Abstract
This cross-sectional study investigates associations of residential building characteristics and markers of neighborhood socioeconomic status (SES) with screen-detected SARS-CoV-2 prevalence among pregnant women delivering in 2 New York City hospitals.
The built environment is associated with infectious disease dynamics, particularly in diseases transmitted by contact, aerosols, or droplets.1,2 A recent study of the ongoing severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic in New York revealed significant differences in hospitalization and death rates among the city’s boroughs, with the highest rates in Queens and the Bronx.3 To our knowledge, no studies have investigated associations between the built environment, markers of neighborhood socioeconomic status, and SARS-CoV-2 transmission. We leveraged a universal testing program for SARS-CoV-2 in pregnant women to examine associations between these factors and SARS-CoV-2 prevalence.
Methods
We conducted a cross-sectional study of New York City residents delivering at NewYork–Presbyterian/Columbia University Irving Medical Center or Allen Hospital after implementation of universal SARS-CoV-2 nasopharyngeal quantitative reverse transcriptase–polymerase chain reaction testing at the time of admission to the labor and delivery unit from March 22 through April 21, 2020. We linked patients to demographic and socioeconomic data from the US Census Bureau’s American Community Survey,4 a national survey with detailed demographic, socioeconomic, and housing data, and to real estate tax data from New York’s Department of City Planning.5 We abstracted building-level variables, including number of residential units per building and mean assessed value (per square foot), and neighborhood-level variables, including median household income, poverty rate, unemployment rate, population density, household membership (persons per household), and household crowding (percentage of households with >1 person per room). Neighborhood was defined using New York City neighborhood tabulation areas, which divide the city into 195 districts, with at least 15 000 residents each.4
We fit bivariable logistic regression models with cluster robust standard errors, modeling exposures as continuous independent variables. Because odds ratios (ORs) associated with a 1-unit change in independent variables can be difficult to interpret, we used these models both to estimate interdecile ORs—ie, the relative odds of SARS-CoV-2 infection for individuals at the 90th percentile of an independent variable relative to those at the 10th percentile—and to predict probabilities (and 95% CIs) of SARS-CoV-2 infection at the 10th and 90th percentiles of the independent variable distribution. Analysis was performed using Stata/MP version 16.0 (StataCorp). Two-sided P < .05 was considered significant. This study was exempted from informed consent and approved by the Columbia University institutional review board.
Results
We identified 434 New York City residents who were tested for SARS-CoV-2. Of the 396 patients (91%) linked to buildings and neighborhoods in the city, 71 (17.9%) were infected with SARS-CoV-2. Cohort characteristics are tabulated in the Table. The likelihood of SARS-CoV-2 varied substantially across measures of built environment and neighborhood socioeconomic status (Figure). The lowest probability of infection was estimated for women living in buildings with very high assessed values (8.2% [95% CI, 1.2%-15.2%]) and the highest was for those residing in neighborhoods with high household membership (23.9% [95% CI, 18.4%-29.4%]). Odds of infection were lower among women living in buildings with more residential units (interdecile OR, 0.34 [95% CI, 0.16-0.72]) and higher assessed values (interdecile OR, 0.29 [95% CI, 0.10-0.89]) and in neighborhoods with higher median incomes (interdecile OR, 0.32 [95% CI, 0.12-0.83]). Odds of infection were higher among women residing in neighborhoods with high unemployment rates (interdecile OR, 2.13 [95 CI, 1.18-3.83]), large household membership (interdecile OR, 3.16 [95% CI, 1.58-6.37]), and greater household crowding (interdecile OR, 2.27 [95% CI, 1.12-4.61]). There was no statistically significant association between SARS-CoV-2 infection and population density (interdecile OR, 0.70 [95% CI, 0.32-1.51]) or poverty rate (interdecile OR, 2.03 [95% CI, 0.97-4.25]). Neighborhood-level variables were moderately to highly correlated (r = 0.66-0.83).
Table. Cohort Characteristics.
| SARS-CoV-2 status | P value | ||
|---|---|---|---|
| Negative (n = 325) | Positive (n = 71) | ||
| Maternal age, median (IQR), y | 31.0 (27.0-35.0) | 27.0 (24.0-32.0) | <.001a |
| Gestational age, median (IQR), wk | 39.0 (38.1-39.7) | 39.0 (37.4-39.7) | .63a |
| Gravidity (IQR) | 2 (1-4) | 2 (1-3) | .04a |
| Parity (IQR) | 1 (0-1) | 0 (0-1) | .37a |
| Hypertension, No. (%)b | 26 (8.0) | 7 (9.9) | .61c |
| Diabetes, No. (%)b | 18 (5.5) | 2 (2.8) | .34c |
Abbreviations: IQR, interquartile range; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
P value based on linear regression with cluster robust standard errors.
Both pregestational and gestational conditions included.
P value based on logistic regression with cluster robust standard errors.
Figure. Built Environment and Neighborhood Socioeconomic Factors Associated With SARS-CoV-2 Infection Among Pregnant Women.
