Abstract
Background
We sought to determine the 10-year survivorship and reasons for revision for a fixed-bearing unicompartmental knee arthroplasty (UKA) design. In addition, we report on patient-reported outcomes and satisfaction and compare results of medial vs lateral compartment UKA and cemented vs cementless UKA with the same design.
Methods
We performed a retrospective cohort study on a single-surgeon case series using a single fixed-bearing UKA design in 158 consecutive patients who underwent 177 UKA procedures between July 2000 and December 2010. Cases missing follow-up within the last year, clinically or via telephone, were excluded (n = 17, 10%). A cumulative incidence competing risk model was used to evaluate the cumulative incidence of failure.
Results
Cumulative incidence of revision at a mean follow-up of 10 years was 13%. The majority of revisions (43%, 10/23) were for aseptic tibial component loosening, followed by progression of osteoarthritis (5/23, 22%). All Patient Reported Outcomes Measurement Information System measures demonstrated mean T-scores within one standard deviation from the US population norm. The mean Knee Injury and Osteoarthritis Outcome Score for Joint Replacement was 96.9 (range, 40-100). The mean pain score was 3.8 (range, 0-8). Eighty-six percent of patients were satisfied with the UKA.
Conclusions
At 10-year follow-up, the most common causes for revision were aseptic tibial loosening and adjacent compartment knee arthroplasty, and similar results were found for medial vs lateral compartment and for cemented vs cementless UKA. Surgeons should consider these findings for future UKA designs, and this represents the first study reporting on survivorship and outcomes of this specific UKA design.
Keywords: Unicompartmental knee arthroplasty, Fixed-bearing arthroplasty, Natural knee unicompartmental, Survivorship, Patient-reported outcomes, Satisfaction
Introduction
Unicompartmental knee arthroplasty (UKA) is an alternative to total knee arthroplasty (TKA) for patients with osteoarthritis (OA) isolated to one tibiofemoral compartment of the knee. UKA is a resurfacing procedure of the arthritic femoral condyle and tibia and aims to recreate the natural tibial slope and maintain the joint line, with less bone resection and preservation of the cruciate ligaments [1,2]. UKA may provide better physiological function [3], more rapid recovery [4], less blood loss [5], and a lower risk of complications [6] and may result in physiologic restoration of knee kinematics, resulting in improved postoperative function and gait [2,7]. However, there are some concerns about the increased risk of revision and possibility of failures of certain designs of UKA [8]. There are limited reports of long-term survival and patient satisfaction for different designs of UKA, making decisions on implant selection challenging to practicing surgeons.
UKA can be divided into fixed-bearing and mobile-bearing designs. Mobile-bearing UKA is characterized by a single-radius femoral component with a congruent mobile polyethylene insert on a polished tibial component [9]. Fixed-bearing UKA uses an anatomic femoral component, with a flat, noncongruent polyethylene insert fixed to the tibial baseplate [10]. Excellent function outcomes and implant survivorship have been reported with both designs for medial UKA [1,[11], [12], [13], [14], [15]]. Furthermore, advocates of mobile bearing UKA have suggested that fixed-bearing designs may have high rates of poly wear and tibial loosening because of the increased sheer stress applied to the implant [16,17]. High failure rates have been reported for lateral mobile-bearing UKA [18]. Lateral compartment UKA represents a small portion, 5%-10% of UKA, and has been considered to have poorer results [19]. There are limited published series comparing outcomes of medial vs lateral UKA with fixed-bearing designs.
There are currently 2 modes of implant fixation for UKA, cemented and cementless. Bone cement, polymethyl methacrylate, is used as a fixation method by a variety of UKA designs. Aseptic loosening of tibial or femoral components is a leading cause of failure for cemented designs [[20], [21], [22], [23]]. Cement in UKA may be technically challenging because of the smaller operative exposure and decreased surface area. Radiolucency either partially or uniformly under implants may be due to stress shielding caused by the use of an inadequate cement technique [24]. Most cementless UKAs have been performed in Europe, and there are only a limited number of designs with clinical outcomes reported.
The purpose of this study was to determine the mean 10-year survivorship and reasons for revision for a single fixed-bearing UKA design. In addition, we sought to evaluate patient-reported outcomes at the last follow-up visit including physical function, physical health, mental health, pain, and overall satisfaction with their knee surgery. Finally, we evaluated the difference in these outcomes between cemented vs cementless implants and medial vs lateral UKA.
