Abstract
Purpose: Off-pump coronary arterial bypass grafting (OPCAB) has become a common practice for coronary artery bypass grafting (CABG) in Japan, with approximately 65% CABG procedures currently being performed using OPCAB. However, it is unclear whether OPCAB is superior in terms of associated mortality, incidence of complications, graft patency rate, and long-term outcomes compared with conventional CABG (CCABG).
Methods: Literature consideration was performed, mainly based on observational studies involving large samples and randomized controlled trials (RCTs).
Results: Many RCTs indicated that the acute-phase and long-term mortality rates were comparable between CCABG and OPCAB or that OPCAB was inferior to CCABG. In contrast, many observational studies indicated that OPCAB was superior to CCABG.
Conclusion: CABG is a delicate procedure, the outcomes of which vary in accordance with the patient’s condition as well as the level of expertise of the associated institution and surgeon. In the future, we hope that reports will emerge with excellent results, including long-term results, from Japanese institutions experienced in performing OPCAB.
Keywords: coronary artery bypass grafting, off-pump coronary artery bypass, OPCAB
Introduction
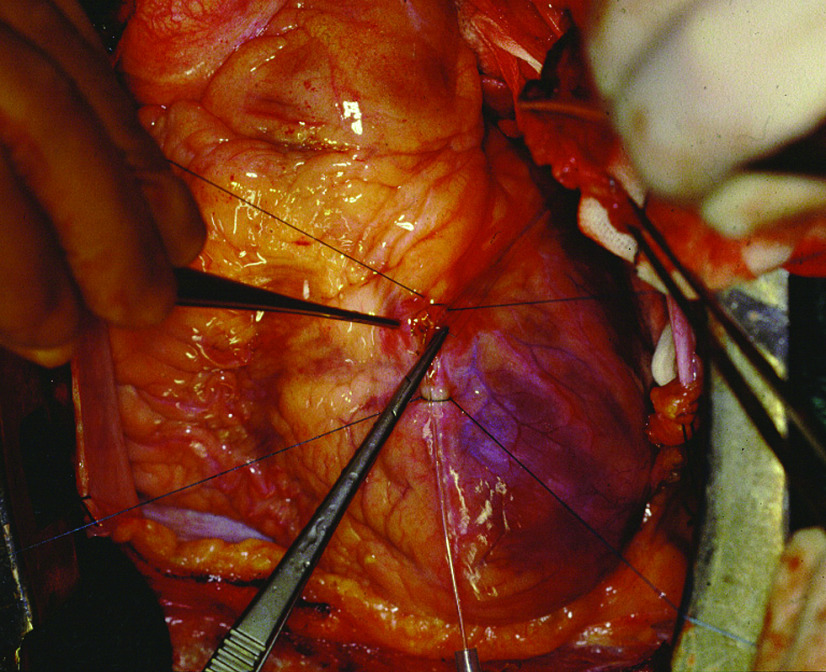
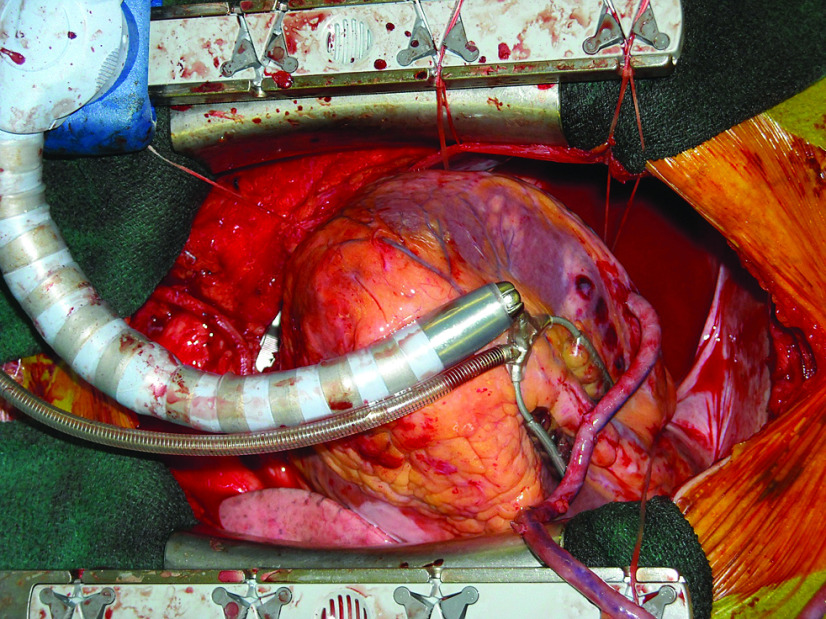
Coronary artery bypass grafting (CABG) was first performed in the 1960s as the sole method of treatment for ischemic heart disease. The first CABG, performed by Goetz in 1960,1,2) was an off-pump CABG (OPCAB) that did not use cardiopulmonary bypass (CPB). OPCAB was chosen because CPB, which was initially used for human in 1953, was inadequate. Thereafter, with advances in CPB, conventional CABG (CCABG) performed with CPB and cardiac arrest became the gold standard. Soon after, OPCAB was not used until reports from Benetti3) and Buffolo et al.4) in 1985 brought it back into the spotlight. Because CPB is not used, OPCAB is minimally invasive and thus, it is expected to reduce the incidence of complications, mortality rate, and medical costs involved. Subsequently, OPCAB gained worldwide attention, and clinical trials commenced. In Japan, OPCAB was performed first on series of patients (Fig. 1), as reported by Tashiro et al.,5,6) and following the advent of the stabilizer (Fig. 2) in 2000, OPCAB has become a common practice for CABG in Japan, with approximately 65% CABG procedures currently being performed using OPCAB. This rate is extremely high in contrast to the rate of OPCAB performed in Western countries (approximately 15%). Thus, we can say that Japan is major country of OPCAB.
Fig. 1. Before 2000, revascularization with OPCAB was performed to anterior coronary artery. At that time, the auxiliary support only a sponge placed on the back of the heart and two strings that blocked and fixed the target coronary artery.
Fig. 2. From 2000, revascularization with OPCAB was performed to all coronary arteries, including the posterior coronary artery. This shift in approach was due to the introduction of stabilizers and deep pericardial suture techniques.
