Abstract
Importance
Patient reported outcomes (PROs) are an important marker of the quality of patient care. However, the extent to which PROs reflect care quality and clinical outcomes in surgical patients remains unclear.
Objective
To measure the association between patient-reported satisfaction and regret and clinical outcomes.
Design, Setting, and Participants
A retrospective, population-based analysis of adults ages 18 and older undergoing surgery across 38 hospitals in Michigan between January 1, 2017 and May 31, 2018. Patients were included if they responded to a PRO survey administered between 30–90 days after surgery.
Exposures
Postoperative complications.
Main Outcomes and Measures
Patient satisfaction (dichotomized as highly satisfied and not highly satisfied) and patient regret (dichotomized as absolutely no regret and regret).
Results
In this study, 9953 patients (mean age 56 years; 5634 women (57%)) underwent 1 of 16 procedures. 9550 (96%) patients experienced no complication, while 240 (2%) and 163 (2%) patients experienced Grade 1 and Grade 2–3 complications, respectively. Postoperative pain scores were: none (908 (9%) patients), mild (3863 (40%) patients), moderate (3893 (40%) patients), and severe (1075 (11%) patients). Overall, 7881 (79%) patients were highly satisfied and 8911 (91%) had absolutely no regret after surgery. Patients were less likely to be highly satisfied if they experienced a Grade 1 complication (OR 0.50, 95% CI 0.37–0.66 ), Grade 2–3 complication (OR 0.44, 95% CI 0.31–0.62), minimal pain (OR 0.80, 95% CI 0.64–0.99, moderate pain (OR 0.39, 95% CI 0.32–0.49), or severe pain (OR 0.23, 95% CI 0.18–0.29 ). Patients were less likely to have no regret if they experienced a Grade 1 complication (OR 0.48, 95% CI 0.33–0.70), Grade 2–3 complication (OR 0.39, 95% CI 0.25–0.60), moderate pain (OR 0.55, 95% CI 0.40–0.76), or severe pain (OR 0.22, 95% CI 0.16–0.31). The predicted probability of being highly satisfied was 79% for patients who had no complications and 88% for patients who had no pain.
Conclusions and Relevance
Patients who experienced postoperative complications and pain were less likely to be highly satisfied or have no regret. Importantly, postoperative pain had a more significant effect on satisfaction and regret after surgery, suggesting this as an important opportunity to improve patient experience.
Introduction
Patient satisfaction has become a priority for clinicians, hospitals, and healthcare payers. Healthcare organizations strive to deliver high-quality care that achieves good health outcomes while addressing patients’ desires as consumers. In addition, hospitals have a financial incentive to deliver satisfactory care. As of 2017, the Centers for Medicare & Medicaid Services (CMS) ties 2% of Medicare reimbursement to hospital performance on various measures, including patient satisfaction as measured by the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey.1 Publicly reported HCAHPS scores formally quantify patient-reported measures, including global satisfaction with care or whether patients would recommend a hospital to friends or family.2 For medical and surgical specialties alike, the commercialization and reporting of patient satisfaction has real impact on physician practice.
A goal of the HCAHPs survey is to incentivize hospitals to improve quality of care based on the assumption that higher quality will be reflected in increased patient satisfaction. It is unclear, however, whether high patient satisfaction scores accurately reflect high quality care, especially in surgical patients. In surgical care, quality measurement has traditionally emphasized clinical outcomes, such as mortality, postoperative complications, or readmissions.3 Evidence of the relationship between outcomes and patient satisfaction is mixed.4 Some studies have demonstrated a direct association between better clinical outcomes and higher patient satisfaction scores.4–10 In contrast, others have found that even patients who experience postoperative complications do not necessarily report lower satisfaction with their care.11–13 Notably, many of these studies used postoperative complication rates and satisfaction scores aggregated at the hospital level, rather than examining the relationship between an individual patient’s clinical outcome and their satisfaction.3,4,6,7,9–11,13–19 Studies that did use patient-level satisfaction and outcome data were relatively small and conducted at single institutions.5,8,12 Additionally, it is unclear whether there are other factors that affect the patient experience that are not measured in traditional outcomes. A patient-level study conducted across a large population could better explain the role that clinical outcomes play in patients’ perception of their care, and whether these outcomes are directly associated with satisfaction and to what degree. Elucidating the association between patient outcomes and patient experience could help clinicians and policymakers better understand the role that the quality of clinical care plays in the patient experience and vice versa.
