Abstract
Lockdown due to the Coronavirus disease 2019 (COVID 19) pandemic may cause weight gain and enhance the risk of type 2 diabetes mellitus (T2DM). We aimed to determine this risk in apparently non-diabetic individuals.
Material methods
Baseline demographic and clinical data from 100 apparently non-diabetic household members (related or unrelated) of patients with type 2 diabetes mellitus were collected until 49 days of lockdown and analyzed using the XL-STAT statistical software. A two-pronged analytical strategy was employed. First, the metabolic risk profile related to age, sex, weight, family history, and exercise pattern was analyzed. This was followed by an assessment of the risk of developing type 2 diabetes using an established risk assessment engine.
Results
There was a trend towards weight gain seen in 40% of the cohort, with 16% of the population experiencing a 2.1–5 kg weight increment. When all the risk parameters were analyzed together using the ADA risk engine, there was an increase in the ADA diabetes risk score in 7% of the population, with 6.66% in the high-risk group. There was a further increase in weight among 3% of the population who were already obese at baseline.
Conclusion
We show an increased risk of T2MD consequent to weight gain during 49 days of lockdown in India.
Keywords: Lockdown, Weight, Type 2 diabetes, Risk factor
Highlights
-
•
The impact of lockdown on weight gain and the risk of developing type 2 diabetes (T2DM) is unknown.
-
•
This is the first data to document a 40% increase in weight and a 6.66% increase in T2DM risk over a 49 days lockdown period.
-
•
The at-risk individuals must be encouraged to exercise regularly and lose weight.
1. Introduction
A lockdown implemented for the COVID-19 (Coronavirus disease 2019) pandemic caused by SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) [1,2] may have slowed the progression of the disease but has caused restriction of movement, resulting in decreased exercise and also dietary indiscretion in patients with type 2 diabetes [3,4]. We have previously reported the impact of this lockdown on worsening of glycated hemoglobin (HBA1c) and the associated complications in type 2 diabetes mellitus(T2DM) [5], probably due to the restriction of movement, limited exercise, improper diet, and psychological stress [6]. Lack of exercise and improper diet caused by poor availability of healthy food may lead to significant weight gain. It is important to note that patients with COVID 19 and obesity are associated with worse in-hospital outcomes. Both mortality rates and the requirement for mechanical ventilation are increased in the presence of obesity in patients diagnosed with COVID-19 [7,8].
While we have generated data on patients with type 2 diabetes, there is a paucity of data in an apparently non-diabetic population. There are indications of unhealthy weight gain, especially in children because of imposed restrictions, akin to weight gain seen during summer recess [9].It is important to gather such data in non-diabetic adults to assess their risk of developing T2DM and other co-morbidities associated with it. This is especially important for Asian Indians where the rate of conversion to T2DM from the prediabetes state is higher than whites [10]. Such increment in the number of patients with diabetes in India would be catastrophic because of further addition to a large pool of patients.
This analysis was therefore undertaken to estimate the risk of diabetes due to lockdown.
2. Materials and methods
Baseline demographic and clinical examination parameters were collected online from 100 household members of T2D patients registered in tertiary care diabetes centre between 42 and 49 days during lockdown. Telephonic interviews were conducted by a trained diabetes educator on a pre-designed questionnaire from people in a household of a known patient with T2DM under our follow up. The total interview time was 3–5 min. No individual refused this interview when approached. Importantly, none of the individuals had any documented history of T2D.
Data prior to lockdown and 49 days post-lockdown were collected in a file in comma separated values (CSV) format. A two-prong analytical strategy was undertaken. The first phase involved performing a simple demographic analysis looking into individual risk parameters. The second phase involved analyzing the impact of lockdown on weight as well as on the risk of developing T2D. The risk of developing diabetes was based on the validated American Diabetes Association risk score(Table 1 ). The components of the risk score were age, sex, history of gestational diabetes or any first degree relative with diabetes, self-reported hypertension, self-reported physical activity, and BMI. Each of these variables was identified using a value (score). A combined score ≥5 is considered a significant risk for T2D and should undergo screening for the same. Analysis was performed using the XL-STAT statistical software (Windows 10, 64 bits, USA).
Table 1.
