Graphical abstract
Keywords: Sarcoidosis, Mediastinal lipomatosis, Cardiac tumor, Steroid therapy, Polyserositis
Highlights
-
•
Sarcoidosis can present with persistent and recurrent polyserositis.
-
•
Steroid therapy is associated with benign ML.
-
•
Advanced imaging can help characterize concerning lesions seen on echocardiography.
Introduction
Symptomatic polyserositis is an extremely unusual presentation of sarcoidosis.1, 2, 3, 4, 5 Benign mediastinal lipomatosis (ML) is an uncommon complication of treatment with steroid therapy.6, 7, 8, 9 Here we describe the simultaneous occurrence of these two rare conditions and the imaging modalities that facilitated diagnosis in the case of a 49-year-old man presenting with acute chest pain.
Case Presentation
A previously healthy 49-year-old man presented to the hospital with pleuritic chest pain for 1 week. Initial transthoracic echocardiography was notable only for small pericardial effusion. He was started on ibuprofen and colchicine for presumed pericarditis. One week later he was readmitted for increasing chest pain and was found to have worsening pericardial effusion and new bilateral pleural effusions. Inflammatory markers including C-reactive protein and ferritin were significantly elevated, and he was initiated on prednisone. Diagnostic thoracentesis revealed exudative effusion, but infectious, rheumatologic, and malignant workup was unrevealing. He clinically improved on steroid therapy and was discharged on a taper with close outpatient follow-up.
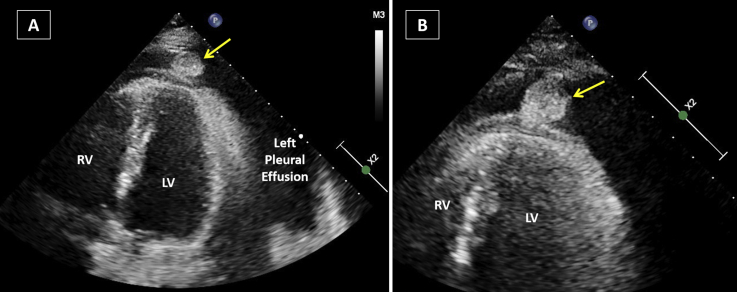
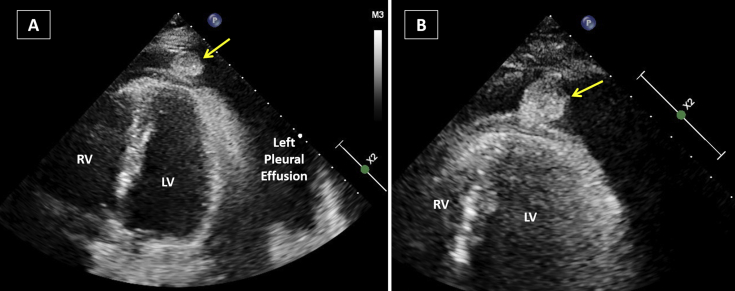
Over the next few days, the patient's C-reactive protein level decreased, and repeat transthoracic echocardiography demonstrated near resolution of the pericardial effusion. However, after his prednisone dose was reduced from 30 to 20 mg/d, he developed dizziness, generalized malaise, fever, and rising C-reactive protein level. Upon readmission to the hospital, contrast-enhanced computed tomography of the chest demonstrated stable pericardial effusion, bilateral pleural effusions, and atelectasis of the left lower lobe (Figure 1). Multiple small mediastinal lymph nodes were also visualized. Repeat diagnostic thoracentesis was performed for diagnostic clarification and again revealed exudative effusion with negative infectious, rheumatologic, and malignant workup.
Figure 1.
Chest computed tomography demonstrating pleural and pericardial effusions in axial (A) and sagittal (B) cuts.
A working diagnosis of polyserositis of unclear etiology was established; the leading differential diagnoses at the time included sarcoidosis and atypical presentation of adult-onset Still's disease. The patient underwent pleuroscopy with biopsy for definitive diagnosis, and histopathology showed noncaseating granulomas consistent with sarcoidosis. Clinically, he continued to improve on prednisone, ibuprofen, and colchicine.
