Abstract
There has been rapid growth in teledermatology over the past decade and teledermatology services are increasingly being utilized to support patient care across a variety of care settings. Teledermatology has the potential to increase access to high quality dermatologic care while maintaining clinical efficacy and cost-effectiveness. Recent expansions in telemedicine reimbursement from the Centers for Medicare & Medicaid Services (CMS) ensure that teledermatology will play an increasingly prominent role in patient care. Therefore, it is important that dermatologists are well-informed of both the promises of teledermatology and the potential practice challenges a continuously evolving mode of care delivery brings. In this article, we will review the evidence on the clinical and cost-effectiveness of teledermatology and we will discuss system-level and practice-level barriers to successful teledermatology implementation as well as potential implications for dermatologists.
Introduction
In the United States, there is a growing demand for dermatologic services but a shortage and maldistribution of dermatologists nationwide.1 Teledermatology is an innovative and evolving model of care delivery with the potential to increase access to high quality dermatologic care. There has been rapid growth in teledermatology over the past decade: according to a national survey conducted by the American Telemedicine Association, there were 102 active programs in 2016, representing a substantial increase from the 37 active programs in 2011.2 In this article – part of a health policy series reviewing a wide-range of policy topics impacting clinical dermatology3 – we will briefly describe the clinical effectiveness and potential pitfalls of teledermatology, review the evidence regarding the cost-effectiveness of teledermatology programs, and discuss the health-policy issues surrounding the adoption and reimbursement of teledermatology services.
Clinical effectiveness of teledermatology
Teledermatology services can be delivered through either a store-and-forward or a live-interactive format. Currently, store-and-forward is most popular due to its lower cost, greater flexibility in coordination, and ability to leverage technological advances in teledermoscopy and web platforms for the secure transmission of high quality images.4 Both formats can be applied between a referring clinician and a consulting dermatologist as a provider-to-provider model (for new or established patients), or between an established patient and a dermatologist as a provider-to-patient model.1 Provider-to-patient models for new patients have also grown in popularity; however, there is a lack of needed regulation to ensure high quality care standards for proper clinical history, documentation, prescribing practices, and follow-up as outlined by the American Academy of Dermatology.5,6 For these reasons, this article is focused on provider-to-provider models or provider-to-patient models for established patients only.
Several studies report a moderate to high degree of diagnostic and management concordance between teledermatology and conventional in-person dermatologic visits. Concordance reports for the primary diagnosis and management of dermatologic disorders and cutaneous malignancies range from 60–100%.1,2 In addition, evidence suggests that teledermatology may be equally effective as conventional care for the management of previously diagnosed chronic inflammatory skin disease, such as atopic dermatitis and psoriasis.5 A 2018 randomized clinical equivalency trial among patients with psoriasis found that an online collaborative health model resulted in equivalent improvements in clinical outcomes compared to a conventional in-person model,4 and a 2015 study among patients with atopic dermatitis reported similar findings.7
Cost-effectiveness of teledermatology
The literature evaluating the economic impact of teledermatology is limited, but most studies suggest that teledermatology may be cost-effective. To evaluate the economic impact of teledermatology, it is useful to establish an economic framework for analysis. There are two perspectives to consider, the first of which is the health care system. Relevant costs may include equipment and staff costs of an in-person visit versus a teledermatology service. The second broader perspective to consider is that of the patient and society, where additional relevant costs may include transportation costs, lost work productivity, and drawbacks of a delayed diagnosis.
We will first review the evidence concerning the economic impact of teledermatology from the perspective of the health care system. Teledermatology may allow greater efficiency in case triage: dermatologists can either return patients to the referring clinician with feedback for management or arrange for further in-person evaluation. Given the reduced costs of teledermatology encounters compared to in-person visits (approximately $10-$80 less per visit for the former), teledermatology can be cost-saving by reducing in-person visits.8 A 2018 study of a store-and-forward teledermatology program in Bages, Spain found that teledermatology saved 4,502 visits over a year, and inclusive of all direct costs, saved £10,350 (US$12,452) per year as compared to a conventional in-person referral model.9 In a single general practice in suburban London, by reducing the number of secondary in-person visits, a store-and-forward teledermatology program for benign-appearing skin lesions saved £12,460 (US$15,015) over 3 years.10 Across the entire United States health system, these savings have the potential to be significant. For example, if 5% of the 35 million annual office-based visits to dermatologists could be shifted to teledermatology visits at a savings of $20 per encounter, healthcare costs could potentially be reduced by $35 million annually.
