Abstract
This study aimed to evaluate the relationship between weather factors (temperature, humidity, solar radiation, wind speed, and rainfall) and COVID-19 infection in the State of Rio de Janeiro, Brazil. Solar radiation showed a strong (−0.609, p < 0.01) negative correlation with the incidence of novel coronavirus (SARS-CoV-2). Temperature (maximum and average) and wind speed showed negative correlation (p < 0.01). Therefore, in this studied tropical state, high solar radiation can be indicated as the main climatic factor that suppress the spread of COVID-19. High temperatures, and wind speed also are potential factors. Therefore, the findings of this study show the ability to improve the organizational system of strategies to combat the pandemic in the State of Rio de Janeiro, Brazil, and other tropical countries around the word.
Keywords: SARS-CoV-2, Coronavirus, Tropical temperature, Solar radiation, Wind speed
Highlights
-
•
Weather factors play an important role in the pandemic.
-
•
High solar radiation can reduce the spread of COVID-19.
-
•
SARS-CoV-2 incidence can be reduced with high temperatures and wind speed.
-
•
Climatic factors studies contribute to pandemic understanding and control.
1. Introduction
In December 2019, an outbreak of coronavirus disease 2019 (COVID-19) broke out in Wuhan, China (Xu et al., 2020). The novel coronavirus, severe acute respiratory disease coronavirus 2 (SARS-CoV-2), is the seventh known to cause human disease (Cui et al., 2019; Zhu et al., 2020). The spread of the disease achieved a global scale quickly, and as of March 11, 2020, the world health organization declared COVID-19 as a pandemic (WHO, 2020). The virus is highly transmissible, and cases of COVID-19 have already been reported in 185 countries (Dong et al., 2020). However, the new dynamics of the outbreaks seem highly variable amongst countries (Dong et al., 2020). The course of an epidemic is defined by several factors, including demographic and environmental, many of which have an unknown correlation for COVID-19 (Anderson et al., 2020). Among the extra-human factors, climatic factors can play an important role in the spread of the coronavirus, which makes it crucial to understand the drivers of the disease spread, as they are vital to guide the imposition of restrictive measures.
Environmental conditions are known to have an impact on the transmission and survival of viruses responsible for respiratory diseases such as influenza and SARS viruses (Tamerius et al., 2013; Yuan et al., 2006). Further, conditions as temperature, air humidity, and air pollution vary among the different countries affected by the pandemic. In Brazil, the number of COVID-19 cases has reached 55,995 cases. Only in the city of Rio de Janeiro, the number of cases was 6,828 on April 26, 2020, according to the Secretariat of Health of the Government of the State of Rio de Janeiro (SHGRJ, 2020). The early stages of the epidemics in Brazil happened during March as the country as in the summer. With the following changes in the seasons towards more temperate weather, it is of pivotal importance to know the role of environmental conditions in the transmission of the virus to raise awareness on the prevention of disease spread. Therefore, this paper evaluated the relationship between weather and COVID-19 in Rio de Janeiro, Brazil.
2. Methods
2.1. Study area
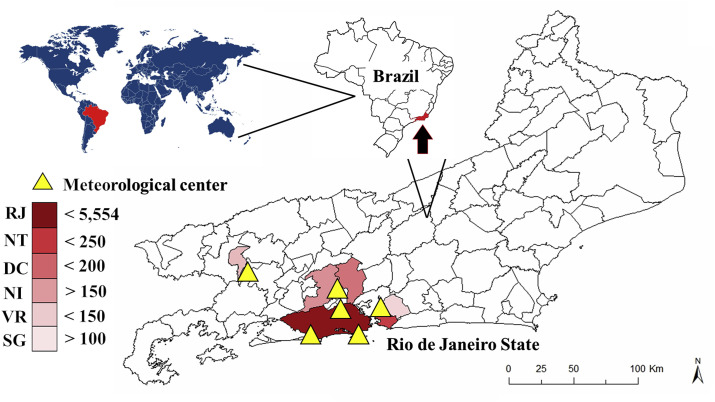
The Rio de Janeiro state consists of an area of 43,750,423 km2 and a population 17,264,943 in 2019 with data projection of the 2010 population census (IBGE, 2020) and a total of 92 cities. The weather is tropical and with high temperatures summers (humid air) and mild temperatures winters (dry air). Six cities were selected (Table 1 ) in this study, representing 59.8% of the total population of the state.
