Abstract
Bimatoprost implant (Durysta™), developed by Allergan, is a sustained-release drug delivery system containing bimatoprost, a prostaglandin analogue with ocular hypotensive activity. The implant, administered intracamerally, involves the use of a biodegradable, solid polymer drug delivery system for slow, sustained drug release, designed to lower intraocular pressure (IOP) over a 4- to 6-months period. In March 2020, bimatoprost implant received its first approval, in the USA, for use to reduce IOP in patients with open angle glaucoma (OAG) or ocular hypertension (OHT). Allergan’s clinical development programme for bimatoprost implant is ongoing. This article summarizes the milestones in the development of bimatoprost implant leading to this first approval for use in the reduction of IOP in patients with OAG or OHT.
Bimatoprost Implant (DurystaTM): Key Points
| A biodegradable sustained-release intracameral implant containing the prostaglandin analogue bimatoprost |
| Developed by Allergan, bimatoprost implant received its first approval on 04 March 2020, in the USA |
| Approved for use to reduce IOP in patients with open angle glaucoma or ocular hypertension |
Introduction
Open-angle glaucoma (OAG) is a chronic and progressive eye disorder that is characterized by optic nerve damage and is commonly associated with elevated intraocular pressure (IOP) [1, 2]. In OAG, disease progression leads to irreversible visual field loss and, if untreated, can result in blindness. Management of OAG centres around the use of medications, laser trabeculoplasty or surgery (or a combination of the three) to lower IOP with the aim of preventing or slowing vision loss. First-line treatment for OAG usually involves the use of topical IOP-lowering medications, most commonly prostaglandin analogues (e.g. bimatoprost, latanoprost, tafluprost, travoprost). Other classes of topical IOP-lowering medications used for the treatment of OAG include cholinergic agonists (e.g. pilocarpine), β-adrenergic receptor blockers (e.g. timolol), α-adrenergic receptor agonists (e.g. brimonidine) and carbonic anhydrase inhibitors (e.g. brinzolamide) [1, 2].
Although topical medications are generally efficacious in lowering IOP, adherence issues frequently complicate disease management [3–6]. Factors reported to negatively impact adherence to topical IOP-lowering medications include a poor understanding of the disease, poor self-efficacy, difficulty in eye drop administration, forgetfulness, multiple dosing requirements, and adverse events [5]. To help overcome or circumvent adherence issues, sustained drug delivery systems have been investigated for the treatment of OAG and ocular hypertension (OHT) [7]. Bimatoprost implant (Durysta™), a bimatoprost sustained-release device developed by Allergan, received its first approval on 04 March 2020, in the USA, for use to reduce IOP in patients with OAG or OHT [8, 9]. The implant, approved for a single intracameral administration, consists of a biodegradable, solid polymer, sustained-release drug delivery 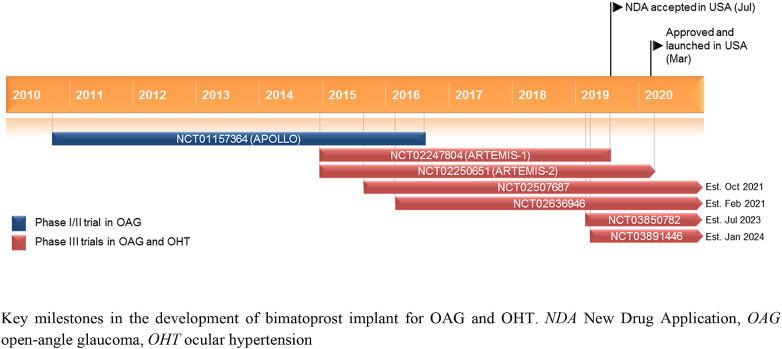 system containing a 10-μg bimatoprost dose [9]. A New Drug Application for bimatoprost implant for use in the treatment of OAG and/or OHT, supported by the findings of the phase III ARTEMIS-1 and ARTEMIS-2 clinical trials (Sect. 2.4.1), was accepted by the US FDA in July 2019 [10].
system containing a 10-μg bimatoprost dose [9]. A New Drug Application for bimatoprost implant for use in the treatment of OAG and/or OHT, supported by the findings of the phase III ARTEMIS-1 and ARTEMIS-2 clinical trials (Sect. 2.4.1), was accepted by the US FDA in July 2019 [10].