Another benefit is that through greater efficiency in case triage, teledermatology may improve access for patients with the highest clinical acuity.9 By improving access to timely care, teledermatology can reduce the number of avoidable urgent care or emergency room visits.8,11 A 2018 study found that a store-and-forward teledermatology program serving an underserved population in Philadelphia reduced in-person dermatology visits by 27% and emergency room visits by 3.3% by providing care plans to local providers that resulted in improve skin disease in patients. This program saved $10.00-$52.65 per consult as compared to conventional in-person care.8 Finally, given that several studies have identified considerable discordance in the management of patients between referring clinicians and dermatologists, teledermatology could be cost-saving by enabling earlier initiation of appropriate therapy, although further studies are needed.8,12
Next, we review the evidence concerning the economic impact of teledermatology from the broader societal perspective. The previously discussed study conducted in Bages, Spain found that societal savings had the greatest impact on the overall cost-effectiveness of teledermatology, saving £40,814 per year (US$48,415).9 A study in New Zealand found that live-interactive teledermatology was more cost-effective than conventional care, largely driven by savings to the patient and society.13 A 2015 study conducted in a Veterans Affairs (VA) Hospital setting found that from the VA perspective, a store-and-forward teledermatology referral process was comparable in cost to a conventional referral process, but from a societal perspective, teledermatology was less costly.14 Similarly, in a Department of Defense setting, store-and-forward teledermatology was more expensive when considering direct costs only, but cost-saving when factoring in lost productivity.15 Additional considerations from the societal perspective include costs to companions who accompany the patient, costs of lost leisure time, and teledermatology-associated educational benefits to clinicians, all of which favor teledermatology to be more cost-effective.9,16,17
Teledermatology may be especially cost-effective for specific patient populations, such as patients who live farther away from specialist care or patients with dermatologic diseases that can be ultimately managed by their primary care physician.18 A study of a store-and-forward teledermatology program conducted in the Netherlands found that while teledermatology was £33 (US$39) more expensive per consult, when applied to specific patient groups with greater travel times and diseases generating a greater proportion of preventable referrals, teledermatology can be cost-effective.12 A 2001 study conducted in the UK evaluating live-interactive teledermatology reported similar results.16 However, for other populations, teledermatology may not be cost-effective. For instance, potential skin cancer cases may be an example of a patient group best suited for conventional in-person care as a large proportion of patients may ultimately require clinic visits for biopsy procedures, generating redundant care.19 A 2018 study conducted in Australia found that teledermoscopy for skin cancer referral cost A$54.6 (US$37) more per case as compared to conventional in-person care, but resulted in clinical resolution 26 days sooner.11 A 2003 study conducted in the US reported similar findings.20 Of note, both studies did not factor in indirect savings to society, and the increase in direct costs may be justifiable for the cost savings and improved quality of life associated with earlier care access and disease management.11,16,21 However, a potential pitfall of teledermatology based on a specific lesion of concern in the absence of a full-body skin examination is underdiagnosis of skin cancer if the referring clinician misses other clinically significant lesions.22 In summary, the literature evaluating the economic consequences of teledermatology is limited but suggest that teledermatology may be cost-effective, especially when applied to certain patient populations, such as those with poor access to dermatologic care (Table 1). Additional comprehensive economic studies are warranted to identify the settings in which teledermatology can be cost-effective and beneficial to the patient and those in which it is not.