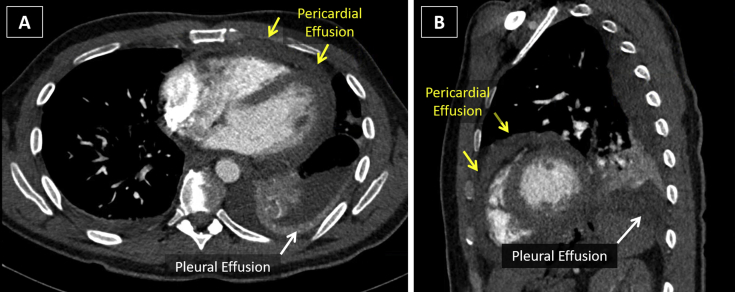
Unexpectedly, repeat transthoracic echocardiography performed approximately 1 week later demonstrated a new, round, mobile mass measuring 1.5 cm in diameter in the pleural space (Figure 2, Video 1) that appeared to be attached to the parietal pericardium near the apex of the left ventricle, suggestive of a possible tumor and malignant etiology of his recurring pleural and pericardial effusions (Video 2).
Figure 2.
Transthoracic echocardiographic images demonstrating ML masquerading as a pericardial pseudo-tumor (arrow) in unzoomed (A) and zoomed (B) apical four-chamber view. Video 1 corresponds to (A). Video 2 demonstrates large left pleural and small pericardial effusions in the parasternal long-axis view on transthoracic echocardiography.
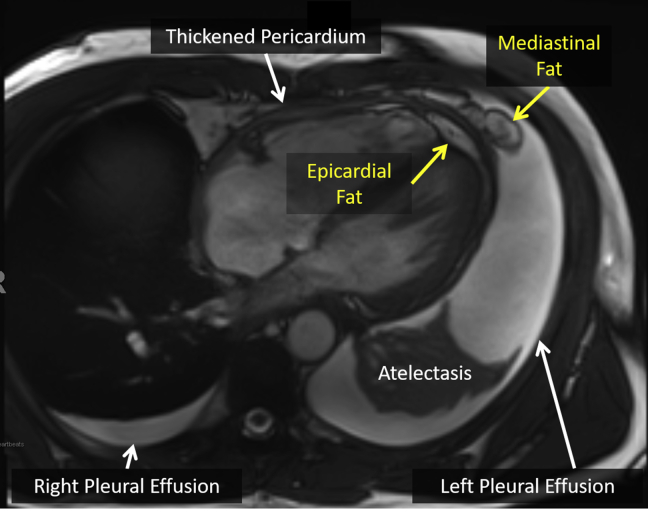
Cardiac magnetic resonance imaging (MRI) was performed to further characterize the mass. High signal intensity was demonstrated on T1-weighted images. When fat saturation was used, the mass was determined to be composed of fatty tissue and not concerning for a cardiac tumor (Figures 3 and 4, Video 3).
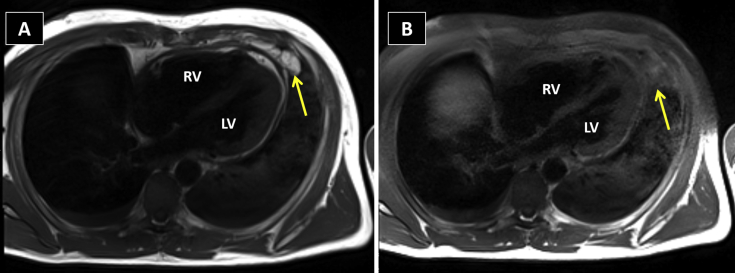
Figure 3.
Cardiac MRI with four-chamber steady-state free precession image showing a thickened pericardium, pleural effusion, prominent epicardial fat at the left and right ventricular apices and lobulated masslike structure outside of the pericardium that is mobile on cine imaging.
Figure 4.
(A) T1-weighted four-chamber magnetic resonance image showing high signal intensity in the extrapericardial mass (arrow), consistent with likely fat tissue. Video 3 corresponds to this panel. (B) Similar T1 image with addition of fat suppression (e.g., “fat saturation”) technique showing signal suppression of the mass (arrow), confirming the fat tissue composition of the mass.