Company Agreements
Bimatoprost implant was originated and developed by Allergan. In March 2015, Allergan was acquired by Actavis [11]. Subsequently, in June 2015, Actavis changed its name to Allergan [12]. In May 2020, Allergan was acquired by, and merged into, AbbVie [13].
Scientific Summary
The US FDA-approved bimatoprost implant product is a sterile intracameral implant that consists of a 10-μg dose of bimatoprost held within a rod-shaped biodegradable solid polymer drug delivery system based on Allergan’s Novadur® platform [9, 14]. For the bimatoprost implant, the Novadur platform was modified to release bimatoprost with non-pulsatile, steady-state drug release [14]. The polymer drug delivery system in the bimatoprost implant consists of poly (d,l-lactide), poly (d,l-lactide-co-glycolide), poly (d,l-lactide) acid end, and polyethylene glycol 3350 [9] .
Drug Delivery
For administration, bimatoprost implant is supplied preloaded in a single-use applicator to facilitate injection directly into the anterior chamber of the eye [9]. With intracameral administration, the implant is designed to target drug delivery directly to the iris–ciliary body, the key site of action of prostaglandin analogue drugs [14]. Once in place, the polymer matrix of the insert slowly degrades (to lactic and glycolic acids), slowly releasing bimatoprost, with the aim to provide an IOP-lowering effect lasting 4–6 months [9, 14]. The intracameral injection procedure must be performed under magnification for clear visualization of the anterior chamber structures and should be carried out using aseptic conditions, with the patient’s head in a stabilized position [9]. The eye should not be dilated prior to the procedure. Bimatoprost implant is currently approved for a single intracameral administration [9].
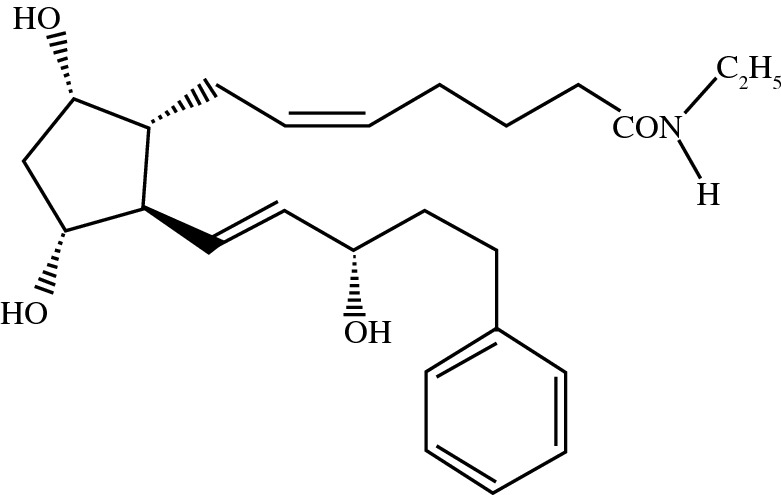
Chemical structure of bimatoprost
Features and properties of bimatoprost implant
| Alternative names | Bimatoprost SR; bimatoprost sustained-release implant; Durysta™ |
|---|---|
| Class | Amides; antiglaucomas; lipids; prostaglandins; small molecules |
| Mechanism of action | Prostaglandin F2α receptor agonist |
| Route of administration | Implantation |
| Pharmacodynamics | Acts to lower intraocular pressure by increasing outflow of aqueous humour through both the trabecular meshwork (conventional) and uveoscleral routes (unconventional) |
| Pharmacokinetics | Following administration of bimatoprost implant, the highest concentrations of bimatoprost plus the metabolite bimatoprost acid are found in the iris–ciliary body (based on a study in dogs); minimal systemic exposure |
| Most common adverse reactions | Conjunctival hyperaemia, foreign body sensation, eye pain, photophobia, conjunctival haemorrhage, dry eye, eye irritation, intraocular pressure increased, corneal endothelial cell loss, vision blurred, iritis, headache |
| ATC codes: | |
| WHO ATC code | S01E-E03 (Bimatoprost) |