Within this context, we utilized data from the Michigan Surgical Quality Collaborative (MSQC), a statewide multi-institutional quality improvement collaborative, to identify the association between clinical outcomes and patient-reported outcomes (PROs), including postoperative satisfaction and decision regret.20,21 Specifically, we sought to analyze the impact of specific clinical outcomes on satisfaction and regret to better understand the main drivers of good and bad patient experiences. We hypothesized that PROs would be inversely associated with number and severity of adverse outcomes after surgery, such as postoperative complications, readmission, and emergency department utilization, and we sought to measure the degree to which these outcomes impacted the patient experience.
Methods
Overview and Data Source
We performed a retrospective cohort study of prospectively collected data from the MSQC. The University of Michigan Institutional Review Board deemed this study exempt from review.
The MSQC is a collaborative of 70 hospitals across the state of Michigan that maintains a validated clinical registry for general surgery, vascular surgery, and gynecologic surgery procedures.19 Variables collected include patient characteristics, perioperative processes of care, 30-day clinical outcomes, 30-day patient-reported outcomes, and 30-day utilization outcomes such as readmission and emergency department (ED) visits. Cases were sampled for data abstraction using an algorithm aimed to represent all eligible cases performed that year and to minimize selection bias.22 Data was abstracted by trained nurses, whose salaries are supported by Blue Cross Blue Shield of Michigan, a major private payer in the state. Participating hospitals are diverse, ranging from small community hospitals to large, urban teaching hospitals, and include all hospitals performing major surgery in the state. MSQC members share data for analysis to improve pre- and post-operative care through quality improvement initiatives.
Starting in January 2017, the MSQC began collecting PROs at a subset of hospitals, including satisfaction with care, regret of undergoing surgery, and postoperative pain score.15 Patients received a telephone, mail, or e-mail survey at postoperative day 30 and were given 90 days to respond. We subsequently examined patient-reported satisfaction with care with the occurrence of a postoperative complication and compared this effect to other postoperative variables such as pain score after surgery.
Variable Definition
The primary outcomes were satisfaction with care and regret of undergoing surgery, collected using questions adapted from the O’Connor and Holmes-Rovner scales of decision satisfaction and regret.23,24 Patients were asked to rate their satisfaction on a Likert scale from 1 (extremely dissatisfied) to 10 (extremely satisfied). The distribution of satisfaction scores was highly skewed towards scores of 9 or 10, with greater than 90% of patients reporting one of those scores. As such, we dichotomized satisfaction into a binary variable of “highly satisfied” (a score of 9 or 10) and “not highly satisfied” (a score of 1–8). Dichotomization of skewed satisfaction scores is done by CMS for many HCAHPS survey questions and has also been used in many studies of patient satisfaction.5,11,25–27 These binary outcomes correspond to how CMS publicly reports hospital results.
Patients were asked to rate their regret of undergoing surgery on a Likert scale from 1 (strongly regret) to 5 (absolutely no regret). Again, due to the skew of regret scores toward no regret, this outcome variable was dichotomized into a binary variable of “absolutely no regret” (a score of 5) and “any regret” (a score of 1–4).
The primary outcome was the presence of any postoperative complication within 30 days as a binary variable. MSQC-defined complications included any of the following: surgical site infection (superficial, deep, and organ space), urinary tract infection (catheter-associated or spontaneous), pneumonia, unplanned intubation, pulmonary embolism, acute renal failure, stroke or cerebrovascular accident, cardiac arrest requiring cardiopulmonary resuscitation, acute myocardial infarction, cardiac dysfunction, deep venous thrombosis requiring therapy, sepsis, septic shock, Clostridium difficile infection, central line infection, and anastomotic leak.
We also adjusted for complication severity grade. Grade 1 complications were defined as non-life-threatening complications including acute renal insufficiency and/or failure, pneumonia, sepsis, superficial incisional SSI, and urinary tract infections. Grade 2 complications were potentially life-threatening complications such as anastomotic leaks, deep incisional SSI, deep vein thrombosis requiring therapy, organ/space SSI, pulmonary embolism, severe sepsis, and unplanned intubation. Grade 3 complications were life-threatening complications with residual or lasting disability or mortality, which includes cardiac arrest requiring CPR, myocardial infarction, stroke/CVA, and mortality. Grades 2 and 3 were combined into a single group due to inadequate sample size of patients with Grade 3 complications.
Covariates for risk adjustment included age (< 45 years, 45 – 64 years, 65+ years), sex, race (white, black, other), obesity (BMI >30 kg/m2), diabetes, chronic obstructive pulmonary disease, hypertension, tobacco use within 1 year, active cancer diagnosis, functional status (independent, not independent), American Society of Anesthesiologists (ASA) classification, surgical priority (elective versus urgent/emergent), surgical setting (outpatient versus inpatient), surgical procedure, and patient-reported pain score one week after surgery on a scale of 1 to 4 (1 = no pain, 2 = minimal pain, 3 = moderate pain, 4 = severe pain). Pain score was collected as part of a survey that patients completed between postoperative days 30–90.
