Abstract
Purpose
Subjective and objective social isolation are important factors contributing to both physical and mental health problems, including premature mortality and depression. This systematic review evaluated the current evidence for the effectiveness of interventions to improve subjective and/or objective social isolation for people with mental health problems. Primary outcomes of interest included loneliness, perceived social support, and objective social isolation.
Methods
Three databases were searched for relevant randomised controlled trials (RCTs). Studies were included if they evaluated interventions for people with mental health problems and had objective and/or subjective social isolation (including loneliness) as their primary outcome, or as one of a number of outcomes with none identified as primary.
Results
In total, 30 RCTs met the review’s inclusion criteria: 15 included subjective social isolation as an outcome and 11 included objective social isolation. The remaining four evaluated both outcomes. There was considerable variability between trials in types of intervention and participants’ characteristics. Significant results were reported in a minority of trials, but methodological limitations, such as small sample size, restricted conclusions from many studies.
Conclusion
The evidence is not yet strong enough to make specific recommendations for practice. Preliminary evidence suggests that promising interventions may include cognitive modification for subjective social isolation, and interventions with mixed strategies and supported socialisation for objective social isolation. We highlight the need for more thorough, theory-driven intervention development and for well-designed and adequately powered RCTs.
Keywords: Loneliness, Perceived social support, Objective social isolation, Mental health, Systematic review, Intervention
Introduction
Subjective social isolation and objective social isolation are conceptually distinct [1] and often only moderately correlated [2]. The terms loneliness and perceived social support both refer to people’s subjective perception of their social world (i.e. subjective social isolation) [1, 3]. Loneliness is defined as the unpleasant experience that occurs when there is a subjective discrepancy between desired and perceived availability and quality of social interactions [4]. Perceived social support is the self-rated adequacy of the social resources available to a person [5]. Well-established and widely used measures of loneliness are available, such as the UCLA Loneliness Scale [6]. Objective social isolation, meanwhile, involves having little social contact with other people [7] and can be objectively defined based on quantitative measures of social network size or the frequency of social contacts with others [8]. A summary table of commonly used measures of subjective and objective social isolation is provided in Appendix 1.
In a UK survey, approximately one in five of the general population reported being lonely in the preceding 2 weeks [9]. For people with mental health problems, the odds of being lonely were eight times greater than for the general population, and the odds were increased 20-fold for those with two or three diagnoses (e.g. depression and schizophrenia), compared to those without any diagnosis [10]. Objective social isolation, including having fewer friends [11] and being less likely to date [12], is also more common among people with mental health problems than in the general population. Loneliness has adverse health effects, such as an impaired immune system [13], elevated blood pressure [14], depression [15], and cognitive decline [16]. Moreover, loneliness is associated with poorer quality of life [17] and personal recovery [18], and with more severe mental health symptoms [19]. Similarly, a number of negative health outcomes have been found to be associated with objective social isolation, for example, increased all-cause mortality rate [20], poor physical health outcomes [21, 22], worse psychotic symptoms [23, 24], depressive symptoms [24], and higher risk of dementia [25]. Conversely, social support that is perceived as sufficient is associated with less severe psychiatric symptoms, higher functioning, better personal recovery, greater self-esteem and empowerment, and improved quality of life [26]. These associations between subjective and objective social isolation and poorer outcomes [27–30] make interventions designed to alleviate social isolation of high interest. Subjective social isolation has recently been increasingly recognised as a treatment priority for people with serious mental illness [31]. By targeting both subjective and objective social isolation as main outcomes in the current review, we aimed to establish the extent of the current evidence base for interventions for each of these potential treatment targets and to understand the similarities or differences between the characteristics of interventions that work for subjective and for objective social isolation.
Some authors have previously systematically reviewed interventions for subjective social isolation [30, 32–35] and objective social isolation [36–38] (Appendix 2). The most recent systematic review focused on subjective social isolation among people with mental health problems was published in 2005 [35]. Three more recent systematic reviews focused on aspects of objective social isolation: one reviewed interventions to increase network size in psychosis [37] and the other two examined interventions targeting social participation in people with mental health problems [36, 38]. Thus, there is no up-to-date systematic review of evidence for a full range of interventions to alleviate subjective and/or objective social isolation among people with a mental health diagnosis.
Masi’s meta-analysis in 2011 [34] has been considered one of the most comprehensive reviews to date examining interventions for loneliness, identifying four main types of intervention. However, Masi’s review included only 20 RCTs and included all populations, not only people with mental health problems. Thus, our paper adds to knowledge from Masi’s review by providing an up-to-date synthesis of interventions for loneliness in people with mental health problems, using a typology of interventions targeting loneliness and related constructs recently developed by Mann and her team [39]. This typology distinguishes among the following: (1) interventions involving changing maladaptive cognitions about others (e.g. cognitive-behavioural therapy or reframing); (2) social skills training and psychoeducation programmes (e.g. family psychoeducation therapy); (3) supported socialisation (e.g. peer support groups, social recreation groups); and (4) wider community approaches (e.g. social prescribing and asset-based community development approaches). These community approaches maximise individuals’ engagement with social resources and/or aim to develop social resources at the level of whole communities.
Methods
We conducted the current systematic review to evaluate the evidence for the effectiveness of interventions designed to alleviate subjective social isolation (including loneliness and perceived social support) and/or objective social isolation among people with mental health problems.
Inclusion criteria
Types of study
Only randomised controlled trials (RCTs) were included, with no restrictions on publication dates, the country of origin or language.
Participants
People primarily diagnosed with mental health conditions were included, including depression, anxiety, post-traumatic disorder, psychosis/schizophrenia or bipolar disorders. Any method of identifying or diagnosing people as mentally ill was acceptable. There was no restriction on the age of the participants. However, studies where the samples were people with a primary diagnosis of intellectual disability, autistic spectrum disorders, dementia, any other organic illnesses, substance misuse or physical health problems were excluded, even if some had comorbid mental health diagnoses.
Interventions
This review included interventions which were designed to alleviate subjective or/and objective social isolation for people with mental health problems. Papers were included if subjective or objective social isolation was a primary outcome and excluded if they were secondary outcomes, with another clearly specified primary outcome. Trials were also included if a clear distinction was not made between primary and secondary outcomes, with subjective and/or objective social isolation as one of a number of main outcomes.
Comparison
We included trials where the control group received treatment-as-usual, however defined, no treatment or a waiting-list control. We also included trials which compared different active treatment groups.
Outcomes
The primary outcomes were subjective social isolation (including loneliness and perceived social support) and objective social isolation. End-of-treatment outcomes, medium-term outcomes (i.e. up to one year beyond the end-of-treatment time point) and longer-term follow-up outcomes (i.e. more than one year beyond the end-of-treatment time point) were reported separately. The following secondary outcomes were also examined: health status, quality of life, and service use.
Search strategy
Three databases were systematically searched for relevant literature: Medline, Web of Science and PsycINFO. Three groups of search terms were combined: (1) subjective and objective social isolation (e.g. loneliness); (2) mental disorders (e.g. psychosis, depression, post-traumatic stress disorder) and (3) trials (e.g. RCT). For detailed search terms, please see Appendix 3. Reference lists from included studies, relevant systematic reviews, and meta-analyses were hand-searched. Grey literature was searched through OpenGrey by using keywords ‘loneliness’, ‘perceived social support’ and ‘social isolation’.
Data extraction
RM and FM reviewed all titles and abstracts, AA screened half of the papers we retrieved, and final decisions regarding whether a paper should be included or not were made by all three independent reviewers. The primary reviewer (RM) reviewed all full-text papers retrieved, and inter-rater reliability was also evaluated as good between reviewers during the screening process. The final list of included papers was confirmed only when RM, FM, and AA agreed on all papers. Any differences were resolved in consultation with a further independent reviewer (SJ). Data were extracted by RM and FM by using a standardised form developed for the review, including items related to publication year and country, study design, experimental settings, participants, the nature of the intervention, follow-up details, primary and secondary outcomes, any exclusions of participants, and the reasons for these, confounders, and risk of bias.
Quality assessment
The Cochrane Risk of Bias tool [40] was used for the quality assessment. Each included paper was assessed by two reviewers (RM and FM/JT) regarding the following domains: sequence generation, allocation concealment, blinding of participants, personnel and outcome assessors, incomplete outcome data, selective outcome reporting and other sources of bias. For each paper, a final decision for each domain was made only if both assessors agreed. If there was disagreement, a third independent assessor (SJ) was consulted.
Synthesis plan
A narrative synthesis was conducted for this systematic review based on the principles from the ESRC’s Guidance on the Conduct of Narrative Synthesis in Systematic Reviews [41]. The included trials were grouped into three categories: (1) trials that included subjective social isolation as an outcome (primary or one of several, with none specified as primary); (2) trials that included objective social isolation as an outcome; and (3) trials that included both outcomes. Due to the expected heterogeneity in samples and intervention types from this broad review, meta-analysis was judged to be inappropriate.
Results
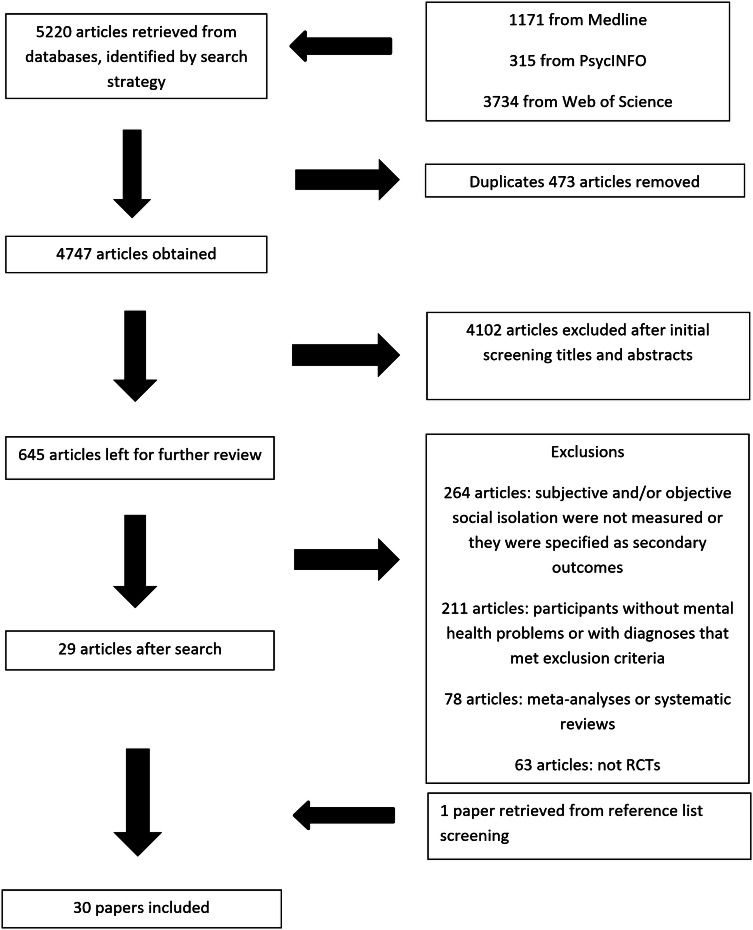
The initial literature search retrieved 5220 papers in total, of which 30 were found to be eligible for inclusion. The PRISMA flow diagram (Fig. 1) shows details of the screening process.
Fig. 1.
PRISMA diagram for literature search
The 30 trials involved 3080 participants in total, with individual trial sample sizes ranging from 21 to 357. Nineteen trials had fewer than 100 participants. The median number was 88, and the interquartile range (IQR) was 104. Authors from nine trials specified sample size calculations. The search was conducted in July 2017 and all trials were published between 1976 and 2016. Thirteen trials were conducted in the US, 11 in Europe, 3 in Israel, 2 in China, and 1 in Canada. Thirteen interventions were conducted individually, nine interventions were delivered in groups, four involved individual and group support, and four were implemented online. Ten trials compared different active treatments, four of which had no control group. The remaining 20 trials compared intervention groups with a control group: 13 involved treatment-as-usual groups, 5 involved waiting-list controls, and 2 involved no-treatment controls.
Interventions to reduce subjective social isolation
Fifteen trials included subjective social isolation as primary outcome, or as one of several outcomes with none specified as primary (Table 1).
Table 1.
