lancet, 394, S91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trenz RC, Scherer M, Duncan A, Harrell PT, Moleko AG, & Latimer WW (2013). Latent class analysis of polysubstance use, sexual risk behaviors, and infectious disease among South African drug users. Drug and Alcohol Dependence, 132(3), 441–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voon P, Hayashi K, Ti L, Kaplan K, Suwannawong P, Wood E, & Kerr T (2015). High prevalence of syringe lending among HIV-positive people who inject drugs in Bangkok, Thailand. Harm reduction journal, 12(1), 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrieze SI (2012). Model selection and psychological theory: a discussion of the differences between the Akaike information criterion (AIC) and the Bayesian information criterion (BIC). Psychological methods, 17(2), 228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zibbell JE, Asher AK, Patel RC, Kupronis B, Iqbal K, Ward JW, & Holtzman D (2018). Increases in acute hepatitis C virus infection related to a growing opioid epidemic and associated injection drug use, United States, 2004 to 2014. American journal of public health, 108(2), 175–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zibbell JE, Iqbal K, Patel RC, Suryaprasad A, Sanders KJ, Moore-Moravian L, … Holtzman D (2015). Increases in hepatitis C virus infection related to injection drug use among persons aged≤ 30 years—Kentucky, Tennessee, Virginia, and West Virginia, 2006–2012. MMWR. Morbidity and mortality weekly report, 64(17), 453. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


