Abstract
This study characterizes the trends in rates of SARS-CoV-2 positive test results among individuals in the Baltimore–Washington, DC area by self-reported race/ethnicity.
The black community has been disproportionally affected by the coronavirus disease 2019 (COVID-19) pandemic in the US.1 Emerging data highlight sharp increases in cases within the Latino community.1,2 We analyzed temporal trends in positivity rates for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the Baltimore–Washington, DC region by race/ethnicity.
Methods
Samples were collected between March 11, 2020, and May 25, 2020, from 5 hospitals, including emergency departments, and 30 outpatient clinics that are part of the Johns Hopkins Health System (JHHS). SARS-CoV-2 testing inclusion criteria broadened over time (ie, initially high-risk individuals only and then all symptomatic patients) as local capacity increased but was standardized across JHHS sites. Samples collected via nasopharyngeal swabs were analyzed using SARS-CoV-2 reverse transcriptase–polymerase chain reaction. Data on patient demographics, comorbidities, SARS-CoV-2 status, and hospitalization were extracted from the integrated electronic health record system.
Patients self-identified race/ethnicity from fixed categories. Racial/ethnic groups were considered mutually exclusive; ie, Latinos were excluded from other groups (white, black, other) regardless of reported race. Those who self-reported American Indian, Alaska Native, Asian American, Native Hawaiian, Pacific Islander, or multiracial were grouped as “other.”
Temporal trends in daily positivity rates (7-day moving average; number positive/number tested over the date and preceding 6 days) and testing volumes stratified by race/ethnicity were evaluated. Total rates of SARS-CoV-2 positivity, hospitalization, and categorical patient characteristics were compared between Latinos and each racial/ethnic group using the χ2 test. Analysis of variance (ANOVA) was used to compare trends in positivity rates between groups. An omnibus ANOVA comparison with significance set at P < .05 was performed, followed by pairwise comparisons using the Latino group as reference, with correction for multiple comparisons (Tukey test). All analyses were performed with R version 3.6.2; a 2-sided P < .05 determined statistical significance. This work was deemed exempt by the Johns Hopkins Institutional Review Board, meeting criteria for quality improvement.
Results
A total of 6162 (16.3% [95% CI, 16.0%-16.7%]) of 37 727 patients tested positive for SARS-CoV-2. The positivity rate for Latino patients was 42.6% (95% CI, 41.1%-44.1%), significantly higher than the rate for white patients (8.8% [95% CI, 8.4%-9.2%]), black patients (17.6% [95% CI, 16.6%-18.3%]), or those of other race/ethnicity (17.2% [95% CI, 16.2%-18.3%]) (P < .001 for each pairwise comparison) (Table).
Table. Demographics of Patients Tested for SARS-CoV-2 at the Johns Hopkins Health Systema.