Material and methods
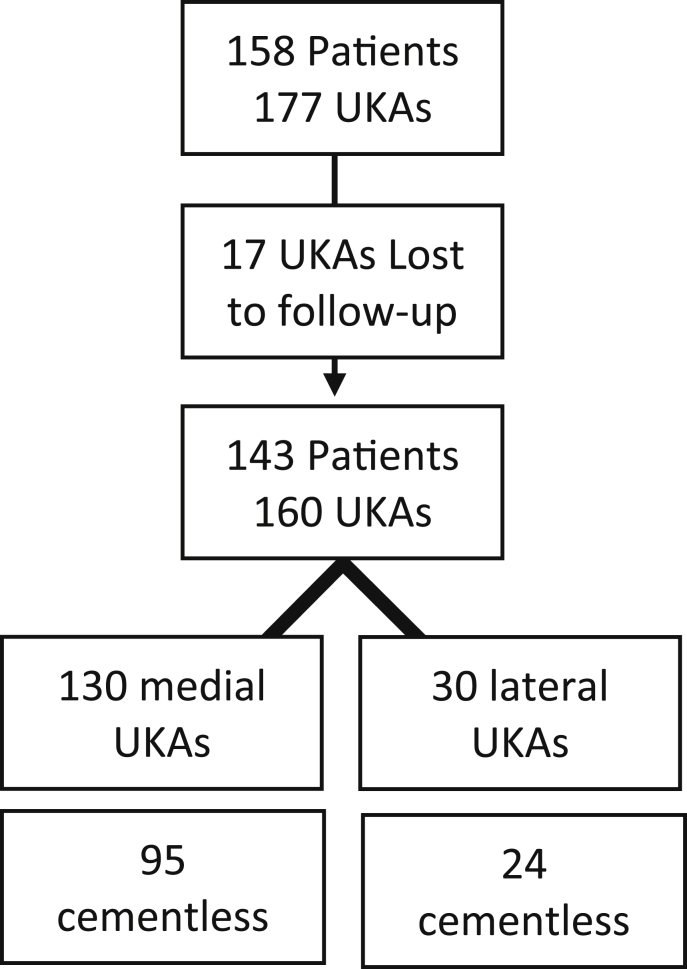
After being deemed exempt from institutional review board approval (# 0,009,672), we performed a retrospective cohort study on 158 consecutive patients who underwent 177 UKAs by a single surgeon between July 2000 and December 2010 at a single academic medical center. The indications for surgery were patients with knee pain that failed extensive nonoperative treatments, radiographic evidence of isolated medial or lateral compartment OA, preoperative flexion of greater than 100 degrees, with less than 10-degree flexion contracture, less than 10 degrees of varus or valgus, asymptomatic patellofemoral joint, and no clinical evidence of anterior cruciate laxity. All surgeries were performed by a single senior surgeon (A.A.H.) using a medial parapatellar approach. Patients who had not reported to the clinic within 1 year of the study start (2018), and who had not been revised before, were considered lost to follow-up (n = 15 patients, n = 17 UKAs; Fig. 1). Ultimately, 160 UKA cases in 143 patients were reviewed. Inspection of the patellofemoral and other compartments was performed on every case as was the status of the anterior cruciate ligament (ACL). An intact ACL was not a prerequisite for continuing with the UKA surgery but was present in the vast majority (157/160). Three cases were found to be ACL deficient, none of which were revised at the last follow-up visit. The mean follow-up for these 3 cases was 11.7 years (range, 10.6-12.7 years). One was a cemented lateral UKA, one was a cemented medial UKA, and the last was a cementless medial UKA.
Figure 1.
Flow chart demonstrating patient attrition and allocation.
In all cases, the Zimmer Natural-Knee UKA (Zimmer Biomet, Warsaw, IN) was implanted. This is a fixed-bearing UKA, and unique to this design was the option for both an all-polyethylene or metal-backed tibial component, as well as a cementless Cancellous-Structured Titanium (Zimmer Biomet, Warsaw, IN) porous coated femoral and tibial component. The tibial component is secured with smooth spikes to help prevent stress shielding and enhance fixation, and the cementless tibial fixation is further enhanced with a titanium cancellous bone screw. The femoral component uses a cruciate stem and a posterior runner to contribute to component fixation as well as mediolateral and rotational stability. The decision to use an all polyethylene tibial component, a metal-backed cemented tibial component, a cementless tibial component, or a cemented or cementless femoral component was made at the time of surgery. The decision was made by the senior surgeon based on patient age, activity level, and an intraoperative assessment of bone quality. The symmetric design of the tibia and design of the femoral component afforded the same implant to be made to the appropriate size and side-matched and used for either medial or lateral UKA surgery.
Chart review was performed to collect information on patient demographics, surgery, complications, and patient-reported outcomes. Cases missing follow-up within the last year, clinically or via telephone, were excluded (n = 17, 10%). As the clinic had not collected patient-reported outcomes measures as routine care until recently, only the patient-reported outcomes measures at the last follow-up visit were collected. They included the National Institute of Health’s Patient Reported Outcomes Measurement Information System (PROMIS) physical function computerized adaptive test, v2.0 (PF CAT), the PROMIS global 10 health assessment, and a satisfaction score. The PROMIS global 10 health assessment allows for both a mental health score and a physical health score [25]. An 11-point numeric pain scale (0-10), derived from the PROMIS global 10 health assessment, is also reported. For this scale, 0 is no pain and 10 is the worst pain imaginable. For PROMIS measures, a higher score indicates more of the item being measured. The scores are reported as transformed scores (T-scores) so that a T-score of 50 (standard deviation [SD], 10) represents the value of the United States general population. The Knee Injury and Osteoarthritis Outcome Score for Joint Replacement (KOOS, JR) was also used [26]. Both the PROMIS PF CAT and the KOOS, JR have been shown to be useful clinical instruments for evaluating changes in the adult reconstruction population [27]. The satisfaction survey was based on the recommendations of Rolfson et al. [28]. It consists of a single question with a five-point Likert scale ranging from very satisfied to very unsatisfied.
Data are reported using descriptive statistics. Given expired patients were no longer at risk for revision, a competing risk model was used to evaluate the cumulative incidence of failure and revision to TKA, with death as the competing risk, and subdistribution hazard ratios (SHRs) are reported. This same model was used in the subgroup analyses while also controlling for age and sex. Given that knees were clustered within patients, regression analyses for all outcomes were performed using generalized estimating equations for the subgroup analyses. Exploratory analyses were performed for between-group comparisons between cemented and cementless UKA, as well as medial vs lateral UKA. For demographic variables, a logistic generalized estimating equation model was used treating the group as the dependent variable and the characteristic as the independent variable. Given the small number of events, a Fishers exact test was used to compare the proportion of patients with each revision diagnosis between groups. All statistical analyses were performed using a commercially available statistical software program (Stata, v14.2; StataCorp, College Station, TX). Significance was assessed at P < .05.
Results
Eighty-one percent were medial UKA (130/160) and 74% (119/160) were cemented. The mean age of the population was 68 years (range, 43-86), and 58% were female (93/160; Table 1). The mean follow-up duration was 9.9 years (range, 0.93-21.8), where some patients had died or been revised before the most recent long-term follow-up time point.
Table 1.
Patient characteristics.
| Characteristic | Value |
|---|---|
| Age, mean (range) | 68 years (43-86) |
| Sex, n (%) | |
| Female | 93 (58%) |
| Male | 67 (42%) |
| BMI, mean (range) | 29 (20-43) |
| ASA score, median (IQR) | 2 (2-2) |
ASA, American Society of Anesthesiologists Physical Status Classification; BMI, body mass index, kg/m; IQR, interquartile range.