| EphMRA ATC code | S1E (Miotics and Antiglaucoma Preparations) |
| Chemical name | (Z)-7-[(1R,2R,3R,5S)-3,5-dihydroxy-2-[(1E,3S)-3-hydroxy-5-phenyl-1-pentenyl]cyclopentyl]-N-ethyl-5-heptenamide |
Pharmacodynamics
Bimatoprost is a synthetic structural analogue of prostaglandin with IOP-lowering activity [9]. The IOP-lowering effect acts to reduce the risk of progressive optic nerve damage and visual field loss that occurs in OAG. In humans, it is believed that bimatoprost acts to lower IOP by increasing outflow of aqueous humour through both the trabecular meshwork (conventional) and uveoscleral routes (unconventional) [9]. In a study in normotensive dogs, intracameral bimatoprost implant was associated with a transient increase in episcleral venous pressure (peaking at day 8) followed by a sustained decrease (mean change from baseline of − 2.4 to − 3.9 mm Hg over days 29–65) [15]. Furthermore, bimatoprost implant treatment was associated with a sustained dilation of aqueous outflow vessels [15]. In further studies in normotensive dogs, intracameral bimatoprost implant was found to have a dose-dependent IOP-lowering effect that was maintained for ≥ 3 months post administration [16, 17]. Interestingly, a study in normotensive monkeys found that intracameral bimatoprost implant had an IOP-lowering effect that was additive to that achieved with topical bimatoprost, suggesting that the intracameral implant may have an additional mechanism of action [18].
Pharmacokinetics
In a study in dogs, peak study drug concentrations in ocular tissues were observed around day 51 after administration of bimatoprost implant 15 μg [14]. At this time, 80.5% of the bimatoprost load had been released. By day 80, at which point > 99% of the bimatoprost load had been released, ocular tissue drug concentrations had declined significantly [14].
Compared with topical bimatoprost, intracameral bimatoprost implant enhances delivery of the study drug to target tissues [14]. Following a single administration of bimatoprost implant 15 μg in dogs, highest concentrations of bimatoprost plus the metabolite bimatoprost acid were detected in the iris–ciliary body, the key site of pharmacologic action; drug concentrations in the eyelid margins, periorbital fat and the area centralis of the retina were below the limit of detection. In contrast, following administration of topical bimatoprost 0.03% once daily for 7 days, highest bimatoprost plus bimatoprost acid concentrations were detected in the upper eyelid margin, the lower eyelid margin and the bulbar conjunctiva [14].
Based on clinical data, there is minimal systemic exposure of bimatoprost following a single administration of bimatoprost implant, with the concentrations of bimatoprost and bimatoprost acid below the limits of quantification (0.001 ng/mL and 0.01 ng/mL, respectively) in ~ 92% and ~ 99% of patients [9]. The highest bimatoprost concentration detected in any patient was 0.00224 ng/mL [9].