Statistical Analysis
Descriptive analysis was used to characterize overall complication rates and pain scores for this cohort. We then isolated the independent association of a postoperative complications with a patient’s satisfaction and regret using hierarchical multivariable logistic regression to adjust for the patient covariates above and the clustering effects of patients within hospitals. This model thus allowed us to control for patient factors, such as demographics and comorbidities, as well as unmeasured hospital effects. All analysis was performed using Stata/SE version 15 (College Station, Texas).
Results
Characteristics of the Cohort
Demographic data for the cohort are presented in Table 1. Overall, our cohort includes 9953 patients across 38 MSQC participating hospitals between January 2017 and May 2018. The mean age (standard deviation) of the cohort was 56.2 (16.5) years, with 5634 female patients (57%), and 91% white, 6% black, and 3% other/unknown. There were 16 procedures included for analysis: abdominal hernia, carotid endarterectomy, creation, re-siting, or closure of ileostomy, laparoscopic hysterectomy, laparoscopic anti-reflux and hiatal hernia, laparoscopic appendectomy, laparoscopic cholecystectomy, laparoscopic colectomy, minor hernia, open appendectomy, open cholecystectomy, open colectomy, open small bowel resection or enterolysis, thyroidectomy, total abdominal hysterectomy, and vaginal hysterectomy.
TABLE 1.
Patient Characteristics*
| N Highly Satisfied (col. %) | N Unsatisfied (col. %) | P-value** | |
|---|---|---|---|
| Sex | 0.058 | ||
| Female | 4,423 (56.12) | 1,211 (58.45) | |
| Male | 3,458 (43.88) | 861 (41.55) | |
| Age | 0.272 | ||
| ≤44 | 1,988 (25.23) | 487 (23.50) | |
| 45—64 | 3,179 (40.34) | 855 (41.26) | |
| ≥65 | 2,714 (34.44) | 730 (35.23) | |
| Race | 0.069 | ||
| White | 7,136 (90.55) | 1,913 (92.33) | |
| Black | 464 (5.89) | 95 (4.58) | |
| Other | 75 (0.95) | 20 (0.97) | |
| Unknown | 206 (2.61) | 44 (2.12) | |
| Cigarette Use Within 1 Year | 0.282 | ||
| Yes | 1,537 (19.50) | 426 (20.56) | |
| No | 6,344 (80.50) | 1,646 (79.44) | |
| >2 drinks/day two weeks before admission? | 0.728 | ||
| Yes | 180 (2,28) | 50 (2.41) | |
| No | 7,701 (97.72) | 2,022 (97.59) | |
| Current Cancer | 0.014** | ||
| Yes | 546 (6.93) | 176 (8.49) | |
| No | 7,335 (93.07) | 1,896 (91.51) | |
| Obesity Status | 0.046** | ||
| Obese | 3,596 (45.63) | 937 (45.22) | |
| Not Obese | 4,277 (54.27) | 1,128 (54.44) | |
| Unknown | 8 (0.10) | 7 (0.34) | |
| ASA Class | 0.000** | ||
| Class 1 | 631 (8.01) | 147 (7.09) | |
| Class 2 | 4,374 (55.50) | 1,032 (49.81) | |
| Class 3 | 2,669 (33.87) | 816 (39.38) | |
| Class 4 | 207 (2.63) | 77 (3.72) | |
| Functional Status | 0.219 | ||
| Independent | 7,778 (98.69) | 2,045 (98.70) | |
| Not Independent | 75 (0.95) | 24 (1.16) | |
| Unknown | 28 (0.36) | 3 (0.14) | |
| Surgical Priority | 0.091 | ||
| Urgent/Emergent | 1,931 (24.50) | 545 (26.30) | |
| Elective | 5,950 (75.50) | 1,527 (73.70) | |
| Inpatient Status | 0.000** | ||
| Inpatient | 4,292 (54.46) | 1,246 (60.14) | |
| Outpatient | 3,589 (45.54) | 826 (39.86) | |
| Diabetes | 0.091 | ||
| Non-Diabetic | 6,797 (86.25) | 1,757 (84.80) | |
| Diabetic | 1,084 (13.75) | 315 (15.20) | |
| Chronic Condition | 0.004** | ||
| Yes | 170 (2.16) | 67 (3.23) | |
| No | 7,711 (97.84) | 2,005 (96.77) | |
| HTN | 0.266 | ||
| Yes | 3,339 (42.37) | 906 (43.73) | |
| No | 4,542 (57.63) | 1,166 (56.27) | |
| COPD | 0.020 | ||