Table 1.
Geographic and epidemiologic information of the six cities studied in Rio de Janeiro state, Brazil.
| City | Latitude and longitude | Area (km2) | Population | Cases of the COVID-19 |
|---|---|---|---|---|
| Rio de Janeiro | −22.921474, −43.196084 | 1,200.3 | 6,718,903 | 5,554 |
| Niterói | −22.889506, −43.118780 | 133.8 | 513,584 | 282 |
| Duque de Caxias | −22.789661, −43.308106 | 467.1 | 919,596 | 337 |
| Nova Iguaçu | −22.760855, −43.456078 | 520.8 | 821,128 | 196 |
| Volta Redonda | −22.512245, −44.090516 | 182.1 | 273,012 | 202 |
| São Gonçalo | −22.823642, −43.046810 | 248.2 | 1,084,839 | 218 |
According IBGE (2020) and SHGRJ (2020).
2.2. Data collection
The number of cases of the COVID-19 was collected from the database of the Secretariat of Health of the Government of the State of Rio de Janeiro (SHGRJ, 2020). The six cities in the state of Rio de Janeiro, with the highest number of cases in COVID-19, were selected for this study. Infection data were collected after March 12, 2020, the date on which local transmission between people started. The sum of the number of cases in these cities represents 79.8% (6,789 cases) of the total number of positives (8,504 cases) on April 28, 2020.
The meteorological data were obtained from six monitoring centers of the National Institute of Meteorology (INMET, 2020) located in the cities studied: Forte de Copacabana, Jacarépagua, Marambaia, Niterói, Vila Militar and Rio Claro (Passa Três) (Fig. 1 ). Data were collected after March 6, 2020. Due to the delay between infection and diagnosis, the initial collection date was equivalent to six days prior to the first day of collection of the COVID-19 case number. The data consist of temperature maximum (°C), temperature minimum (°C), temperature average (°C), solar radiation (kJ/m2), relative humidity (%), wind speed (m/s) and Rainfall (mm).
Fig. 1.
Geographic patterns of COVID-19 confirmed case counts in six cities of Rio de Janeiro State in Brazil, on April 28, 2020. RJ: Rio de Janeiro city, NT: Niterói, DC: Duque de Caxias, NI: Nova Iguaçu, VR: Volta Redonda, SG: São Gonçalo.
2.3. Statistical analysis
Shapiro Wilk's test was applied to evaluate the normality of the data. The data on daily cases of the COVID-19 showed non-normal distribution, so the relationship between weather and COVID-19 incidence was studied using the Spearman rank correlation test. A descriptive study of the data was performed using the median and quartiles represented by a box-plot graph. The arithmetic mean was used to obtain a single and representative data set for the six meteorological centers per day. Statistica 12® (Statsoft, Tulsa, OK, USA) software and the significance level of 0.01 were used.
