Introduction
Dear Editor, Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19, is primarily transmitted between people through respiratory droplets and contact routes.1, 2, 3 Based on the available evidence, the World Health Organization has recommended stringent contact and droplet-preventive measures for caregivers of patients with COVID-19 and also airborne precautions for clinical settings where aerosol-generating procedures are performed.4
Routine dental practice involves the use of air-rotor high-speed handpieces, ultrasonic scalers and three-way air–water syringes. These create a visible spray comprising water, saliva, blood, microorganisms and other debris. This spatter settles out quickly, travelling only a short distance and landing on dental health-care personnel (DHCP), patients and nearby surfaces. The spray may also contain certain aerosols which can travel distances of over one metre.
There are currently no existing data to assess the risk of SARS-CoV-2 transmission during dental practice or to ascertain adequate protection of DHCP using standard precautions when providing dental treatment. Clusters attributed to dental settings or personnel have not been reported till date. Hence, it is prudent to minimise exposure of patients to dental clinic settings in the current scenario.
Telehealth is the term given to health-care services and public health delivered with the aid of information and communication technology to facilitate patient consultation, diagnosis, self-care, treatment planning and scheduling by a health-care provider at a site distant to the patient.
Teledentistry is a subhead of telehealth which provisions for dental care at a distance with the aid of information and communication technology. All current dental practice, legal and professional obligations that apply to in-clinic care also apply to teledentistry.5 Teleconsult and telescreening have also been suggested in the ‘Guidelines for Dental Professionals in Covid-19 Pandemic Situation’ issued by the Ministry of Health & Family Welfare, Government of India.6
Teledentistry in the current scenario of COVID-19 focuses on ‘dental triage’, the relief of pain or infection, provision of dental care by remote consultation, planning and scheduling of definitive dental treatment. Teledentistry may incorporate the following modalities:
-
(a)
Live audio-visual (AV) communication (synchronous): Real-time, two-way interaction between the patient and care provider aided by AV telecommunication technology using apps such as WhatsApp video call, Skype, Google Duo, Zoom, etc. or plain audio by use of fixed line or mobile phone conversation.
-
(b)
Store-and-forward (asynchronous): Transmission of recorded health information (e.g., radiographs, photographs, video, digital impressions and photomicrographs of patients) through a secure electronic communication system to a care provider using apps such as WhatsApp or e-mail to evaluate a patient's condition or render a service/advice outside of a real-time or live interaction.
-
(c)
Remote patient monitoring: Medical data of a patient in one location transmitted to a provider in a different location for use in telehealth.
An emergency in dentistry is a potentially life-threatening condition necessitating immediate treatment. It includes
-
(a)
Oral and maxillofacial trauma.
-
(b)
Cellulitis or other significant infection, especially if compromising the patient's airway.
-
(c)
Prolonged bleeding.
-
(d)
Pain/swelling that cannot be managed by over-the-counter medication.
However, most patients construe deterioration in quality of life owing to poor masticatory function secondary to a fractured restoration, broken denture or uncomfortable orthodontic appliance also as an emergency. Thus, it is essential to minimise the number of patients attending dental establishments to reduce the risk of transmission of COVID-19 both to personnel at dental establishments and also to patients. Hence, it should be limited to only those patients with severe or uncontrolled symptoms that they cannot manage themselves.
Procedure
The designated e-mail/mobile number must be intimated to the dependent population. The working hours may also be specified with a dental officer designated specially for this duty. The use of Resident Welfare Association WhatsApp groups may be used to disseminate necessary information in addition to conventional Armed Forces channels. It must be ensured at all times that no sensitive information is exchanged over unsecure civil channels of communication.
Patients may be advised to initially communicate their problem through SMS, WhatsApp message or email. The clinician may then decide if an AV inspection is required. If an AV inspection is warranted, the patient may be informed of the same along with the approximate time and mode of AV communication. The patient may be asked to be ready with a torch light, a spoon and a family member who can facilitate the clinician's visual assessment by assisting the patient to retract the tongue, cheek, etc. with the back of a spoon and to focus the torch light.
General principles
On confirming the identity of the patient, teledentistry may be initially used for triage of patients. Appropriate and relevant medical history and details of the patient's present complaint to ascertain the nature of emergency may be obtained. Reliability, quality and timeliness of the patient's health information obtained via teledentistry must be ensured for adequacy to justify providing or assisting in dental care. Appropriate records of all teledentistry appointment must be maintained.
The COVID-19 status must be established and recorded using the standard protocol. This will determine how their care is managed at the dental centres, if in-clinic care is planned. Assessment of the patient should consider patient safety, professional judgement, human resource and infrastructure available at the dental centre for appropriate treatment and prioritisation of the most urgent treatment needs.
Primary care dental triage should focus on the provision of the three ‘A's:
-
(a)
Appropriate Advice.
-
(b)
Appropriate Analgesia.
-
(c)
Appropriate Antimicrobials.
Patients are advised to contact again in 48–72 h for a teledentistry consultation if their symptoms have not resolved. Dental conditions that cannot be managed by the patient after a teleconsultation and require urgent dental care should be attended to at the dependent dental centre with requisite safety precautions and personal protective equipment in place. The advisories in vogue as promulgated by the Director General of Medical Services (DGAFMS), Dental Council of India, Ministry of Health and Family Welfare (MoHFW) and the local authorities must be strictly adhered to.