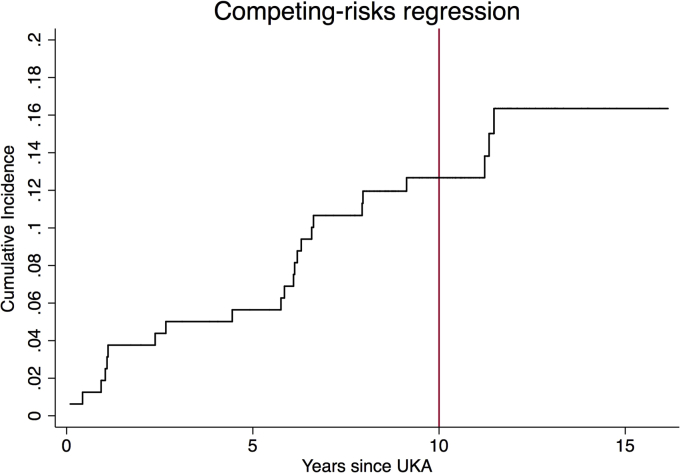
The cumulative incidence of revision to TKA at a mean follow-up of 10 years was approximately 13% when including death as a competing risk (Fig. 2). Overall, 23 cases underwent revision to TKA and 43 expired before revision. The mean time to death was 8 years (range, 1-15). The mean age of those who expired was 71 (range, 53-86 years). Most revisions (10/23) were for aseptic tibial component loosening. This was followed by progression of OA requiring conversion to TKA (5/23). Two underwent revision due to infection (2/23) and 3 for periprosthetic fracture (3/23). Finally, 3 cases were revised at outside hospitals, and documentation regarding reason for revision was not available for review. The mean time to failure in aseptic loosening cases was 4 years (range, 0.93-11.2).
Figure 2.
A cumulative incidence plot demonstrating revision to total knee arthroplasty.
At the last follow-up visit, all PROMIS measures demonstrated mean T-scores within one SD from the US population norm (Table 2). The KOOS, JR scores were excellent with a mean score of 96.9 (range, 40-01). The mean pain score was 3.8 (range, 0-8) and the median satisfaction score was 4 (satisfied, interquartile range, 4-5). When dichotomizing satisfaction to either satisfied (satisfied [3] or very satisfied [4]) or unsatisfied (neutral [2], unsatisfied [1], very unsatisfied [29]), 86% of patients were satisfied with the index UKA procedure.
Table 2.
Patient reported outcomes.
| Outcome | Entire cohort |
|---|---|
| PF CAT, mean (range) | 41.8 (23-57.1) |
| Global Physical Health, mean (range) | 46.4 (26.7-67.7) |
| Global Mental Health, mean (range) | 42.9 (21.2-63) |
| Global Pain, mean (range) | 3.8 (0-8) |
| Global Pain, median (IQR) | 4 (1-7) |
| KOOS, JR, mean (range) | 96.9 (40-100) |
| Satisfaction, median (IQR) | 4 (4-5) |
IQR, interquartile range; KOOS, JR, Knee Injury and Osteoarthritis Outcome for Joint Replacement; PF CAT, physical function computerized adaptive test.
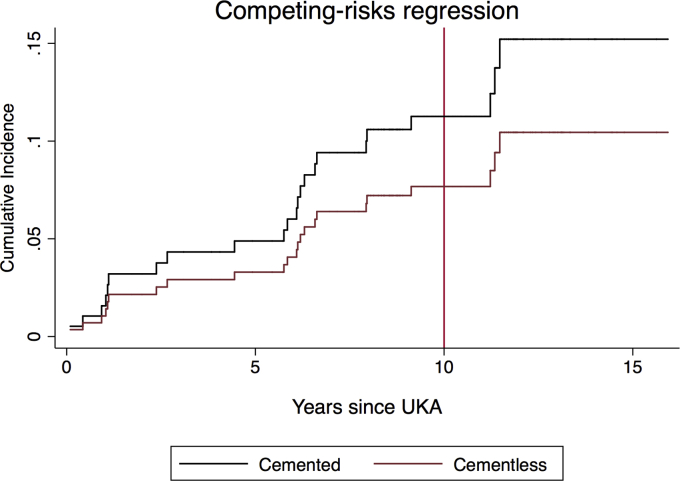
Cementless UKAs were younger (P < .001), and there was a greater proportion of males, in the cementless UKAs (P = .007; Table 3). There was no difference in body mass index (P = .572) or American Society of Anesthesiologists Physical Status Classification scores (P = .740; Table 3) between cemented and cementless UKAs. The cumulative incidence of revision TKA at 10 years was approximately 11% for the cemented group and 8% for the cementless group (SHR, 0.67; 95% confidence interval, 0.22-20.2, P = .476) when including death as a competing risk (Fig. 3). Aside from the KOOS JR (P = .017), PROs did not differ between groups (all, P > .05; Table 4). Satisfaction was 85% (101/119) in the cemented group and 88% (36/41) in the cementless (P = .570). Overall, 15 patients (12.6%) in the cemented group and 8 patients (19.5%) in the cementless group underwent revision to TKA (P = .580, Table 5). With the numbers available, reasons for revision did not differ between the groups (all, P > .05; Table 5).
Table 3.
Comparison of patient demographics between cemented and cementless UKA.
| Characteristic | Cemented, n = 119 | Cementless, n = 41 | P value |
|---|---|---|---|
| Agea, mean (range) | 70 (49-86) | 63 (43-80) | <.001 |
| Male Sex, n (%) | 41/119 (34%) | 26/41 (63%) | .007 |
| BMI, mean (range) | 27.8 (20.2-43.3) | 29.2 (22-39.6) | 0.572 |
| ASA, median (IQR) | 2 (2-2) | 2 (2-2) | .740 |
ASA, American Society of Anesthesiologists physical status classification; BMI, body mass index measured as kg/m; IQR, interquartile range.
Age in years.
Figure 3.
A cumulative incidence plot demonstrating revision in cemented and cementless unicompartmental knee arthroplasty cases.
Table 4.