Table 1:
Teledermatology (TD) Cost-Effectiveness Studies
| Author(s) | Year | Population | Modality Type | Method | Outcome |
|---|---|---|---|---|---|
| Wootton et al. | 2000 | UK: four health centers, two regional hospitals | Live-interactive | RCT | TD was more costly compared to conventional care (£132.1 vs. £48.7, US$159 vs. US$59). TD can be cost-saving in settings with greater traveling distances and lower equipment prices. No major differences in clinical outcomes. |
| Loane et al. | 2001 | New Zealand: rural health centers | Live-interactive | RCT | TD was less costly compared to conventional care from a societal perspective comparing total costs (NZ$279.2 vs. NZ$283.8, US$176 vs. US$179) and marginal costs (NZ$135 vs. NZ$284, US$85 vs. US$179) |
| Whited et al. | 2003 | US: unspecified | Store-and-forward | RCT | TD was more costly compared to conventional care but decreased time to treatment. TD can be cost-saving in settings with longer wait times. |
| Pak et al. | 2009 | Texas: Department of Defense affiliated clinics | Store-and-forward | RCT | TD was more costly compared to conventional care considering direct costs only ($294 vs. $283). Factoring in productivity loss, TD was cost-saving ($340 vs. $372). |
| Eminovic et al. | 2010 | Almere, Netherlands & Zeist, Netherlands: general district hospitals | Store-and-forward | RCT | TD was €32.5 (US$36) more costly compared to conventional care. TD can be cost-saving if distance to dermatologist is larger or when more consultations can be avoided. |
| Datta et al. | 2015 | Columbia, MO & Minneapolis, MN: two VA medical facilities | Store-and-forward | RCT | TD was similar in cost compared to conventional care considering direct costs only. Factoring in societal costs, TD was cost-saving. No evidence of difference in utility. |
| Livingston and Solomon | 2015 | Suburban Greater London: single general practice | Store-and-forward | Retrospective analysis | TD saved £12,460 (US$15,015) over a 3-year period by reducing secondary in-person visits. Patient satisfaction was high. |
| Snoswell et al. | 2018 | Australia | Store-and-forward | Retrospective analysis | Teledermoscopy for skin cancer referral and triage was A$54.6 (US$37) more costly but resulted in clinical resolution 26 days sooner |
| Vidal-Alaball et al. | 2018 | Bages, Spain: 14 primary health care teams | Store-and- forward | Retrospective analysis | TD saved £10,350 (US$12,452) per year in direct costs and £51,164 (US$61,555) in societal costs. Societal savings were most significant. |
| Yang et al. | 2018 | Philadelphia: underserved population in city health clinics | Store-and-forward | Retrospective analysis | 27% of in-person visits and 3.3% of ER visits were avoided using TD. TD had cost savings of $10.00-$52.65 per consult. |
Health Policy Challenges and Barriers to Adoption
Though teledermatology is increasingly being utilized to support patient care, many obstacles remain, hindering widespread adoption. First, providers face high barriers to adoption. Implementation and maintenance costs of a teledermatology program are significant and include equipment costs, technological competencies, and staff training. A secure network for the transmission and storage of confidential patient data and images is essential, and data should be protected to safeguard patient privacy.23 A mechanism that links transmitted patient information with data from a patient’s electronic health record is needed to support final decisions regarding diagnosis and management.23–25 In addition, staff training on proper imaging and taking a relevant medical history is necessary.24 Finally, as teledermatology programs depend on imaging and/or videoconferencing systems, the quality and reliability of the communications technology is important, and so far there exists no universal imaging, equipment, or technique standards.23 The implementation of quality and sustainable processes are critical to the success and cost-effectiveness of any teledermatology program.
Medicolegal issues also pose considerable challenges. Dermatologists often cite legal risks as a point of concern, and questions of legal responsibility in cases of incorrect diagnosis and management remains ambiguous.23 However, malpractice risk has not yet been well-characterized. While a recent 2019 study found zero reported cases of medical malpractice against direct-to-patient telemedicine, and a 2015 study on primary care providers’ perceptions found that 94% did not perceive mobile store-and-forward teledermatology to increase medical liability, malpractice cases will inevitably arise in the future.26–28 A related challenge is that patient privacy is put at risk through the capturing, transmission, and storage of clinical images, especially as personal smartphones and devices are increasingly being used for these purposes. Failure to ensure Health Insurance Portability and Accountability Act (HIPAA) compliance with images and failure to follow appropriate security precautions could expose providers to legal penalities.29 Finally, a comprehensive federal regulatory framework addressing these telehealth privacy and security risks has yet to be established.30 For best practice, providers should be sure to obtain patient consent for taking images, explain how the images will be used, and ensure HIPAA-compliant security in image storage and transmission.31
Likely the most significant barrier to the widespread adoption of teledermatology is the lack of reliable systems for reimbursement. Teledermatology programs depend on sustainable business models, and different models such as capitated service contracts, per-case service contracts, direct-to-consumer, and standard fee-for-service reimbursement have been implemented in various care settings.32 Currently, self-pay is the most frequent method of payment for teledermatology services.2 Medicare, Medicaid, and some private payers offer some form of reimbursement; however, reimbursement policies vary by state and payer, change frequently, and generally, there is a lack of parity in reimbursement or federal funding to support teledermatology programs.1,33,34 Given the significant adoption and maintenance costs, without reliable mechanisms for reimbursement, providers may lose money by participating in teledermatology. This creates a strong disincentive for provider participation when performing similar work offers greater reimbursement and less uncertainty with regard to potential medico-legal risks.