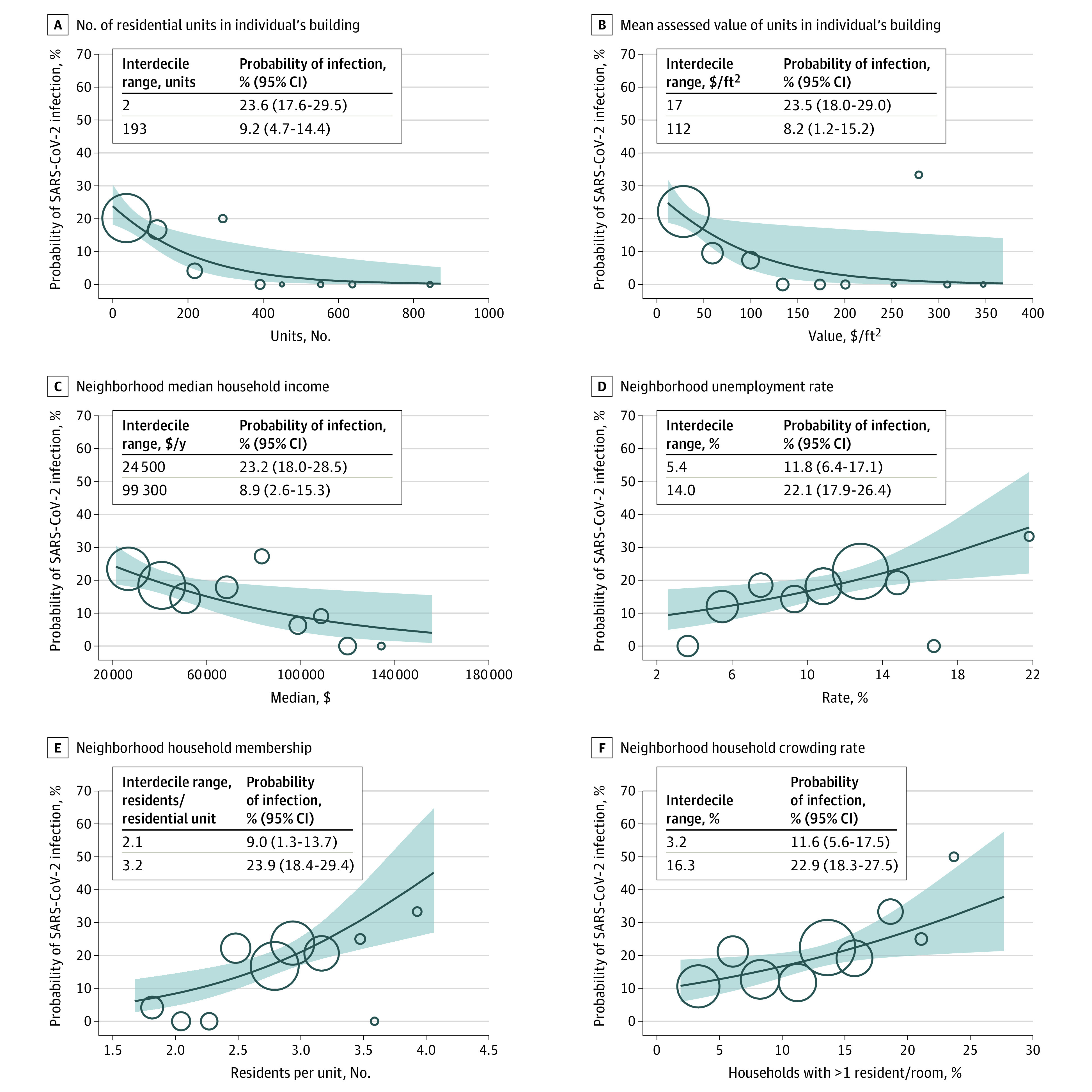
Values plotted against the probability of identifying severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection at universal testing. Solid lines indicate the predicted probability of infection from bivariable logistic regression models; shaded areas, 95% confidence bands. For each independent variable, circles are plotted at the mean values of the women residing in 10 equal-width bins. The circle size is proportionate to the number of women within each bin. Since bins may contain no patients, there are fewer than 10 circles in some panels. Interdecile range indicates 10th and 90th percentiles. The probability (and 95% CI) of SARS-CoV-2 infection for women at the 10th and 90th percentile of each independent variable was predicted from the regressions shown in each panel.
Discussion
In this study, SARS-CoV-2 transmission among pregnant women in New York City was associated with neighborhood- and building-level markers of large household membership, household crowding, and low socioeconomic status. These data may aid policy makers in the design of interventions to reduce the spread of SARS-CoV-2. A key strength of this study was the use of a universally tested population, which allowed for ascertainment of asymptomatic cases among a defined at-risk population. Limitations of the study include that the findings may not apply to other populations given the unique demographic, physiologic, and social features of pregnant women. Additionally, the small sample size and high degree of correlation between neighborhood-level variables precluded multivariable analysis. Nonetheless, this study provides empirical support for the hypothesis that variation in the urban environment may be an important social determinant of SARS-CoV-2 transmission.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Pinter-Wollman N, Jelić A, Wells NM. The impact of the built environment on health behaviours and disease transmission in social systems. Philos Trans R Soc Lond B Biol Sci. 2018;373(1753):20170245. doi: 10.1098/rstb.2017.0245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Virtanen M, Terho K, Oksanen T, et al. Patients with infectious diseases, overcrowding, and health in hospital staff. Arch Intern Med. 2011;171(14):1296-1298. doi: 10.1001/archinternmed.2011.313 [DOI] [PubMed] [Google Scholar]
- 3.Wadhera RK, Wadhera P, Gaba P, Figueroa JF, Joynt Maddox KE, Yeh RW, Shen C. Variation in COVID-19 hospitalizations and deaths across New York City boroughs. JAMA. 2020;323(21):2192-2195. doi: 10.1001/jama.2020.7197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Community Survey by neighborhood tabulation area. New York City Department of City Planning. Accessed May 6, 2020. https://www1.nyc.gov/site/planning/data-maps/open-data/dwn-acs-nta.page
- 5.PLUTO database. New York City Department of City Planning. Accessed May 6, 2020. https://www1.nyc.gov/site/planning/data-maps/open-data.page