Advances in CPB have clearly improved cardiac surgery; however, regardless of the constant progress, the non-physiological impact of CPB causes tissue damage and organ dysfunction.7) In particular, cerebrovascular accidents arising in association with CPB are a major problem.8,9) However, it is unclear whether OPCAB is superior in terms of associated mortality, incidence of complications, graft patency rate, and long-term outcomes compared with CCABG.
The popularization of OPCAB has given rise to several questions:
(1) Does OPCAB really reduce hospital morbidity and mortality in CABG?
(2) What is the patency and quality of grafts in OPCAB compared with that in CABG using CPB?
(3) Is OPCAB reproducible in average surgeon?
Because multiple studies have been performed to address these questions, the available evidence should be evaluated by cardiac surgeons to examine how OPCAB should be performed in clinical practice.
Hospital Morbidity and Mortality
Initial studies were retrospective analyses, particularly those involving large databases, and small observational studies. These studies indicated that OPCAB reduces hospital morbidity and mortality in CABG.10-12) Furthermore, mortality and morbidity rates were found to be similar to those associated with CCABG.13) Thereafter, observational studies involving a large subject sample and randomized controlled trials (RCT) initially including a small subject sample and low-risk patients were commenced. Gerola et al.14) compared the results of OPCAB and CCABG in low-risk patients and found that although the in-hospital mortality rate was lower for OPCAB than for CCABG, it was not significantly different. They mentioned reason why there is no significant difference between OPCAB and CCABG in-hospital mortality are their study did not involve patients with three vessel disease and the operation lasted a short cardiopulmonary bypass time, in the mean time of 50 minutes. They also reported no significant difference regarding the incidence of postoperative complications.
The first RCT, the Randomized On/Off Bypass (ROOBY) trial,15) compared 2023 patients who were randomly assigned to undergo OPCAB or CCABG. No significant difference was observed between the two groups in terms of in-hospital mortality, and the results revealed inferior postoperative graft patency with OPCAB. However, practitioners in the ROOBY trial included residents who were unfamiliar with OPCAB, which could have resulted in the high rate of CPB conversion and poor surgical outcomes; thus, there has been some criticism that the comparison was biased.16) It is argued that OPCAB is a delicate surgical procedure that requires considerable expertise and in this respect, it appears to have low reproducibility.
More than 4700 patients were enrolled in the multicenter, multinational study by the CABG Off or On-Pump Revascularization Study (CORONARY) group, for which a report was published in 2012.17) Outcomes of OPCAB and CCABG on postoperative day 30 were compared. This study showed that although the hospital mortality is similar between surgery with and without CPB, OPCAB significantly reduced the need for transfusion and reoperation for bleeding in addition to the incidence of acute renal failure and respiratory complications. In this RCT study, the 30-day hospital mortality in OPCAB and CCABG groups was similar. However, morbidity was lower in the OPCAB group.