American Diabetes Association diabetes risk calculator with scores [11].
| Attributes | Score | |
|---|---|---|
| Age (Years) | <40 | 0 |
| 40–49 | 1 | |
| 50–59 | 2 | |
| ≥60 | 3 | |
| Gender | Female | 0 |
| Male | 1 | |
| First degree relative with diabetes | No | 0 |
| Yes | 1 | |
| Hypertension | No | 0 |
| Yes | 1 | |
| Physically active | No | 0 |
| Yes | −1 | |
| BMI (kg/m2) | <25 | 0 |
| 25–30 | 1 | |
| 30–40 | 2 | |
| ≥40 | 3 | |
Score ≥5 is an indication for diabetes screening.
3. Results
Data from the hundred healthy individuals were analyzed in a sequential fashion. This was a single-centre data collection electronically.
3.1. Core analysis - weight and diabetes risk score
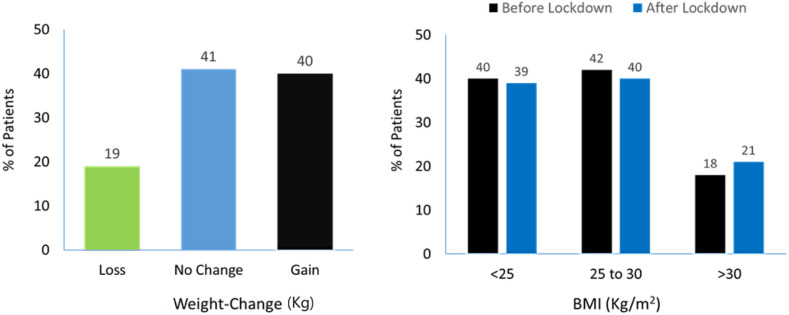
There was a 0.1kg-5.0 kg increase in weight in 40% of individuals (Fig. 1 ). In 16% of the recruited population, weight gain was in the range of 2.1–5.0 kg. Weight remained unchanged in 41% of the population, and there was a varying degree of weight loss in 19% of individuals (Fig. 1). The risk score for diabetes was calculated using BMI. In 7% of the population, the diabetes risk score increased from baseline, while in 90% it remained unchanged (Fig. 2 ). In 3% of the population, the risk score decreased. The chance of crossing the total score of 5 and hence a higher risk of developing T2D was 6.66% (Table 2 ).
Fig. 1.
Weight and BMI changes pre- and post-lockdown. BMI: Body mass index.
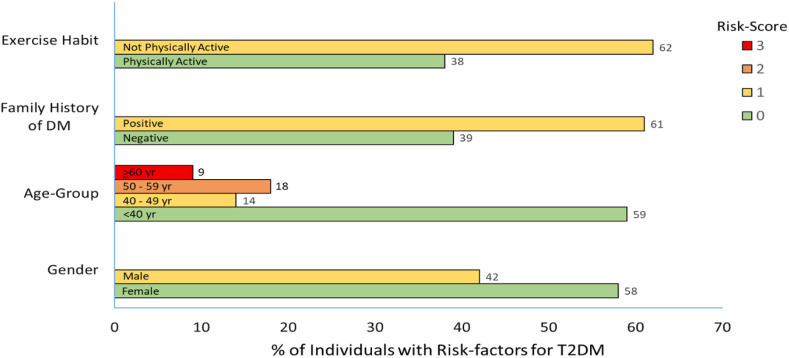
Fig. 2.
Baseline demographics of household members of T2D patients included for analysis showing percentage of risk factors for T2DM. Numbers 0,1,2, and 3 indicate cores for the individual attributes (see Table 1).
Table 2.
Summary of weight and diabetes risk score data (pre- and post-lockdown). BMI: Body mass index, ADA: American Diabetes Association.
| Attributes | Baseline | Change post-lockdown(count) | Change post-lockdown (%) |
|---|---|---|---|
| Weight gain (0.1–5.0 kg) | 40 | 40 | |
| Weight gain (2.1–5.0 kg) | 16 | 16 | |
| BMI (<25 kg/m2) | 40 | 39 | −1 |
| BMI (25–30 kg/m2) | 42 | 40 | −2 |
| BMI (30-<40 kg/m2) | 18 | 21 | 3 |
| Any increase in ADA risk score | 7 | 7 | |
| ADA risk score ≥5 | 15 | 16 | 6.66 |
3.2. Risk-based demographics
The individuals recruited for this analysis were predominantly young (59% were below 40 years of age) and of the female gender (58%) (Fig. 2). Males were at a higher risk for T2DM than females. Individuals below the age of 40 years had no risk. But age above 40 years was associated with an increased risk of T2DM per decade. Individuals who were at or above 60 years of age, comprising 9% of the population, were at the highest risk (designated with a risk score of 3). A history of T2D in first-degree relatives was present in 61% of the population, also considered at risk (score of 1) in comparison to those who did not (Fig. 2). Only 38% of the individuals exercised for at least 3 days a week, with 62% in this group at risk of developing T2D (score of 1). 60% of this group was obese at baseline. During 49 days of lockdown, 40% of the cohort gained weight, with 16% gaining between 2.0 and 5.0 kg in weight. At baseline, 18% of individuals had a BMI greater than 30 kg/m2. After 49 days of lockdown, 21% of individuals had a BMI greater than 30 kg/m2, indicating a 3% increase (Fig. 2).