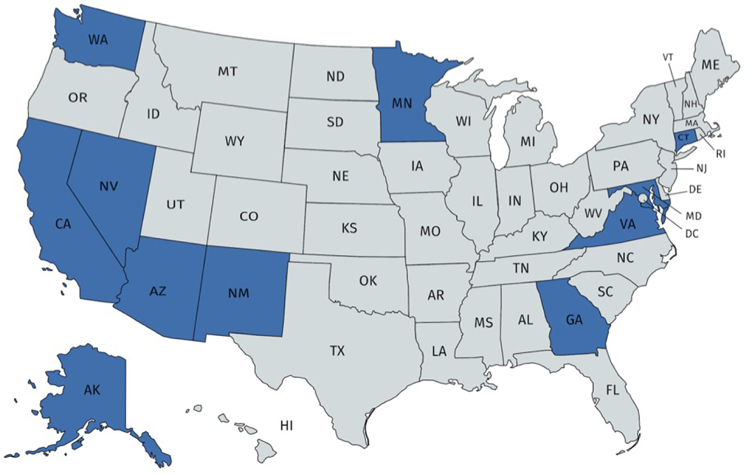
As the United States’ largest health care payer and model for the private payer system, policies from the Center of Medicare & Medicaid Services (CMS) have important implications for the future of teledermatology. Among Medicare beneficiaries, telemedicine utilization is on the rise: between 2014 and 2016, 275,000 telehealth services were provided to almost 90,000 beneficiaries.35 However, until recently, restrictive rules have rendered reimbursement a challenge. Excluding CMS demonstration projects in Alaska and Hawaii, telemedicine reimbursement was only available for services delivered via live-interactive format. Geographic restrictions limited reimbursement to patients residing in federally designated rural areas and originating site restrictions required patients to travel to valid originating sites such as a physician’s office, hospital, or health facility. Notably, a patient’s home was not considered a valid originating site.34 These restrictions have prevented many underserved populations from receiving care, especially elderly, disabled, and American Indian populations where geographic and physical limitations pose major barriers to in-person care, and where telemedicine may prove especially valuable to reduce disparities in access.36, 37. Regarding Medicaid, telehealth coverage varies by state. In most states, only live-interactive format is reimbursable, and only 11 states reimburse store-and-forward services (Figure 1). Similar to Medicare, many states also have geographic and originating site restrictions.38
Figure 1:
States Providing Medicaid Reimbursement for Store-and-Forward Teledermatologya
a States in dark blue include: Alaska, Arizona, Connecticut, California, Georgia, Maryland, Minnesota, New Mexico, Nevada, Virginia, Washington41
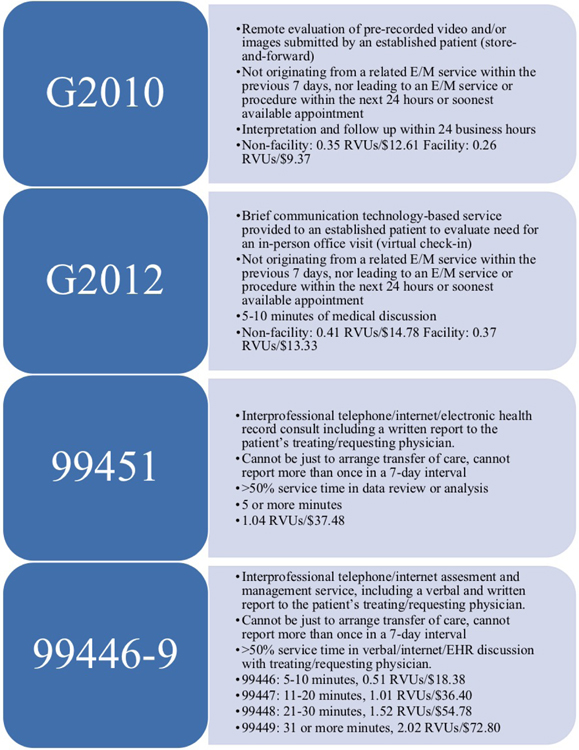
Despite these challenges, the future of teledermatology is promising, and CMS is beginning to relax previous restrictions to promote telehealth adoption. Starting in the 2020 plan year, telehealth geographic restrictions in Medicare Advantage plans will be eliminated, enabling patients residing in urban areas to receive services, and from their own homes.39 In 2019, virtual patient check-ins, consultations between physicians, and of special significance, remote evaluation of pre-recorded patient information, became eligible for Medicare reimbursement. Although reimbursement for these services are lower than expected (Figure 2), these changes still represent a significant step towards acceptance of store-and-forward services. CMS has expressed that expansion of telehealth reimbursement is a top priority, and it recognizes that telehealth can augment the goals of a value-driven healthcare system by providing high quality, convenient care.31 With an expanding Medicare and Medicaid population and a relative shortage of physicians, the need to embrace technology and innovation to improve care access is greater than ever. However, until payers and policymakers implement more reliable methods for reimbursement, the full potential benefits and cost savings associated with teledermatology remain to be realized.36
Figure 2:
New 2019 Medicare Communication Technology HCPCS Codes and RVU/Reimbursement Amountsa
a These services are not considered Medicare telehealth services and thus are not subject to geographic restrictions (patients must reside in federally designated rural areas) and originating site restrictions (patients must travel to valid originating sites such a provider office, hospital, or health facility).
E/M: evaluation and management; RVUs: relative value units