Taken together, the patient's clinical and imaging findings were consistent with steroid-associated ML with an unusual presentation of a tumorlike mass in the extrapericardial space in the setting of treatment for sarcoidosis-induced polyserositis.
He continued to improve clinically, and his steroid dose was gradually tapered over several months. No procedural intervention of the mass was required.
Discussion
In this case report we present two unique findings: (1) sarcoidosis-induced polyserositis and (2) steroid-associated ML.
Sarcoidosis is a granulomatous disease that typically presents with pulmonary involvement. Polyserositis is an extremely rare presentation of this disease. Prevalence of pleural effusions in sarcoidosis is estimated to be between 1% and 2%, and only 0.6% of patients with sarcoidosis presented with pericardial effusion in one retrospective study.1 Ours may be only the fifth documented case of sarcoidosis presenting with simultaneous pericardial and pleural involvement in the English-language literature.2, 3, 4, 5
While receiving steroid therapy, our patient was also found to have an unusual presentation of ML. ML is the benign deposition of excess adipose tissue within the mediastinum. ML can be idiopathic or associated with steroid use, obesity, or Cushing's syndrome.10 Steroid use has been associated with increased pericardial and epicardial fat in a dose-dependent fashion.11 Adipocytes can also infiltrate the interatrial septum to cause lipomatous atrial septal hypertrophy.12 Radiographically, ML can present as a mimic of widened mediastinum, pleural effusion, pericardial effusion, or cardiac mass.6, 7, 8, 9,13
The duration of steroid therapy necessary to produce clinically significant fat deposition is unclear, as the vast majority of cases of steroid-associated ML are reported in patients who have been on chronic steroid therapy for months to years.6, 7, 8, 9 In this case, new epicardial lipomatosis was discovered on imaging merely 3 weeks after the patient was initiated on steroid therapy.
In suspected pericardial disease, echocardiography is the initial diagnostic test of choice; however, its utility is limited by the acoustic characterization of tissue.14 As demonstrated in this case, advanced imaging modalities can offer superior tissue characterization for potentially concerning lesions. Because of the short relaxation time of its protons and resulting high signal intensity, fat can be more easily identified on MRI than computed tomography.15 Fat signal on MRI can also be suppressed because of the differing resonance frequencies between fat and water.15 These fat suppression techniques further aid in correct identification of fatty tissue on MRI and also facilitate the identification of contrast-enhancing tumors that may otherwise be obscured by fat signal. The treatment of a benign lipomatous cardiac mass in a patient with an appropriate history is typically weight loss or steroid taper; surgical intervention is uncommon.6,13 Thus, the use of echocardiography and other advanced imaging modalities as necessary to achieve the correct diagnosis of a cardiac mass is clinically significant and may prevent further unnecessary and invasive procedures.
Conclusion
We describe recurrent polyserositis as a rare presentation of sarcoidosis, as well as steroid-associated benign ML presenting with a cardiac mass. The mass was initially diagnosed on echocardiography, then further characterized on cardiac MRI. Clinicians should consider the diagnosis of sarcoidosis in cases of persistent polyserositis and be mindful of benign ML as a potential consequence of steroid therapy. Advanced imaging techniques should be pursued before invasive procedures to further characterize potentially concerning lesions.
Footnotes
Conflicts of interest: The authors reported no actual or potential conflicts of interest relative to this document.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.case.2020.01.005.
Supplementary Data
Transthoracic echocardiographic clip demonstrating ML masquerading as a pericardial pseudo-tumor (arrow) in the apical four-chamber view.
Transthoracic echocardiographic clip demonstrating large left pleural and small pericardial effusions in the parasternal long-axis view.
Cardiac MRI with four-chamber steady-state free precession image showing a thickened pericardium, pleural effusion, prominent epicardial fat at the left and right ventricular apices, and lobulated masslike structure outside of the pericardium that is mobile on cine imaging.