4. Discussion
4.1. What we already know about weight gain and its metabolic impact
In this study, we show an increased risk for the development of T2DM in apparently non-diabetic individuals, predominantly ascribed to weight gain during the COVID19 pandemic. Weight gain hold paramount importance in any individual, but more so in the current era. First, it increases the risk of T2DM, hypertension, and dyslipidemia. Furthermore, it increases the mortality risk from COVID19. Previously, there has been no research focusing on the enhanced risk of diabetes during lockdown. This is particularly important for India because Asian Indians have a heightened propensity to develop T2DM [12].
We have adequate data implicating weight gain as a significant factor for the development of metabolic disorders. Weight gain in the background of obesity results in the expansion of visceral fat resulting in activation of inflammatory response in adipocytes [13]. There is also an inverse relationship between body mass index and brown adipose tissue (BAT). An increase in BMI from baseline results in a decrease in BAT and a consequent increase in white adipose tissues (WAT) responsible for worsening of insulin resistance and its associated metabolic complications. In another study, our group showed a marked decrease in physical activity and increased intake of carbohydrates and snacking, all reasons that could add to weight gain and destabilize metabolism [14]. Further, Ford et al. [15] documented that a 5 kg weight gain from baseline could result in a 27% increased risk of developing T2D. In addition, gaining weight on the background of preexisting obesity could increase the risk of T2DM by a further 26.2%, indicating that the risk of T2D increases continuously per every kilogram of weight gained [15]. The adverse impact of weight gain in this study was documented in 8545 US adults followed up for a period of 10 years. In addition, there is robust evidence illustrating weight loss as an effective means of preventing T2DM from a pre-diabetic stage. Collectively, this information accentuates the need to aggressively pursue weight control to prevent T2D [16].
As stated previously, our analysis was the first in India and globally to document the impact of externally imposed restrictive lifestyle on weight and the effects of weight gain on the risk of developing T2D. Our findings indicate an immediate need to address this important aspect of diabetes risk, as an additional 6.66% increase in high-risk diabetes score could add substantially to patients with T2DM and increase the burden of complications, spelling disastrous consequences to the health and beleaguered economy of nation [17]. In addition, we can also expect an increase in other weight gain-related morbidities, hypertension, dyslipidemia, and cardiovascular disease further exacerbating the epidemic of non-communicable diseases in India. For the present cohort, since these individuals were relatives of T2D patients registered in the recruiting clinic, based on their risk profile, blood glucose monitoring and assessment for T2D can be done in a phase-wise manner later.
4.2. Strengths of the study
In the absence of any evidence on the hypothesis being investigated, and the difficulty in collecting data in the current scenario, this is the first and the best available data. In addition, the baseline age and gender distribution in this cohort matches the demographics of our country, and thereby, some degree of generalization of the findings could be permitted. Finally, and most importantly, since the Indian diabetes risk score required measurement of waist circumference, which was not possible to conduct due to technical difficulties, the BMI cutoff was measured. This was higher than the Indian criteria, suggesting that our estimates are underestimated rather than overestimation of the scenario. This should be acceptable as a limitation because the risk of overestimation is a major challenge when analyzing smaller populations.
4.3. Limitations of the study
This was a single centre study and conducted in a tertiary centre; hence, its reproducibility should not be automatically assumed without larger, multi-centric studies. Moreover, diabetes risk assessment identifies those at-risk, not necessarily those with diabetes, and hence it should not be assumed that there was an increment in T2D prevalence. To provide conclusive evidence on this, risk assessment should be followed by blood glucose measurement; this was not done in our study. In addition, only a very small number of patients were studied, and this could have skewed the data. Finally, an Indian diabetes risk score would have been more appropriate instead of the ADA criteria, due to the difference in criteria for defining obesity based on BMI.