Key clinical trials of bimatoprost implant (Allergan)
| Identifier | Indication | Phase | Drugs/procedures | Location(s) | Status |
|---|---|---|---|---|---|
|
ARTEMIS-1; |
OAG or OHT | III | Bimatoprost implant; sham implant; timolol; timolol vehicle (placebo) | Multinational | Completed |
|
ARTEMIS-2; |
OAG or OHT | III | Bimatoprost implant; sham implant; timolol; timolol vehicle (placebo) | Multinational | Ongoing |
| NCT02636946 | OAG or OHT | III | Bimatoprost implant; sham implant; SLT; sham SLT | Multinational | Ongoing |
| NCT02507687 | OAG or OHT | III | Bimatoprost implant; sham implant; SLT; sham SLT | Multinational | Ongoing |
| NCT03850782 | OAG or OHT | III | Bimatoprost implant | Multinational | Recruiting |
| NCT03891446 | OAG or OHT | III | Bimatoprost implant | Multinational | Recruiting |
| NCT04285580 | OAG or OHT | III | Bimatoprost implant; bimatoprost ophthalmic solution | USA | Planned |
| APOLLO; NCT01157364 | OAG | I/II | Bimatoprost implant; bimatoprost ophthalmic solution | Multinational | Completed |
OAG open-angle glaucoma, OHT ocular hypertension, SLT selective laser trabeculoplasty
Therapeutic Trials
Phase III Trials
Bimatoprost implant reduces IOP with a sustained effect in patients with OAG or OHT based on available data from two randomized, masked, parallel-group, multinational, phase III clinical trials of identical design (ARTEMIS-1 and -2) [19–21].
In each of the trials, patients (n = 594 and 528) were randomized to receive study eye treatment with bimatoprost implant 10 or 15 μg intracamerally on day 1, week 16 and week 32 or topical timolol 0.5% twice daily [19–21]. Previous IOP-reducing medications were washed out before baseline. The trials each involved a 12-month treatment period with an 8-month extended follow-up. Rescue treatment with topical medication was permitted if the investigator judged that IOP was inadequately controlled [19–21].
Based on pooled data from the two trials, both bimatoprost implant dose strengths were non-inferior to timolol in lowering IOP through week 12 (primary endpoint) [19]. Across the trials, mean reductions in IOP from the baseline of 24.5 mmHg in bimatoprost implant recipients were ~ 7–8 mmHg at weeks 2 and 6 and ~ 6–7 mmHg at week 12 [9]. From pooled data, responder rates for the achievement of at least 20%, 25%, 30%, 35% and 40% reduction in IOP from baseline at weeks 2, 6 and 12 were numerically higher in bimatoprost recipients compared with timolol recipients [20]. Currently available data from the trials over a longer timeframe (with data cut-off after the last enrolled patient had completed the week 52 and week 12 visits in ARTEMIS-1 and -2, respectively) show that bimatoprost implant has a durable effect, evidenced by an 82% and 86% probability of bimatoprost implant 10 and 15 μg recipients (pooled across trials) not having added IOP-lowering medication at 360 days after the third bimatoprost implant [21]. Interim 1-year pooled data from the trials also indicate that eyes that had received three bimatoprost implant administrations had less visual field loss than topical timolol-treated eyes [22].
Phase I/II Trial
Further data supporting the efficacy of bimatoprost implant in reducing IOP with a sustained duration of effect are available from a prospective, 24-month, dose-ranging, paired-eye controlled, multinational, phase I/II clinical trial (APOLLO) in 75 adult patients with OAG [23, 24]. Following washout, patients were randomized to receive bimatoprost implant 6, 10, 15 or 20 μg intracamerally in the study eye; the fellow eye was treated with topical bimatoprost 0.03% once daily. Rescue treatment with topical IOP-lowering medication or a single repeat administration with bimatoprost implant was permitted at the investigator’s discretion (with censoring of data) [23, 24].