While expansion of teledermatology services has several potential benefits, one concern is that expanded access to teledermatology could increase the volume of total dermatologic visits. However, evidence from previous expansions suggests that this is unlikely to occur. A 2016 study found that after a California Medicaid managed care plan began reimbursing for a teledermatology program incorporating both consultative and direct care elements, the number of dermatologic visits of any type was 60.1 vs 64.6 per 1000 enrollees in practices that did not use teledermatology versus those that did use teledermatology, respectively. This was a small, yet statistically significant increase in visits; however, the service filled a large unmet need for dermatologic care among Medicaid enrollees. Furthermore, teledermatology services generally served a younger patient population with more benign skin conditions, and patients with neoplastic processes and severe diseases were able to see an in-person dermatologist more easily.40 In addition, a 2018 study reported that a state-wide implementation of Medicaid-funded store-and-forward consultative teledermatology in Connecticut did not lead to a significant change in the volume of consultations.21
In summary, to encourage widespread adoption and provider participation in high quality teledermatology, more uniform reimbursement policies by the government and private payers need to be implemented. For dermatologists, specific recommendations include establishing best-practice standards, providing education on teledermatology adoption and use, and being aware of potential practice pitfalls (Table 2).
Table 2:
Potential Teledermatology Practice Pitfalls
|
Inability to properly diagnose - Inadequate information sent (insufficient history, lack of context) - Inability to palpate lesions or perform complete physical exam - Poor quality or wrong clinical photographs (out of focus, inadequate number, bias with regard to which lesions were photographed) - Lack of imaging, equipment, or technique standards - Lack of access to prior medication records |
|
Inability to complete the circle of care - Lack of continuity and/or longitudinal care - Inability to see the patient in person if needed - Inability or difficulty in preforming diagnostic or lab tests - Lack of communication with primary care providers - Lack of integration into health systems |
|
Policy and legal risk - Medico-legal/malpractice risk - Security breaches - HIPAA violations |
|
Reimbursement for services/costs - Lack of universal payment through Centers for Medicare & Medicaid Services in all states - Lack of universal private payer parity - Adoption and maintenance costs for individual systems |
Conclusion
There is a growing demand for dermatologic services and a shortage of dermatologists to meet this need. This lack of access, especially pronounced in rural and underserved populations, results in worse clinical outcomes, reduced quality of life, and increased health care costs.7 Evidence supports that teledermatology may be an effective, convenient, and cost-effective model of care delivery to improve access to care and patient satisfaction when implemented properly. To encourage provider participation in high quality teledermatology, future efforts should prioritize the implementation of reliable systems for appropriate reimbursement and the mitigation of potential medico-legal risks. Finally, as evidence suggests that certain patient populations may be more or less well-suited for teledermatology, additional research into how and in what settings teledermatology can be most effective is warranted in order to appreciate both the benefits and limitations of teledermatology.