Patient-reported outcome measures between cemented and cementless UKA cases.
| Outcome | Cemented | Cementless | ß (95% CI), P value |
|---|---|---|---|
| PF CAT | 41.4 (39.1 to 43.6) | 44.3 (10.1 to 48.6) | 2.96 (−1.03 to 6.96), 0.144 |
| Physical Health | 45.9 (42.9 to 48.8) | 49.2 (44.6 to 53.8) | 3.32 (−1.77 to 8.40), 0.194 |
| Mental Health | 42.1 (40.0 to 44.3) | 44.5 (41.1 to 47.9) | 2.38 (−0.88 to 5.6), 0.151 |
| Pain | 3.7 (2.8 to 4.6) | 3.3 (2.2 to 4.4) | −0.38 (−1.7 to 0.97), 0.571 |
| KOOS, JR | 99.1 (95.4 to 102.7) | 92.7 (88.4 to 97.0) | −6.37 (−11.6 to −1.2), 0.017 |
CI, confidence interval; KOOS, JR, Knee Injury and Osteoarthritis Outcome for Joint Replacement; PF CAT, physical function computerized adaptive test.
Outcomes reported as adjusted mean (95% CI).
Table 5.
Reasons for revision between cemented and cementless implants.
| Diagnosis | Cemented | Cementless |
|---|---|---|
| Aseptic loosening | 7/15 | 3/8 |
| Osteoarthritis progression | 3/15 | 2/8 |
| Periprosthetic fracture | 3/15 | 0 |
| Infection | 0 | 2/8 |
| Unknown | 2/15 | 1/8 |
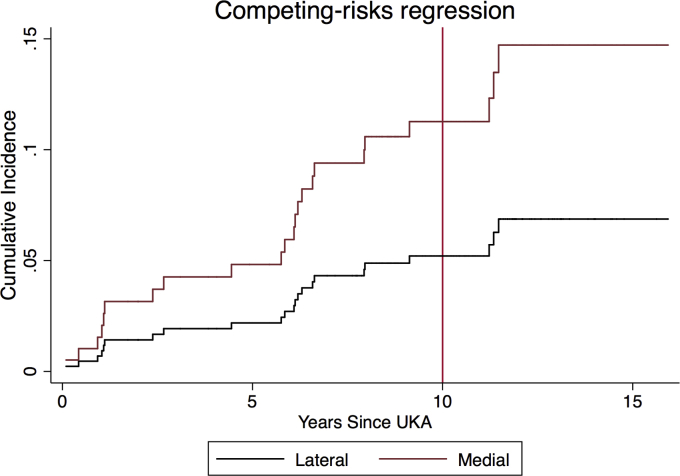
There was no difference in age, sex, or American Society of Anesthesiologists Physical Status Classification score between medial and lateral UKAs (Table 6). Body mass index was lower in the lateral UKA cohort (P = .026; Table 6). The cumulative incidence of revision TKA at 10 years was approximately 11% for the medial UKAs and 5% for the lateral UKAs (SHR, 0.67; 95% confidence interval, 0.22-20.2, P = .476) when including death as a competing risk (Fig. 4). Aside from the PROMIS global physical health score (P = .021), and with the numbers available, PROs did not differ between groups (all, P > .05; Table 7). Satisfaction was 85% (109/130) in the medial UKAs and 92% (28/30) in the lateral UKAs (P = .309). Overall, 21 patients (16.2%) in the medial group and 2 patients (6.7%) in the lateral group underwent revision to TKA (P = .253; Table 8). With the numbers available, reasons for revision did not differ between the groups (all, P > .05; Table 8).
Table 6.
Comparison of patient demographics between medial and lateral UKA.
| Characteristic | Medial, n = 130 | Lateral, n = 30 | P value |
|---|---|---|---|
| Agea, mean (range) | 68 (43-86) | 69 (52-58) | .710 |
| Female sex, n (%) | 59/130 (55%) | 22/30 (73%) | .123 |
| BMI, mean (range) | 29.4 (20-43) | 26.2 (20.2-35.8) | .026 |
| ASA, median (IQR) | 2 (2-2) | 2 (2-2) | .589 |
ASA, American Society of Anesthesiologists physical status classification; BMI, body mass index measured as kg/m; IQR, interquartile range.
Age in years.
Figure 4.
A cumulative incidence plot demonstrating revision in medial and lateral unicompartmental knee arthroplasty cases.
Table 7.
Patient-reported outcome measures between medial vs Lateral UKAs
| Outcome | Medial | Lateral | ß (95% CI), P value |
|---|---|---|---|
| PF CAT | 41.1 (39.2 to 42.9) | 44.1 (40.9 to 47.3) | −3.01 (−6.7 to 0.60), 0.101 |
| Physical health | 45.04 (42.9 to 47.2) | 51.0 (46.9 to 55.2) | −6.0 (−11.03 to −0.95), 0.021 |
| Mental health | 42.6 (41.0 to 44.3) | 43.2 (39.8 to 46.7) | −0.61 (−4.55 to 3.33), 0.758 |
| Pain | 3.74 (2.90 to 4.70) | 3.2 (1.6 to 4.7) | 0.57 (−1.23 to 2.41), 0.531 |
| KOOS, JR | 96.0 (91.8 to 100.3) | 101.3 (94.5 to 108.02) | −5.2 (−13.1 to 2.7), P = .186 |
CI, confidence interval; KOOS JR, Knee Injury and Osteoarthritis Outcome for Joint Replacement; PF CAT, physical function computerized adaptive test.
Outcomes reported as adjusted mean (95% CI).
Table 8.
Reasons for revision between medial and lateral UKAs.
| Diagnosis | Medial | Lateral |
|---|---|---|
| Aseptic loosening | 10/21 | 0 |
| OA progression | 4/21 | 1/2 |
| Periprosthetic fracture | 3/21 | 0 |
| Infection | 2/21 | 0 |
| Unknown | 2/21 | 1/2 |
OA, osteoarthritis.