3. Results
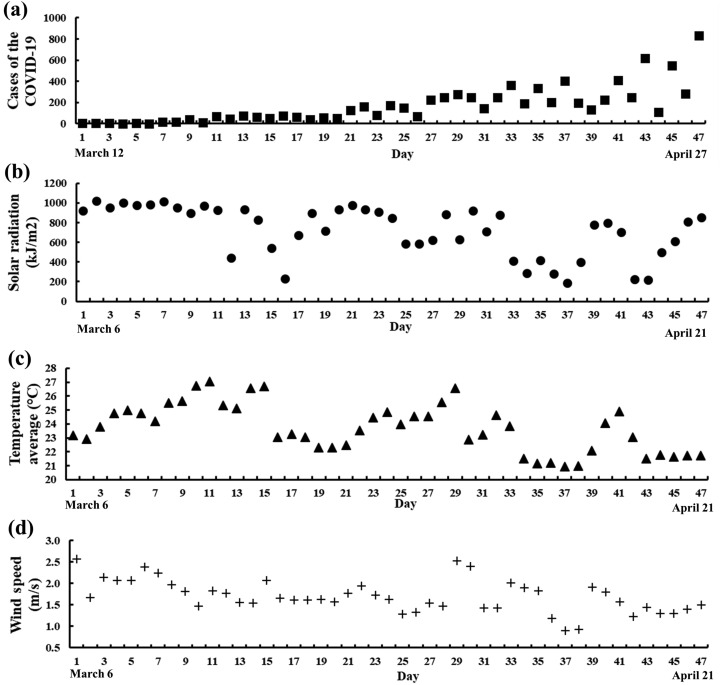
Table 1 contains the number of COVID-19 cases per city and Fig. 2 a shows the number of cases over time. The spread of COVID-19 began slowly in the State of Rio de Janeiro with 14 days to reach a lower value of 50 cases, after March 5, 2020, the day of occurrence of the first case (Fig. 2). However, with an additional 14 days (28 days after the first case), the exponential growth became evident, with nearly 1,000 confirmed cases. The latest epidemiological data describes a total of 6,828 on April 26, 2020, cases statewide. During the 47 days evaluated in this study, the climatic data presented highest temperature maximum of 34.2 °C (with the lowest temperature maximum of 23.1 °C), the highest minimum temperature of 23.9 °C (with the lowest minimum temperature of 16.9 °C), the highest average temperature of 27.0 °C (with the lowest average temperature of 20.9 °C), the highest humidity of 90.8% (with the lowest humidity of 69.5%), and the highest rainfall of 1.6 mm (with the lowest of 0 mm), the highest solar radiation of 1,017.6 kJ/m2 (with the lowest of 189.2 kJ/m2) and the highest wind speed of 2.6 m/s (with the lowest of 0.9 m/s).
Fig. 2.
Cases of the COVID-19 (a), solar radiation (kJ/m2) (b), temperature average (°C) (c), and wind speed (m/s) (d) in Rio de Janeiro (average of six meteorological centers) between March 06, 2020 and April 21, 2020.
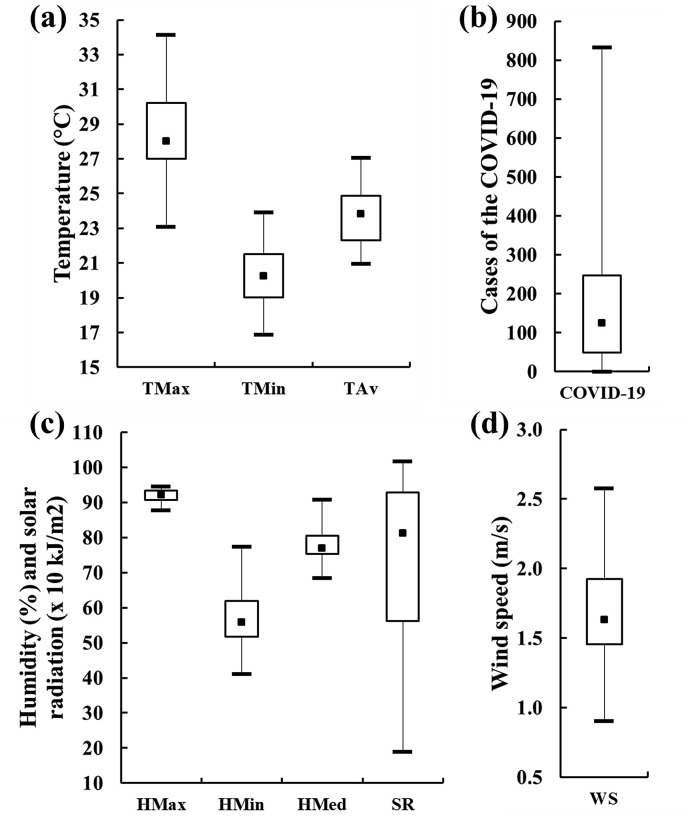
Descriptive analysis indicates that the maximum temperature has a high proportion of high values and showed more considerable variability among temperatures (Fig. 3 a). Concerning COVID-19 cases, greater variability in data is already expected as the disease spread progress exponentially. The maximum humidity showed high data homogeneity. Solar radiation showed a high amount of low values indicated by the prolongation of the third and fourth quartiles (Fig. 3c). Higher wind speeds were more frequent.