Murzi et al.18) compared 548 patients who had undergone CCAB with 548 patients who had undergone OPCAB; the patients were matched using the propensity-score analysis of 2375 patients who had undergone isolated CABG. Compared with CCAB, OPCAB was associated with lower in-hospital mortality, incidence of stroke, postoperative renal dysfunction, pulmonary complications, and infectious complications.
Furthermore, in a meta-analysis of a large number of RCTs, Kowalewski et al.19) concluded the following: OPCAB is associated with a significant reduction in the odds of cerebral stroke compared with CCABG. In addition, benefits of OPCAB in terms of death, myocardial infarction, and cerebral stroke are significantly related to patient risk profile, suggesting that OPCAB should be strongly considered in high-risk patients.
A meta-analysis of 37 RCTs (n = 3449) and 22 risk-adjusted (logistic regression or propensity-score) observational studies (n = 293617) was performed by Wijeysundera et al.20) The study tabulated several RCTs and observational studies comparing OPCAB and CCABG, with excellent content. It was found that the difference between OPCAB and CCABG was negligible in RCTs, whereas OPCAB was found to be considerably superior in the observational studies. In RCTs, although no significant difference was found regarding mortality, OPCAB was found to be significantly superior to CCABG for a few items, including atrial fibrillation and blood transfusion. In contrast, for all items including mortality, stroke, myocardial infarction, and atrial fibrillation, OPCAB proved to be superior in observational studies. In terms of ethical considerations in RCTs because patients who provided consent for both methods were included, the subjects tended to be low-risk cases. On the other hand, in observational studies, there were many severe cases included, which is closer to an actual clinical situation and, therefore, gave superior results for OPCAB. Furthermore, Puskas et al.21) compared OPCAB and CCABG in STS database cases with high STS scores, and they found that in high STS score cases in-hospital morbidity and mortality was considerably lower for OPCAB.
Survival
Many RCTs have found that early mortality rate of OPCAB is comparable with that of CCABG. Thus, it would be interesting to determine whether long-term survival differs between OPCAB and CCABG.
Angelini et al.22) studied 401 patients from two separate RCT for a period of up to 6 and 8 years. There were no differences between the OPCAB and CCABG groups in terms of survival, survival free from major adverse cardiac events (MACEs, including myocardial infarction, angina recurrence, and need for revascularization), survival free from death or MACEs, graft patency, and quality of life. Similar results were reported by Hueb et al. in the MASS III trial.23) In the SMART trial, Puskas et al.24) observed patients for 5 years postoperatively to compare long-term outcomes, and they reported that survival was considerably better for OPCAB than for CCABG.
Studies of the ROOBY and CORONARY groups which are RCTs with large subject samples have also drawn attention.
Among the largest trials are the ROOBY15) trial, which included 2203 patients from the veterans affairs medical system, and the CORONARY trial,25) which included 4752 patients. They provided divergent results. In the ROOBY trial,15) the 30-day observation results were comparable, whereas the results of the 1-year observations revealed that survival and cardiac mortality rates of OPCAB were inferior to that of CCABG. However, the ROOBY trial included non-expert results, the trial was criticized because the reported 12.4% rate of intraoperative conversion from planned OPCAB to on-pump CABG was five times that reported in the national database of the Society of Thoracic Surgeons.16) In the CORONARY trial, at the 1-year observation, the mortality rate and incidence of myocardial infarction, angina, and repeat revascularization were comparable. Thus, it was concluded that long-term outcomes of OPCAB and CCABG were comparable. Furthermore, the 5-year long-term observation test from the CORONARY trial subsequently announced that results for OPCAB and CCABG were comparable.26) The results differed between the two trials, as the CABG experts performed the CORONARY trial, while the ROOBY trial included non-expert results. Moreover, this resulted in a major discrepancy in intraoperative conversion rates from planned OPCAB to CCABG of 7.9% and 12.4%, respectively. Because OPCAB is a surgical procedure that requires expert skill, benefits of the procedure begin to appear when it is performed by a surgeon with such skills.