Discussion
Making decisions on implant selection is challenging for surgeons because of a lack of long-term reports of different UKA designs. There is a paucity of literature comparing outcomes of medial and lateral fixed-bearing UKAs and those of cemented and cementless UKAs, and to our knowledge, this is the only report of mid- to long-term follow-up of this implant. The cumulative incidence of revision after a single fixed-bearing UKA design in this study was 13% at 10 years. Overall 23 patients underwent revision to TKA, with most revisions (43%, 10/23) required for aseptic tibial component loosening, followed by progression of OA (5/23, 22%). PROs were within 1 SD of the US general population, KOOS Jr. knee function scores were 96.9 (40-100), and 86% of patients were satisfied (satisfied or very satisfied) with the index UKA. Medial and lateral compartment and cemented and cementless UKA performed similarly with no difference in the cumulative incidence of revision to TKA, reason for revision, PROs, or patient satisfaction between these groups.
This study has several limitations. First this was a single surgeon experience, at a single academic medical center, and the results may not be broadly generalizable. This was a retrospective study introducing the potential for selection bias both for the UKA procedure and for the type of implant chosen. However, this was a consecutive series of patients undergoing UKA all treated by the same surgeon; no other UKA implants were used by this surgeon during the study period. Further follow-up was performed either by the operating surgeon or his predecessors at the surgical institution. Owing to geographic restrictions, there was no complete radiographic follow-up for every patient. However, as part of their routine care, every patient had completed in-clinic or telephone follow-up within the last year. An intact ACL was not a prerequisite for UKA in this cohort, and this may confound our results. However, other investigations have found equivalent survivorship of fixed-bearing UKA in knees with ACL deficiency [30]. Furthermore, as this was a convenience sample of all cases, subgroup analyses between cemented and cementless and medial vs lateral UKA are likely underpowered to detect a difference. In addition, in 2 of the 3 periprosthetic fracture failures, imaging before the fracture was not available for review; thus, it is possible that loosening may have contributed to the fracture.
Our results showed slightly lower survivorship than other single-center cohort studies reported in the literature on fixed-bearing UKA from 93% to 98% at 10 years [[31], [32], [33], [34]]. Our results are more similar to the upper-level survivorship reported in recent large national registries which have found UKA 10-year survivorship between 81% and 88% [[35], [36], [37]]. Our results outperform the 16.1% revision rate using this implant seen at 7 years in the Australian registry [38]. Upon examining the registry studies, it is noted that the causes of UKA failure are often not described in detail. This is seen in the registry of Norway which does not report progression of OA as a cause for failure, which is our second most frequently noted failure mechanism [39]. Furthermore, registry studies reporting causes of UKA failure often differs from cohort studies with high rates of revision for “unexplained pain” [40,41]. It is possible that some “unexplained pain” could be a surrogate in these studies for progression of OA, as Park et al. assessed patients with unexplained pain after UKA and found 82% of patients had grade 3 or 4 OA based on magnetic resonance imaging evaluation of the other compartment [42].
The most common cause for revision in this series was aseptic tibial component loosening, followed by progression of OA. This is similar to the findings by ven der List et al. who reviewed failure mechanisms of medial UKA in a review of 37 cohort studies and 2 registry-based studies showing aseptic loosening (36%) and progression of OA (20%) to be the most common failure modes [43]. While our cohort included both lateral and medial UKAs, Ernstbrunner et al. evaluated failure mechanisms of lateral UKA in a review of 14 cohort studies and 2 registry-based studies showing progression of OA (30%) and aseptic loosening (22%) as the most common causes of failure [44].
Proponents of mobile-bearing UKA have suggested that fixed-bearing designs may have high rates of poly wear and tibial loosening due to the increased sheer stress applied to the implant [16,17]. In their review of medial UKA failure mechanisms, ven der List et al. found no difference in aseptic loosening rates between fixed-bearing and mobile-bearing designs but did find higher rates of polyethylene wear in the fixed-bearing group [43]. In our study, the mean time to failure in aseptic loosening was 4 years, and aseptic tibial component loosening was the most frequent failure mechanism similar to those of prior publications. Fixation of the Natural-Knee (Zimmer Biomet, Warsaw, IN) UKA tibial component relies on cemented smooth spikes, and the cementless tibial fixation is further enhanced with a cancellous bone screw. Other similar fixed-bearing UKA designs such as the ZUK or Miller-Galante (Zimmer Biomet, Warsaw, IN) have added a rotational fin, which is intended to guard against sheer and rotational forces. In their review of 460 medial UKAs with the ZUK (Zimmer Biomet, Warsaw, IN), Winnock de Grave et al. found at mean follow-up of 5.5 years no cases of component loosening [32]. At 10 years follow-up with the Miller-Galante medial UKA, Berger et al. found no cases of tibial component loosening in 62 knees [33] and Naudie et al. only found one case of tibial component loosening in 112 knees [45]. Argenson et al reviewed their experience with the Miller-Galante medial UKA at 3- to 10-year follow-up and noted no failures for aseptic loosening; however, in their follow-up report of the same cohort at a mean of 20-year follow-up, they noted aseptic loosening in 2 knees [1,12].
Looking at other current data on UKA outcomes, 10-year functional outcomes after mobile-bearing UKA were reported by the Oxford group, who found mean Oxford Knee Score of 40 (SD, 9; range, 2-48) with 79% of knees having an excellent or good outcome. For fixed-bearing UKA designs, at a mean follow-up of 20 years, Argenson et al. found average clinical and functional Knee Society scores of 91 and 88, respectively [12]. At 10-year follow-up, HSS knee scores of 92 have been reported [33], and mean clinical and function Knee Society scores of 93 and 80 have been reported [45]. Similar to these studies, we also found very high functional outcome scores; at 10 years, our mean KOOS, JR score was 96.9 (40-100). One limitation of the KOOS, JR is potential ceiling effects; however, this is a validated outcome instrument. In addition, we were able to report patient-reported outcomes using the PROMIS PF CAT, Global Physical health, Global Mental Health, and Global Pain scores all within 1 SD of the US general population.