Trials that included subjective social isolation as outcome
| Main author, sample and setting | Intervention categorisation | Intervention name and duration | Follow-up | Social isolation and other outcome measures | Subjective social isolation outcomes |
|---|---|---|---|---|---|
| Group-based intervention | |||||
|
Hasson-Ohayon [42]—210 adults with severe mental illness Psychiatric community rehabilitation centre in Israel (secondary care setting) |
Psychoeducation, social skills training |
Illness Management and Recovery Programme vs. treatment-as-usual control group Duration: 8 months |
End-of-treatment follow-up (8 months) |
Subjective social isolation outcome: the Multidimensional Scale of Perceived Social Support (MSPSS) [57] Other outcome: personal recovery |
No significant changes in perceived social support for either group. p > 0.05a |
|
Silverman [43]—96 adults with varied Axis I diagnoses Acute care psychiatric unit in a University hospital, the Midwestern region in the US (secondary care setting) |
Psychoeducation |
Live educational music therapy (condition A), recorded educational music therapy (condition B), education without music (condition C), recreational music therapy without education (condition D) Duration: 24 weeks |
End-of-treatment follow-up (24 weeks) | Subjective social isolation outcome: the MSPSS [57] |
No significant between-group difference in total perceived social support for condition A vs. B, condition A and B vs. condition C, as well as for condition A and B vs. D (all p > 0.05) (F (3.87) = 1.50, p = 0.22) Partial effect size = 0.028 for support from significant other, 0.015 for support from family, 0.094 for support from friends, and 0.049 for total support Only a significant between-group difference between condition A vs. D on a friend subscale, 95% CI (0.47, 10.40), adjusted p = 0.02, mean difference = 5.34 |
|
Boevink [44] - 163 adults with mental illness Mental health care organisations (community treatment team and sheltered housing organisations) in the Netherlands (secondary care setting) |
Supported socialisation |
Toward Recovery, Empowerment and Experiential Expertise (TREE) + care-as-usual vs. care-as-usual control group Duration: 104 weeks for early starters and 52 weeks for late starters |
1 medium-term follow-up: 12 months (post-baseline) 1 long-term follow-up: 24 months (post-baseline) |
Subjective social isolation outcome: the De Jong-Gierveld Loneliness Scale [58] Other outcomes: quality of Life; psychiatric symptoms |
No between-group difference in loneliness, 95% CI (− 0.31, 0.30) (effect size linear tread B = − 0.053, p = 0.98), standardised effect size was − 0.001 for each year of exposure to TREE programme |
|
Eggert [45]—105 high school students with poor grades (moderate or severe depression) 5 urban high schools in the US (general population setting) |
Supported socialisation, social skills training and wider community approaches |
Assessment protocol plus 1-semester Personal Growth Class (PGCI) vs. Assessment protocol plus a 2-semester Personal Growth Class (PGCII) vs. an assessment protocol-only Duration: 5 months or 90 class days in length for PGCI, and 10 months or 190 class days in length for PGCII |
2 medium-term follow-ups: 5 and 10 months (post-baseline) |
Subjective social isolation outcomes: perceived social support was measured by calculating average ratings across 6 network support sources. Instrumental and expressive support provided by each network support source (e.g. family, friends) was also rated on a scale Other outcome: depressive symptoms |
All 3 groups showed increased network social support F linear (1,100) = 32.08, p < 0.001 No significant between-group difference between all groups F linear (1,100) = 1.98, p = 0.143 |
| Individual-based intervention | |||||
|
Zang [46]—30 adults aged 28–80 with post-traumatic stress disorder (PTSD) Beichuan County in China (general population setting) |
Changing cognitions |
Narrative Exposure Therapy (NET) vs. Narrative Exposure Therapy Revised (NET-R) vs. waiting-list control group Duration: 2 weeks for NET and 1 week for NET-R group |
End-of-treatment follow-up (2 weeks for NET, 1 week for NET-R) 2 medium-term follow-ups: 1 week (for NET) or 2 weeks (for NET-R), and 3 months |
Subjective social isolation outcome: the MSPSS [57] Other outcomes: anxiety and depressive symptoms; PTSD symptoms |
Both NET and NET-R showed effects on perceived social support after treatment, but no significant between-group difference between the two groups (F (2,26) = 0.14, p > 0.05) No significant between-group difference between either treatment group (NET and NET-R) and the waiting-list control in perceived social support (both p > 0.05) |
|
Zang [47]—22 adults aged 37–75 with PTSD Beichuan Country in China (general population setting) |
Changing cognitions |
NET intervention vs. waiting-list control group Duration: 2 weeks |
End-of-treatment follow-up (2 weeks) 2 medium-term follow-ups: 2 weeks, and 2 months |
Subjective social isolation outcome: the MSPSS [57] Other outcomes: subjective level of distress; depressive symptoms |
No significant between-group difference in perceived social support (F (1,19) = 4.25, p = 0.05, d = 0.33) |
|
Gawrysiak [48]—30 adults aged ≥ 18 with depression A public Southeastern University in the US (general population setting) |
Psychoeducation, social skills training and supported socialisation |
Behavioural Activation Treatment for Depression (BATD) vs. no-treatment control group Duration: single session lasted 90 min |
1 medium-term follow-up: 2 weeks |
Subjective social isolation outcome: the MSPSS [57] Other outcomes: depressive symptoms; anxiety symptoms |
No significant between-group difference in perceived social support (F (1,28) = 3.11, p = 0.08, d = 0.70) |
|
Conoley [49]—57 female psychology undergraduate students with moderate depression University Psychology department in the US (general population setting) |
Changing cognitions |
Reframing vs. self-control vs. waiting-list control group Duration: 2 weeks |
End-of-treatment follow-up (2 weeks) 1 medium-term follow-up: 2 weeks |
Subjective social isolation outcome: the Revised University of California Los Angeles (UCLA) Loneliness Scale [59]; The Causal Dimension Scale [60] Other outcome: depressive symptoms |
No significant treatment effect was found (F (2,108) = 0.60, p > 0.05b) |
|
Bjorkman [50]—77 adults aged 19–51 with severe mental illness Case management service in Sweden (secondary care setting) |
Social skills training |
The case management service vs. standard care Duration: unclear |
2 long-term follow-ups: 18 and 36 months |
Subjective social isolation outcome: the abbreviated version of the Interview Schedule for Social Interaction (ISSI) [61] Other outcomes: psychiatric symptoms; quality of life; use of psychiatric services |
No significant between-group difference between two groups in social outcomes (p > 0.05)c |
| Mixed-format (group- and individual-based) | |||||
|
Mendelson [51]—78 depressed women aged 14–41 who were either pregnant or had a child less than 6 months old Home visiting programme in Baltimore City in the US (general population setting) |
Changing cognitions |
Standard home visiting services + The Mother and Babies (MB) course vs. standard home visiting services + information on perinatal depression Duration: 6 weeks |
End-of-treatment follow-up (6 weeks) 2 medium-term follow-ups: 3 and 6 months |
Subjective social isolation outcome: the Interpersonal Support Evaluation List (ISEL) [62] | No significant between-group difference in perceived social support, β = 6.67, SE = 0.03, p < 0.10d |
|
Masia-Warner [52]—35 high school students with social anxiety disorder 2 parochial high schools in New York, US (general population setting) |
Psychoeducation/social skills training, supported socialisation and changing cognitions |
Skills for Social and Academic Success vs. waiting-list control group Duration: 3 months |
End-of-treatment follow-up (3 months) 1 medium-term follow-up: 9 months |
Subjective social isolation outcome: Loneliness Scale [63] Other outcomes: anxiety symptoms; social phobic symptoms; depressive symptoms |
No significant treatment effect, effect size = 0.20e, p > 0.05 |
| Online intervention | |||||
|
Kaplan [53]—300 adults with schizophrenia spectrum or affective disorder Online in the US (general population setting) |
Supported socialisation |
Experimental peer support listserv vs. experimental peer support bulletin board vs. waiting-list control group Duration: 12 months |
2 medium-term follow-ups: 4 and 12 months (post-baseline) |
Subjective social isolation outcome: the Medical Outcomes Study (MOS) Social Support Survey [64] Other outcomes: personal recovery; quality of life; psychiatric symptoms |
No significant between-group difference on MOS (F (1,298) = 0.08, p = 0.93), also not significant when two experimental groups compared to the control group separately (p > 0.05) |
|
Rotondi [54]—30 patients aged ≥ 14 with schizophrenia or schizoaffective disorder In- and out-patient psychiatric care units and psychiatric rehabilitation centres in Pittsburgh, Pennsylvania (secondary care setting) |
Psychoeducation |
Telehealth intervention vs. usual care group Duration: unclear |
2 medium-term follow-ups: 3 and 6 months (post-baseline) | Subjective social isolation outcome: the informational support and emotional support subscales of the instrument that was developed by Krause and Markides [65] | No significant between-group difference on perceived social support (F (1,27) = 3.79, p = 0.062) |
|
O’Mahen [55]—83 women aged > 18 with major depressive disorder (MDD) Online in the UK (general population setting) |
Psychoeducation and supported socialisation |
Netmums Helping with Depression (HWD) vs. treatment-as-usual control group Duration: unclear |
End-of-treatment follow-up (unclear) 1 medium-term follow-up: 6 months |
Subjective social isolation outcome: the Social Provision Scale [66] Other outcomes: depressive symptoms; anxiety symptoms |
No significant between-group difference in perceived support between the intervention and control group (95% CI 1.02, − 0.02), medium effect size = 0.50 (p = 0.27) |
|
Interian [56]—103 veterans with PTSD Online in the US (primary care setting) |
Psychoeducation and changing cognitions |
The Family of Heroes intervention vs. no-treatment control group Duration: unclear |
1 medium-term follow-up: 2 months (post-baseline) | Subjective social isolation outcome: the family subscale of the MSPSS [57] | Intervention group reported a higher chance of having a decreased perceived family support over time than the control group (p = 0.04)f |
aEffect size, confidence interval and actual p value not available in the paper
bConfidence interval and actual p value not available in the paper
cEffect size, confidence interval and actual p value not available in the paper
dEffect size and confidence interval not available in the paper
eConfidence interval and actual p value not available in the paper
fEffect size not available in the paper
Two trials included only end-of-treatment outcomes [42, 43]. The follow-up period of the other 13 trials ranged from 1 week to 36 months beyond the end of treatment. The Multidimensional Scale of Perceived Social Support (MSPSS) and UCLA Loneliness Scale were frequently administered. The measures used in 14 trials have been shown to have good validity and reliability, but one trial [44] did not use a well-established scale. Nine trials involved people with common mental illnesses (e.g. depression), three involved people with severe mental illnesses (e.g. schizophrenia), and three included people with a variety of mental health diagnoses. The majority of the trials had small sample sizes (< 100); only four trials had more than 200 participants. Five trials included a sample size calculation.
Three trials involved online interventions, one trial combined online intervention and telephone support, four trials implemented face-to-face group intervention, five used face-to-face individual therapy, and the remaining two combined both group and individual formats. Interventions in two trials involved supported socialisation, four trials evaluated psychoeducation/social skills training, four had cognition modification elements, and five trials mixed different intervention types. The duration of the interventions ranged from 1 week to 104 weeks, while such information was missing in four trials and one trial involved only a single intervention session (Appendices 4 and 5).
Regarding quality assessment, method of randomisation was mentioned in half of the trials. Information on allocation concealment, missing data, and blinding were not sufficiently described in most trials. For detailed quality assessments, please see Appendix 6.
Of the ten trials that compared an active intervention with a control group [42, 44, 47, 48, 50–52, 54–56], none of the authors reported a significant between-group difference. In the five trials comparing at least two different active interventions [43, 45, 46, 49, 53], only Silverman and colleagues [43] found significant between-group differences, reporting a greater improvement in perceived social support from friends (measured by MSPSS friend subscale) in an intervention group involving both music therapy and psychoeducation than in other treatment groups (e.g. music alone). However, differences were not found in other outcomes and this trial did not involve a waiting-list or treatment-as-usual control. As most trials had small samples and lacked sample size calculations, clear conclusions cannot be drawn from negative results.
Eleven out of 15 trials included measures of other relevant outcomes [42, 44–50, 52, 53, 55]. Of these 11 trials, positive outcomes were reported by authors of seven trials. Improved depressive symptoms were reported in trials of interventions with mixed strategies with the following participant groups: adults in the community [48], urban high schoolers [45], and women with major depressive disorders [55]. Another mixed intervention had an effect on social avoidance and social phobia among high school students [52]. A diagnostically mixed participant group exhibited improved progress towards personal recovery and personal goals with psychoeducation/social skills training [42], and a mixed sample who received supported socialisation [44] also reported an improvement in quality of life. However, results on some outcomes in some of the trials did not show significant differences: an intervention with positive results for depression did not improve anxiety [48]; a case management service was not associated with any change in quality of life [50]; an online intervention for people with schizophrenia did not lead to any differences in quality of life or symptoms [53].
Interventions to reduce objective social isolation
Eleven trials included objective social isolation as primary outcome, or as one of several outcomes with none identified as primary (Table 2).
Table 2.
Trials that included objective social isolation as outcome
| Main author, sample and setting | Intervention categorisation | Intervention name and duration | Follow-up | Objective social isolation and other outcome measures | Objective social isolation outcome |
|---|---|---|---|---|---|
| Group-based intervention | |||||
|
Atkinson [67]—146 registered patients with schizophrenia Community clinic in south Glasgow, UK (secondary care setting) |
Psychoeducation |
The education group vs. waiting-list control group Duration: 20 weeks |
End-of-treatment follow-up (20 weeks) 1 medium-term follow-up: 3 months |
Objective social isolation outcome: a modified Social Network Schedule (SNS) [78] Other outcomes: quality of life; psychiatric symptoms; overall functioning |
Significant between-group difference in the total number of contacts after the intervention (t = 4.4, p < 0.001) and at follow-up (t = 3.6, p < 0.001). Significant between-group difference in the number of confidants after the intervention (t = 3, p = 0.004) and at follow-up (t = 2.8, p = 0.006) Significant between-group difference over time from post-group (t = 2.8, p = 0.007) to follow-up (t = 2.5, p = 0.02) |
|
Hasson-Ohayon [68]—55 adults aged 21–62 with various mental illness 3 psychiatric rehabilitation agencies and the University Community Clinic in Bar-Ilan University, Israel (secondary care setting) |
Wider community approaches, psychoeducation/social skills training and changing cognitions |
Social Cognition and Interaction Training (SCIT) + social mentoring vs. social mentoring only Duration: unclear |
1 medium-term follow-up: 6 months | Objective social isolation outcome: the socio-engagement and interpersonal-communication subscales of the Social Functioning Scale (SFS) [79] | Experimental group showed significantly more improvement in social engagement than the controls (F (1,53) = 28.9, p < 0.001, effect size = 0.35), but no significant between-group difference for the interpersonal communication subscale (F (1,53) = 0.55, p = 0.464, effect size = 0.01) |
|
Bøen [69]—138 seniors with mild depression 2 Municipal districts in eastern and western Oslo, Norway (general population setting) |
Supported socialisation and wider community approaches |
A preventive senior centre group programme vs. waiting-list control Duration: 1 year |
End-of-treatment follow-up (1 year) |
Objective social isolation outcome: the Oslo-3 Social Support Scale [80]a Other outcomes: depressive symptoms; life satisfaction |
Both groups had an increased level of social support, but greater improvement in the intervention group than the control group, d = 0.12, 95% CI (− 0.47, 0.81). |
| Individual-based intervention | |||||
|
Solomon [70]—96 adults with schizophrenia or major affective disorders A community mental health centre in the US (secondary care setting) |
Supported socialisation and wider community approaches |
Consumer management team vs. non-consumer management team Duration: unclear |
2 medium-term follow-ups: 1 month and 1 year (post-baseline) |
Objective social isolation outcomes: family and social contacts; Pattison’s Social Network Scale [81] Other outcomes: use of services; quality of life; psychiatric symptoms |
No significant between-group difference in social networks (p > 0.05)b On average, participants identified 2.72 persons in their social network, 1.55 positive network members and 1.60 family members |
|
Aberg-Wistedt [71]—40 adults with schizophrenia or long-term psychotic disorder The Kungsholmen sector in Stockholm, Sweden (secondary care setting) |
Psychoeducation/social skills training |
The intensive case management programme vs. standard services Duration: 2 years |
One long-term follow-up: 2 years (post-baseline) |
Objective social isolation outcome: the number of people in participants’ social life was measured by a standardised procedure developed from work with child psychiatric patients [82] Other outcomes: quality of life; service use |
Social network of the experimental group increased, while it decreased for the control group, but no significant between-group difference (p > 0.004)c |
|
Stravynski [72]—22 adults aged 22–57 with diffuse social phobia and avoidant personality disorder The Maudsley hospital in London, UK (secondary care setting) |
Social skills training and changing cognitions |
Social skills training vs. Social skill training + cognitive modification Duration: 14 weeks |
End-of-treatment follow-up (14 weeks) 1 medium-term follow-up: 6 months |
Objective social isolation outcome: objective social isolation subscale of the Structured and Scaled Interview to Assess Maladjustment (SSIAM) [83] Other outcome: depressive symptoms |
No significant between-group difference in social isolation, all groups reported less experience of social isolation over time p > 0.05d |
|
Terzian [73]—357 adults aged < 45 diagnosed as on the schizophrenia spectrum by the ICD-10th 47 community mental health services (SPT) in Italy (secondary care setting) |
Supported socialisation and wider community approaches |
Social network intervention + usual treatments vs. usual treatments Duration: 3–6 months |
1 medium-term follow-up: 1 year (post-baseline) 1 long-term follow-up: 2 years (post-baseline) |
Objective social isolation outcome: social networks measured by different parameters of relationships were assessed, all were summarised into a score Other outcomes: psychiatric symptoms; hospitalisation over the follow-up year |
In this paper, a social network improvement was defined as an increase in the number, frequency, importance or closeness of relationships, and an overall social network improvement was definied as an improvement in intimate or working relationships. Significant between-group differences in the improvement of social network and overall social network improvement were found An improvement in social network was found at year 1 in 25% of patients in control group and 39.9% of patients in the experimental group (OR 2.0, 95% CI 1.3–3.1; AOR 2.4, 95% CI 1.4–3.9) At year 1, an overall social network improvement was reported for 30.8% of the routine group and 44.5% of the experimental group (OR 1.8, 95% CI 1.2–2.8; AOR 2.1, 95% 1.3–3.4) These differences remained significant at year 2 for social network improvement (31.5% in the control group and 45.5% in the experimental group, OR 1.8, 95% CI 1.1–2.8; AOR 2.1, 95% CI 1.3–3.5) and for overall social network improvement (33.3% for routine group, 47.9% for the experimental group, OR 1.8, 95% CI 1.2–2.9; AOR 2.2, 95% CI 1.3–3.5) |
|
Solomon [74]—96 adults with schizophrenia or major affective disorders A community mental health centre in the US (secondary care setting) |
Supported socialisation and wider community approaches |
Consumer case management team vs. nonconsumer management team Duration: 2 years |
2 medium-term follow-ups: 1 month and 1 year (post-baseline) 1 long-term follow-up: 2 years (post-baseline) |
Objective social isolation outcome: Pattison’s Social Network [81] Other outcomes: quality of life; psychiatric symptoms |
No significant between-group difference in social outcome; also no significant time and condition effect (F (12,78) = 1.19, p > 0.05e) |
|
Marzillier [75]—21 adults aged 17–43 with a diagnosis of personality disorder or neurosis The Maudsley Hospital in London, UK (secondary care setting) |
Social skills training and changing cognitions |
Systematic Desensitisation (SD) vs. Social Skills Training (SST) vs. waiting-list control Duration: 3.5 months |
End-of-treatment follow-up (3.5 months) 1 medium-term follow-up: 6 months |
Objective social isolation outcome: Revised-Social Diary and Standardised interview Schedule [75] Other outcomes: anxiety disorders; mental state; personality assessment |
No between-group difference between SST and SD in social activities and social contacts (p > 0.05) SST had a greater improvement in the range of social activities (F (1,18) = 7.56, p < 0.025) and social contacts (F (1,18) = 9.47, p < 0.0.01) than the waiting-list group SD had a greater increase in social contacts than the waiting-list group (F (1,18) = 12.46, p < 0.001) |
|
Cole [76]—32 adults with major depression, dysthymic disorder or other affective disorder St. Mary’s Hospital in Montreal, Canada (primary care setting) |
Nonspecific type (intervention group received a psychaitric assessment at home, compared to a standard treatment group who received an assessment at clinic) |
Home assessment group vs. clinic assessment group (treatment-as-usual) Duration: unclear |
3 medium-term follow-ups: 4, 8 and 12 weeks (post-baseline) |
Objective social isolation outcome: Social Resources (SR) subscale from The Older Americans Research and Service Centre Instrument (OARS) [84] Other outcomes: mental state; psychiatric symptoms |
No significant between-group differences in social resources (p > 0.05)f |
| Mixed format (group- and individual-based) | |||||
|
Rivera [77]—203 adults with a psychotic or mood disorder on axis I An inpatient unit in a city hospital in New York, US (secondary care setting) |
Supported socialisation |
Peer-assisted care vs. Nonconsumer assisted vs. standard care vs. clinic-based care Duration: unclear |
2 medium-term follow-ups: 6 and 12 months (post-baseline) |
Objective social isolation outcome: a modification of the Pattison Network Inventory [85] Other outcomes: quality of life; psychiatric symptoms |
Only peer-assisted group showed an increase in social contacts from baseline to 12-month follow-up (F (2, 118) = 7.25, p < 0.01, effect size = 0.11) No significant between-group difference in other network measures (p > 0.05) |
aDue to the fact that the Oslo-3 scale focuses primarily on the practical aspects of social support, Bøen’s study was considered as a study only of objective social isolation
bEffect size, confidence intervals, and actual p value not available in the paper
cEffect size, confidence intervals, and actual p value not available in the paper; the significant level used in this study was p < 0.004
dEffect size not available in the paper
eEffect size, confidence interval, and actual p value not available in the paper
fEffect size, confidence interval, and actual p value not available in the paper
Of 11 trials, one trial [67] only included end-of-treatment outcomes. The follow-up period of the other ten trials ranged from 4 weeks to 2 years beyond the end-of-treatment. In eight trials, validated objective social isolation scales were used. In one trial, objective social isolation was measured by summarising the number, frequency, and type of social connections [73], one trial combined both methods [70], and we could not establish the validity of the measure used in another trial because too little detail was provided [71]. Three trials included people with common mental health problems, six trials involved people with severe mental illnesses, and two trials included diagnostically mixed populations. Most trials involved fewer than 100 participants, and only two had more than 200. Three trials included a sample size calculation.