In an observational study with a large subject sample, Dalen et al.27) compared 50676 patients who had undergone primary isolated non-emergent CABG in Sweden between 1998 and 2008 (3337 patients who had undergone OPCAB and 47339 patients who had undergone CCABG). The 10-year survival rate and incidence of re-hospitalization for myocardial infarction, heart failure, or stroke were similar between off-pump and on-pump CABG. Murzi et al.18) compared patients who had undergone isolated CABG (1297 patients who had undergone OPCAB and 1078 patients who had undergone CCAB) and found that the 1-, 5-, and 10-year survival rates were similar for OPCAB and CCABG groups. Kirmani et al.28) conducted follow-up observation for a median of 7.0 years for 8055 patients. They included 2082 patients by propensity matching, and upon comparing the CCABG and OPCAB groups, they reported that survival rates between the groups were comparable.
Quality of Surgery: Complete Revascularization and Graft Patency
Factors used to determine the quality of CABG include complete myocardial revascularization achieved at the necessary site as well as short- and long-term postoperative graft patency. Therefore, complete myocardial revascularization is an important factor for determining long-term outcomes.
Incomplete revascularization at coronary artery bypass grafting compromises patient outcomes. In 1981, Buda et al.29) reported a 5-year survival of 69% vs 84% in patients with incomplete revascularization vs in those with complete revascularization. Scott et al.30) reported that incomplete revascularization was an independent risk factor for late mortality with a 20-year survival of 42%–44% in patients with incomplete revascularization compared with that of 75% in those with complete revascularization. In recent studies, in elderly patients, incomplete revascularization does not affect long-term survival.31) This indicates that incomplete revascularization could be permitted for many elderly patients who undergo OPCAB.
OPCAB requires expert skill in revascularization of the coronary artery on the posterior surface of the heart. Therefore, at institutions with inexperienced surgeons, such revascularization can be inadequate, and OPCAB tends to be selected for patients who require revascularization only on the anterior surface of the heart. As a result, reports can be found indicating that in OPCAB, few coronary anastomoses are performed.18,22,28,33) With respect to postoperative graft patency, several reports indicate that patency is inferior in OPCAB; thus, compared with CCABG, OPCAB is associated with a higher rate of long-term events because of incomplete revascularization and graft occlusion.23,32,33,34) In recent years, reports have emerged indicating that at institutions with surgeons experienced in OPCAB, long-term outcomes for graft patency in OPCAB are comparable with those in CCABG.25,35-39) Thus, the quality of OPCAB can only be maintained when performed by an expert surgeon and at an experienced institution.
OPCAB in High-Risk Patients
The proportion of elderly people in Japan has increased considerably over recent decades, it is assumed that an increasing number of elderly patients will become a candidate for CABG. Most of these patients have significant comorbidities; thus, coronary revascularization is associated with an increased risk of death and overall postoperative morbidity, compromising the length of hospital stay and medical bills required. The past decade heralded improvements in surgical, anesthetic, and perfusion procedures. This progress led to CABG being regarded as a safe option for treatment of this high-risk group.40)
In a meta-analysis of patients aged ≥70 years,41) it was concluded that OPCAB may be associated with a lower incidence of death, stroke, and AF in elderly individuals, which may result in a shorter length of hospital stay. This meta-analysis has confirmed that the elderly benefit more from OPCAB surgery.
Two recent RCTs42,43) in which the effect of surgery with or without CPB was compared in patients aged >75 years showed no significant difference in-hospital mortality and survival at 6 months and 1 year.
For RCT involving high-risk patients in whom OPCAB was expected to be more effective, Lemma et al.44) included 411 patients with a EuroScore of >6 (195 patients who had undergone CCABG and 216 patients who had undergone OPCAB). Therefore, the rate of composite primary end point (operative mortality, myocardial infarction, stroke, renal failure, reoperation for bleeding, and adult respiratory distress syndrome within 30 days postoperatively) was significantly lower in the OPCAB group than in the CCABG group (5.8% vs 13.3%).
Møller et al.45) conducted RCT of high-risk patients with a EuroScore of ≥5 and reported no difference in rates of complications and mortality between OPCAB and CCABG groups during the 30-day postoperative observation.
Observational studies of high-risk patients using EuroScores revealed no difference in the 1- and 5-year survival rates; however, the incidence of stroke was lower for OPCAB.46)
Cavallaro et al.47) compared 83914 patients who had undergone CABG depending on whether they underwent OPCAB or CCABG. Among the high-risk patients (≥85 years, COPD, renal failure, peripheral artery disease, and aortic atherosclerosis), although there was no difference in the incidence of early death, the incidence of stroke was predominantly lower in those who had undergone OPCAB.