Advantages of teledentistry
Teledentistry during times of COVID-19 serves to assuage the limitations of in-clinic care owing to lockdown imposed by the government and also the concerns of social distancing and yet provide professional dental advice to patients, thereby also aiding in the effort to ‘flatten the curve’ of the COVID-19 pandemic. Teledentistry provides a direct patient–clinician communication, helps schedule consultations for emergency and nonemergency but urgent treatment and assists to diagnose potential emergencies and identify other procedures that can be scheduled at a later date. It also aids in staggered scheduling of treatment at dental centres to prevent overcrowding and follow adequate social distancing protocols. Antimicrobials and pain medication may be prescribed if the patient is experiencing pain and infection. Patient management by collaborating with other specialists may also be facilitated if that clinician is also using telehealth.
Barriers to the use of teledentistry
The perception of many patients and few clinicians is the lack of personal and direct on-site contact of clinician with the patient. Diagnostic aids such as dental radiographs are not possible. Poor availability of bandwidth or uninterrupted internet access in most parts of this country is also a barrier for its use. Some patients may not be sufficiently technologically enabled to communicate with the clinician for teledentistry. There is a lack of contemporary guidelines on dispensing medicines at the service dispensaries on digital prescriptions and also acceptance of cross-referrals for associated medical ailments/morbidities.
Triage of commonly presenting dental problems
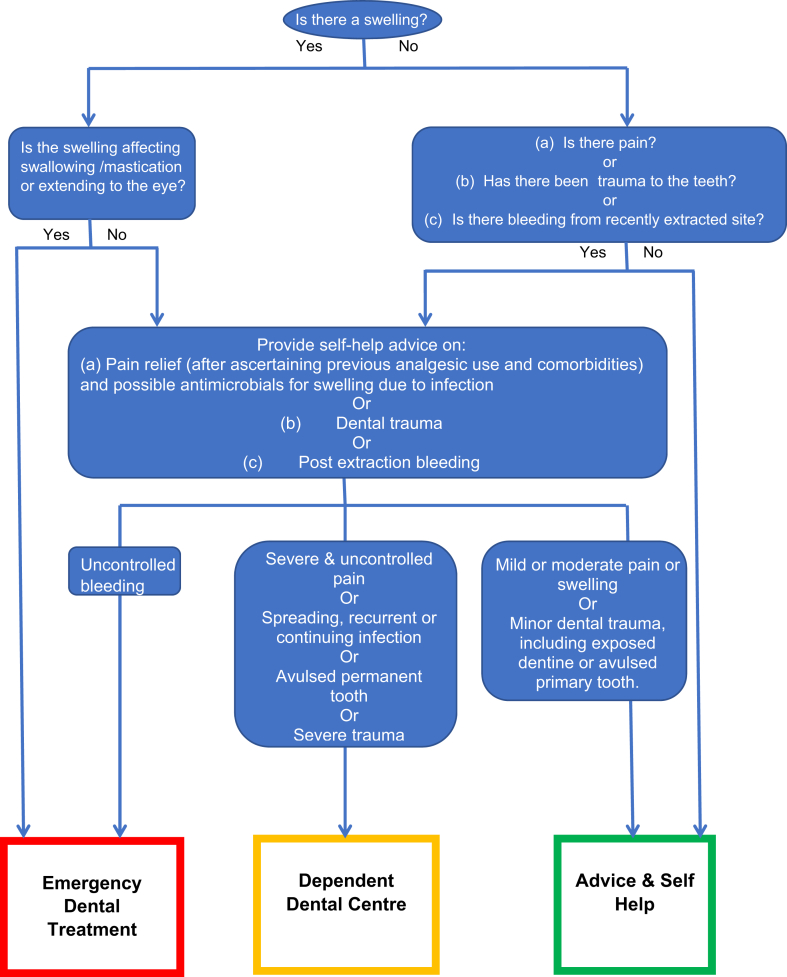
The following flow chart (Fig. 1) illustrates a simple method for dental care for patients by AV triage. Although not comprehensive, it encompasses the most common presenting symptoms in dental practice.
Fig. 1.
Outline of dental care in teledentistry.
Modes of management provided by teledentistry
Advice and/or self-help: Mild and moderate symptoms managed only by providing AV advice and/or self-help, which may include prescription of analgesics and antimicrobials.
Urgent care: Severe or uncontrolled symptoms that cannot be managed using the AV advice to the patient and require the treatment by a dental officer at the dependent dental centre.
Emergency care: Emergency conditions that require immediate clinical attention at the dependent hospital/dental centre.
Conclusion
While use of telehealth technology is yet to evolve as an integral aspect of oral health-care delivery in Armed Forces dental establishments, the current pandemic may be used as an opportunity to develop teledentistry to play a larger role in the future. It is imperative to use telehealth where access to care is challenging. Dental emergencies can happen to anyone, but nobody should feel the need to decide which aspect of their health to favour in situations such as the current COVID-19 outbreak. If the Armed Forces personnel and their families need to remain in self-isolation and follow social distancing and the lockdown norms imposed by the government, the dedicated team of AD Corps must provide the appropriate dental advice and reassurance they need. Teledentistry may continue to be used after lockdown until the threat of COVID 19 persists and subsequently to provide efficient, specialised and rapid care to the furthest posts where easy access to dental officers by troops is not possible.
Disclosure of competing interest
The authors have none to declare.
References
- 1.Chan J., Yuan S., Kok K. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020 doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morawskaa L., Cao J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ Int. 2020;139:105730. doi: 10.1016/j.envint.2020.105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations Available from:
- 4.WHO Infection Prevention and Control Guidance for COVID-19. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/infection-prevention-and-control Available at:
- 5.Jampani N.D., Nutalapati R., Dontula B.S., Boyapati R. Applications of teledentistry: a literature review and update. J Int Soc Prev Community Dent. 2011;1:37–44. doi: 10.4103/2231-0762.97695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guidelines for Dental Professionals in Covid 19 Pandemic Situation. MoHFW; 19 May 2020. https://www.mohfw.gov.in/pdf/DentalAdvisoryF.pdf [Google Scholar]