We report high satisfaction at a mean of 10 years, with 86% of patients reported being satisfied or very satisfied at the last follow-up visit. There is a paucity of other studies reporting mid- to long-term satisfaction after UKA. At 3- to 10-year follow-up after medial fixed-bearing UKA, Argenson et al. report 60% (96/160) of patients were enthusiastic, 36% (57/160) were satisfied, 3% (4/160) reported no change, and 2% (3/160) were not satisfied [1]. In their follow-up study at a mean of 20 years, they do not report satisfaction scores [12].
Historically lateral compartment UKA has been considered to be more challenging and to have poorer results, representing only 5%-10% of UKA [19]. Liebs and Herzberg found similar survival rates for medial (90%) and lateral (83%) UKA but improved Western Ontario and McMaster Universities Osteoarthritis Index pain, and Short Form 36 scores for the medial UKA group [46]. These findings differ from our finding of equivalent survivorship, PROs, functional outcomes, and satisfaction between medial and lateral UKAs but may be explained by the use of mobile-bearing lateral UKA, which have shown to have worse outcomes compered with fixed-bearing lateral UKA [47]. Supporting our findings but with only short-term follow-up, van der List et al. found equivalent function outcomes between medial and lateral UKA [48].
Most cementless UKAs have been performed in Europe, and there are only a limited number of fixed-bearing cementless designs with clinical outcomes reported. The AlpinaUNI (Biomet, France, Valence) was primarily used in France and is a cementless hydroxyapatite-coated anatomic prosthesis; 65 knees with a minimum of 10-year follow-up showed 88% survivorship for revision for any reason [49]. The Unix UKR (Stryker Orthopedics, Mahwah, NJ) is also a hydroxyapatite-coated implant with a unique horizontal fin inserted under the tibial spine; it has no pegs or keel, and the surgeon can use up to 5 screws to augment the tibial component fixation. Two centers have evaluated this prosthesis at 5-13 years, with one reporting 1 failure for ACL rupture and 1 failure for a fall in 125 implants [50] and the other center reporting on 85 implants with an overall survival of 76% at 12 years [51]. In this study, we found a cumulative incidence of revision to TKA at 10 years to be 8% for the cementless group, with no differences noted in survivorship, PROs, functional outcomes, or satisfaction scores between cemented and cementless UKAs.
Conclusions
This study found survivorship for this fixed-bearing UKA design similar to the upper-level survivorship found in registry studies for UKA. We found no differences in PROs, function scores, and satisfaction for medial vs lateral nor cemented vs cementless UKA. We hope surgeons consider our findings when counseling patients who may be candidates for medial or lateral UKA and when considering fixation types. Future research should continue to follow up these patients to a longer term, and properly powered randomized multicenter studies can appropriately assess outcomes of cemented vs cementless designs of UKA.
Conflict of interest
Ryland Kagan, MD, Research support from KCI Acelity Inc.; Mike B. Anderson, MSC, Pain employee of Ortho Development Corp.; Paid consultant for OrthoGrid Systems, Inc.; Stock OrthoGrid Systems, Inc.; Aaron A. Hofmann, MD, Royalties from Zimmer Biomet; Unpaid consultant for TJO (Total Joint Orthopedics); Christopher E. Pelt, MD, Royalties from TJO (Total Joint Orthopedics); Speakers bureau/paid presentations for KCI Acelity Inc., TJO, Zimmer Biomet; Paid consultant for KCI Acelity Inc., TJO, Zimmer Biomet; Stock Joint Development LLC; Research support from Zimmer Biomet; Board member/committee appointments for AAOS, American Association of Hip and Knee Surgeons (AAHKS).
The other authors declare no potential conflict of interest. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2020.02.016
Supplementary data
References
- 1.Argenson J.N., Chevrol-Benkeddache Y., Aubaniac J.M. Modern unicompartmental knee arthroplasty with cement: a three to ten-year follow-up study. J Bone Joint Surg Am. 2002;84-A(12):2235. [PubMed] [Google Scholar]
- 2.Newman J., Pydisetty R.V., Ackroyd C. Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg Br. 2009;91(1):52. doi: 10.1302/0301-620X.91B1.20899. [DOI] [PubMed] [Google Scholar]
- 3.Laurencin C.T., Zelicof S.B., Scott R.D., Ewald F.C. Unicompartmental versus total knee arthroplasty in the same patient. A comparative study. Clin Orthop Relat Res. 1991;(273):151. [PubMed] [Google Scholar]
- 4.Kozinn S.C., Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am. 1989;71(1):145. [PubMed] [Google Scholar]
- 5.Schwab P.E., Lavand'homme P., Yombi J.C., Thienpont E. Lower blood loss after unicompartmental than total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3494. doi: 10.1007/s00167-014-3188-x. [DOI] [PubMed] [Google Scholar]
- 6.Morris M.J., Molli R.G., Berend K.R., Lombardi A.V., Jr. Mortality and perioperative complications after unicompartmental knee arthroplasty. Knee. 2013;20(3):218. doi: 10.1016/j.knee.2012.10.019. [DOI] [PubMed] [Google Scholar]