Acknowledgments
Funding Sources: Dr. Barbieri is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under award number T32-AR-007465 and receives partial salary support through a Pfizer Fellowship grant to the Trustees of the University of Pennsylvania.
Robert Stavert receives salary compensation as a part-time employee for Philips.
Abbreviations Used
- CMS
Center of Medicare & Medicaid Services
- HIPAA
Health Insurance Portability and Accountability Act
- VA
Veterans Affairs
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosure: We have no other conflicts to disclose.
References
- 1.Campagna M, Naka F, Lu J. Teledermatology: An updated overview of clinical applications and reimbursement policies. Int J Womens Dermatol. 2017;3(3):176–179. doi: 10.1016/j.ijwd.2017.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yim KM, Florek AG, Oh DH, McKoy K, Armstrong AW. Teledermatology in the United States: An Update in a Dynamic Era. Telemed J E-Health Off J Am Telemed Assoc. 2018;24(9):691–697. doi: 10.1089/tmj.2017.0253 [DOI] [PubMed] [Google Scholar]
- 3.Nguyen HP, Barbieri JS, Forman HP, Bolognia JL, VanBeek MJ, Group for Research of Policy Dynamics in Dermatology. Introducing the Group for Research of Policy Dynamics in Dermatology: “Future considerations for clinical dermatology in the setting of 21st century American policy reform” manuscript series. J Am Acad Dermatol. 2017;76(1):168–169. [DOI] [PubMed] [Google Scholar]
- 4.Armstrong AW, Chambers CJ, Maverakis E, et al. Effectiveness of Online vs In-Person Care for Adults With Psoriasis: A Randomized Clinical Trial. JAMA Netw Open. 2018;1(6):e183062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Academy of Dermatology. Position Statement on Teledermatology. https://www.aad.org/Forms/Policies/Uploads/PS/PS-Teledermatology.pdf Accessed July 8, 2019.
- 6.Peart JM, Kovarik C. Direct-to-patient teledermatology practices. J Am Acad Dermatol. 2015;72(5):907–909. doi: 10.1016/j.jaad.2015.01.019 [DOI] [PubMed] [Google Scholar]
- 7.Armstrong AW, Johnson MA, Lin S, Maverakis E, Fazel N, Liu F-T. Patient-centered, direct-access online care for management of atopic dermatitis: a randomized clinical trial. JAMA Dermatol. 2015;151(2):154–160. [DOI] [PubMed] [Google Scholar]
- 8.Yang X, Barbieri JS, Kovarik CL. Cost analysis of a store-and-forward teledermatology consult system in Philadelphia. J Am Acad Dermatol. October 2018. doi: 10.1016/j.jaad.2018.09.036 [DOI] [PubMed] [Google Scholar]
- 9.Vidal-Alaball J, Lluís Garcia Domingo J, Garcia Cuyas F, et al. A cost savings analysis of asynchronous teledermatology compared to face-to-face dermatology in Catalonia. BMC Health Serv Res. 2018;18. doi: 10.1186/s12913-018-3464-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Livingstone J, Solomon J. An assessment of the cost-effectiveness, safety of referral and patient satisfaction of a general practice teledermatology service. Lond J Prim Care. 2015;7(2):31–35. doi: 10.1080/17571472.2015.11493433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Snoswell CL, Caffery LJ, Whitty JA, Soyer HP, Gordon LG. Cost-effectiveness of Skin Cancer Referral and Consultation Using Teledermoscopy in Australia. JAMA Dermatol. 2018;154(6):694–700. doi: 10.1001/jamadermatol.2018.0855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eminović N, Dijkgraaf MG, Berghout RM, Prins AH, Bindels PJ, de Keizer NF. A cost minimisation analysis in teledermatology: model-based approach. BMC Health Serv Res. 2010;10:251. doi: 10.1186/1472-6963-10-251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loane M, Oakley A, Rademaker M, et al. A cost-minimization analysis of the societal costs of realtime teledermatology compared with conventional care: Results from a randomized controlled trial in New Zealand. J Telemed Telecare. 2001;7:233–238. doi: 10.1258/1357633011936453 [DOI] [PubMed] [Google Scholar]