5. Conclusion
Weight gain is a very important determinant as far as the development or worsening of metabolic disorders are concerned. The lockdown implemented after the SARS-CoV-2 pandemic may negatively impact weight and predispose individuals to risk of metabolic decompensation. This analysis was the first to document weight gain over a period of 49 days post lockdown along with a tendency towards increased risk of developing type 2 diabetes.
Financial disclosure
None.
Declaration of competing interest
None to declare.
References
- 1.Zhang Y., Geng X., Tan Y., Li Q., Xu C., Xu J. New understanding of the damage of SARS-CoV-2 infection outside the respiratory system. Biomedicine & Pharmacology. 2020:127. doi: 10.1016/j.biopha.2020.110195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Losifidis C. The socio-economic implications of the coronavirus and COVID-19 pandemic: a review. Int J Surg. 2020 doi: 10.1155/2016/1216783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tobias A. Evaluation of the lockdowns for the SARS-CoV-2 epidemic in Italy and Spain after one month follow up. Sci Total Environ. 2020:725. doi: 10.1016/j.scitotenv.2020.138539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghosal S., Sinha B., Majumder M., Misra A. Estimation of effects of nationwide lockdown for containing coronavirus infection on worsening of glycosylated haemoglobin and increase in diabetes-related complications: a simulation model using multivariate regression analysis. Diabetes & Metabolic Syndrome: Clin Res Rev. 2020;14:319–323. doi: 10.1016/j.dsx.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang Y., Ma Z.M. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in liaoning province, China: a cross-sectional study. Int J Environ Res Publ Health. 2020;17(7):2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frühbeck G., Baker L.J., Busetto L., Dicker D., Goossens G.H., Halford J.C.G. European association for the study of obesity position statement on the global COVID-19 pandemic. Obes Facts. 2020;13:292–296. doi: 10.1159/000508082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Simonnet A., Chetboun M., Poissy J., Raverdy V., Noulette J., Duhamel A. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-Cov-2) requiring invasive mechanical ventilation. Obesity. 2020 doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rundle A.G., Park Y., Herbstman J.B., Kinsey E.W., Wang W.C. COVID-19–Related school closings and risk of weight gain among children. Obesity. 2020 doi: 10.1002/oby.22813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sattar N., Gill J.M. Type 2 diabetes in migrant south Asians: mechanisms, mitigation, and management. Lancet Diabetes Endocrinol. 2015;3(12):1004–1016. doi: 10.1016/S2213-8587(15)00326-5. [DOI] [PubMed] [Google Scholar]
- 11.Bang H., Edwards A.M., Bomback A.S., Ballantyne C.M., Brillon D., Callahan M.A. Development and validation of a patient self-assessment score for diabetes risk. Ann Intern Med. 2009;151(11):775–783. doi: 10.1059/0003-4819-151-11-200912010-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Misra A., Sattar N., Tandon N., Shrivastava U., Vikram N.K., Khunti K., Hills A.P. Clinical management of type 2 diabetes in south Asia. Lancet Diabetes Endocrinol. 2018 Dec;6(12):979–991. doi: 10.1016/S2213-8587(18)30199-2. [DOI] [PubMed] [Google Scholar]
- 13.Gómez-Hernández A., Beneit N., Díaz-Castroverde S., Escribano O. Differential Role of Adipose Tissues in Obesity and Related Metabolic and Vascular Complications. International Journal of Endocrinology. 2016;2016 doi: 10.1155/2016/1216783. Article ID. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ghosh A., Arora B., Gupta R., Anoop S., Misra A. Effects of nationwide lockdownduring COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in northIndia, Diabetes & Metabolic Syndrome. Clin Res Rev. 2020 doi: 10.1016/j.dsx.2020.05.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ford E.S., Williamson D.F., Liu S. Weight change and diabetes incidence: findings from a national cohort of US adults. Am J Epidemiol. 1997;146:214–222. doi: 10.1093/oxfordjournals.aje.a009256. [DOI] [PubMed] [Google Scholar]
- 16.Resnick H.E., Valsania P., Halter J.B., Lin X. Relation of weight gain and weight loss on subsequent diabetes risk in overweight adults. J Epidemiol Community Health. 2000;54:596–602. doi: 10.1136/jech.54.8.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shrivastava U., Misra A., Mohan V., Unnikrishnan R., Bachani D. Obesity, diabetes and cardiovascular diseases in India: public health challenges. Curr Diabetes Rev. 2017;13(1):65–80. doi: 10.2174/1573399812666160805153328. [DOI] [PubMed] [Google Scholar]