Seven trials were implemented in an individual format, three were group-based interventions, and one involved both group and individual sessions, plus telephone support. Two trials involved a psychoeducation component/social skills training, one included supported socialisation opportunities, the intervention type of another trial was unclear, and the other seven trials involved interventions with multiple components. The duration of the interventions ranged from 12 weeks to 2 years where this was specified, but such information was not given in four trials (Appendices 4 and 5).
A description of the randomisation process was only included in three trials. Allocation concealment detail was described in five trials. Authors of seven trials did not report how they dealt with missing data. For detailed quality assessments, please see Appendix 6.
Of the six trials that compared an active treatment group with a control group [67–69, 71, 73, 76], findings of four trials suggested superior outcomes for their intervention groups over their control groups on objective social isolation measures: a psychoeducation programme for adults with schizophrenia [67], a social network intervention for people diagnosed with schizophrenia spectrum disorders [73], a preventive senior centre group for seniors with mild depression [69], and Social Cognition and Interaction Training (SCIT) for patients with various diagnoses [68]. One trial involving social education for people with schizophrenia and one trial involving home assessment teams for people with mood disorders did not lead to any improvements in objective social isolation [71, 76].
Of the five trials that compared different active interventions [70, 72, 74, 75, 77], positive findings were reported in two trials. One trial included systematic desensitisation and social skills training interventions: both were found to be superior to the control group for increasing social contacts in a sample with personality or mood disorders, although there was no between-group difference between the two active treatment groups [75]. Rivera and colleagues [77] reported an increased contact with staff for participants receiving a consumer-provided programme, compared to non-consumer support. However, Solomon and colleagues [70, 74] also compared consumer versus non-consumer provided mental health care in their two studies and found no significant differences between the groups, or compared to a control group, in social network size or clinical outcomes. Stravynski and colleagues examined whether adding a cognitive modification component to social skills training for people with social phobia and/or avoidant personality disorders improved its effectiveness [72], but found no significant difference between groups. Therefore, the overall evidence regarding the effectiveness of consumer-provided intensive case management for objective social isolation is unclear.
Other relevant outcomes were included in 10 out of 11 trials [67, 69–77]. Of these ten trials, positive findings were reported in four trials: improved mental state was reported by Rivera and his team, who evaluated a supported socialisation intervention for adults with schizophrenia, other psychotic disorders or mood disorders [77]; reduced depression and social avoidance were reported by Stravynski and colleagues, who evaluated a mixture of strategies for people with social phobia and/or avoidant personality disorder [72]. Atkinson and colleagues also reported a greater quality of life when psychoeducation/social skills training was offered to people with schizophrenia [67], and fewer emergency visits were also reported for a cohort of people with schizophrenia and psychotic symptoms receiving psychoeducation/social skills training [71]. However, Solomon and her team found no differences in psychiatric symptoms or service use for participants who received consumer-led case management [70, 74], and no clinical differences were reported by Terzian and colleagues in a social network intervention for people with schizophrenia [73].
Interventions targeting both subjective and objective social isolation
Four trials included both subjective and objective social isolation as outcomes (Table 3).
Table 3.
Trials that included both subjective and objective social isolation as outcomes
| Main authors, sample and setting | Intervention categorisation | Intervention name | Follow-up | Subjective/objective social isolation and other outcome measures | Subjective social isolation outcomes | Objective social isolation outcomes |
|---|---|---|---|---|---|---|
| Group-based intervention | ||||||
|
Castelein [86]—106 adults aged ≥ 18 with schizophrenia or related psychotic disorders 4 mental health centres in the Netherlands (secondary care setting) |
Supported socialisation |
Care as usual + Guided Peer Support Group (GPSG) vs. a waiting- list (WL) condition Duration: 8 months |
End-of-treatment follow-up (8 months) |
Subjective social isolation outcome: the Social Support List (SSL) [90] Objective social isolation outcome: Personal Network Questionnaire (PNQ) [86] Other outcomes: quality of life; screening for psychosis |
Experimental group had a significantly greater increase in esteem support (p = 0.02), compared to WLa | Experimental group had a significantly greater improvement in social contacts with peers after the sessions (p = 0.03), compared to WL |
|
Gelkopf [87]—34 adults with chronic schizophrenics by DSM-III-R 7 chronic schizophrenia wards in Israel (secondary care setting) |
Changing cognitions |
Video projection of humorous movies vs. treatment-as-usual control group Duration: 3 months |
1 medium-term follow-up: 2 weeks |
Subjective social isolation outcome: the Social Support Questionnaire 6 (SSQ6) [91] Objective social isolation outcomes: 2 measures of social network sum up the size and dispersion; 4 measures assess the source of the support |
A significantly greater improvement in the experimental group than the control group, in perceived amount of support from staff (F = 7.90, p < 0.01), emotional support (F = 4.80, p < 0.05), and instrumental support, (F = 4.94, p < 0.05) No significant results in satisfaction towards the support (F = 1.90, p > 0.05b) |
A significantly greater improvement in the experimental group than the control group in the number of supporters (F = 4.87, p < 0.05) |
| Individual-based intervention | ||||||
|
Ammerman [88]—93 females aged from 16–37 with MDD A community-based home visiting programme in Southwestern Ohio and Northern Kentucky in the US (general population setting) |
Changiing cognitions |
In-Home Cognitive Behavioural Therapy (IH-CBT) + home visiting vs. home visit alone Duration: about 5 months |
End-of-treatment follow-up (5 months) 1 medium-term follow-up: 3 months |
Subjective social isolation outcome: Interpersonal Support Evaluation List (ISEL) [62] Objective social isolation outcome: Social Network Index (SNI) [92] Other outcome: psychiatric symptoms |
IH-CBT group reported a greater increase in social support (p < 0.001) than SHV. Small effect size for social support (0.38) at post-treatment, and moderate effect size (0.65) at follow-up | No significant between-group difference in network size (F = 1.88, p > 0.05), network diversity (F = 0.63, p > 0.05), and embedded networks (F = 2.23, p > 0.05)c |
| Mixed format (group- and individual-based) | ||||||
|
Schene [89]—222 adults aged > 60 with various mental disorders University Psychiatric Clinic of the Academic Hospital in Utrecht, the Netherlands (secondary care setting) |
Psychoeducation/social skills training, and supported socialisation |
Psychiatric day treatment vs. inpatient treatment (treatment-as-usual) Duration: on average 37.6 weeks for day treatment, and 24.9 weeks for inpatient treatment |
End-of-treatment follow-up (on average 37.6 weeks for day treatment, 24.9 weeks for inpatient treatment) 1 medium-term follow-up: 6 months |
Subjective and objective social isolation outcomes: Social Network and Social Support Questionnaire (SNSS) [93] Other outcomes: mental state; psychiatric symptoms; social dysfunction |
No significant between-group difference in social support (F = 0.20, p > 0.05), and no change over time (F = 1.25, p > 0.05)d | No significant between-group difference in network scope (F = 0.05, p > 0.05) and network contacts (F = 0.02, p > 0.05) |
aEffect size and confidence interval not available in the paper
bEffect size, confidence interval and actual p value not available in the paper
cEffect size, confidence interval and actual p value not available in the paper
dEffect size, confidence interval and the actual p value not available in the paper
One trial [86] only included end-of-treatment outcomes. The follow-up period was between 2 weeks and 6 months in the other three trials [87–89]. Measures with established reliability and validity were used in three trials, but the measure in one trial [86] was developed by the team and not clearly described. One trial included people with common mental health problems, two included people with severe mental illness, and one included people with a variety of different mental health diagnoses. Two trials had fewer than 100 participants and only one had more than 200. A sample size calculation was included in one trial.
One trial involved an individual intervention, two trials involved group interventions, and one trial combined individual, group and phone elements. The length of interventions ranged from 3 to 8 months. One trial was of a supported socialisation intervention, two of cognitive modification, and another used a mixture of strategies (Appendices 4 and 5).
Two trials were judged as at low risk of bias for sequence generation, two trials were at low risk for allocation concealment, and only one trial included a strategy for missing data. All trials were at high risk of bias for their blinding process and other sources of bias, but all were at low risk for selective outcome reporting (Appendix 6).
In all four trials, an intervention group was compared to either a waiting-list or a treatment-as-usual control group. Significant between-group differences in subjective social isolation were demonstrated in three out of four trials: a peer support group for adults with psychosis [86], a group-based intervention involving showing humorous movies for adults with schizophrenia [87], and in-home cognitive behavioural therapy for women with major depressive disorders [88]. Of the three trials in which a significant effect on subjective isolation was reported, significant effects on objective social isolation were also reported in two trials [86, 87]. Schene and colleagues [89] did not find any significant between-group differences for either outcome in a diagnostically mixed sample receiving psychiatric day treatment, compared to standard inpatient care.
In terms of other relevant outcomes, reduction in symptoms were reported by authors in three out of four trials: by Schene and colleagues who examined a mixture of strategies for people with a range of diagnoses [89], by Ammerman and his team who evaluated an intervention with a cognitive modification component for women with depression [88], and by Castelein and colleagues, who evaluated a supported socialisation intervention for people with schizophrenia [86]. Castelein and colleagues also reported additional benefits for quality of life.
Overall results
Table 4 summarises the results for each type of intervention for subjective and objective social isolation, including the ones targeting both subjective and objective social isolation.
Table 4.
Summary of different types of intervention and results: objective and subjective social isolation
| Type of intervention | Comparison | Outcomes for subjective isolation | Outcomes for objective isolation |
|---|---|---|---|
| Changing cognitions | Intervention versus TAU or no treatment | 2/4 studies found significant positive results | 1/2 studies found significant positive results |
| two or more active treatments | 0/2 studies found significant positive results for one form of intervention over others | N/A | |
| Social skills training and/or psychoeducation | Intervention versus TAU or no treatment | 0/3 studies found significant positive results | 1/2 studies found significant positive results |
| Two or more active treatments | 1/1 studies found significant positive results for one form of intervention over others | N/A | |
| Supported socialisation | Intervention versus TAU or no treatment | 1/2 studies found significant positive results | 1/1 studies found significant positive results |
| Two or more active treatments | 0/1 studies found significant positive results for one form of intervention over others | 1/1 studies found significant positive results for one form of intervention over others | |
| Wider community approaches | Intervention versus TAU or no treatment | N/A | N/A |
| Two or more active treatments | N/A | N/A | |
| Mixed approaches (interventions with mixed components) | Intervention versus TAU or no treatment | 0/5 studies found significant positive results | 3/4 studies found significant positive results |
| 2 or more active treatments | 0/1 studies found significant positive results for one form of intervention over others | 0/4 studies found significant positive results for one form of intervention over others |
Of all the trials that included a subjective social isolation measure (i.e. combining 15 trials including only a subjective social isolation measure and the four trials targeting both subjective and objective social isolation—19 trials in total), positive results were reported in two out of the six trials that examined interventions with a cognition modification component, one out of the three trials of supported socialisation, and one out of the four trials of social skills training/psychoeducation programmes. Authors who evaluated mixed intervention strategies found no significant positive results. None of the trials evaluated wider community approaches alone.
Regarding all the trials which included an objective social isolation measure (i.e. 15 trials), findings from one out of the two trials that involved changing cognitions, one out of the two trials that examined social skills training and psychoeducation, three out of the eight trials with a mixed intervention strategy, as well as all trials (i.e. two trials) that provided supported socialisation, suggested improvements in objective social isolation. No included trials for objective social isolation involved wider community approaches alone. Small samples and lack of sample size calculations need to be borne in mind throughout.
In many of the included trials, subjective and/or objective social isolation was one of several outcomes (with no clearly specified primary outcome), and for some trials, strategies to reduce social isolation were part of an often much broader service improvement approach (e.g. [70, 74, 76, 89]). Just six trials [43, 72, 73, 75, 86, 87] had a measure of social isolation as the clearly stated primary outcome. Four out of these six trials included either a waiting-list or a treatment-as-usual control group [73, 75, 86, 87], and findings from all of these indicated a superior effect of their intervention compared to the control condition on the trials’ objective social isolation outcomes. In these trials, one intervention involved mixed strategies for adults with schizophrenia [73]; one involved supported socialisation for adults with schizophrenia/psychosis [86]; one compared two treatment groups (i.e. systematic desensitisation and social skills training) to a waiting-list control in a sample of people with personality disorders or neurosis [75]; and another trial investigated an intervention with a cognitive modification component for adults with schizophrenia [87]. Similar to Marzillier’s trial [75], Stravynski and colleagues [72] also offered cognitive modification and social skills training to a comparable sample. Stravynksi’s trial involved a very small sample and the authors failed to find any additional improvement when a cognitive modification element was added to their social skills training. In one trial of four active conditions without a control group, for people with varied Axis I mental health diagnoses (e.g. depression, bipolar disorders) [43], the authors reported a positive effect of its psychoeducation component over other intervention groups (e.g. music alone), though only on one outcome: perceived social support from friends. In most trials in which subjective or objective social isolation was specifically targeted as the primary outcome, and interventions were tailored accordingly, positive results were reported: this specific focus may be important for intervention effectiveness.