Fig. 3.
Box-plot of the weather conditions in Rio de Janeiro State for 47 days. TMAx: temperature maximum (°C), TMin: temperature minimum (°C) and TAv: temperature average (°C) (a). HMax: humidity maximum (%), HMin: humidity minimum (%), HMed: humidity average (%) and SR: solar radiation ( × 10 kJ/m2) (c). WS: wind speed (m/s) (d).
The correlation coefficients are shown in Table 2 . Between nine climatic factors studied, four were significant (temperature maximum and average, radiation and wind speed). In addition, all significative variables show a negative correlation with the number of cases. Evans (1996) classified the correlation levels at 0.00–0.19 as “very weak”, 0.20–0.39 “weak”, 0.40–0.59 “moderate”, 0.60–0.79 “strong” and 0.80–1.0 “very strong”. Hence, solar radiation showed a strong negative correlation with COVID-19. Wind speed and temperature average presented a negative moderate correlation, and temperature maximum a weak negative correlation.
Table 2.
The correlation coefficients of the Spearman rank test between COVID-19 and weather variables.
| Weather variables | Spearman correlation coefficient |
|---|---|
| Temperature maximum (°C) | −0.332a |
| Temperature minimum (°C) | −0.243 |
| Temperature average (°C) | −0.406a |
| Humidity maximum (%) | 0.174 |
| Humidity minimum (%) | 0.112 |
| Humidity average (%) | 0.265 |
| Rainfall (mm) | 0.127 |
| Solar radiation (kJ/m2) | −0.609a |
| Wind speed (m/s) | −0.440a |
Significative value (p < 0.01).
4. Discussion
The behavior of an enveloped virus is affected by extra-human conditions, such as climatic conditions (Cohen, 2020). In this study, solar radiation plays an important role in the propagation of COVID-19 in Brazil. In Iran, Ahmadi et al. (2020) found that radiation was inversely related to COVID-19 infection, using a linear correlation tool (Pearson's correlation). However, it was not significant (p > 0.05). In the present study, the relationship between these two variables was inverse and significative (p < 0.01). A non-linear correlation tool (Spearman rank correlation) was used to analyze the data from Rio de Janeiro. Therefore, although Iran (an arid or semi-arid and subtropical country) presented approximately twice more solar radiation in a similar period to Rio de Janeiro (Ahmadi et al., 2020), radiation can be effective in lower conditions in Brazil. Hence, it is possible to suggest that the increase in the doses of solar radiation may collaborate with the virus reduction in the environment of a tropical region in a non-linear way. On the other hand, vitamin D production by human metabolism may be an underlying connection linked to the interpretations described above. Solar radiation plays an important role in vitamin D production, and scientific evidence supports the role of this compound in preventing COVID-19 infections (Grant et al., 2020).
Among weather features, the influence of temperature has been the most studied (Tosepu et al., 2020; Liu et al., 2020; Prata et al., 2020). In this study, temperature (average and maximum) was associated (p < 0.01) with lower number of COVID-19 infection. High temperatures damage the virus lipid layer decreasing its stability and infection potential and may even cause virus inactivation, therefore lowering the transmission rate (Moriyama et al., 2020; Solá et al., 2020). In a survival test, Prussin II et al. (2018), using an enveloped virus, suggested as “equivalent to influenza and coronavirus” (bacteriophage Phi6), verified the temperature effect on the virus inactivation. The increase from 14 to 34 °C caused the 6-log reduction of the microorganism studied (Prussin II et al., 2018). The previous findings corroborate with the significant and negative correlation found for temperature (average and maximum) and the number of cases in Rio de Janeiro.