Bimatoprost implant at all dose strengths tested in the trial effectively reduced IOP with an effect that was broadly similar to the reduction achieved with topical bimatoprost [23, 24]. Mean IOP reduction from baseline (24.5–26.6 mm Hg across groups) in study eyes (primary endpoint) in the bimatoprost implant 6, 10, 15 and 20 μg dose groups, respectively, was 7.2, 7.4, 8.1 and 9.5 mm Hg through week 16 and 7.5, 7.3, 7.3, and 8.9 mm Hg at month 24 compared with mean reductions from baseline (24.1–25.5 mm Hg across groups) in topical bimatoprost-treated pooled fellow eyes of 8.4 mm Hg at week 16 and 8.2 mm Hg at month 24 [23, 24]. Consistent with findings in the phase III trials, there was evidence that bimatoprost implant had a durable effect, with no use of rescue medication/retreatment in 68%, 40% and 28% of pooled study eyes at months 6, 12 and 24, respectively [23]. Additionally, patient-reported outcomes showed that bimatoprost implant was well received, with 82.9% of patients at month 24 reporting that they would be very or extremely likely to have another implant procedure if given the choice, and 88.6% reporting that they would recommend the procedure to someone else with the same eye condition [23].
Adverse Events
In clinical trials in patients with OAG or OHT, the intracameral bimatoprost implant had acceptable safety and tolerability [9, 19, 20, 23, 24]. The most common adverse reactions in bimatoprost implant recipients in the ARTEMIS-1 and -2 trials were conjunctival hyperaemia (reported in 27% of patients), foreign body sensation, eye pain, photophobia, conjunctival haemorrhage, dry eye, eye irritation, intraocular pressure increased, corneal endothelial cell loss, vision blurred, and iritis (all in 5–10% of patients) [9]. Ocular adverse events observed in clinical trials most typically occurred within 2 days after the implantation procedure and were transient [24]. The most common non-ocular adverse reaction in bimatoprost implant recipients in the phase III trials was headache (reported in 5% of patients) [9].
The US prescribing information provides further information on warnings and precautions related to the use of bimatoprost implant, including regarding risks of corneal adverse reactions (including corneal endothelial cell loss), macular oedema (including cystoid macular oedema), intraocular inflammation, pigmentation changes (e.g. of the iris) and endophthalmitis [9]. Bimatoprost implant should be used with caution in patients with narrow iridocorneal angles or anatomical obstruction that may prohibit settling in the inferior angle. Due to the risk of implant migration into the posterior segment, bimatoprost implant is contraindicated in patients whose posterior lens capsule is absent or ruptured. Bimatoprost implant is also contraindicated in patients with active or suspected ocular or periocular infections; with corneal endothelial cell dystrophy; and with prior corneal transplantation, or endothelial cell transplants [9].
Ongoing or Planned Clinical Trials
Five further phase III trials in patients with OAG or OHT are ongoing or planned as part of Allergan’s clinical development programme for bimatoprost implant:
NCT02636946 and NCT02507687 – these randomized, masked, parallel assignment trials are evaluating the IOP-lowering effect and safety of bimatoprost implant compared with selective laser trabeculoplasty in patients who are not adequately managed with topical IOP-lowering medication.
NCT03850782 – this randomized, masked, parallel assignment trial is evaluating the duration of IOP-lowering effect and safety of as needed administrations of bimatoprost implant in patients who are not adequately managed with topical IOP-lowering medication for reasons other than medication efficacy.
NCT03891446 – this non-randomized, open-label, parallel assignment extension trial will evaluate the long-term safety and efficacy of bimatoprost implant in patients who completed one of ARTEMIS-1 (NCT02247804), ARTEMIS-2 (NCT02250651), NCT02636946 or NCT02507687 trials and received bimatoprost implant.
NCT04285580 – this non-randomized, open-label, parallel assignment trial will evaluate the 24-h IOP-lowering effect and safety after a single administration of bimatoprost implant.
Current Status
Bimatoprost implant received its first approval on 04 March 2020, in the USA, for use to reduce IOP in patients with open angle glaucoma or ocular hypertension [8, 9].
Compliance with Ethical Standards
Funding
The preparation of this review was not supported by any external funding.