Discussion
With growing interest in tackling subjective and objective social isolation due to the negative health impact of both issues, we conducted the current systematic review to summarise evidence from RCTs for interventions with subjective and/or objective social isolation as main outcome(s) in people with mental health problems. Given the quality and sample size of many included studies, conclusions need to be cautious. The strategies found were extremely diverse. A tendency not to clearly specify primary outcomes in earlier trials meant that some of the trials meeting our criteria were broad socially oriented programmes in which social isolation measures were among a number of outcomes. The great diversity of interventions and low quality of reporting in some trials made meta-analysis inappropriate.
A small number of mainly small trials (in a mixture of populations) provided some evidence that perceived social support may be increased by interventions that involve cognitive modification (e.g. [88]), although there were also some trials, generally with short follow-ups in which an effect was not found (e.g. [46, 47]). Small sample sizes and lack of sample size calculations make it difficult to draw firm conclusions from the negative studies. In terms of psychoeducation/social skills training programmes (e.g. [42, 43]), no clear supporting evidence was found for subjective social isolation, although an evaluation of one educational intervention found positive results on one subscale [43]. Again, the lack of large well-powered trials with clearly focused interventions makes definitive conclusions hard to draw.
There is also evidence supporting some of the interventions targeting objective social isolation (e.g. [67–69]). However, studies included a wide range of types of intervention, none of which can be identified as clearly more effective than others. Group-based interventions and interventions involving supported socialisation appeared to have more evidence supporting their effectiveness in reducing objective social isolation than they do for subjective social isolation. All objective social isolation interventions delivered in a group format demonstrated effectiveness, compared to only two out of eight individual-based interventions, though again, lack of power and of clear theory-driven methods for alleviating isolation diminish our confidence in making firm negative conclusions. For people with mental health problems (especially people with psychosis), initiating and maintaining good social relationships can be disrupted by several difficulties, including self-stigma, psychiatric symptoms, and societal discrimination [94]. Therefore, group-based interventions may offer a pathway to initiating social contacts and practising social skills in a relatively safe environment. It is of note that a good quality multicentre trial of peer support groups from the Netherlands, in which the supported socialisation intervention led to increased social contact, did not improve subjective social isolation [8]. The supported socialisation interventions in our review did not have clear effects on subjective social isolation either. It thus seems possible that supported socialisation is more effective in reducing objective than subjective social isolation. There are two possible explanations: first, a lack of social relationships may not be the only factor contributing to subjective social isolation: social cognitions may also play a significant role [95]; second, organised groups may simply not be an effective way to help lonely people initiate meaningful friendships, start intimate relationships, or maintain or improve current relationships. However, most included studies were small and not informed by power calculations, so few definite conclusions can be drawn.
Some (e.g. [68, 69]), but not all (e.g. [70, 72]), interventions with multiple components appeared to have substantial impacts on improving objective social isolation. Solomon and her colleagues [70, 74] failed to find any significant between-group difference in their two trials, which demonstrated comparable effectiveness of consumer-provided and non-consumer provided support in terms of clinical and psychosocial outcomes. However, it must be noted that multi-component interventions often had multiple outcomes and multiple aims extending beyond alleviating social isolation: they met our inclusion criteria because social isolation was among a number of outcomes, with no specified primary outcome. Psychoeducation programmes/social skills training were evaluated in only two trials [67, 71]: only Atkinson found a significant change on their social isolation outcome, so the effectiveness of this type of intervention remains unclear. It is possible that, as suggested by Mann and colleagues [39], social skills training is more suitable for client groups who are preparing to attend wider community groups, or that it works best when combined with other types of interventions (e.g. [68]).
Cognitive modification has not been shown to be effective for objective social isolation: of the two trials using this technique to target objective social isolation [87, 88], significant changes were only observed in one trial [87] with a short follow-up period and a small sample size. In another trial [72], cognitive modification showed no additional benefits when added to social skills training, but the sample was very small and firm conclusions could not be drawn.
We did not find any relevant trial on interventions focusing on the wider community approaches alone, such as the social prescribing and community asset-development approaches described by Mann and her team [39]. It is possible that interventions where the focus is at community-level are difficult to evaluate via individually randomised trials, but such trials are potentially feasible for individual-level approaches such as social prescribing.
Limitations
To the best of our knowledge, this systematic review is the first to provide an overall synthesis of evidence on the effectiveness of interventions for subjective and/or objective social isolation across a range of mental health diagnoses. But it has important limitations. First, we included trials in which subjective and/or objective social isolation was either a primary outcome or one of a list of outcomes with none specified as primary. This means that we have excluded some trials which might offer relevant evidence based on secondary outcomes, and we have included trials where social isolation is one of a list of outcomes, but may not have been clearly the principal target of the intervention. Few of the included trials involved theory-driven interventions for which social isolation was the clear main target. Second, the conclusions we have drawn are limited by the heterogeneity of the intervention types and patient groups, and the low methodological quality of many included trials. Each type of intervention was only evaluated in a small number of trials and the content of programmes varied greatly. Factors such as lack of information on randomisation processes and allocation concealment resulted in high ratings for risk of bias in many of the studies. Many studies were essentially feasibility or pilot trials, with small sample sizes and no underpinning power calculations: thus no clear conclusions could be drawn from either positive or negative results from these studies, including several trials comparing two or more active interventions. As expected, variations between studies regarding interventions, study participants and outcomes measurement methods precluded meta-analysis. Additionally, four trials did not include a well-established outcome measure (e.g. [45, 73]). Last, although there were no restrictions on the language of the included trials and no filter of language was used during the literature search, no eligible trials in other languages were retrieved. Great efforts were made to retrieve all relevant papers, but some trials in other languages may have been missed.
Research implications
Compared with objective social isolation and social support, the concept of loneliness has only recently been subjected to scientific research. This review identified few trials that included loneliness as their main outcome, and none yielded positive results. Recently published pilot trials have established that loneliness is a feasible target for intervention in severe mental illness, either through face-to-face or digital programmes [31, 96]. However, there is still a pressing need to evaluate interventions for loneliness scientifically in large-scale RCTs, given growing enthusiasm for these approaches. We have thus identified an important gap in the literature.
Some trials focusing on objective social isolation and perceived social support were retrieved, but some advances need to be made to develop a substantial body of evidence in this area. First, most trials were vague in articulating a theoretical basis. The development of a clear theory of change is now regarded as an important step in the development of complex health interventions [97, 98]. Developing such theoretical models could helpfully be informed by a richer understanding of experiences of subjective and objective social isolation among people with mental health problems and their views about what may alleviate these. Thus a co-produced approach to intervention development may result in interventions with a more robust theoretical basis and a closer fit to recipients’ needs. Second, greater advances are likely to be made in this area if future trials can specify interventions in greater detail, and if future systematic reviews use clear systems, such as those applied in this review, to categorise interventions. We found that the descriptions of most interventions were typically vague, and most involved several components and delivery methods. Thus the main components of each intervention were often unclear, and exactly which elements contributed to any positive outcomes was difficult to determine. However, this should not limit the development of future interventions with multiple components (e.g. interventions combining cognitive modification with addressing social/environmental barriers to social participation and developing social relationships). Cacioppo and colleagues [99] proposed that loneliness is a multi-dimensional concept, and there is a clear distinction between intimate, relational, and collective loneliness. Thus, as a complex multi-faceted phenomenon, loneliness may well need to be addressed through multiple means.
Computer/mobile technology has become a popular format for the implementation of interventions in the medical field. Online interventions, including online support groups or chatrooms, may potentially be an effective way to provide social support [100]. However, only four trials targeting online interventions were retrieved in the current review and none has shown positive effects. Authors from existing systematic reviews [101, 102] conclude that there is great future potential for the development and utilisation of mobile apps in the mental health field. Meta-analyses have also demonstrated the use of online interventions as an acceptable and practical method to deliver healthcare for people with depression and anxiety [103, 104]. Another systematic review examined the feasibility of web- and phone-based interventions for people with psychosis: authors supported the feasibility of such interventions, and reported a range of positive outcomes in some of the studies included, including improved social connectedness and socialisation [105]. However, only few trials included in this review were RCTs and social isolation was not generally a primary outcome so that studies were not eligible for inclusion in the current review. One pilot trial has also investigated a novel online intervention called HORYZONS for young people with First Episode Psychosis (FEP), and participants became more socially connected after using HORYZONS [106]. Currently, a full trial utilising a single-blind RCT design to evaluate the effectiveness of this intervention over an 18-month follow-up period is taking place for young people with FEP [107]. In another recent feasibility trial [96], authors developed a digital smartphone application (app) named +Connect, which sought to utilise a positive psychology intervention (PPI) for young adults with early psychosis. The programme was found to be effective in reducing loneliness from baseline to 3-month post-intervention follow-up. Programme users also highlighted the benefits in their social lives of positive reinforcement provided by the app. Thus, although digital interventions have been insufficiently tested in substantial RCTs to date, it is feasible to implement such interventions for people with severe mental health problems in order to reduce loneliness, and there is a need for future research to develop and further examine digital interventions on a larger scale. Additionally, the successful implementation of interventions involving positive psychology in the two pilot trials from Lim and her colleagues [31, 96] supports the idea that subjective social isolation is increasingly recognised as a primary treatment outcome for people with psychosis in the mental health field, and future research should also focus on the development and examination of new types of intervention that target loneliness directly for people with mental health problems.
Other forms of intervention that are so far untested but with potential to have effects on loneliness and social isolation include “friends interventions”, which involve patients’ friends in treatment with the aim of strengthening relationships [108] and other interventions aimed at reinvigorating or restoring existing relationships [109]. By focusing on existing social networks, this type of intervention has potential to improve the quality of social relationships already established prior to mental health diagnosis. Beyond the individual level, there is also potential for the development and robust evaluation of the impact on people with mental health problems of interventions on a larger scale, for example, aimed at developing social connections within groups, communities or neighbourhoods, or at maximising the use of existing community assets [39]. Interventions involving wider communities have been seen as crucial in providing social opportunities for people with mental health problems to engage with their local communities and increase their sense of belonging and self-confidence [39]. Indirect interventions targeting upstream factors that contribute to social isolation [110–113] are potentially effective, such as programmes to improve housing and reduce poverty.
Clinical implications
There is substantial evidence demonstrating the significant impact of objective and subjective social isolation on health. However, lack of empirical evidence on the efficacy of targeted interventions means that we cannot yet make clear recommendations for interventions. As argued in a recent Lancet editorial [114], there is a need for life science funding prioritising under-researched social, behavioural, and environmental determinants of health. Subjective and objective social isolation are among the social determinants of health that have received insufficient attention. Some of the research we report does provide a starting point for further work: in a few studies there is some evidence of effectiveness, while other studies with small samples have at least demonstrated that interventions are feasible and acceptable.
To conclude, based on this systematic review, current evidence does not yet clearly support scaled-up implementation of any types of intervention for subjective or objective social isolation in mental health services. Even though cognitive modification shows some promise for subjective social isolation, and interventions with mixed approaches and supported socialisation have also demonstrated their effectiveness for objective social isolation, quality of these trials limited our confidence in publicising their effectiveness. Therefore, innovation in intervention development and more high-quality research is needed. We also note that there is much innovative and interesting practice in this field that is not currently underpinned by research, especially in the voluntary sector: defining, establishing the theoretical premises for and evaluating existing models may thus be a promising direction.
Acknowledgements
SJ and BLE are partly supported by the NIHR Mental Health Policy Research Unit the UKRI Loneliness and Social Isolation in Mental Health Cross-Disciplinary Network, the UCLH NIHR Biomedical Research Centre and the NIHR Collaboration for Leadership in Applied Health Research and Care (CLAHRC) North Thames. FM is a Wellcome Clinical Research Training Fellow.
Appendix 1: Measures and scales for subjective and objective social isolation
| Measures | Description | For which populations | |
|---|---|---|---|
| Subjective social isolation | The University of California at Los Angeles (UCLA) Loneliness Scale [115] | A unidimensional scale to assess the frequency and intensity of one’s lonely experiences, 20 items |
General population (e.g. elderly, lonely students, immigrants) People with mental health problems (e.g. psychiatric inpatients, people with depression) |
| UCLS-8 [6] | A short-form of UCLA Loneliness Scale, 8 items |
General population (e.g. university students, adolescents, elderly sample) People with mental health problems (e.g. people with depression, mixed sample with various diagnoses) |
|
| The De Jong-Gierveld Loneliness Scale [116] |
A 11-item scale measures the feeling of severe loneliness, contains 5 positive and 6 negative items A short-form contains 6 items of the original De Jong-Gierveld Loneliness Scale (3 items for emotional loneliness and 3 items for social loneliness) |
General population (e.g. national survey samples from several countries, elderly Chinese) People with mental health problems (e.g. mixed samples with various diagnoses) |
|
| Multidimensional Scale of Perceived Social Support (MSPSS) [57] | A 12-item scale to measure perceived overall amount of social support and support from significant other/friends/family |
General population (e.g. Chinese university students, young adults, adults with physical disabilities) People with mental health problems (e.g. people with post-traumatic stress disorder, women with severe depressive symptoms) |
|
| Objective social isolation | Social Network Index (SNI) [92] | A 12-item scale, measures the number of people one has regular contact with |
General population (e.g. women with breast cancer, people with severe traumatic brain injury, African-Americans in urban area) People with mental health problems (e.g. old adults with depressive symptoms, people with post-traumatic stress disorder) |
| The Pattison Psychosocial Kinship Inventory (PPKI) [117] | Measures the number of people and relationships one considers as important |
General population (e.g. dysfunctional families) People with mental health problems (e.g. adults with schizophrenia, people with psychosis) |
|
| Measures focus on both domains | Lubben Social Network Scale (LSNS-6) | A revised version, contains 6 items, evaluates the quantity and quality of one’s relationship with family and friends |
General population (e.g. community-dwelling elderly, Korean American caregivers) People with mental health problems (e.g. mixed samples with different diagnoses, depressed immigrants) |
| Social Network Schedule (SNS) [78] | A 6-item scale, measures both quantitative (i.e. the size of one’s social network, the frequency of social communication and the time one spent on socialisation) and qualitative (i.e. quality and intimacy of one’s social relationships, the intensity of social interactions) aspects of one’s social connections | People with mental health problems (e.g. people with non-organic psychosis, people with intellectual disability) | |
| Medical Outcomes Study (MOS) Social Support Scale [64] | A 19-item survey measures dimensions of social support: emotional/informational, tangible, affectionate and positive social interactions |
General population (people with heart failure in Hong Kong, mothers with children in treatment) People with mental health problems (e.g. adults with schizophrenia spectrum or affective disorder) |
|
| Interview Schedule for Social interaction (ISSI) [61] | 50 items, measures the availability and perceived adequacy of attachment and social integration |
General population (e.g. patients with rheumatoid arthritis, people from Canberra suburbs) People with mental health problems (e.g. outpatients with schizophrenia, inpatient male offenders) |
Appendix 2: Existing systematic reviews and meta-analyses
| Authors (published years) | Published years of included studies | Review method | Included participants | How interventions were categorised | Number of studies | Types of study included |
|---|---|---|---|---|---|---|
| Subjective social isolation interventions | ||||||
| Findlay [30] | 1982–2002 | Systematic review | Older people |
(1) Increase social support (2) Psychoeducation/social skills training |
17 | RCTs, non-randomised comparison studies |
| Cattan et al. [32] | 1970–2002 | Systematic review | Older people |
(1) Social skills training (2) Provide social support (3) Psychoeducation/social skills training |
30 | RCTs, non-randomised comparison studies |
| Dickens et al. [33] | 1976–2009 | Systematic review | Older people |
(1) Increase social opportunities (2) Provide social support (3) Psychoeducation/social skills training (4) Address maladaptive social cognitions |
32 | RCTs, non-randomised comparison studies |
| Masi et al. [34] | 1970–2009 | Meta-analysis | Adults, adolescents and children |
(1) Increase social opportunities (2) Provide social support (3) Address maladaptive social cognitions (4) Provide social skill trainings |
50 | RCTs, non-randomised comparison studies |
| Perese and Wolf [35] | Unclear | Narrative synthesis | People with mental health problems | Social network interventions: include support groups, psychosocial clubs, self-help groups, mutual help groups and volunteer groups | 36 | Unclear |
| Objective social isolation interventions | ||||||
| Newlin et al. [36] | Up to September 2014 | Systematic Review and modified narrative synthesis | People with mental health problems | All types of psychosocial interventions | 16 | RCTs, non-randomised comparison studies and qualitative studies |
| Anderson et al. [37] | 2008–2014 | Systematic review | People with psychosis | All types of social network interventions | 5 | RCTs |
| Webber and Fendt-Newlin [38] | 2002–2016 | Narrative synthesis | People with mental health problems | Social participation interventions: include social skills training, supported community engagement, group-based community activities, employment interventions and peer support interventions | 19 | RCTs, non-randomised comparison studies, and qualitative studies |
Appendix 3: Search terms in Medline and PsycINFO
Same terms were used for the search in Web of Science with minor changes.