The wind was implied as a critical climatic factor for the transmission of COVID-19; however, studies on this factor are scarce (She et al., 2020). Yuan et al. (2006) found that wind speed was a significate factor for the SARS-CoV outbreak in Beijing, China. In Rio de Janeiro, higher speed winds were associated with lower incidences of COVID-19, due to the significative (p < 0.01) negative correlation (Table 2). In an external environment, higher wind speed contributes to the dilution and removal of the droplets that decrease the concentration of the virus in the air, thus reducing the transmission potential of the SARS (WHO, 2003; Cai et al., 2007). Indeed, studies are suggesting that the concentration of atmospheric pollutants is an important contributor to SARS-CoV-2 spread (Martelletti and Martelletti, 2020; Ogen, 2020). In an internal environment, Jiang et al. (2003) found that higher wind speeds decrease the viral load of indoor environments, which can prevent SARS outbreaks. In addition, we suggest that the wind renew the air and also increase the exposure of the virus to the solar radiation effects, a factor of strong negative correlation in the present study.
The understanding obtained in this study of the climatic effect on the spread of coronavirus in a tropical state such as Rio Janeiro can collaborate with the decision-making process to control the pandemic, indicating the locations with weather more susceptible to the disease spreading. In addition, it is noteworthy that, currently, the Northern Hemisphere is on its way to summer, a time when COVID-19 may lose strength due to climatic effects. However, the Southern Hemisphere is close to entering winter, where climatic factors increase the spread of the virus. This study demonstrates the association of COVID-19 with climatic characteristics in an alarming way for tropical regions of the Southern Hemisphere. Unlike the other countries of the Northern Hemisphere, it is predicted that Brazil will enter the winter near the major epidemic stage. Hence, considering the climatic conditions, there is a high potential for Brazil to be the main country affected by COVID-19, mainly also due to its high population density. Worldwide, the growth in the number of COVID-19 cases is a highly non-linear process, where each day of inertia results in a significant impact on future health and economic prospects. Just a few inert days down the road can mean the difference between a controllable process and an inevitably overburdened health system. Furthermore, in times of urgency, even the most straightforward study can be very advanced, and small gaps between different fields of research may appear to be precipices.
5. Conclusion
The weather plays a critical role in the spread of COVID-19 in Rio de Janeiro, Brazil. Solar radiation was the most critical weather factor, presenting a significantly strong correlation with the incidence of COVID-19. Notwithstanding, temperature average and wind speed showed moderate correlation. In general, temperature, wind speed, and solar radiation increases are potential climatic factors that gradually reduce the effects of the pandemic in Rio de Janeiro. Finally, our findings have the potential to collaborate with strategies to suppress the SAR-CoV-2 epidemic in an important tropical region of Brazil and other tropical countries around the world.
Declaration of competing interest
The authors declared no conflict of interests.
Acknowledgments
The authors are thankful for the financial support provided by the Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ), grant number [E-26/203.049/2017, E-26/010.000148/2020], and the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), grant number [311422/2016-0, 140947/2019-1]. This study was partially financed by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES, Brazil)—Finance Code 001.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijheh.2020.113587.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Ahmadi M., Sharifi A., Dorosti S., Ghoushchi S.J., Ghanbari N. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci. Total Environ. 2020:138705. doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Q.C., Lu J., Xu Q.F., Guo Q., Xu D.Z., Sun Q.W., Yang H., Zhao G.M., Jiang Q.W. Influence of meteorological factors and air pollution on the outbreak of severe acute respiratory syndrome. Publ. Health. 2007;121:258–265. doi: 10.1016/j.puhe.2006.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Sick time. Science. 2020;367:1294–1297. doi: 10.1126/science.367.6484.1294. [DOI] [PubMed] [Google Scholar]