Conflicts of Interest
During the peer review process the manufacturer of the agent under review was offered an opportunity to comment on the article. Changes resulting from any comments received were made by the authors on the basis of scientific completeness and accuracy. Matt Shirley is a salaried employee of Adis International Ltd/Springer Nature, is responsible for the article content and declares no relevant conflicts of interest.
Footnotes
This article note shall be added: “The original version of this article was revised due to a retrospective Open Access order”.
Enhanced material
for this AdisInsight Report can be found at: 10.6084/m9.figshare.12269417
This profile has been extracted and modified from the AdisInsight database. AdisInsight tracks drug development worldwide through the entire development process, from discovery, through pre-clinical and clinical studies to market launch and beyond.
Change history
6/19/2020
The article Bimatoprost Implant: First Approval, written by Matt Shirley, was originally published Online First without Open Access. After publication in volume 37, issue 6, pages 457���462 Allergan, an Abbvie company requested that the article be Open Choice to make the article an open access publication. Post-publication open access was funded by Allergan, an Abbvie company. This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit.
References
- 1.Weinreb RN, Leung CK, Crowston JG, et al. Primary open-angle glaucoma. Nat Rev Dis Primers. 2016;2:16067. doi: 10.1038/nrdp.2016.67. [DOI] [PubMed] [Google Scholar]
- 2.Prum BE, Jr, Rosenberg LF, Gedde SJ, et al. Primary open-angle glaucoma Preferred Practice Pattern® guidelines. Ophthalmology. 2016;123(1):P41–111. doi: 10.1016/j.ophtha.2015.10.053. [DOI] [PubMed] [Google Scholar]
- 3.Friedman DS, Quigley HA, Gelb L, et al. Using pharmacy claims data to study adherence to glaucoma medications: methodology and findings of the Glaucoma Adherence and Persistency Study (GAPS) Invest Ophthalmol Vis Sci. 2007;48(11):5052–5057. doi: 10.1167/iovs.07-0290. [DOI] [PubMed] [Google Scholar]
- 4.Mansouri K, Iliev ME, Rohrer K, et al. Compliance and knowledge about glaucoma in patients at tertiary glaucoma units. Int Ophthalmol. 2011;31(5):369–376. doi: 10.1007/s10792-011-9468-2. [DOI] [PubMed] [Google Scholar]
- 5.Newman-Casey PA, Robin AL, Blachley T, et al. The most common barriers to glaucoma medication adherence: a cross-sectional survey. Ophthalmology. 2015;122(7):1308–1316. doi: 10.1016/j.ophtha.2015.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reardon G, Kotak S, Schwartz GF. Objective assessment of compliance and persistence among patients treated for glaucoma and ocular hypertension: a systematic review. Patient Prefer Adherence. 2011;5:441–463. doi: 10.2147/PPA.S23780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh RB, Ichhpujani P, Thakur S, et al. Promising therapeutic drug delivery systems for glaucoma: a comprehensive review. Ther Adv Ophthalmol. 2020;12:2515841420905740. doi: 10.1177/2515841420905740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.US FDA. Durysta (bimatoprost implant)—NDA approval. 2020. https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2020/211911Orig1s000ltr.pdf. Accessed 20 Apr 2020.
- 9.Allergen. DurystaTM (bimatoprost implant), for intracameral administration: US prescribing information. 2020. https://media.allergan.com/products/durysta_pi.pdf. Accessed 20 Apr 2020.
- 10.Allergan. U.S. FDA accepts Allergan's New Drug Application for bimatoprost sustained-release in patients with open-angle glaucoma or ocular hypertension [media release]. 2019. https://www.allergan.com/News/Details/2019/07/US%20FDA%20Accepts%20Allergans%20New%20Drug%20Application%20for%20Bimatoprost%20SustainedRelease%20in%20Patients%20with%20Open. Accessed 20 Apr 2020.