| # | Search term |
|---|---|
| 1 | loneliness.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 2 | Loneliness.mp. or Loneliness/ |
| 3 | lonely.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 4 | (social support adj5 (subjective or personal or perceived or quality)).mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 5 | Confiding relationship*.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 6 | Social isolation.mp. or Social Isolation/ |
| 7 | Social network*.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 8 | socially isolated.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 9 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 |
| 10 | Mental Disorders/ |
| 11 |
Alcoholism/or Middle Aged/or Child Behaviour Disorders/or Child/or Adolescent/or Stress Disorders, Post-Traumatic/or Adult/or Depression/or Mental Disorders/or mental health problems.mp. or Substance-Related Disorders/ |
| 12 | Bipolar Disorder/or Psychotic Disorders/or Aged/or Stress, Psychological/or Middle Aged/or Community Mental Health Services/or Adult/or Mental Disorders/or mental illnesses.mp. or Schizophrenia/ |
| 13 | mental.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 14 | Psychiatr*.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 15 | Schizo*.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 16 | Psychosis.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 17 | Depress*.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 18 | Suicid*.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 19 | Mania*.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 20 | Manic.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 21 | Bipolar.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 22 | Anxiety.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 23 | Personality disorder*.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 24 | Eating disorder*.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 25 | Anorexia.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 26 | Bulimia.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 27 | PTSD.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 28 | Post-traumatic stress disorder*.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 29 | 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 |
| 30 | 9 and 29 |
| 31 | Clinical trial.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 32 | Controlled study.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 33 | Randomized controlled trial.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 34 | Randomised controlled trial.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 35 | RCT.mp. [mp = title, abstract, original title, name of substance word, subject heading word, keyword heading word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier] |
| 36 | 31 or 32 or 33 or 34 or 35 |
| 37 | 30 and 36 |
Appendix 4: Characteristics of included trials
| Main author | Setting | Participants | Follow-up | Social isolation outcomes | Other outcomes | Intervention type |
|---|---|---|---|---|---|---|
| Subjective social isolation trials | ||||||
| Kaplan [53] | Online intervention, US | 300 adults with a diagnosis of a schizophrenia spectrum or an affective disorder | 2 medium-term follow-ups: 4 and 12 months (post-baseline) | The Medical Outcomes Study (MOS) Social Support Survey [64] |
(1) Personal recovery (2) Quality of Life (3) Psychiatric symptoms |
Supported socialisation |
| Hasson-Ohayon [42] | Psychiatric community rehabilitation centre, Israel | 210 adults with severe mental illness | End-of-treatment follow-up | Multidimensional Scale of Perceived Social Support [57] | Personal recovery | Psychoeducation/social skills training |
| Rotondi [54] | In- and outpatient psychiatric care units and psychiatric rehabilitation centres, Pittsburgh, Pennsylvania | 30 patients aged ≥ 14 with schizophrenia or schizoaffective disorder | 2 medium-term follow-ups: 3 and 6 months (post-baseline) | The informational support and emotional support subscales of the instrument that was developed by Krause and Markides [65] | N/A | Psychoeducation |
| Silverman [43] | Acute care psychiatric unit, a university hospital, the Midwestern region, US | 96 adults with varied Axis I diagnoses | End-of-treatment follow-up | The Multidimensional Scale of Perceived Social Support (MSPSS) [57] | N/A | Psychoeducation |
| Boevink [44] | Mental health care organisations, the Netherlands | 163 adults with varied mental illness |
1 medium-term follow-up: 12 months (post-baseline) One long-term follow-up: 24 months (post-baseline) |
The De Jong-Gierveld Loneliness Scale [58] |
(1) Quality of Life (2) Psychiatric symptoms |
Supported socialisation |
| Zang [46] | Beichuan County, China | 30 aged 28–80 with PTSD |
End-of-treatment follow-up 2 medium-term follow-ups: 1 week or 2 weeks, and 3 months |
The Multidimensional Scale of Perceived Social Support (MSPSS) [57] |
(1) Anxiety and depressive symptoms (2) PTSD symptoms |
Changing cognitions |
| Zang [47] | Beichuan County, China | 22 aged 37–75 with PTSD |
End-of-treatment follow-up 2 medium-term follow-ups: 2 weeks and 2 months |
The Multidimensional Scale of Perceived Social Support (MSPSS) [57] |
(1) Subjective level of distress (2) Depressive symptoms |
Changing cognitions |
| Gawrysiak [48] | A public Southeastern university, US | 30 aged ≥ 18 with depression | 1 medium-term follow-up: 2 weeks | The Multidimensional Scale of Perceived Social Support (MSPSS) [57] |
(1) Depressive symptoms (2) Anxiety symptoms |
Psychoeducation/social skills training and supported socialisation |
| Bjorkman [50] | Case management service, Sweden | 77 adults aged 19–51 with severe mental illness | 2 long-term follow-ups: 18 and 36 months | The abbreviated version of the Interview Schedule for Social Interaction (ISSI) [61] |
(1) Psychiatric symptoms (2) Quality of life |
Social skills training |
| Mendelson [51] | Baltimore City, US | 78 depressed women aged 14–41 who either were pregnant or had a child less than 6 months old |
End-of-treatment follow-up 2 medium-term follow-ups: 3 and 6 months |
The Interpersonal Support Evaluation List (ISEL) [62] | N/A | Changing cognitions |
| O’Mahen [55] | Online intervention, UK | 83 women aged > 18 with MDD |
End-of-treatment follow-up 1 medium-term follow-up: 6 months |
The Social Provision Scale [66] |
(1) Depressive symptoms (2) Anxiety symptoms |
Psychoeducation and supported socialisation |
| Conoley [49] | Psychology Department, US | 57 female psychology undergraduate students with moderate depression |
End-of-treatment follow-up 1 medium-term follow-up: 2 weeks |
The Revised UCLA Loneliness Scale [59] The Causal Dimension Scale [60] |
Depressive symptoms | Changing cognitions |
| Eggert [45] | 5 urban high schools, US | 105 high school students with poor grades (moderate or severe depression) | 2 medium-term follow-ups: 5 and 10 months (post-baseline) | Perceived social support: measured by calculating average ratings across six network support sources. The instrumental and expressive support provided by each support source was also rated | Depressive symptoms | Supported socialisation, social skills training, and wider community approaches |
| Masia-Warner [52] | Two parochial high schools, New York city, US | 35 high school students with social anxiety disorder |
End-of-treatment follow-up 1 medium-term follow-up: 9 months |
Loneliness Scale [63] |
(1) Anxiety symptoms (2) Social phobic symptoms (3) Depressive symptoms |
Psychoeducation/social skills training, supported socialisation and changing cognitions |
| Interian [56] | Online intervention, US | 103 veterans with PTSD | 1 medium-term follow-up: 2 months (post-baseline) | The family subscale of the Multidimensional Scale for Perceived Social Support [57] | N/A | Psychoeducation and changing cognitions |
| Objective social isolation trials | ||||||
| Solomon [70] | A community mental health centre, US | 96 adults with schizophrenia or major affective disorders | 2 medium-term follow-ups: 1 month and 1 year (post-baseline) |
(1) Family and social contacts (2) Pattison’s Social Network scale [81] |
(1) Use of services (2) Quality of Life (3) Psychiatric symptoms |
Supported socialisation and wider community approaches |
| Aberg-Wistedt [71] | The Kungsholmen sector, Stockholm, Sweden | 40 adults with schizophrenia or long-term psychotic disorder, diagnosed by DSM-III-R schizophrenic disorders | 1 long-term follow-up: 2 years (post-baseline) | The number of people in participants’ social life was measured by a standardised procedure developed from work with child psychiatric patients [82] |
(1) Quality of life (2) Service use |
Psychoeducation/social skills training |
| Stravynski [72] | Maudsley Hospital, London, UK | 22 adults aged 22–57 with diffuse social phobia and/or avoidant personality disorder |
End-of-treatment follow-up 1 medium-term follow-up: 6 months |
Structured and Scaled Interview to Assess Maladjustment (SSIAM) [83] | Depressive symptoms | Social skills training and changing cognitions |
| Atkinson [67] | Community clinic, South Glasgow, UK | 146 registered patients with schizophrenia |
End-of-treatment follow-up 1 medium-term follow-up: 3 months |
A modified Social Network Schedule (SNS) [78] |
(1) Quality of life (2) Psychiatric symptoms (3) Overall functioning |
Psychoeducation |
| Terzian [73] | 47 community mental health services (SPT), Italy | 357 adults aged < 45 diagnosed as schizophrenia spectrum disorder by the ICD-10th |
1 medium-term follow-up: 1 year (post-baseline) 1 long-term follow-up: 2 years (post-baseline) |
Social network: different parameters of relationships were assessed, all were summarized into a score |
(1) Psychiatric symptoms (2) Hospitalisation over the follow-up year |
Supported socialisation and wider community approaches |
| Hasson-Ohayon [68] | 3 psychiatric rehabilitation agencies and the University Community Clinic, Bar-Ilan University, Israel | 55 adults aged 21–62 with various serious mental illness | 1 medium-term follow-up: 6 months | Social Functioning Scale (SFS) [79] | N/A | Wider community approaches, psychoeducation/social skills training and changing cognitions |
| Rivera [77] | A city hospital, New York, US | 203 adults with a psychotic or mood disorder on axis I | 2 medium-term follow-ups: 6 and 12 months (post-baseline) | A modification of the Pattison Network Inventory [85] |
(1) Quality of life (2) Psychiatric symptoms |
Supported socialisation |
| Solomon [74] | A community mental health centre, US | 96 adults with schizophrenia or major affective disorders |
2 medium-term follow-ups: 1 month and 1 year (post-baseline) 1 long-term follow-up: 2 years (post-baseline) |
Pattison’s Social Network [81] |
(1) Quality of Life (2) Psychiatric symptoms |
Supported socialisation and wider community approaches |
| Marzillier [75] | The Maudsley Hospital, UK | 21 adults aged 17–43 with a diagnosis of personality disorder or neurosis |
End of treatment follow-up 1 medium-term follow-up: 6 months |
Revised-Social Diary and Standardised Interview Schedule [75] |
(1) Anxiety disorders (2) Mental state (3) Personality assessment |
Social skills training and changing cognitions |
| Bøen [69] | 2 municipal districts, eastern and western Oslo, Norway | 138 seniors with mild depression | End-of-treatment follow-up | The Oslo-3 Social Support Scale [80] |
(1) Depressive symptoms (2) Life satisfaction |
Supported socialisation and wider community approaches |
| Cole [76] | St. Mary’s hospital, Montreal, Canada | 32 adults with major depression, dysthymic disorder or other affective disorder | 3 medium-term follow-ups: 4, 8 and 12 weeks (post-baseline) | The Older Americans Research and Service Centre Instrument (OARS) [84] |
(1) Mental state (2) Symptoms |
N/A |
| Trials for both subjective and objective social isolation | ||||||
| Schene [89] | University Psychiatric Clinic of the Academic Hospital, Utrecht, the Netherlands | 222 adults aged > 60 with various mental disorders |
End-of-treatment follow-up 1 medium-term follow-up: 6 months |
Subjective social isolation outcome: Social Network and Social Support Questionnaire (SNSS) [93] Objective social isolation outcome: Social Network and Social Support questionnaire (SNSS) [93] |
(1) Mental state (2) Psychiatric symptoms (3) Social dysfunction |
Psychoeducation/social skills training, and supported socialisation |
| Castelein [86] | 4 mental health centres, the Netherlands | 106 adults aged ≥ 18 with schizophrenia or related psychotic disorders | End-of-treatment follow-up |
Subjective social isolation outcome: The Social Support List (SSL) Objective social isolation outcome: Personal Network Questionnaire (PNQ) [86] |
(1) Quality of Life (2) Screening for psychosis |
Supported socialisation |
| Gelkopf [87] | 7 chronic schizophrenic wards, Israel | 34 adults with a diagnosis of chronic schizophrenia, based on DSM-III-R | 1 medium-term follow-up: 2 weeks |
Subjective social isolation outcome: The Social Support Questionnaire 6 (SSQ6) [91] Objective social isolation outcomes: (1) 2 measures of social network sum up the size and dispersion (2) 4 measures assess the source of the support |
N/A | Changing cognitions |
| Ammerman [88] | Southwestern Ohio and Northern Kentucky, US | 93 females aged from 16 to 37 with MDD |
End-of-treatment follow-up 1 medium-term follow-up: 3 months |
Subjective social isolation outcome: Interpersonal Support Evaluation List (ISEL) [62] Objective social isolation outcome: Social Network Index (SNI) [92] |
Psychiatric symptoms | Changing cognitions |
Appendix 5: Characteristics of interventions
| Main author | Intervention and control group | Mode of delivery | Number of sessions + duration of each session + duration of intervention | Intervention descriptions | Characteristics of intervention providers |
|---|---|---|---|---|---|
| Subjective social isolation | |||||
| Kaplan [53] | Experimental peer support listserv vs. experimental peer support bulletin board vs. waiting-list control group | Online | Unclear, overall duration of the study was 12 months |
Experimental peer support listserv: participants communicated anonymously with each other via a group distribution email list Experimental peer support bulletin board: participants were instructed on how to create account and log in to board |
The online communication of both listserv and bulletin board group were solely peer directed, but technical support was provided via phone or email |
| Hasson-Ohayon [42] | Illness Management and Recovery Programme vs. treatment-as-usual | Face-to-face sessions (group) |
Weekly sessions, an hour each session Duration of the intervention was 8 months |
Intervention group: Illness Management and Recovery Programme is a standarised curriculum-based programme, which provides essential information and skills to people with severe mental illness. The information and skills provided are designed to help patients manage their illness and work towards their personal recovery goals. In this study, educational handouts in Hebrew were provided to participants, focused primarily on self-management, personal goals, social support, medication use, relapse prevention, and coping with psychiatric symptoms | Interventions were led by two clinicians, one of whom had weekly training sessions. For the first 8 months of intervention, clinicians attended monthly supervision sessions |
| Rotondi [54] | Telehealth intervention vs. usual care group | Online | Unclear | Intervention group: including online therapy groups, ask questions and receive answers, a library of previous questions, activities in the community, news items, and educational reading materials | The 3 therapy groups were facilitated by master of social work and PhD clinicians, they were all trained in the monitoring and management of web-based interventions |
| Silverman [43] | Live educational music therapy (Condition A) vs. recorded educational music therapy (Condition B) vs. education without music (Condition C) vs. recreational music therapy without education (Condition D) | Face-to-face sessions (group) |
24 weekly sessions, 45 min per session Duration of intervention: 24 weeks |
Condition A: live music, a scripted educational lyric analysis session using song lyrics that focused on social support Condition B: recorded music, a scripted educational lyric analysis session about lyrics that focused on social support Condition C: Without music, a scripted educational session without music concerning support and coping Condition D: investigator led the group in playing rock and roll bingo, no scripted educational session |
A certified music therapist with more than 12 years of clinical psychiatric experience conducted therapy sessions |
| Boevink [44] | TREE + CAU vs. CAU (waiting-list control) | Face-to-face sessions (group) |
The early starters: each session lasted 2 h, met every two weeks Duration of the intervention: 104 weeks The Late starters: each session lasted 2 h, met every two weeks; Duration of the intervention: 52 weeks |
TREE model: (1) Training course ‘start with recovery’ (2) Developing strength (3) A one-day recovery training course |
The recovery self-help working groups were facilitated by two senior peer workers, and two mental health care managers facilitated the training course |
| Zang [46] | NET vs. NET-R vs. waiting-list control | Face-to-face sessions (individual) |
NET group: ≥ 4 sessions, 60–90 min per session, twice weekly Duration of intervention: 2 weeks NET-R group: ≥ 3 sessions, 60–120 min per session, and each session was 1–2 days apart; Duration of intervention: 1 week |
For both groups, the narrative was recorded and corrected in subsequent reading sessions NET group: created a detailed biography that focused on traumatic experiences NET-R group: a modified version of NET; the participants first constructed an earthquake narrative and then an autobiography |
All treatments were carried out by the first author and one female psychological counsellor; they both speak Chinese and have the Chinese national psychological counsellor certificate (master) and also were trained in the use of NET and NET-R Weekly case and personal supervisions were conducted; the counsellors were also supervised before they have contact with participants |
| Zang [47] | NET vs. waiting-list control group | Face-to-face sessions (individual) |
NET group: 4 sessions, 60–90 min per session Duration of intervention: 2 weeks |
NET group: created a chronological report of biography with a focus on traumatic experiences. A written report of their biography was provided in the last session |