- 7.Wiik A.V., Manning V., Strachan R.K., Amis A.A., Cobb J.P. Unicompartmental knee arthroplasty enables near normal gait at higher speeds, unlike total knee arthroplasty. J Arthroplasty. 2013;28(9 Suppl):176. doi: 10.1016/j.arth.2013.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vasso M., Corona K., D'Apolito R., Mazzitelli G., Panni A.S. Unicompartmental knee arthroplasty: modes of failure and conversion to total knee arthroplasty. Joints. 2017;5(1):44. doi: 10.1055/s-0037-1601414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greco N.J., Lombardi A.V., Jr., Price A.J., Berend M.E., Berend K.R. Medial mobile-bearing unicompartmental knee arthroplasty in young patients aged less than or equal to 50 years. J Arthroplasty. 2018;33:2435. doi: 10.1016/j.arth.2018.03.069. [DOI] [PubMed] [Google Scholar]
- 10.Forster-Horvath C., Artz N., Hassaballa M.A. Survivorship and clinical outcome of the minimally invasive Uniglide medial fixed bearing, all-polyethylene tibia, unicompartmental knee arthroplasty at a mean follow-up of 7.3years. Knee. 2016;23(6):981. doi: 10.1016/j.knee.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Cartier P., Cheaib S. Unicondylar knee arthroplasty. 2-10 years of follow-up evaluation. J Arthroplasty. 1987;2(2):157. doi: 10.1016/s0883-5403(87)80023-2. [DOI] [PubMed] [Google Scholar]
- 12.Argenson J.N., Blanc G., Aubaniac J.M., Parratte S. Modern unicompartmental knee arthroplasty with cement: a concise follow-up, at a mean of twenty years, of a previous report. J Bone Joint Surg Am. 2013;95(10):905. doi: 10.2106/JBJS.L.00963. [DOI] [PubMed] [Google Scholar]
- 13.Neufeld M.E., Albers A., Greidanus N.V., Garbuz D.S., Masri B.A. A comparison of mobile and fixed-bearing unicompartmental knee arthroplasty at a minimum 10-year follow-up. J Arthroplasty. 2018;33:1713. doi: 10.1016/j.arth.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 14.Alnachoukati O.K., Barrington J.W., Berend K.R. Eight hundred twenty-five medial mobile-bearing unicompartmental knee arthroplaties: the first 10-year US multi-center survival analysis. J Arthroplasty. 2018;33(3):677. doi: 10.1016/j.arth.2017.10.015. [DOI] [PubMed] [Google Scholar]
- 15.Parratte S., Ollivier M., Lunebourg A., Abdel M.P., Argenson J.N. Long-term results of compartmental arthroplasties of the knee: long term results of partial knee arthroplasty. Bone Joint J. 2015;97-B(10 Suppl A):9. doi: 10.1302/0301-620X.97B10.36426. [DOI] [PubMed] [Google Scholar]
- 16.Argenson J.N., Parratte S. The unicompartmental knee: design and technical considerations in minimizing wear. Clin Orthop Relat Res. 2006;452:137. doi: 10.1097/01.blo.0000229358.19867.60. [DOI] [PubMed] [Google Scholar]
- 17.Kim K.T., Lee S., Lee J.I., Kim J.W. Analysis and treatment of complications after unicompartmental knee arthroplasty. Knee Surg Relat Res. 2016;28(1):46. doi: 10.5792/ksrr.2016.28.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walker T., Zahn N., Bruckner T. Mid-term results of lateral unicondylar mobile bearing knee arthroplasty: a multicentre study of 363 cases. Bone Joint J. 2018;100-B(1):42. doi: 10.1302/0301-620X.100B1.BJJ-2017-0600.R1. [DOI] [PubMed] [Google Scholar]
- 19.Fiocchi A., Condello V., Madonna V., Bonomo M., Zorzi C. Medial vs lateral unicompartmental knee arthrroplasty: clinical results. Acta Biomed. 2017;88(2S):38. doi: 10.23750/abm.v88i2-S.6510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Furnes O., Espehaug B., Lie S.A., Vollset S.E., Engesaeter L.B., Havelin L.I. Failure mechanisms after unicompartmental and tricompartmental primary knee replacement with cement. J Bone Joint Surg Am. 2007;89(3):519. doi: 10.2106/JBJS.F.00210. [DOI] [PubMed] [Google Scholar]
- 21.Hamilton W.G., Collier M.B., Tarabee E., McAuley J.P., Engh C.A., Jr., Engh G.A. Incidence and reasons for reoperation after minimally invasive unicompartmental knee arthroplasty. J Arthroplasty. 2006;21(6 Suppl 2):98. doi: 10.1016/j.arth.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 22.Knight J.L., Atwater R.D., Guo J. Early failure of the porous coated anatomic cemented unicompartmental knee arthroplasty. Aids to diagnosis and revision. J Arthroplasty. 1997;12(1):11. doi: 10.1016/s0883-5403(97)90041-3. [DOI] [PubMed] [Google Scholar]
- 23.Aleto T.J., Berend M.E., Ritter M.A., Faris P.M., Meneghini R.M. Early failure of unicompartmental knee arthroplasty leading to revision. J Arthroplasty. 2008;23(2):159. doi: 10.1016/j.arth.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 24.Pandit H., Jenkins C., Beard D.J. Cementless Oxford unicompartmental knee replacement shows reduced radiolucency at one year. J Bone Joint Surg Br. 2009;91(2):185. doi: 10.1302/0301-620X.91B2.21413. [DOI] [PubMed] [Google Scholar]
- 25.Hays R.D., Bjorner J.B., Revicki D.A., Spritzer K.L., Cella D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res. 2009;18(7):873. doi: 10.1007/s11136-009-9496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lyman S., Lee Y.Y., Franklin P.D., Li W., Cross M.B., Padgett D.E. Validation of the KOOS, JR: a short-form knee arthroplasty outcomes survey. Clin Orthop Relat Res. 2016;474(6):1461. doi: 10.1007/s11999-016-4719-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hung M., Saltzman C.L., Greene T. Evaluating instrument responsiveness in joint function: the HOOS JR, the KOOS JR, and the PROMIS PF CAT. J Orthop Res. 2018;36(4):1178. doi: 10.1002/jor.23739. [DOI] [PubMed] [Google Scholar]
- 28.Rolfson O., Wissig S., van Maasakkers L. Defining an international standard set of outcome measures for patients with hip or knee osteoarthritis: consensus of the international consortium for health outcomes measurement hip and knee osteoarthritis working group. Arthritis Care Res (Hoboken) 2016;68(11):1631. doi: 10.1002/acr.22868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Noble P.C., Conditt M.A., Cook K.F., Mathis K.B. The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35. doi: 10.1097/01.blo.0000238825.63648.1e. [DOI] [PubMed] [Google Scholar]