| Latino patients | White patients | P valueb | Black patients | P valueb | Patients of other race/ethnicity | P valueb | |
|---|---|---|---|---|---|---|---|
| Overall | |||||||
| Tested, No. | 4169 | 17 113 | 11 639 | 4806 | |||
| Positive, No. | 1776 | 1508 | 2050 | 828 | |||
| % of tested (95% CI) | 42.6 (41.1-44.1) | 8.8 (8.4-9.2) | <.001 | 17.6 (16.6-18.3) | <.001 | 17.2 (16.2-18.3) | <.001 |
| Female sex, No. | 821 | 762 | 1100 | 424 | |||
| % of positive (95% CI) | 46.2 (43.9-48.6) | 50.5 (48.0-53.0) | .02 | 53.7 (51.5-55.8) | <.001 | 51.2 (47.8-54.6) | .02 |
| Age, y | |||||||
| <18, No. | 97 | 25 | 44 | 26 | |||
| % of positive (95% CI) | 5.5 (4.5-6.6) | 1.7 (1.1-2.4) | <.001 | 2.1 (1.6-2.9) | <.001 | 3.1 (2.2-4.6) | .01 |
| 18-44, No. | 1092 | 422 | 586 | 323 | |||
| % of positive (95% CI) | 61.5 (59.2-63.7) | 28.0 (25.8-30.3) | <.001 | 28.6 (26.7-30.6) | <.001 | 39.0 (35.7-42.4) | <.001 |
| 45-64, No. | 487 | 443 | 855 | 243 | |||
| % of positive (95% CI) | 27.4 (25.4-29.5) | 29.4 (27.1-31.7) | .23 | 41.7 (39.6-43.9) | <.001 | 29.3 (26.3-32.5) | .33 |
| 65-74, No. | 70 | 264 | 334 | 101 | |||
| % of positive (95% CI) | 3.9 (3.1-5.0) | 17.5 (15.7-19.5) | <.001 | 16.3 (14.8-18.0) | <.001 | 12.2 (10.1-14.6) | <.001 |
| >74, No. | 30 | 354 | 231 | 135 | |||
| % of positive (95% CI) | 1.7 (1.2-2.4) | 23.5 (21.4-25.7) | <.001 | 11.3 (10.0-12.7) | <.001 | 16.3 (13.9-19.0) | <.001 |
| Admitted to the hospital | |||||||
| Patients, No. | 516 | 604 | 854 | 238 | |||
| % of positive (95% CI) | 29.1 (27.0-31.2) | 40.1 (37.6-42.5) | <.001 | 41.7 (39.5-43.8) | <.001 | 28.7 (25.8-31.9) | .91 |
| Female sex, No. | 181 | 274 | 385 | 115 | |||
| % of admitted (95% CI) | 35.1 (31.1-39.3) | 45.4 (41.4-49.4) | <.001 | 45.1 (41.8-48.4) | <.001 | 48.3 (42.0-54.6) | <.001 |
| Age, y | |||||||
| <18, No. | 15 | 2 | 5 | 6 | |||
| % of admitted (95% CI) | 2.9 (1.8-4.7) | 0.3 (0.1-1.2) | .001 | 0.6 (0.3-1.4) | .001 | 2.5 (1.2-5.4) | .95 |
| 18-44, No. | 223 | 79 | 112 | 43 | |||
| % of admitted (95% CI) | 43.2 (39.0-47.5) | 13.1 (10.6-16.0) | <.001 | 13.1 (11.0-15.5) | <.001 | 18.1 (13.7-23.4) | <.001 |
| 45-64, No. | 207 | 138 | 373 | 76 | |||
| % of admitted (95% CI) | 40.1 (36.0-44.4) | 22.8 (19.7-26.4) | <.001 | 43.7 (40.4-47.0) | .22 | 31.9 (26.3-38.1) | .04 |
| 65-74, No. | 50 | 137 | 207 | 50 | |||
| % of admitted (95% CI) | 9.7 (7.4-12.5) | 22.7 (19.5-26.2) | <.001 | 24.2 (21.5-27.2) | <.001 | 21.0 (16.3-26.6) | <.001 |
| >74, No. | 21 | 248 | 157 | 63 | |||
| % of admitted (95% CI) | 4.1 (2.7-6.1) | 41.1 (37.2-45.0) | <.001 | 18.4 (15.9-21.1) | <.001 | 26.5 (21.3-32.4) | <.001 |
| Comorbidities | |||||||
| Hypertension, No. | 231 | 425 | 703 | 174 | |||
| % of admitted (95% CI) | 44.8 (40.5-49.1) | 70.4 (66.6-73.9) | <.001 | 82.3 (79.6-84.7) | <.001 | 73.1 (67.1-78.3) | <.001 |
| CHF, No. | 212 | 342 | 479 | 96 | |||
| % of admitted (95% CI) | 41.1 (36.9-45.4) | 56.6 (52.6-60.5) | <.001 | 56.1 (52.7-59.4) | <.001 | 40.3 (34.3-46.7) | .91 |
| Diabetes, No. | 169 | 179 | 451 | 102 | |||
| % of admitted (95% CI) | 32.8 (28.8-36.9) | 29.6 (26.1-33.4) | .29 | 52.8 (49.5-56.1) | <.001 | 42.9 (36.7-49.2) | .01 |
| Pulmonary disease, No. | 107 | 205 | 281 | 53 | |||
| % of admitted (95% CI) | 20.7 (17.5-24.4) | 33.9 (30.3-37.8) | <.001 | 32.9 (29.8-36.1) | <.001 | 22.3 (17.4-28.0) | .70 |
| COPD, No. | 99 | 181 | 238 | 49 | |||
| % of admitted (95% CI) | 19.2 (16.0-22.8) | 30.0 (26.4-33.7) | <.001 | 27.9 (25.0-31.0) | <.001 | 20.6 (15.9-26.2) | .73 |
Abbreviations: CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Patients self-reported their race/ethnic group, and those who self-reported American Indian, Alaska Native, Asian American, Native Hawaiian, Pacific Islander, or multiracial were grouped as “other.”