The team was led by the first author, consisted of 3 female therapists, and they all speak Chinese, and all have the Chinese national psychological counsellor certificate (Master) Therapists were trained for NET and they were tutored under supervision before they work with participants. Weekly case and personal supervisions were also carried out |
| Gawrysiak [48] | BATD vs. no treatment control | Face-to-face session (individual) | Single session lasted 90 min | BA intervention: education, assessments of values and goals, construct an activity hierarchy, selection of value-based behaviours, establish structured behavioural goals, and behavioural checkout form | One male doctoral students in clinical psychology was trained in BATD and conducted the individualised interview |
| Bjorkman [50] | The case management service vs. standard care | Face-to-face sessions (individual) |
1.45 per week during the first 18 months, and the case manager spent on average 1.9 h in client contacts every week Duration of intervention: unclear |
The case management service: moderately focused on skills training, strong emphasis on consumer input | All staff had experiences in working in social services, psychiatric services or vocational rehabilitation. The team consisted of two registered nurses and two social workers. Supervision was done by a psychiatrist and a psychologist |
| Mendelson [51] | Standard home visiting services + MB course vs. standard home visiting services + information on perinatal depression | Face-to-face sessions (group and individual) |
6 weekly sessions, 2 h each session Duration of intervention: 6 weeks |
Intervention group: Sessions cover core cognitive behavioural concepts, including pleasant activities, thoughts, and contact with others | A licensed clinical social worker or clinical psychologist |
| O’Mahen [55] | NetmumsHWD vs. treatment-as-usual | Online and telephone support |
12-session treatment online course, weekly telephone support sessions of 20–30 min Duration of each session and intervention: unclear |
NetmumsHWD: including a core behavioural activation (BA) model, a relapse prevention session, plus two optional modules. Also a chat room that was moderated by peer supporters, and weekly supported phone call from mental health workers |
Mental health supporters with undergraduate degrees and 1 year of clinical qualification in psychological therapies Peer supporters had previous training in low-intensity BA, received 5 days of training in high-intensity perinatal-specific BA approach |
| Conoley [49] | Reframing vs. self-control vs. waiting list | Face-to-face sessions (individual) |
2 sessions with 1 week apart, each session 30 min Duration of intervention: 2 weeks |
Intervention groups: aimed to increase understanding in loneliness. First half of the session consisted of loneliness and reflective responses, the second half included either 3–5 positive reframing directives for reframing subjects, and self-control directives for self-control subjects | Two male doctoral students with 3-year counselling experience, received training in both interventions |
| Eggert [45] | PGCI vs. PGCII vs. an assessment protocol-only | Face-to-face sessions (group) |
PGCI: met daily, 55 min per meeting Duration of intervention: 5 months or 90 class days in length PGCII: met daily, 55 min per meeting Duration of intervention: 10 months or 180 class days in length |
Both PGCI and PGCII: small group work focused on social support; weekly monitoring of activities; and life skills training PGCI: emphasised bonding to PGC group, included training to give and receive social support; focused on motivating to change and acquire essential skills, and rehearsing real-life issues in the group setting with a main focus on problems with friends, teachers and parents PGCII: emphasised broader school bonding, included training to transfer skills to real life situations, providing and seeking social support, and developing health-promoting social activities to reduce the negative impacts of suicidal thoughts and behaviours, anger and/or depression, and drug involvement |
The interventions were delivered by trained school staff who functioned as group leaders |
| Masia-Warner [52] | Skills for Social and Academic Success vs. waiting-list group | Face-to-face sessions (group and individual) |
12 weekly group school sessions (40 min); 2 brief individual meetings (15 min); 2 monthly group booster sessions; and 4 weekend social events (90 min) Duration of intervention: 3 months |
12 group sessions: 1 psychoeducational session, 1 realistic thinking session, 4 social skills training sessions, 5 exposure sessions, and 1 relapse prevention session Individual meetings: met with group leaders at least twice, aim to identify individual treatment goals and problem solving Social events: met and practiced programme skills with peers in their community |
A behaviourally trained clinical psychologist and a clinical psychology graduate student co-led all groups Peer assistants: nominated by teachers and administrators, help with exposures and skill practice |
| Interian [56] | The Family of Heroes intervention vs. control group | Online |
1 h online intervention Duration of intervention: unclear |
The Family of Heroes Intervention: provided psychoeducation and stimulated conversations regarding post-deployment stress and mental health treatment; and three conversation scenarios | N/A |
| Objective social isolation trials | |||||
| Solomon [70] | Consumer management team vs. non-consumer management team | Face-to-face sessions (individual) | Unclear |
Both consumer and non-consumer management team followed an assertive community treatment model (1) Provided activities: housing, rehabilitation and social activities (2) Case managers provided assistance and supported clients, supervised by consumer supervisor |
Requirements for consumer management team: have major mental health problems, ≥ 1 previous psychiatric hospitalisation, a minimum of 14 days of psychiatric hospitalisation, or at least 5 psychiatric emergency service contacts within a year Requirements for non-consumer case management team: consisted of mental health professionals and recent college graduates |
| Aberg-Wistedt [71] | The intensive case management programme vs. standard services | Face-to-face sessions (individual) |
1 h individual meeting every other week; psychiatric nurse/nurse assistant met with patients at least 4 h per week. Crisis intervention services were available 24 h every day and 7 days a week. Duration of intervention: 2 years |
Intervention group: (1) The team provided assertive outreach; patients received skill training and instruction in critical life task (2) Specific services also provided based on individual needs and assessments (3) Family psychoeducation and support |
The team consisted of a psychologist/psychiatrist, a psychiatric social worker, a social service officer, and a psychiatric nurse/nurse assistant |
| Stravynski [72] | Social skills training vs. Social skill training + cognitive modification | Face-to-face sessions (individual) |
12 sessions, 90 min per session Duration of intervention: 14 weeks |
Social skills training: focused on individual needs by discussing specific social targets; techniques included instructions, modelling, role-rehearsal, feedback, self-monitoring, and homework Social skill training + cognitive modification: previously described elements for social skills training. For cognitive modification, participants analysed a distressing event in five steps: (1) activating event with descriptions; (2) irrational beliefs; (3) emotional consequences; (4) dispute; (5) plan for new actions |
Provided by one psychiatrist |
| Atkinson [67] | The education group vs. waiting-list control | Face-to-face sessions (group) |
1.5 h per session Duration of intervention: 20 weeks |
The education group: sessions generally covered schizophrenia topics, and alternated between an information session and a problem-solving session | Led by community psychiatric nurses, occupational therapists and registrars. Trainings were also provided |
| Terzian [73] | Social network intervention + usual treatments vs. usual treatments | Face-to-face (individual) |
Unclear information regarding intervention sessions Duration of intervention: 3–6 months |
Social network intervention: participants were helped to identify their possible areas of interest, and social activities were suggested | Provided by a staff member or natural facilitators such as families, neighbours, or volunteers |
| Hasson-Ohayon [68] | Social Cognition and Interaction Training (SCIT) + social mentoring vs. social mentoring only | Face-to-face sessions (group) |
SCIT intervention: 1 h weekly session Social mentoring service: 3 weekly meetings Duration of intervention: unclear |
Participants received social, leisure, support, and employment services, as well as standard services SCIT intervention group: besides intervention, they also received educational handouts, videos, and slides All received the same social mentoring services to support practical steps toward achieving personally meaningful goals |
Social mentors were staff of psychiatric rehabilitation agencies Lead clinicians received training and ongoing supervision. All clinicians had experiences in providing psychiatric rehabilitation services and completed a SCIT workshop |
| Rivera [77] | Peer-assisted care vs. Nonconsumer assisted vs. standard care vs. clinic-based care | Face-to-face sessions (group & individual), and phone calls |
Unclear information regarding intervention sessions and duration But telephone coverage is 24 h |
Peer assisted care group: professionals provided conventional crisis management, therapeutic services and concrete services; paraprofessional consumers facilitated social networks and provided social support through activities, home visits and phone calls Clinic based care group: only provided office-based services |
All professionals were licensed clinical social workers, also received training and supervisions Consumers had a history of multiple hospitalisations for mood or psychotic disorders, were eligible for disability benefits, relied on medication, but had 3–8 years of sobriety and stability. They had the same trainings as professional, and were supervised by social worker |
| Solomon [74] | Consumer case management team vs. nonconsumer management team | Face-to-face sessions (individual) |
The consumer team: Three times per week The nonconsumer team: met biweekly Duration of the intervention: 2 years |
Case managers offered individualised social support for community living, activities included goals related to income, living situation, social and family relations, and psychiatric treatment |
Requirements for consumer case managers: have a major mental health disorder; at least one prior psychiatric hospitalisation and a minimum of 14 days of psychiatric hospitalisation, or at least 5 psychiatric emergency service contacts over a 1-year period; regular contact in community mental health services, psychosocial services, or other outpatient treatment Consumer team: 3 consumer managers and 1 nonconsumer case manager initially, later, the nonconsumer member was replaced by a consumer, and a clinical director and a psychiatrist started involved. Consumer mangers received supervisions and support Nonconsumer team: all nonconsumer managers, two specialists started involved at the second year. Managers received supervisions and support The interviewer: a trained professional research worker independent of service providers. Intensive, experiential training was provided in both the Brief Psychiatric Rating Scale (BPRS) and Addiction Severity Index (ASI) |
| Marzillier [75] | Systematic Desensitisation (SD) vs. Social Skills Training (SST) vs. waiting-list control | Face-to-face sessions (individual) |
15 45-min sessions, once a week, occasionally twice a week Duration of intervention: 3 and half months |
Systematic desensitisation: included relaxation training and hierarchy construction, practice in both imagination and reality Social skills training: combined elements of both assertive and social skills training, included role playing, modelling, and practice in real-life and with volunteers |
Assessments were done by 2 independent assessors; one was a trained psychologist, and the other was a senior psychiatrist The therapist was a trained clinical psychologist with experience in behavioural treatments |
| Bøen [69] | A preventive senior centre group programme vs. control | Face-to-face sessions (group) |
Weekly group meetings, 3 h per meeting, about 35–38 times totally; Duration of intervention: 1 year |
The experimental group: included group meeting, physical training programme, and a self-help group. Transportation and warm meals were also provided | The team consisted of volunteers; all completed a training course and were supervised by a registered nurse and an experienced senior centre leader |
| Cole [76] | Home assessment group vs. clinic assessment group | Face-to-face sessions (individual) | Unclear | Unclear | Study psychiatrists (MC or DR) assessed participants |
| Trials for both subjective and objective social isolation | |||||
| Schene [89] | Psychiatric day treatment vs. inpatient treatment | Varied: mostly face-to-face sessions or phone interview (group and individual) |
Day treatment: length of programme varied Average duration of intervention: 37.6 weeks Inpatient treatment: length of programmes varied Average duration of intervention: 24.9 weeks |
Nine main groups of treatment programmes: (1) individual psychotherapy or supportive therapy; (2) individual counselling; (3) group psychotherapy; (4) sociotherapy; (5) family counselling; (6) occupational therapy; (7) psychomotor therapy; (8) drama therapy; (9) secondary environmental activities Extra care for day clinic participants after office hours, such as phone call or face-to-face talks with resident on duty in the clinic, or use of clinical bed |
Social psychiatric nurses, psychiatrists, and psychologists |
| Castelein [86] | Care as usual + GPSG vs. a waiting- list condition | Face-to-face sessions (group) |
90 min per session, 16 biweekly sessions Duration of intervention: 8 months |
Peer support group: included about 10 patients, patients decided the topic of each session, discussing daily life experiences in pairs and groups | Nurses guided the peer groups with minimal involvement |
| Gelkopf [87] | Video projection of humorous movies vs. control group | Face-to-face sessions (group) |
The experimental group: four times daily (5 days a week) Duration of intervention: 3 months |
The experimental group: exposed exclusively to comedies The control group: 15% of the films were comedies; others are different types of films |
A psychology student was involved to answer questions during experimental testing |
| Ammerman [88] | IH-CBT + home visiting vs. home visit alone | Face-to-face sessions (individual) |
15 weekly sessions, 60 min per session with a booster session 1 month after treatment Duration of intervention: about 5 months |
IH-CBT: primarily targeted depression reduction, consisted of behavioural activation, identification of automatic thoughts and schemas, thought restructuration, and relapse prevention | 2 licensed master level social workers, received weekly supervision, a review of audiotaped sessions and a self-report checklist |
Appendix 6: Quality assessment
| First author (publication year) | Sequence generation | Allocation concealment | Blinding | Incomplete outcome data | Selective outcome reporting | Other sources of bias |
|---|---|---|---|---|---|---|
| Kaplan [53] | Low risk | Unclear | High risk | Unclear | Low risk | Low risk |
| Hasson-Ohayon [42] | Low risk | Unclear | High risk | Unclear | Low risk | High risk |
| Rotondi [54] | Unclear | Unclear | High risk | Unclear | Low risk | High risk |
| Silverman [43] | Unclear | Unclear | High risk | Unclear | Low risk | Low risk |
| Boevink [44] | Low risk | Unclear | High risk | Unclear | Low risk | Low risk |
| Zang [46] | Low risk | Unclear | High risk | Unclear | Low risk | High risk |
| Zang [47] | Low risk | Unclear | High risk | Unclear | Low risk | High risk |
| Gawrysiak [48] | Unclear | Unclear | High risk | Unclear | Low risk | Low risk |
| Bjorkman [50] | Low risk | Low risk | High risk | Unclear | Low risk | High risk |
| Mendelson [51] | Unclear | Unclear | High risk | Unclear | Low risk | High risk |
| O’Mahen [55] | Low risk | Low risk | High risk | Low risk | Low risk | Low risk |
| Conoley [49] | Unclear | Unclear | High risk | Unclear | Low risk | High risk |
| Eggert [45] | Unclear | Unclear | High risk | Unclear | Low risk | High risk |
| Masia-Warner [52] | Unclear | Unclear | High risk | Low risk | Low risk | High risk |
| Interian [56] | Low risk | Unclear | High risk | Unclear | Low risk | High risk |
| Solomon [70] | Unclear | Unclear | High risk | Low risk | Low risk | High risk |
| Aberg-Wistedt [71] | Unclear | Unclear | High risk | Unclear | Low risk | High risk |
| Atkinson [67] | Unclear | Unclear | High risk | Unclear | Low risk | High risk |
| Terzian [73] | Unclear | Low risk | High risk | Unclear | Low risk | High risk |
| Hasson-Ohayon [68] | Unclear | Unclear | High risk | Unclear | Low risk | High risk |
| Rivera [77] | Unclear | Low risk | High risk | Low risk | Low risk | Low risk |
| Solomon [74] | Unclear | Unclear | High risk | Low risk | Low risk | High risk |
| Marzillier [75] | Low risk | Low risk | High risk | Unclear | Low risk | High risk |
| Stravynski [72] | Unclear | Unclear | High risk | Unclear | Low risk | High risk |
| Bøen [69] | Low risk | Low risk | High risk | Unclear | Low risk | High risk |
| Cole [76] | Low risk | Low risk | High risk | Low risk | Low risk | High risk |
| Schene [89] | Unclear | Unclear | High risk | Unclear | Low risk | High risk |
| Castelein [86] | Low Risk | Low risk | High risk | Unclear | Low risk | High risk |
| Gelkopf [87] | Low risk | Unclear | High risk | Unclear | Low risk | High risk |
| Ammerman [88] | Unclear | Low risk | High risk | Low risk | Low risk | High risk |
Author contributions
SJ, BLE and RM conceived the review. SJ and BLE commented on search strategy and review protocol, JW recommended search terms. RM developed the search strategy and created review protocol, conducted the literature search, wrote and co-ordinated the drafts. RM, FM and AA independently contributed to the screening process. RM and FM extracted data. RM, FM and JT independently assessed the methodological quality of each included paper. RM screened reference lists of included studies and relevant systematic reviews and meta-analyses. SJ involved in any disagreement between reviewers in the screening process. SJ, BLE, FM and JW contributed comments to the drafts. All authors read and approved the final manuscript.