Although there have been no RCTs that have included dialysis patients with end-stage renal disease, which is a high-risk factor for CABG, several observational studies including such patients have been reported.48-52) Many reports have indicated that OPCAB is superior with respect to the rate of acute-phase death and incidence of acute-phase complications. Regarding long-term survival, it has been reported that OPCAB is comparable or inferior in the event of incomplete revascularization. Because both of these reports included a small subject sample, we hope that studies involving more subjects will be performed in the future.
The effect of OPCAB has also been examined in patients with chronic kidney disease, who are not dialysis-dependent. Lim et al.53) conducted a meta-analysis on nine observational studies and one RCT that included patients with non-dialysis-dependent renal dysfunction undergoing CABG (1850 patients who had undergone on-pump CABG and 1183 patients who had undergone OPCAB). They reported that OPCAB was much more beneficial than conventional surgery in preventing the development of acute renal failure (OR 0.55; P = 0.01) and early mortality was lower following OPCAB (OR 0.62; P = 0.04). Chawla et al.54) examined 742909 patients (584348 patients who had undergone on-pump CABG and 158561 patients who had undergone OPCAB) from the Society of Thoracic Surgery Database. They reported that in-hospital mortality and renal replacement therapy rates were lower with OPCAB than with CCABG in patients with renal failure.
Puskas et al.21) conducted an observational study using STS database, and for severe cases, which are defined as patients having a risk of mortality of ≥5% as calculated using the STS score, they found that compared with CCABG, OPCAB was associated with significantly reduced in-hospital morbidity and mortality.
In a comparative study of high-risk patients, RCTs revealed no significant difference between CCABG and OPCAB because the subject sample included relatively mild cases for ethical reasons, and the participation of surgeons who were inexperienced in OPCAB meant that the quality of OPCAB cannot be ensured in many instances. For these reasons, RCT results for OPCAB and CCABG were comparable or those for OPCAB were inferior. On the other hand, in the observational studies, as more severe cases were included in the comparison, the results revealed that OPCAB was remarkably effective as well as superior to CCABG.
Conclusions
CABG is a delicate procedure, the outcomes of which vary in accordance with the patient’s condition as well as the level of expertise of the associated institution and surgeon. For example, even if the surgery is completed safely, if postoperative imaging shows that graft patency has not been achieved, the effect of the surgery is consequently extremely poor. For CCABG performed for cardiac arrest using an artificial heart–lung machine, short- and long-term postoperative patency can also be a problem. In OPCAB, it is suggested that the greater technical expertise required makes the reproducibility of OPCAB difficult.
RCT is a means for examining the validity of a treatment method under general clinical conditions and produce many significant results that contribute to the creation of guidelines. However, RCTs can include biased factors, such as limiting the subject sample to mild cases who meet the ethical requirement and the participation of institutions and surgeons who are inexperienced in the procedure. Many reports of RCTs indicate that the acute-phase and long-term mortality rates were comparable between CCABG and OPCAB or that OPCAB was inferior to CCABG. In contrast, many reports of observational studies indicated that OPCAB was superior. The difficulty of reproducing OPCAB is reflected in these results.
In Japan, 65% of CABG procedures are performed using OPCAB, and there are some institutions in which this figure is close to 100%. In the future, we hope that reports will emerge with excellent results, including long-term results, from such institutions experienced in OPCAB.
Disclosure Statement
The authors state that they have no conflict of interest and have received no payment in the preparation of this manuscript.