- 11.Allergan. Actavis completes Allergan acquisition [media release]. 2015. https://www.allergan.com/News/Details/2015/03/Actavis%20Completes%20Allergan%20Acquisition. Accessed 20 Apr 2020.
- 12.Allergan. Actavis plc is now Allergan plc [media release]. 2015. https://www.allergan.com/News/Details/2015/06/Actavis%20plc%20is%20now%20Allergan%20plc. Accessed 20 Apr 2020.
- 13.AbbVie. AbbVie completes transformative acquisition of Allergan [media release]. 2020. http://news.abbvie.com/news/press-releases/abbvie-completes-transformative-acquisition-allergan.htm. Accessed 27 May 2020.
- 14.Seal JR, Robinson MR, Burke J, et al. Intracameral sustained-release bimatoprost implant delivers bimatoprost to target tissues with reduced drug exposure to off-target tissues. J Ocul Pharmacol Ther. 2019;35(1):50–57. doi: 10.1089/jop.2018.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee SS, Burke J, Shen J, et al. Bimatoprost sustained-release intracameral implant reduces episcleral venous pressure in dogs. Vet Ophthalmol. 2018;21(4):376–381. doi: 10.1111/vop.12522. [DOI] [PubMed] [Google Scholar]
- 16.Lee SS, Dibas M, Almazan A, et al. Dose-response of intracameral bimatoprost sustained-release implant and topical bimatoprost in lowering intraocular pressure. J Ocul Pharmacol Ther. 2019;35(3):138–144. doi: 10.1089/jop.2018.0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shen J, Robinson MR, Struble C, et al. Nonclinical pharmacokinetic and pharmacodynamic assessment of bimatoprost following a single intracameral injection of sustained-release implants. Transl Vis Sci Technol. 2020;9(4):1–11. doi: 10.1167/tvst.9.4.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee SS, Almazan A, Decker S, et al. Intraocular pressure effects and mechanism of action of topical versus sustained-release bimatoprost. Transl Vis Sci Technol. 2019;8(1):15. doi: 10.1167/tvst.8.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Craven ER, Walters T, Christie WC, et al. Phase 3 evaluation of bimatoprost sustained-release implant in patients with glaucoma or ocular hypertension: results at primary database lock [Abstract No. PA054]. In: American Academy of Ophthalmology Annual Meeting, San Francisco, CA, 1–15 October 2019.
- 20.Walters T, Christie WC, Bejanian M, et al. Bimatoprost sustained-release implant (bimatoprost SR) responder rates in patients with glaucoma or ocular hypertension: phase 3 study results at primary database lock [Abstract No. PO101]. In: American Glaucoma Society Annual Meeting, Washington, DC, 27 February–1 March 2020.
- 21.Myers JS, Bejanian M, Chen M, et al. Profile of IOP response to bimatoprost sustained-release implant (bimatoprost SR) before added treatment with topical medication: phase 3 study results [Abstract No. PO090]. In: American Glaucoma Society Annual Meeting, Washington, DC, 27 February–1 March 2020.
- 22.Medeiros F, Bejanian M, Goodkin ML, et al. Visual field outcomes in open-angle glaucoma patients treated with bimatoprost SR in phase 3 evaluation: results at primary database lock [Abstract No. PA17]. In: American Glaucoma Society Annual Meeting, Washington, DC, 27 February–1 March 2020.
- 23.Craven ER, Walters T, Christie WC, et al. 24-month phase I/II clinical trial of bimatoprost sustained-release implant (bimatoprost SR) in glaucoma patients. Drugs. 2020;80(2):167–179. doi: 10.1007/s40265-019-01248-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lewis RA, Christie WC, Day DG, et al. Bimatoprost sustained-release implants for glaucoma therapy: 6-month results from a phase I/II clinical trial. Am J Ophthalmol. 2017;175:137–147. doi: 10.1016/j.ajo.2016.11.020. [DOI] [PubMed] [Google Scholar]