Compliance with ethical standards
Conflict of interest
The authors state that they have no conflicts of interest.
Footnotes
This article is part of the focused issue ‘Loneliness: contemporary insights on causes, correlates, and consequences’.
References
*Studies included in the systematic review
- 1.Wang J, Lloyd-Evans B, Giacco D, et al. Social isolation in mental health: a conceptual and methodological review. Soc Psychiatry Psychiatr Epidemiol. 2016;52:1451–1461. doi: 10.1007/s00127-017-1446-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coyle CE, Dugan E. Social isolation, loneliness and health among older adults. J Aging Health. 2012;24(8):1346–1363. doi: 10.1177/0898264312460275. [DOI] [PubMed] [Google Scholar]
- 3.Andersson L. Loneliness research and interventions: a review of the literature. Aging Ment Health. 1998;2(4):264–274. doi: 10.1080/13607869856506. [DOI] [Google Scholar]
- 4.Peplau LA, Perlman D. Theoretical approaches to loneliness. In: Peplau LA, Perlman D, editors. Loneliness: a sourcebook of current theory, research and therapy. New York: Wiley; 1982. pp. 1–134. [Google Scholar]
- 5.Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. 2011;52(2):145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- 6.Hays RD, DiMatteo MR. A short form measure of loneliness. J Pers Assess. 1987;51(1):69–81. doi: 10.1207/s15327752jpa5101_6. [DOI] [PubMed] [Google Scholar]
- 7.Wilson WJ. The truly disadvantaged: the inner city, the underclass, and public policy. Chicago: The University of Chicago Press; 1987. [Google Scholar]
- 8.Wenger GC, Davies R, Shahtahmasebi S, Scott A. Social isolation and loneliness in old age: review and model refinement. Ageing Soc. 1996;16:333–358. doi: 10.1017/s0144686x00003457. [DOI] [Google Scholar]
- 9.Victor CR, Scambler SJ, Bowling A, Bond J. The prevalence of, and risk factors for, loneliness in later life: a survey of older people in Great Britain. Ageing Soc. 2005;25:357–375. [Google Scholar]
- 10.Meltzer H, Bebbington P, Dennis MS, et al. Feelings of loneliness among adults with mental disorder. Soc Psychiatry Psychiatr Epidemiol. 2013;48(1):5–13. doi: 10.1007/s00127-012-0515-8. [DOI] [PubMed] [Google Scholar]
- 11.Boeing L, Murray V, Pelosi A, McCabe R, Blackwood D, Wrate R. Adolescent-onset psychosis: prevalence, needs and service provision. Br J Psychiatry. 2007;190:18–26. doi: 10.1192/bjp.190.1.18. [DOI] [PubMed] [Google Scholar]
- 12.Remschmidt HE, Schulz E, Martin M, Warnke A, Trott GE. Childhood-onset schizophrenia: history of the concept and recent studies. Schizophr Bull. 1994;20:727–745. doi: 10.1093/schbul/20.4.727. [DOI] [PubMed] [Google Scholar]
- 13.Russell DW, Cutrona CE, de la Mora A, Wallace RB. Loneliness and nursing home admission among rural older adults. Psychol Aging. 1997;12(4):574–589. doi: 10.1037//0882-7974.12.4.574. [DOI] [PubMed] [Google Scholar]
- 14.Cacioppo JT, Hawkley LC, Crawford LE, et al. Loneliness and health: potential mechanisms. Psychosom Med. 2002;64:407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Alpass FM, Neville S. Loneliness, health and depression in older males. Aging Ment Health. 2003;7:212–216. doi: 10.1080/1360786031000101193. [DOI] [PubMed] [Google Scholar]
- 16.Holwerda TJ, Beekman AT, Deeg DJ, Stek ML, van Tilburg TG, et al. Increased risk of mortality associated with social isolation in older men: only when feeling lonely? Results from the Amsterdam Study of the Elderly (AMSTEL) Psychol Med. 2012;42:843–853. doi: 10.1017/S0033291711001772. [DOI] [PubMed] [Google Scholar]
- 17.Bastiaansen D, Koot HM, Ferdinand RF. Determinants of quality of life in children with psychiatric disorders. Qual Life Res. 2005;14(6):1599–1612. doi: 10.1007/s11136-004-7711-2. [DOI] [PubMed] [Google Scholar]
- 18.Pernice-Duca F. Family network support and mental health recovery. J Marital Fam Ther. 2010;36(1):13–27. doi: 10.1111/j.1752-0606.2009.00182.x. [DOI] [PubMed] [Google Scholar]
- 19.Wang JY, Mann F, Lloyd-Evans B, Ma RM, Johnson S. Association between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. 2018;18(1):156. doi: 10.1186/s12888-018-1736-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Research Council (2011) Explaining divergent levels of longevity in high-income countries. In: Crimmins EM, Preston SH, Cohen B (eds) Panel on understanding divergent trends in longevity in high-income countries. Committee on Population, Division of Behavioral and Social Sciences and Education. The National Academies Press, Washington, DC. https://www.ncbi.nlm.nih.gov/books/NBK62369/pdf/Bookshelf_NBK62369.pdf on July 2019 [PubMed]
- 22.Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. Social isolation: a predictor of mortality comparable to traditional clinical risk factors. Am J Public Health. 2013;103(11):2056–2062. doi: 10.2105/AJPH.2013.301261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bratlien U, Øie M, Haug E, et al. Environmental factors during adolescence associated with later development of psychotic disorders—a nested case–control study. Psychiatry Res. 2014;215(3):579–585. doi: 10.1016/j.psychres.2013.12.048. [DOI] [PubMed] [Google Scholar]
- 24.Palumbo C, Volpe U, Matanov A, Priebe S, Giacco D. Social networks of patients with psychosis: a systematic review. BMC Res Notes. 2015;8:560. doi: 10.1186/s13104-015-1528-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Drolet L et al (2013) Assess the contribution of social factors on cognitive performance in older adults. Inpact 2013: international psychological applications conference and trends, pp 282–284
- 26.Goldberg RW, Rollins AL, Lehman AF. Social network correlates among people with psychiatric disabilities. Psychiatr Rehabil J. 2003;26(4):393–402. doi: 10.2975/26.2003.393.402. [DOI] [PubMed] [Google Scholar]
- 27.Davidson L, Stayner D. Loss, loneliness, and the desire for love: perspectives on the social lives of people with schizophrenia. Psychiatr Rehabil J. 1997;20(3):3–12. [Google Scholar]
- 28.Holwerda TJ, Deeg DJ, Beekman AT, et al. Feelings of loneliness, but not social isolation, predict dementia onset: results from the Amsterdam Study of the Elderly (AMSTEL) J Neurol Neurosurg Psychiatry. 2014;85(2):135–142. doi: 10.1136/jnnp-2012-302755. [DOI] [PubMed] [Google Scholar]
- 29.Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE. Reducing suicide: a national imperative. Washington, DC: National Academy Press; 2002. [PubMed] [Google Scholar]
- 30.Findlay RA. Interventions to reduce social isolation amongst older people: where is the evidence? Ageing Soc. 2003;23:647–658. [Google Scholar]
- 31.Lim MH, Penn DL, Thomas N, Gleeson JFM. Is loneliness a feasible treatment target in psychosis? Soc Psychiatry Psychiatr Epidemiol. 2019 doi: 10.1007/s00127-019-01731-9. [DOI] [PubMed] [Google Scholar]
- 32.Cattan M, White M, Bond J, Learmouth A. Preventing social isolation and loneliness among older people: a systematic review of health promotion interventions. Ageing Soc. 2005;25:41–667. doi: 10.1017/S0144686X04002594. [DOI] [PubMed] [Google Scholar]
- 33.Dickens AP, Richards SH, Greaves CJ, Campbell JL. Interventions targeting social isolation in older people: a systematic review. BMC Public Health. 2011;11:647. doi: 10.1186/1471-2458-11-647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Masi CM, Chen H-Y, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Pers Soc Pyschol Rev. 2011 doi: 10.1177/1088868310377394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Perese EF, Wolf M. Combating loneliness among persons with severe mental illness: social network interventions’ characteristics, effectiveness, and applicability. Issues Ment Health Nurs. 2005;26(6):591–609. doi: 10.1080/01612840590959425. [DOI] [PubMed] [Google Scholar]
- 36.Newlin M, Webber M, Morris D, Howarth S. Social participation interventions for adults with mental health problems: a review and narrative synthesis. Soc Work Res. 2015;39(3):167–180. doi: 10.1093/swr/svv015. [DOI] [Google Scholar]
- 37.Anderson K, Laxhman N, Priebe S. Can mental health interventions change social networks? A systematic review. BMC Psychiatry. 2015;15:297. doi: 10.1186/s12888-015-0684-. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Webber M, Fendt-Newlin M. A review of social participation interventions for people with mental health problems. Soc Psychiatry Psychiatr Epidemiol. 2017;52:369–380. doi: 10.1007/s00127-017-1372-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mann F, Bone JK, Lloyd-Evans B, et al. A life less lonely: the state of the art in interventions to reduce loneliness in people with mental health problems. Soc Psychiatry Psychiatr Epidemiol. 2017;52:627–638. doi: 10.1007/s00127-017-1392-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Higgins JPT, Green S (2011) Assessing risk of bias in included studies, chapter 8. In: Higgins JPT, Altman DG, Sterne JAC (eds) On behalf of the Cochrane Statistical Methods Group and the Cochrane Bias Methods Group: Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. http://www.handbook.cochrane.org. Retrieved Oct 2016
- 41.Popay J, Roberts H et al (2006) Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC Methods Programme. Lancaster University. 10.13140/2.1.1018.4643. https://www.researchgate.net/publication/233866356_Guidance_on_the_conduct_of_narrative_synthesis_in_systematic_reviews_A_product_from_the_ESRC_Methods_Programme. Retrieved Oct 2016
- 42.Hasson-Ohayon I, Roe D, Kravetz S. A randomized controlled trial of the effectiveness of the illness management and recovery program. Psychiatr Serv. 2007;58(11):1461–1466. doi: 10.1176/ps.2007.58.11.1461. [DOI] [PubMed] [Google Scholar]
- 43.Silverman MJ. Effects of a live educational music therapy intervention on acute psychiatric inpatients’ perceived social support and trust in the therapist: a four-group randomized effectiveness study. J Music Ther. 2014;51(3):228–249. doi: 10.1093/jmt/thu011. [DOI] [PubMed] [Google Scholar]
- 44.Boevink W, Kroon H, van Vugt M, Delespaul P, van Os J. A user-developed, user run recovery programme for people with severe mental illness: a randomised control trial. Psychosis. 2016;8(4):287–300. [Google Scholar]
- 45.Eggert LL, Elaine RN, Thompson A, et al. Reducing suicide potential among high-risk youth: tests of a school-based prevention program. Suicide Life Threat Behav. 1995;25(2):276–296. [PubMed] [Google Scholar]
- 46.*Zang Y, Hunt N, Cox T (2014) Adapting narrative exposure therapy for Chinese earthquake survivors: a pilot randomised controlled feasibility study. BMC Psychiatry 14:262. http://www.biomedcentral.com/1471-244X/14/262 [DOI] [PMC free article] [PubMed]
- 47.Zang Y, Hunt N, Cox T. A randomised controlled pilot study: the effectiveness of narrative exposure therapy with adult survivors of the Sichuan earthquake. BMC Psychiatry. 2013;13:41. doi: 10.1186/1471-244x-13-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gawrysiak M, Nicholas C, Hopko DR. Behavioral activation for moderately depressed university students: randomized controlled trial. J Couns Psychol. 2009;56(3):468–475. [Google Scholar]
- 49.Conoley CW, Garber RA. Effects of reframing and self-control directives on loneliness, depression, and controllability. J Couns Psychol. 1985;32:139–142. [Google Scholar]
- 50.Bjorkman T, Hansson L, Sandlund M. Outcome of case management based on the strengths model compared to standard care. A randomised controlled trial. Soc Psychiatry Psychiatr Epidemiol. 2002;37(4):147–152. doi: 10.1007/s001270200008. [DOI] [PubMed] [Google Scholar]
- 51.Mendelson T, Leis JA, Perry DF, Stuart EA, Tandon DS. Impact of a preventive intervention for perinatal depression on mood regulation, social support, and coping. Arch Womens Ment Health. 2013;16(3):211–218. doi: 10.1007/s00737-013-0332-4. [DOI] [PubMed] [Google Scholar]
- 52.Masia-Warner C, Klein RG, Dent HC, et al. School-based intervention for adolescents with social anxiety disorder: results of a controlled study. J Abnorm Child Psychol. 2005;33(6):707–722. doi: 10.1007/s10802-005-7649-z. [DOI] [PubMed] [Google Scholar]
- 53.Kaplan K, Salzer M, Solomon P, Brusilovskiy E, Cousounis P. Internet peer support for individuals with psychiatric disabilities: a randomized controlled trial. Soc Sci Med. 2011;72:54–62. doi: 10.1016/j.socscimed.2010.09.037. [DOI] [PubMed] [Google Scholar]
- 54.Rotondi AJ, Haas GL, Anderson CM, et al. A clinical trial to test the feasibility of a telehealth psychoeducational intervention for persons with schizophrenia and their families: intervention and 3-month findings. Rehabil Psychol. 2005;50(4):325–336. doi: 10.1037/0090-5550.50.4.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.O’Mahen HA, Richards DA, Woodford J, et al. Netmums: a phase II randomized controlled trial of a guided Internet behavioural activation treatment for postpartum depression. Psychol Med. 2014;44(8):1675–1689. doi: 10.1017/S0033291713002092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Interian A, Kline A, Perlick D, et al. Randomized controlled trial of a brief Internet-based intervention for families of Veterans with posttraumatic stress disorder. J Rehabil Res Dev. 2016;53(5):629–640. doi: 10.1682/JRRD.2014.10.0257. [DOI] [PubMed] [Google Scholar]