References
- 1).Goetz RH, Rohman M, Haller JD, et al. Internal mammary-coronary artery anastomosis. A nonsuture method employing tantalum rings. J Thorac Cardiovasc Surg 1961; 41: 378-86. [PubMed] [Google Scholar]
- 2).Konstantinov IE, Robert H. Goetz: the surgeon who performed the first successful clinical coronary artery bypass operation. Ann Thorac Surg 2000; 69: 1966-72. [DOI] [PubMed] [Google Scholar]
- 3).Benetti FJ. Direct coronary surgery with saphenous vein bypass without either cardiopulmonary bypass or cardiac arrest. J Cardiovasc Surg 1985; 26: 217-22. [PubMed] [Google Scholar]
- 4).Buffolo E, Andrade JC, Succi J, et al. Direct myocardial revascularization without cardiopulmonary bypass. Thorac Cardiovasc Surg 1985; 33: 26-9. [DOI] [PubMed] [Google Scholar]
- 5).Tashiro T, Todo K, Haruta Y, et al. Coronary artery bypass without cardiopulmonary bypass. Jap J Thorac Cardiovasc Surg 1993; 41: 598-602. [PubMed] [Google Scholar]
- 6).Tashiro T, Todo K, Haruta Y, et al. Coronary artery bypass grafting without cardiopulmonary bypass for high-risk patients. Cardiovasc Surg 1996; 4: 207-11. [DOI] [PubMed] [Google Scholar]
- 7).Warren OJ, Smith AJ, Alexiou C, et al. The inflammatory response to cardiopulmonary bypass: part 1--mechanisms of pathogenesis. J Cardiothorac Vasc Anesth 2009; 23: 223-31. [DOI] [PubMed] [Google Scholar]
- 8).Baufreton C. Role of surgical factors in strokes after cardiac surgery. Arch Cardiovasc Dis 2010; 103: 326-32. [DOI] [PubMed] [Google Scholar]
- 9).McKhann GM, Grega MA, Borowicz LM, et al. Stroke and encephalopathy after cardiac surgery: an update. Stroke 2006; 37: 562-71. [DOI] [PubMed] [Google Scholar]
- 10).Li Z, Yeo KK, Parker JP, et al. Off-pump coronary artery bypass graft surgery in California, 2003 to 2005. Am Heart J 2008; 156: 1095-102. [DOI] [PubMed] [Google Scholar]
- 11).Mack MJ, Pfister A, Bachand D, et al. Comparison of coronary bypass surgery with and without cardiopulmonary bypass in patients with multivessel disease. J Thorac Cardiovasc Surg 2004; 127: 167-73. [DOI] [PubMed] [Google Scholar]
- 12).Puskas JD, Edwards FH, Pappas PA, et al. Off-pump techniques benefit men and women and narrow the disparity in mortality after coronary bypass grafting. Ann Thorac Surg 2007; 84: 1447-54; discussion 1454-6. [DOI] [PubMed] [Google Scholar]
- 13).Chu D, Bakaeen FG, Dao TK, et al. On-pump versus off-pump coronary artery bypass grafting in a cohort of 63,000 patients. Ann Thorac Surg 2009; 87: 1820-6; discussion 1826-7. [DOI] [PubMed] [Google Scholar]
- 14).Gerola LR, Buffolo E, Jasbik W, et al. Off-pump versus on-pump myocardial revascularization in low-risk patients with one or two vessel disease: perioperative results in a multicenter randomized controlled trial. Ann Thorac Surg 2004; 77: 569-73. [DOI] [PubMed] [Google Scholar]
- 15).Shroyer AL, Grover FL, Hattler B, et al. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med 2009; 361: 1827-37. [DOI] [PubMed] [Google Scholar]
- 16).Puskas JD, Mack MJ, Smith CR. On-pump versus off-pump CABG. N Engl J Med 2010; 362, 851; author reply 853-4. [DOI] [PubMed] [Google Scholar]
- 17).Lamy A, Devereaux PJ, Prabhakaran D, et al. Off-pump or on-pump coronary-artery bypass grafting at 30 days. N Engl J Med 2012; 366: 1489-97. [DOI] [PubMed] [Google Scholar]
- 18).Murzi M, Caputo M, Aresu G, et al. On-pump and off-pump coronary artery bypass grafting in patients with left main stem disease: a propensity score analysis. J Thorac Cardiovasc Surg 2012; 143: 1382-8. [DOI] [PubMed] [Google Scholar]
- 19).Kowalewski M, Pawliszak W, Malvindi PG, et al. Off-pump coronary artery bypass grafting improves short-term outcomes in high-risk patients compared with on-pump coronary artery bypass grafting: meta-analysis. J Thorac Cardiovasc Surg 2016; 151: 60-77.e1-58. [DOI] [PubMed] [Google Scholar]
- 20).Wijeysundera DN, Beattie WS, Djaiani G, et al. Off-pump coronary artery surgery for reducing mortality and morbidity: meta-analysis of randomized and observational studies. J Am Coll Cardiol 2005; 46: 872-82. [DOI] [PubMed] [Google Scholar]