P values were calculated from χ2 tests using the Latino patient group as reference for each pairwise comparison with a P < .05 threshold for significance. The 95% CIs for proportions were calculated using the Wilson score method without continuity correction.
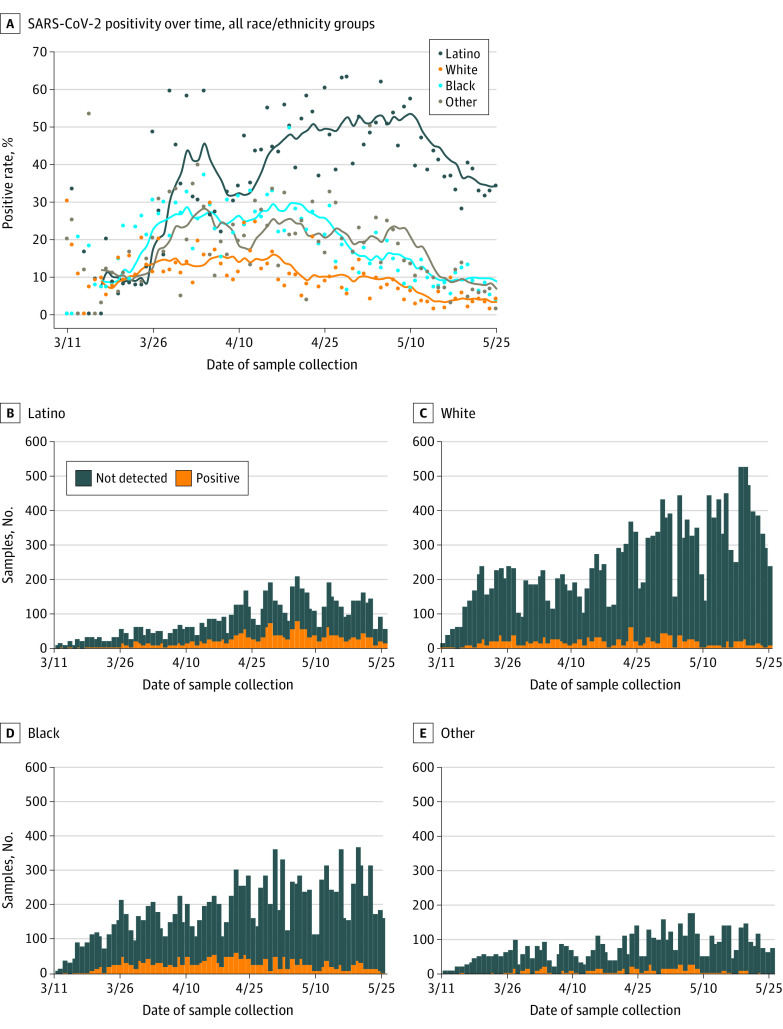
The daily positivity rate was higher for Latino patients than patients in the other racial/ethnic groups (P < .001 for each pairwise comparison; Figure, A). Moving average trends in positivity rate peaked later for Latino patients at 53.4% (95% CI, 49.6%-57.3%) on May 10, 2020, compared with white patients (16.1% [95% CI, 14.1%-18.3%]) on April 16, 2020, and black patients (29.6% [95% CI, 26.9%-32.6%]) on April 19, 2020. As testing volume increased over time for all racial/ethnic groups (Figure, B, C, D, and E), positivity rates declined (Figure, A).