- 57.Zimet GD, Powell SS, Farley GK, et al. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess. 1990;55:610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 58.De Jong Gierveld J, Van Tilburg T. Manual of the Loneliness Scale. Amsterdam: VU University, Faculty of Social Sciences, Department of Sociology; 1991. [Google Scholar]
- 59.Russell D, Peplau LA, Cutrona CE. The Revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J Pers Soc Psychol. 1980;39:472–480. doi: 10.1037//0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- 60.Russell D. The Causal Dimension Scale: a measure of how individuals perceive causes. J Pers Soc Psychol. 1982;42:1137–1145. [Google Scholar]
- 61.Henderson S, Duncan-Jones P, Byrne DG, Scott R. Measuring social relationships: the Interview Schedule for Social Interaction. Psychol Med. 1980;10:723–734. doi: 10.1017/s003329170005501x. [DOI] [PubMed] [Google Scholar]
- 62.Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. J Appl Soc Psychol. 1983;13:99–125. [Google Scholar]
- 63.Asher SR, Wheeler VA. Children’s loneliness: a comparison of rejected and neglected peer status. J Consult Clin Psychol. 1985;53:500–505. doi: 10.1037//0022-006x.53.4.500. [DOI] [PubMed] [Google Scholar]
- 64.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 65.Krause N, Markides K. Measuring social support among older adults. Int J Aging Hum Dev. 1990;30:37–53. doi: 10.2190/CY26-XCKW-WY1V-VGK3. [DOI] [PubMed] [Google Scholar]
- 66.Cutrona CE, Russell D. The provisions of social relationships and adaptation to stress. In: Jones H, Perlman D, editors. Advances in personal relationships. Greenwich: JAI Press; 1987. pp. 37–67. [Google Scholar]
- 67.Atkinson JM, Coia DA, Gilmour HG, Harper JP. The impact of education groups for people with schizophrenia on social functioning and quality of life. Br J Psychiatry. 1996;168(2):199–204. doi: 10.1192/bjp.168.2.199. [DOI] [PubMed] [Google Scholar]
- 68.Hasson-Ohayon I, Mashiach-Eizenberg M, Avidan M, Roberts DL, Roe D. Social cognition and interaction training: preliminary results of an RCT in a community setting in Israel. Psychiatr Serv. 2014;65:555–558. doi: 10.1176/appi.ps.201300146. [DOI] [PubMed] [Google Scholar]
- 69.Bøen H, Dalgard OS, Johansen R, Nord E. A randomized controlled trial of a senior centre group programme for increasing social support and preventing depression in elderly people living at home in Norway. BMC Geriatr. 2012;12:20. doi: 10.1186/1471-2318-12-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Solomon P, Draine J. One year outcomes of a randomized trial of case management. Eval Programme Plan. 1995;18(2):117–127. [Google Scholar]
- 71.Aberg-Wistedt A, Cressell T, Lidberg Y, Liljenberg B, Osby U. Two-year outcome of team-based intensive case management for patients with schizophrenia. Psychiatr Serv. 1995;46(12):1263–1266. doi: 10.1176/ps.46.12.1263. [DOI] [PubMed] [Google Scholar]
- 72.Stravynski A, Marks I, Yule W. Social skills problems in neurotic outpatients. Social skills training with and without cognitive modification. Arch Gen Psychiatry. 1982;39(12):1378–1385. doi: 10.1001/archpsyc.1982.04290120014003. [DOI] [PubMed] [Google Scholar]
- 73.Terzian E, Tognoni G, Bracco R, et al. Social network intervention in patients with schizophrenia and marked social withdrawal: a randomized controlled study. Can J Psychiatry. 2013;58(11):622–631. doi: 10.1177/070674371305801108. [DOI] [PubMed] [Google Scholar]
- 74.Solomon P, Draine J. The efficacy of a consumer case management team: 2-year outcomes of a randomized trial. J Ment Health Admin. 1995;22(2):135–146. doi: 10.1007/BF02518754. [DOI] [PubMed] [Google Scholar]
- 75.Marzillier J, Lambert C, Kellett J. A controlled evaluation of systematic desensitization and social skills training for socially inadequate psychiatric patients. Behav Res Ther. 1976;14:225–238. doi: 10.1016/0005-7967(76)90015-2. [DOI] [PubMed] [Google Scholar]
- 76.Cole MG, Rochon DT, Engelsmann F, Ducic D. The impact of home assessment on depression in the elderly: a clinical trial. Int J Geriatr Psychiatry. 1995;10(1):19–23. [Google Scholar]
- 77.Rivera J, Sullivan AM, Valenti SS. Adding consumer-providers to intensive case management: does it improve outcome? Psychiatr Serv. 2007;58:802–809. doi: 10.1176/appi.ps.58.6.802. [DOI] [PubMed] [Google Scholar]
- 78.Dunn M, O’Drischoll C, Dayson D, et al. The TAPS project 4: an observational study of the social life of long stay patients. Br J Psychiatry. 1990;157:842–848. doi: 10.1192/bjp.157.6.842. [DOI] [PubMed] [Google Scholar]
- 79.Birchwood M, Smith J, Cochrane R, et al. The Social Functioning Scale: the development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Br J Psychiatry. 1990;157:853–859. doi: 10.1192/bjp.157.6.853. [DOI] [PubMed] [Google Scholar]
- 80.Korkeila J, Lehtinen V, Bijl R, et al. Establishing a set of mental health indicators for Europe. Scand J Public Health. 2003;31:451–459. doi: 10.1080/14034940210165208. [DOI] [PubMed] [Google Scholar]
- 81.Pattison EM, Difrancisco D, Wood P, Frazier H, Crowder JA. A psychosocial kinship model for family therapy. Am J Psychiatry. 1975;132:1246–1251. doi: 10.1176/ajp.132.12.1246. [DOI] [PubMed] [Google Scholar]
- 82.Swaling J, Ensani S, Lundgren K, et al. Social network therapy at a child and youth clinic. J Soc Med. 1990;1–2:56–64. [Google Scholar]
- 83.Gurland B, Yorkston NJ, Stone AR, et al. The structured and scaled interview to assess maladjustment. Arch Gen Psychiatry. 1972;27:259–267. doi: 10.1001/archpsyc.1972.01750260101017. [DOI] [PubMed] [Google Scholar]
- 84.Centre for Aging and Human Development . Multi-dimensional functional assessment: the OARS methology. 2. Durham: Centre for Aging and Human Development, Duke University; 1978. [Google Scholar]
- 85.Pattison EM, et al. A theoretical–empirical base for social system therapy. In: Foulks EF, Wintrob RN, Westermyer J, et al., editors. Current perspectives in cultural psychiatry. New York: Spectrum; 1977. [Google Scholar]
- 86.Castelein S, Bruggeman R, van Busschbach JT, et al. The effectiveness of peer support groups in psychosis: a randomized controlled trial. Acta Psychiatr Scand. 2008;118(1):64–72. doi: 10.1111/j.1600-0447.2008.01216.x. [DOI] [PubMed] [Google Scholar]
- 87.Gelkopf M, Sigal M, Kramer R. Therapeutic use of humor to improve social support in an institutionalized schizophrenic inpatient community. J Soc Psychol. 1994;134(2):175–182. doi: 10.1080/00224545.1994.9711380. [DOI] [PubMed] [Google Scholar]
- 88.Ammerman RT, Putnam FM, Altaye M, et al. Treatment of depressed mothers in home visiting: impact on psychological distress and social functioning. Child Abuse Neglect. 2013;37(8):544–554. doi: 10.1016/j.chiabu.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Schene AH, van Wijngaarden B, Poelijoe NW, Gersons BPR. The Utrecht comparative study on psychiatric day treatment and inpatient treatment. Acta Psychiatr Scand. 1993;87(6):427–436. doi: 10.1111/j.1600-0447.1993.tb03400.x. [DOI] [PubMed] [Google Scholar]
- 90.Bridges KR, Sanderman R, van Sonderen E. An English language version of the Social Support List: preliminary reliability. Psychol Rep. 2002;90:1055–1058. doi: 10.2466/pr0.2002.90.3.1055. [DOI] [PubMed] [Google Scholar]
- 91.Sarason IG, Sarason BR, Shearin EN, Pierce GR. A brief measure of social support: practical and theoretical implications. J Soc Pers Relat. 1987;4:497–510. [Google Scholar]
- 92.Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM., Jr Social ties and susceptibility to the common cold. JAMA. 1997;277:1940–1944. [PubMed] [Google Scholar]
- 93.Wijngaarden BV. Social network, social steun, gebeurtenissen vragenlijst. Utrecht: Rijksuniversiteit Utrecht; 1987. [Google Scholar]
- 94.Daumerie N, Vasseur Bacle S, Giordana JY, Bourdais Mannone C, Caria A, Roelandt JL. Discrimination perceived by people with a diagnosis of schizophrenic disorders. INternational study of DIscrimination and stiGma Outcomes (INDIGO): French results. Encephale. 2012;3:224–231. doi: 10.1016/j.encep.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 95.Cacioppo JT, Hawkley LC. Loneliness. In: Leary MR, Hoyle RH, editors. Handbook of individual differences in social behaviour. New York: Guilford Press; 2009. pp. 227–239. [Google Scholar]
- 96.Lim MH, Gleeson JFM, Rodebaugh TL, Eres R, Long KM, Casey K, Abbott JM, Thomas N, Penn DL. A pilot digital intervention targeting loneliness in young people with psychosis. Soc Psychiatry Psychiatr Epidemiol. 2019 doi: 10.1007/s00127-019-01681-2. [DOI] [PubMed] [Google Scholar]
- 97.Weiss CH. Nothing as practical as good theory: exploring theory-based evaluation for comprehensive community initiatives for children and families. In: Connell JP, Kubisch AC, Schorr LB, Weiss CH, editors. New Approaches to evaluating community initiatives, vol 1. Concepts, methods and contexts. Washington, DC: The Aspen Institute; 1995. pp. 65–92. [Google Scholar]
- 98.De Silva MJ, Breuer E, Lee L, Asher L, Chowdhary N, Lund C, Patel V. Theory of change: a theory-driven approach to enhance the medical research council’s framework for complex interventions. Trials. 2014;15:267. doi: 10.1186/1745-6215-15-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cacioppo S, Grippo AJ, London S, Gossens L, Cacioppo JT. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10(2):238–249. doi: 10.1177/1745691615570616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Davison KP, Pennebaker JW, Dickerson SS. Who Talks? The social psychology of illness support groups. Am Psychol. 2000;55:205–217. [PubMed] [Google Scholar]
- 101.Lui JHL, Marcus DK, Barry CT. Evidence-based apps? A review of mental health mobile applications in a psychotherapy context. Prof Psychol Res Pract. 2017 doi: 10.1037/pro0000122. [DOI] [Google Scholar]
- 102.Donker T, Petrie K, Proudfoot J et al (2013) Smartphones for Smarter Delivery of Mental Health Programs: a systematic review. J Med Internet Res 15(11):e247. 10.2196/jmir.2791 (published online 15 Nov 2013). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3841358/#ref7 (accessed Feb 2018) [DOI] [PMC free article] [PubMed]
- 103.Andrews G, Basu A, Cuijpers P, Craske MG, McEvoy P, English CL, Newby JM. Computer therapy for the anxiety and depression disorders is effective, acceptable and practical health care: an update meta-analysis. J Anxiety Disord. 2018;55:70–78. doi: 10.1016/j.janxdis.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 104.Spek V, Cuijpers P, Nyklícek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med. 2007;3:319–328. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- 105.Alvarez-Jimenez M, Alcazar-Corcoles MA, Blanch CG, Bendall S, McGorry PD, Gleeson JF. Online, social media and mobile technologies for psychosis treatment: a systematic review on novel user-led interventions. Schizophr Res. 2014;16:96–106. doi: 10.1016/j.schres.2014.03.021. [DOI] [PubMed] [Google Scholar]
- 106.Alvarez-Jimenez M, et al. On the HORYZON: moderated online social therapy for long-term recovery in first episode psychosis. Schizophr Res. 2012 doi: 10.1016/j.schres.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 107.Alvarez-Jimenez M, Bendall S, Koval P, et al. HORYZONS trial: protocol for a randomised controlled trial of a moderated online social therapy to maintain treatment effects from first-episode psychosis services. BMJ Open. 2019;9:e024104. doi: 10.1136/bmjopen-2018-024104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Harrop C, Ellett L, Brand R, Lobban F. Friends interventions in psychosis: a narrative review and call to action. Early Interv Psychiatry. 2015;9(4):269–278. doi: 10.1111/eip.12172. [DOI] [PubMed] [Google Scholar]
- 109.Biegel D, Tracy E, Corvo K. Strengthening social networks: intervention strategies for mental health case managers. Health Soc Work. 1994;19(3):206–216. doi: 10.1093/hsw/19.3.206. [DOI] [PubMed] [Google Scholar]
- 110.Hector-Taylor L, Adams P. State versus trait loneliness in elderly New Zealanders. Psychol Rep. 1996;78:1329–1330. doi: 10.2466/pr0.1996.78.3c.1329. [DOI] [PubMed] [Google Scholar]
- 111.Fokkema T, De Jong Gierveld J, Dykstra PA. Cross-national differences in older adult loneliness. J Psychol. 2012;146(1–2):201–228. doi: 10.1080/00223980.2011.631612. [DOI] [PubMed] [Google Scholar]
- 112.Ross CE, Jang SJ. Neighborhood disorder, fear, and mistrust: the buffering role of social ties with neighbors. Am J Community Psychol. 2000;28:401–420. doi: 10.1023/a:1005137713332. [DOI] [PubMed] [Google Scholar]
- 113.Ackley B, Ladwig G. Nursing diagnosis handbook: an evidence-based guide to planning care. 9. Mosby: Maryland Heights; 2010. [Google Scholar]
- 114.Lancet Editorial (2018) UK life science research: time to burst the biomedical bubble. Lancet 392:10143. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)31609-X/fulltext (accessed 16 Aug 2018) [DOI] [PubMed]
- 115.Russell D, Peplau LA, Ferguson ML. Developing a measure of loneliness. J Pers Assess. 1978;42:290–294. doi: 10.1207/s15327752jpa4203_11. [DOI] [PubMed] [Google Scholar]
- 116.de Jong-Gierveld J, Kamphuis F. The development of a Rasch-type loneliness scale. Appl Psychol Meas. 1985;9(3):289–299. doi: 10.1177/014662168500900307. [DOI] [Google Scholar]
- 117.Pattison EM, Pattison ML. Analysis of a schizophrenia psychosocial network. Schizophr Bull. 1981;7(1):135–143. doi: 10.1093/schbul/7.1.135. [DOI] [PubMed] [Google Scholar]