- 21).Puskas JD, Thourani VH, Kilgo P, et al. Off-pump coronary artery bypass disproportionately benefits high-risk patients. Ann Thorac Surg 2009; 88: 1142-7. [DOI] [PubMed] [Google Scholar]
- 22).Angelini GD, Culliford L, Smith DK, et al. Effects of on- and off-pump coronary artery surgery on graft patency, survival, and health-related quality of life: long-term follow-up of 2 randomized controlled trials. J Thorac Cardiovasc Surg 2009; 137: 295-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23).Hueb W, Lopes NH, Pereira AC, et al. Five-year follow-up of a randomized comparison between off-pump and on-pump stable multivessel coronary artery bypass grafting. The MASS III trial. Circulation 2010; 122: S48-52. [DOI] [PubMed] [Google Scholar]
- 24).Puskas JD, Williams WH, O'Donnell R, et al. Off-pump and on-pump coronary artery bypass grafting are associated with similar graft patency, myocardial ischemia, and freedom from reintervention: long-term follow-up of a randomized trial. Ann Thorac Surg 2011; 91: 1836-42, discussion 1842-3. [DOI] [PubMed] [Google Scholar]
- 25).Lamy A, Devereaux PJ, Prabhakaran D, et al. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med 2013; 368: 1179-88. [DOI] [PubMed] [Google Scholar]
- 26).Lamy A, Devereaux PJ, Prabhakaran D, et al. Five-year outcomes after off-pump or on-pump coronary-artery bypass grafting. N Engl J Med 2016; 375: 2359-68. [DOI] [PubMed] [Google Scholar]
- 27).Dalén M, Ivert T, Holzmann MJ, et al. Long-term survival after off-pump coronary artery bypass surgery: a Swedish nationwide cohort study. Ann Thorac Surg 2013; 96: 2054-60. [DOI] [PubMed] [Google Scholar]
- 28).Kirmani BH, Brazier A, Sriskandarajah S, et al. Long-term survival after off-pump coronary artery bypass grafting. Ann Thorac Surg 2016; 102: 22-7. [DOI] [PubMed] [Google Scholar]
- 29).Buda AJ, Macdonald IL, Anderson MJ, et al. Long-term results following coronary bypass operation. Importance of preoperative actors and complete revascularization. J Thorac Cardiovasc Surg 1981; 82: 383-90. [PubMed] [Google Scholar]
- 30).Scott R, Blackstone EH, McCarthy PM, et al. Isolated bypass grafting of the left internal thoracic artery to the left anterior descending coronary artery: late consequences of incomplete revascularization. J Thorac Cardiovasc Surg 2000; 120: 173-84. [DOI] [PubMed] [Google Scholar]
- 31).Mohammadi S, Kalavrouziotis D, Dagenais F, et al. Completeness of revascularization and survival among octogenarians with triple-vessel disease. Ann Thorac Surg 2012; 93: 1432-7. [DOI] [PubMed] [Google Scholar]
- 32).Hattler B, Messenger JC, Shroyer AL, et al. Off-Pump coronary artery bypass surgery is associated with worse arterial and saphenous vein graft patency and less effective revascularization: results from the veterans affairs randomized on/off bypass (ROOBY) trial. Circulation 2012; 125: 2827-35. [DOI] [PubMed] [Google Scholar]
- 33).Houlind K, Fenger-Grøn M, Holme SJ, et al. Graft patency after off-pump coronary artery bypass surgery is inferior even with identical heparinization protocols: results from the Danish on-pump versus off-pump randomization study (DOORS). J Thorac Cardiovasc Surg 2014; 148: 1812-9.e2. [DOI] [PubMed] [Google Scholar]
- 34).Takagi H, Matsui M, Umemoto T. Lower graft patency after off-pump than on-pump coronary artery bypass grafting: an updated meta-analysis of randomized trials. J Thorac Cardiovasc Surg 2010; 140: e45-7. [DOI] [PubMed] [Google Scholar]
- 35).Lingaas PS, Hol PK, Lundblad R, et al. Clinical and radiologic outcome of off-pump coronary surgery at 12 months follow-up: a prospective randomized trial. Ann Thorac Surg 2006; 81: 2089-95. [DOI] [PubMed] [Google Scholar]
- 36).Magee MJ, Alexander JH, Hafley G, et al. Coronary artery bypass graft failure after on-pump and off-pump coronary artery bypass: findings from PREVENT IV. Ann Thorac Surg 2008; 85: 494-9. [DOI] [PubMed] [Google Scholar]
- 37).Nathoe HM, van Dijk D, Jansen EW, et al. A comparison of on-pump and off-pump coronary bypass surgery in low-risk patients. N Engl J Med 2003; 348: 394-402. [DOI] [PubMed] [Google Scholar]