- 14.Datta SK, Warshaw EM, Edison KE, et al. Cost and utility analysis of a store-and-forward teledermatology referral system: A randomized clinical trial. JAMA Dermatol. September 2015:1–7. doi: 10.1001/jamadermatol.2015.2362 [DOI] [PubMed] [Google Scholar]
- 15.Pak HS, Datta SK, Triplett CA, Lindquist JH, Grambow SC, Whited JD. Cost minimization analysis of a store-and-forward teledermatology consult system. Telemed J E-Health Off J Am Telemed Assoc. 2009;15(2):160–165. doi: 10.1089/tmj.2008.0083 [DOI] [PubMed] [Google Scholar]
- 16.Wootton R, Bloomer SE, Corbett R, et al. Multicentre randomised control trial comparing real time teledermatology with conventional outpatient dermatological care: societal cost-benefit analysis. BMJ. 2000;320(7244):1252–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mohan GC, Molina GE, Stavert R. Store and forward teledermatology improves dermatology knowledge among referring primary care providers: A survey-based cohort study. J Am Acad Dermatol. 2018;79(5):960–961. doi: 10.1016/j.jaad.2018.05.006 [DOI] [PubMed] [Google Scholar]
- 18.Snoswell C, Finnane A, Janda M, Soyer HP, Whitty JA. Cost-effectiveness of Store-and-Forward Teledermatology: A Systematic Review. JAMA Dermatol. 2016;152(6):702–708. doi: 10.1001/jamadermatol.2016.0525 [DOI] [PubMed] [Google Scholar]
- 19.Barbieri JS, Yang X, Kovarik CL. Evaluating the cost-effectiveness of teldermatology. J Am Acad Dermatol. October 2018. doi: 10.1016/j.jaad.2018.06.074 [DOI] [PubMed] [Google Scholar]
- 20.Whited JD, Datta S, Hall RP, et al. An economic analysis of a store and forward teledermatology consult system. Telemed J E-Health Off J Am Telemed Assoc. 2003;9(4):351–360. doi: 10.1089/153056203772744671 [DOI] [PubMed] [Google Scholar]
- 21.Naka F, Lu J, Porto A, Villagra J, Wu ZH, Anderson D. Impact of dermatology eConsults on access to care and skin cancer screening in underserved populations: A model for teledermatology services in community health centers. J Am Acad Dermatol. 2018;78(2):293–302. doi: 10.1016/j.jaad.2017.09.017 [DOI] [PubMed] [Google Scholar]
- 22.Viola KV, Tolpinrud WL, Gross CP, Kirsner RS, Imaeda S, Federman DG. Outcomes of referral to dermatology for suspicious lesions: implications for teledermatology. Arch Dermatol. 2011;147(5):556–560. doi: 10.1001/archdermatol.2011.108 [DOI] [PubMed] [Google Scholar]
- 23.Tensen E, van der Heijden JP, Jaspers MWM, Witkamp L. Two Decades of Teledermatology: Current Status and Integration in National Healthcare Systems. Curr Dermatol Rep. 2016;5:96–104. doi: 10.1007/s13671-016-0136-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee KJ, Finnane A, Soyer HP. Recent trends in teledermatology and teledermoscopy. Dermatol Pract Concept. 2018;8(3):214–223. doi: 10.5826/dpc.0803a13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Armstrong AW, Kwong MW, Ledo L, Nesbitt TS, Shewry SL. Practice Models and Challenges in Teledermatology: A Study of Collective Experiences from Teledermatologists. PLoS ONE. 2011;6(12):e28687. doi: 10.1371/journal.pone.0028687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barbieri JS, Kovarik CL. Inpatient and Tertiary Consultations in Teledermatology. Curr Dermatol Rep. 2016;5(2):83–89. [Google Scholar]
- 27.Fogel AL, Kvedar JC. Reported Cases of Medical Malpractice in Direct-to-Consumer Telemedicine. JAMA. 2019;321(13):1309–1310. doi: 10.1001/jama.2019.0395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barbieri JS, Nelson CA, Bream KD, Kovarik CL. Primary care providers’ perceptions of mobile store-and-forward teledermatology. Dermatol Online J. 2015;21(8). [PubMed] [Google Scholar]
- 29.Houghton V. The full picture. Dermatol World. April 2015.