- Cui J., Li F., Shi Z.-L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 2019;17:181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;19 doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans J.D. Brooks/Cole Publishing; Pacific Grove, CA: 1996. Straightforward Statistics for the Behavioral Sciences. [Google Scholar]
- Grant W.B., Lahore H., McDonnell S.L., Baggerly C.A., French C.B., Aliano J.L., Bhattoa H.P. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020;12:988. doi: 10.3390/nu12040988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBGE Instituto Brasileiro de Geografia e Estatística Panorama Rio de Janeiro. 2020. https://cidades.ibge.gov.br/brasil/rj/rio-de-janeiro/panorama (accessed 29.04.20)
- INMET Instituto Nacional de Meteorologia 2020. http://www.inmet.gov.br/portal/index.php?r=estacoes/estacoesAutomaticas (accessed 29.04.20)
- Jiang S., Huang L., Chen X., Wang J., Wu W., Yin S., Chen W., Zhan J., Yan L., Ma L., Li J., Huang Z. Ventilation of wards and nosocomial outbreak of severe acute respiratory syndrome among healthcare workers. Chin. Med. J. 2003;116:1293–1297. [PubMed] [Google Scholar]
- Liu J., Zhou J., Yao J., Zhang X., Li L., Xu X., He X., Wang B., Fu S., Niu T., Yan J., Shi Y., Ren X., Niu J., Zhu W., Li S., Luo B., Zhang K. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726:138513. doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martelletti L., Martelletti P. Air pollution and the novel covid-19 disease: a putative disease risk factor. Sn compr. Clin. Med. 2020:1–5. doi: 10.1007/s42399-020-00274-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriyama M., Hugentobler W.J., Iwasaki A. Seasonality of respiratory viral infections. Annu. Rev. Virol. 2020;7 doi: 10.1146/annurev-virology-012420-022445. [DOI] [PubMed] [Google Scholar]
- Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Sci. Total Environ. 2020;726:138605. doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata D.N., Rodrigues W., Bermejo P.H. Temperature significantly changes COVID-19 transmission in (sub)tropical cities of Brazil. Sci. Total Environ. 2020:138862. doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prussin A.J., Schwake D.O., Lin K., Gallagher D.L., Buttling L., Marr L.C. Survival of the enveloped virus Phi6 in droplets as a function of relative humidity, absolute humidity, and temperature. Appl. Environ. Microbiol. 2018;84 doi: 10.1128/AEM.00551-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- She J., Jiang J., Ye L., Hu L., Bai C., Song Y. 2019 novel coronavirus of pneumonia in Wuhan, China: emerging attack and management strategies. Clin. Transl. Med. 2020;9:19. doi: 10.1186/s40169-020-00271-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SHGRJ Secretariat of Health of the Government Painel coronavirus COVID-19. 2020. http://painel.saude.rj.gov.br/monitoramento/covid19.html (accessed 29.04.20)
- Solá D.E. de Á., Wang L., Vázquez M., Lázaro P.A.M. n.d. Weathering the pandemic: How the Caribbean Basin can use viral and environmental patterns to predict, prepare and respond to COVID-19. J. Med. Virol. 2020 doi: 10.1002/jmv.25864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamerius J.D., Shaman J., Alonso W.J., Bloom-Feshbach K., Uejio C.K., Comrie A., Viboud C. Environmental predictors of seasonal influenza epidemics across temperate and tropical climates. PLoS Pathog. 2013;9 doi: 10.1371/journal.ppat.1003194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tosepu R., Gunawan J., Effendy D.S., Ahmad L.O.A.I., Lestari H., Bahar H., Asfian P. Correlation between weather and covid-19 pandemic in jakarta, Indonesia. Sci. Total Environ. 2020;725:138436. doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Consensus document on the epidemiology of severe acute respiratory syndrome (SARS) 2003. http://www.who.int/csr/sars/WHOconsensus.pdf (accessed 29.04.20)
- World Health Organization WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed 29.04.20)
- Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L., Tai Y., Bai C., Gao T., Song J., Xia P., Dong J., Zhao J., Wang F.-S. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan J., Yun H., Lan W., Wang W., Sullivan S.G., Jia S., Bittles A.H. A climatologic investigation of the SARS-CoV outbreak in Beijing, China. Am. J. Infect. Contr. 2006;34:234–236. doi: 10.1016/j.ajic.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.