- 38).Puskas JD, Williams WH, Mahoney EM, et al. Off-pump vs conventional coronary artery bypass grafting: early and 1-year graft patency, cost, and quality-of-life outcomes: a randomized trial. JAMA 2004; 291: 1841-9. [DOI] [PubMed] [Google Scholar]
- 39).Robertson MW, Buth KJ, Stewart KM, et al. Complete revascularization is compromised in off-pump coronary artery bypass grafting. J Thorac Cardiovasc Surg 2013; 145: 992-8. [DOI] [PubMed] [Google Scholar]
- 40).Ascione R, Caputo M, Angelini GD. Off-pump coronary artery bypass grafting: not a flash in the pan. Ann Thorac Surg 2003; 75: 306-13. [DOI] [PubMed] [Google Scholar]
- 41).Panesar SS, Athanasiou T, Nair S, et al. Early outcomes in the elderly: a meta-analysis of 4921 patients undergoing coronary artery bypass grafting—comparison between off-pump and on-pump techniques. Heart 2006; 92: 1808-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42).Diegeler A, Börgermann J, Kappert U, et al. Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med 2013; 368: 1189-98. [DOI] [PubMed] [Google Scholar]
- 43).Houlind K, Kjeldsen BJ, Madsen SN, et al. On-pump versus off-pump coronary artery bypass surgery in elderly patients: results from the Danish on-pump versus off-pump randomization study. Circulation 2012; 125: 2431-9. [DOI] [PubMed] [Google Scholar]
- 44).Lemma MG, Coscioni E, Tritto FP, et al. On-pump versus off-pump coronary artery bypass surgery in high-risk patients: operative results of a prospective randomized trial (on-off study). J Thorac Cardiovasc Surg 2012; 143: 625-31. [DOI] [PubMed] [Google Scholar]
- 45).Møller CH, Perko MJ, Lund JT, et al. No major differences in 30-day outcomes in high-risk patients randomized to off-pump versus on-pump coronary bypass surgery: the best bypass surgery trial. Circulation 2010; 121: 498-504. [DOI] [PubMed] [Google Scholar]
- 46).Marui A, Okabayashi H, Komiya T, et al. Benefits of off-pump coronary artery bypass grafting in high-risk patients. Circulation 2012; 126: S151-7. [DOI] [PubMed] [Google Scholar]
- 47).Cavallaro P, Itagaki S, Seigerman M, et al. Operative mortality and stroke after on-pump vs off-pump surgery in high-risk patients: an analysis of 83,914 coronary bypass operations. Eur J Cardiothorac Surg 2014; 45: 159-64. [DOI] [PubMed] [Google Scholar]
- 48).Dewey TM, Herbert MA, Prince SL, et al. Does coronary artery bypass graft surgery improve survival among patients with end-stage renal disease? Ann Thorac Surg 2006; 81: 591-8; discussion 598. [DOI] [PubMed] [Google Scholar]
- 49).Beckermann J, Van Camp J, Li S, et al. On-pump versus off-pump coronary surgery outcomes in patients requiring dialysis: perspectives from a single center and the United States experience. J Thorac Cardiovasc Surg 2006; 131: 1261-6. [DOI] [PubMed] [Google Scholar]
- 50).Shroff GR, Li S, Herzog CA. Survival of patients on dialysis having off-pump versus on-pump coronary artery bypass surgery in the United States. J Thorac Cardiovasc Surg 2010; 139: 1333-8. [DOI] [PubMed] [Google Scholar]
- 51).Boulton BJ, Kilgo P, Guyton RA, et al. Impact of preoperative renal dysfunction in patients undergoing off-pump versus on-pump coronary artery bypass. Ann Thorac Surg 2011; 92: 595-601; discussion 602. [DOI] [PubMed] [Google Scholar]
- 52).Lim JY, Deo SV, Jung SH, et al. Does off-pump coronary artery bypass confer any advantage in patients with end-stage renal failure? A systematic review and meta-analysis. Heart Lung Circ 2015; 24: 55-61. [DOI] [PubMed] [Google Scholar]
- 53).Lim JY, Deo SV, Altarabsheh SE, et al. Off-pump coronary artery bypass grafting may prevent acute renal failure in patients with non-dialysis dependent chronic renal dysfunction: an aggregate meta-analysis. Int J Cardiol 2015; 182: 181-3. [DOI] [PubMed] [Google Scholar]
- 54).Chawla LS, Zhao Y, Lough FC, et al. Off-pump versus on-pump coronary artery bypass grafting outcomes stratified by preoperative renal function. J Am Soc Nephrol 2012; 23: 1389-97. [DOI] [PMC free article] [PubMed] [Google Scholar]