- 30.Hall JL, McGraw D. For Telehealth To Succeed, Privacy And Security Risks Must Be Identified And Addressed. Health Aff (Millwood). 2014;33(2):216–221. doi: 10.1377/hlthaff.2013.0997 [DOI] [PubMed] [Google Scholar]
- 31.Stevenson P, Finnane AR, Soyer HP. Teledermatology and clinical photography: safeguarding patient privacy and mitigating medico-legal risk. Med J Aust. 2016;204(5):198–200e1. [DOI] [PubMed] [Google Scholar]
- 32.R Rosen A, Littman-Quinn R, L Kovarik C, Lipoff J. Landscape of business models in teledermatology. Cutis. 2016;97:302–304. [PubMed] [Google Scholar]
- 33.Mayer JE. Reimbursement for teledermatology in the United States: a review. Health Technol. 2015;5(2):67–71. doi: 10.1007/s12553-015-0103-5 [DOI] [Google Scholar]
- 34.National Consortium of Telehealth Research Centers. National Consortium of Telehealth Research Centers. https://www.telehealthresourcecenter.org/ Accessed June 24, 2019.
- 35.Centers for Medicare & Medicaid Services. Information on Medicare Telehealth. U.S. Department of Health and Human Services; 2018. [Google Scholar]
- 36.RevCycleIntelligence. Medicare Reimbursement Rules Limit Telehealth Adoption. RevCycleIntelligence. https://revcycleintelligence.com/news/medicare-reimbursement-rules-limit-telehealth-adoption Published November 26, 2018 Accessed June 20, 2019.
- 37.Morenz AM, Wescott S, Mostaghimi A, Sequist TD, Tobey M. Evaluation of Barriers to Telehealth Programs and Dermatological Care for American Indian Individuals in Rural Communities. JAMA Dermatol. June 2019. doi: 10.1001/jamadermatol.2019.0872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Current State Laws and Reimbursement Policies | CCHP Website. https://www.cchpca.org/telehealth-policy/current-state-laws-and-reimbursement-policies?jurisdiction=All&category=128&topic=4 Accessed July 9, 2019.
- 39.mHealthIntelligence. CMS Finalizes Telehealth Expansion for Medicare Advantage Plans. mHealthIntelligence. https://mhealthintelligence.com/news/cms-finalizes-telehealth-expansion-for-medicare-advantage-plans. Published April 8, 2019 Accessed June 24, 2019.
- 40.Uscher-Pines L, Malsberger R, Burgette L, Mulcahy A, Mehrotra A. Effect of Teledermatology on Access to Dermatology Care Among Medicaid Enrollees. JAMA Dermatol. 2016;152(8):905–912. [DOI] [PubMed] [Google Scholar]
- 41.Current State Laws and Reimbursement Policies | CCHP Website. https://www.cchpca.org/telehealth-policy/current-state-laws-and-reimbursement-policies?jurisdiction=All&category=128&topic=4# Accessed September 17, 2019.
- 42.New Medicare Payments for Virtual Services Effective January 1, 2019. PYA. https://www.pyapc.com/insights/new-medicare-payments-for-virtual-services-effective-january-1-2019/ Accessed September 17, 2019.
- 43.Technology-Based Encounters in Dermatology. Dermatology World. AAD. https://www.aad.org/dw/monthly/2019/august/technology-based-encounters-in-dermatology Accessed September 12, 2019.
- 44.Overview of the Medicare Physician Fee Schedule Search. https://www.cms.gov/apps/physician-fee-schedule/overview.aspx Accessed September 17, 2019.