- 30.Engh G.A., Ammeen D.J. Unicondylar arthroplasty in knees with deficient anterior cruciate ligaments. Clin Orthop Relat Res. 2014;472(1):73. doi: 10.1007/s11999-013-2982-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fabre-Aubrespy M., Ollivier M., Pesenti S., Parratte S., Argenson J.N. Unicompartmental knee arthroplasty in patients older than 75 results in better clinical outcomes and similar survivorship compared to total knee arthroplasty. A matched controlled study. J Arthroplasty. 2016;31(12):2668. doi: 10.1016/j.arth.2016.06.034. [DOI] [PubMed] [Google Scholar]
- 32.Winnock de Grave P., Barbier J., Luyckx T., Ryckaert A., Gunst P., Van den Daelen L. Outcomes of a fixed-bearing, medial, cemented unicondylar knee arthroplasty design: survival analysis and functional score of 460 cases. J Arthroplasty. 2018;33:2792. doi: 10.1016/j.arth.2018.04.031. [DOI] [PubMed] [Google Scholar]
- 33.Berger R.A., Meneghini R.M., Jacobs J.J. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg Am. 2005;87(5):999. doi: 10.2106/JBJS.C.00568. [DOI] [PubMed] [Google Scholar]
- 34.Cartier P., Sanouiller J.L., Grelsamer R.P. Unicompartmental knee arthroplasty surgery. 10-year minimum follow-up period. J Arthroplasty. 1996;11(7):782. doi: 10.1016/s0883-5403(96)80177-x. [DOI] [PubMed] [Google Scholar]
- 35.Niinimaki T., Eskelinen A., Makela K., Ohtonen P., Puhto A.P., Remes V. Unicompartmental knee arthroplasty survivorship is lower than TKA survivorship: a 27-year Finnish registry study. Clin Orthop Relat Res. 2014;472(5):1496. doi: 10.1007/s11999-013-3347-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liddle A.D., Judge A., Pandit H., Murray D.W. Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet. 2014;384(9952):1437. doi: 10.1016/S0140-6736(14)60419-0. [DOI] [PubMed] [Google Scholar]
- 37.The New Zealand Joint Replacement Registry. Eighteen Year Report January 1999 to December 2016. nzoa.org.nz. [Accessed 1 December 2016].
- 38.AOANJRR; 2010. The Australian Orthopaedic Association National Joint Replacement Registry.aoanjrr.sahmri.com [DOI] [PubMed] [Google Scholar]
- 39.Norwegian National Advisory Unit on Arthroplasty and Hip Fractures; 2018. Norwegian National Arthroplasty Register Report.nrlweb.ihelse.net/eng [Google Scholar]
- 40.Baker P.N., Jameson S.S., Deehan D.J., Gregg P.J., Porter M., Tucker K. Mid-term equivalent survival of medial and lateral unicondylar knee replacement: an analysis of data from a National Joint Registry. J Bone Joint Surg Br. 2012;94(12):1641. doi: 10.1302/0301-620X.94B12.29416. [DOI] [PubMed] [Google Scholar]
- 41.Baker P.N., Petheram T., Avery P.J., Gregg P.J., Deehan D.J. Revision for unexplained pain following unicompartmental and total knee replacement. J Bone Joint Surg Am. 2012;94(17):e126. doi: 10.2106/JBJS.K.00791. [DOI] [PubMed] [Google Scholar]
- 42.Park C.N., Zuiderbaan H.A., Chang A., Khamaisy S., Pearle A.D., Ranawat A.S. Role of magnetic resonance imaging in the diagnosis of the painful unicompartmental knee arthroplasty. Knee. 2015;22(4):341. doi: 10.1016/j.knee.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 43.van der List J.P., Zuiderbaan H.A., Pearle A.D. Why do medial unicompartmental knee arthroplasties fail today? J Arthroplasty. 2016;31(5):1016. doi: 10.1016/j.arth.2015.11.030. [DOI] [PubMed] [Google Scholar]
- 44.Ernstbrunner L., Imam M.A., Andronic O., Perz T., Wieser K., Fucentese S.F. Lateral unicompartmental knee replacement: a systematic review of reasons for failure. Int Orthop. 2018;42:1827. doi: 10.1007/s00264-017-3662-4. [DOI] [PubMed] [Google Scholar]
- 45.Naudie D., Guerin J., Parker D.A., Bourne R.B., Rorabeck C.H. Medial unicompartmental knee arthroplasty with the Miller-Galante prosthesis. J Bone Joint Surg Am. 2004;86-A(9):1931. doi: 10.2106/00004623-200409000-00011. [DOI] [PubMed] [Google Scholar]
- 46.Liebs T.R., Herzberg W. Better quality of life after medial versus lateral unicondylar knee arthroplasty. Clin Orthop Relat Res. 2013;471(8):2629. doi: 10.1007/s11999-013-2966-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Marson B., Prasad N., Jenkins R., Lewis M. Lateral unicompartmental knee replacements: early results from a District General Hospital. Eur J Orthop Surg Traumatol. 2014;24(6):987. doi: 10.1007/s00590-013-1277-z. [DOI] [PubMed] [Google Scholar]
- 48.van der List J.P., Chawla H., Villa J.C., Pearle A.D. Different optimal alignment but equivalent functional outcomes in medial and lateral unicompartmental knee arthroplasty. Knee. 2016;23(6):987. doi: 10.1016/j.knee.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 49.Lecuire F., Berard J.B., Martres S. Minimum 10-year follow-up results of ALPINA cementless hydroxyapatite-coated anatomic unicompartmental knee arthroplasty. Eur J Orthop Surg Traumatol. 2014;24(3):385. doi: 10.1007/s00590-013-1192-3. [DOI] [PubMed] [Google Scholar]
- 50.Epinette J.A., Manley M.T. Is hydroxyapatite a reliable fixation option in unicompartmental knee arthroplasty? A 5- to 13-year experience with the hydroxyapatite-coated unix prosthesis. J Knee Surg. 2008;21(4):299. doi: 10.1055/s-0030-1247836. [DOI] [PubMed] [Google Scholar]
- 51.Hall M.J., Connell D.A., Morris H.G. Medium to long-term results of the UNIX uncemented unicompartmental knee replacement. Knee. 2013;20(5):328. doi: 10.1016/j.knee.2012.09.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.