References
- 1.Sharma S.K., Soneja M., Sharma A., Sharma M.C., Hari S. Rare manifestations of sarcoidosis in modern era of new diagnostic tools. Indian J Med Res. 2012;135:621–629. [PMC free article] [PubMed] [Google Scholar]
- 2.Krawczyk I., Sedlaczek A.M. A case of sarcoidosis with massive pleural and pericardial effusion. Pneumonol Alergol Pol. 1997;65:81–85. [PubMed] [Google Scholar]
- 3.Navaneethan S.D., Venkatesh S., Shrivastava R., Mehta J., Israel R. Recurrent pleural and pericardial effusions due to sarcoidosis. PLoS Med. 2005;2:e63. doi: 10.1371/journal.pmed.0020063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Currie G.P., Kerr K., Buchan K., Garg D. A rare cause of recurrent massive pericardial and pleural effusions. QJM. 2008;101:989–990. doi: 10.1093/qjmed/hcn116. [DOI] [PubMed] [Google Scholar]
- 5.Jenkins D.N., Beean K.V., Malik M.S. “Idiopathic” effusions get a proper name. Respiration. 2016;92:114–117. doi: 10.1159/000448378. [DOI] [PubMed] [Google Scholar]
- 6.Fonseka N., Ruel E. A benign cause of widened mediastinum: a case of mediastinal lipomatosis. Med Forum. 2013;14:15–16. [Google Scholar]
- 7.Kaur N., Singh J., Haq S., Garg S., Bhatnagar S. Pleural and mediastinal lipomatosis with subpleural fat as a mimicker of pleural effusion—a rare case report. J Clin Diagn Res. 2017;11:TD03–TD04. doi: 10.7860/JCDR/2017/26182.10156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsu Y.M., Yao N.S., Liu J.M. Steroid-induced mediastinal lipomatosis with radiographic features of pericardial effusion. Am J Emerg Med. 2000;18:346–348. doi: 10.1016/s0735-6757(00)90140-2. [DOI] [PubMed] [Google Scholar]
- 9.Van de Putte L.B.A., Wagenaar J.P.M., Kwa H.S. Paracardiac lipomatosis in exogenous Cushing's syndrome. Thorax. 1973;28:653–656. doi: 10.1136/thx.28.5.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mohapatra P.R., Janmeja A.K. Asymptomatic mediastinal lipomatosis. N Engl J Med. 2010;363:1265. doi: 10.1056/NEJMicm1000714. [DOI] [PubMed] [Google Scholar]
- 11.Kitterer D., Latus J., Henes J., Birkmeier S., Backes M., Braun N. Impact of long-term steroid therapy on epicardial and pericardial fat deposition: a cardiac MRI study. Cardiovasc Diabetol. 2015;14:130. doi: 10.1186/s12933-015-0289-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saric M., Applebaum R.M., Culliford A.T., Huang J., Scholes J.V., Kronzon I. Massive atrial septal lipomatous hypertrophy. Echocardiography. 1999;16:833–834. doi: 10.1111/j.1540-8175.1999.tb00137.x. [DOI] [PubMed] [Google Scholar]
- 13.Gajjar T., Rao N., Desai N. A giant benign epicardial lipomatosis of the left ventricle. Cardiovasc Surg Int. 2016;3:84–87. [Google Scholar]
- 14.Klein A.L., Abbara S., Agler D.A., Appleton C.P., Asher C.R., Hoit B. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr. 2013;26:965–1012.e15. doi: 10.1016/j.echo.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 15.De Kerviler E., Leroy-Willig A., Clement O., Frija J. Fat suppression techniques in MRI: an update. Biomed Pharmacother. 1998;52:69–75. doi: 10.1016/S0753-3322(98)80006-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transthoracic echocardiographic clip demonstrating ML masquerading as a pericardial pseudo-tumor (arrow) in the apical four-chamber view.
Transthoracic echocardiographic clip demonstrating large left pleural and small pericardial effusions in the parasternal long-axis view.
Cardiac MRI with four-chamber steady-state free precession image showing a thickened pericardium, pleural effusion, prominent epicardial fat at the left and right ventricular apices, and lobulated masslike structure outside of the pericardium that is mobile on cine imaging.