Figure. SARS-CoV-2 Positivity Rate by Racial/Ethnic Groups in the Baltimore–Washington, DC Region, March 11 to May 25, 2020.
A, Daily positivity rates of SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) as points and 7-day moving averages (number positive/number tested over the plotted date and preceding 6 days) as solid lines by race/ethnicity. Statistically significant differences (P < .001) in daily positivity rates were evaluated across groups with 1-way analysis of variance (ANOVA). Multiple post hoc pairwise comparisons (Tukey test) of each group (black, white, other) to the Latino reference group also demonstrated significant differences (P < .001 for each pairwise comparison). B-E, Testing volume stratified by SARS-CoV-2 test result and grouped by race/ethnicity. This included an omnibus ANOVA comparison with significance (P < .05) resulting in correction for multiple pairwise comparisons using the Latino group as reference.
Among those who tested positive, 2212 (35.9% [95% CI, 34.7%-37.1%]) patients were admitted to a JHHS hospital. The admission rate was lower for Latino patients (29.1% [95% CI, 27.0%-31.2%]) than for white patients (40.1% [95% CI, 37.6%-42.5%]) or black patients (41.7% [95% CI, 39.5%-43.8%]) (P < .001 for each pairwise comparison) (Table). Hospitalized Latino patients were younger (a greater proportion aged 18-44 years), more likely to be male, and had lower rates of hypertension, congestive heart failure, pulmonary disease, and chronic obstructive pulmonary disease than white or black patients (P < .001 for each pairwise comparison) (Table).
Discussion
More than 40% of Latinos in the Baltimore–Washington, DC metropolitan region who were tested for SARS-CoV-2 were positive, a much higher proportion than for any other racial/ethnic group. While SARS-CoV-2 testing inclusion criteria were standardized, differential access to testing may have contributed to higher rates of positivity; Latino patients have historically demonstrated lower rates of insurance and health care utilization.3 However, an alternative explanation may be higher disease prevalence, with the spread of infection among Latinos driven by decreased opportunity for social distancing in the setting of dense housing and continued work engagement due to essential worker status and economic necessity.1,4,5
This study was limited to patients visiting JHHS, excluding those tested for SARS-CoV-2 elsewhere in the region. In addition, this study cannot determine whether differences in Latino patient SARS-CoV-2 positivity represent a higher disease prevalence, differences in access to health care (eg, reluctance in seeking care), or both.
Addressing the unique needs of the Latino community may help mitigate the spread of SARS-CoV-2 infection and prevent COVID-19.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.Yancy CW. COVID-19 and African Americans. JAMA. Published online April 15, 2020. doi: 10.1001/jama.2020.6548 [DOI] [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services Office of Minority Health Profile: Hispanic/Latino Americans. Posted August 22, 2019. Accessed June 6, 2020. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=64
- 3.Health insurance historical tables: HIC series. US Census Bureau. Posted September 26, 2019. Accessed June 6, 2020. https://www.census.gov/data/tables/time-series/demo/health-insurance/historical-series/hic.html
- 4.Bureau of Labor Statistics Job Flexibilities and Work Schedules—2017-2018 Data From the American Time Use Survey. US Dept of Labor; 2019:32. [Google Scholar]
- 5.Page KR, Venkataramani M, Beyrer C, Polk S. Undocumented U.S. immigrants and Covid-19. N Engl J Med. 2020;382(21):e62. doi: 10.1056/NEJMp2005953 [DOI] [PubMed] [Google Scholar]