| Yes | 431 (5.47) | 141 (6.81) | |
| No | 7,450 (94.53) | 1,931 (93.19) | |
| Surgical Procedure | 0.000** | ||
| Abdominal Hernia | 428 (5.43) | 125 (6.03) | |
| Carotid Endarterectomy | 44 (0.56) | 13 (0.63) | |
| Creation, Re-siting, or Closure of Ileostomy | 132 (1.67) | 57 (2.75) | |
| Laparoscopic Hysterectomy | 579 (7.35) | 155 (7.48) | |
| Laparoscopic Anti-Reflux and Hiatal Hernia | 68 (0.86) | 33 (1.59) | |
| Laparoscopic Appendectomy | 618 (7.84) | 139 (6.71) | |
| Laparoscopic Cholecystectomy | 2,136 (27.10) | 468 (22.59) | |
| Laparoscopic Colectomy | 405 (5.14) | 103 (4.97) | |
| Minor Hernia | 2,128 (27.00) | 517 (24.95) | |
| Open Appendectomy | 38 (0.48) | 19 (0.92) | |
| Open Cholecystectomy | 40 (0.51) | 30 (1.45) | |
| Open Colectomy | 359 (4.56) | 160 (7.72) | |
| Open Small Bowel Resection or Enterolysis | 135 (1.71) | 65 (3.14) | |
| Thyroidectomy | 166 (2.11) | 39 (1.88) | |
| Total Abdominal Hysterectomy | 259 (3.29) | 56 (2.70) | |
| Vaginal Hysterectomy | 346 (4.39) | 93 (4.49) | |
N=9,953
P-values of <0.05 are considered significant
With regard to primary outcomes, 9550 patients (96%) experienced no complications, 240 (2%) experienced a Grade 1 complication, and 163 (2%) experienced a Grade 2 or 3 complication (Table 2). 908 patients (9%) rated their postoperative pain as “none”, while 3863 (40%) rated their pain as “mild”, 3893 (40%) as “moderate”, and 1075 (11%) as “severe”. Across the entire cohort, 7881 patients (79%) were highly satisfied and 8911 (91%) had absolutely no regret with their decision to undergo surgery.
TABLE 2.
Cohort Outcomes*
| N | % | |
|---|---|---|
| Complication | ||
| No Complication | 9550 | 96 |
| Grade 1 | 240 | 2 |
| Grade 2,3 | 163 | 2 |
| Postoperative Pain | ||
| None | 908 | 9 |
| Mild | 3863 | 40 |
| Moderate | 3893 | 40 |
| Severe | 1075 | 11 |
| Satisfaction | ||
| Highly Satisfied | 7881 | 79 |
| Not Highly Satisfied | 2072 | 21 |
| Regret | ||
| Absolutely No Regret | 8911 | 91 |
| Regret | 859 | 9 |
N=9,953
Association between Satisfaction/Regret, Complications, and Pain
A multilevel hierarchical logistic regression was used to analyze the association of a number of patient- and hospital-level factors with satisfaction and regret (Table 3). Patients who experienced any complication were less likely to be highly satisfied and more likely to regret their surgery. Specifically, those with Grade 1 complications had 50% lower odds (1-OR: 0.50, 95% CI: 0.37–0.66) of being highly satisfied and 52% lower odds (1-OR: 0.48, 95% CI: 0.33–0.70) of having absolutely no regret compared to patients without any complication. Patients who experienced a Grade 2–3 complication had 56% lower odds (1-OR: 0.44, 95% CI: 0.0.31–0.62) of being highly satisfied and 61% lower odds (1-OR: 0.39, 95% CI: 0.25–0.60) compared to those without complications.
TABLE 3.
Multilevel Hierarchical Logistic Regression
|
Highly Satisfied |
Absolutely No Regret |
|||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P-value** | OR | 95% CI | P-value** | |
| Complication | ||||||
| No Complication | Reference | |||||
| Grade 1 | 0.50 | 0.37–0.66 | <0.001** | 0.48 | 0.33–0.67 | <0.001** |
| Grade 2–3 | 0.44 | 0.31–0.62 | <0.001** | 0.39 | 0.25–0.60 | <0.001** |
| Postoperative Pain | ||||||
| No Pain | Reference | |||||
| Minimal Pain | 0.80 | 0.64–0.99 | 0.046** | 1.09 | 0.78–1.51 | 0.621 |
| Moderate Pain | 0.39 | 0.32–0.49 | <0.001** | 0.55 | 0.40–0.76 | <0.001** |
| Severe Pain | 0.23 | 0.18–0.29 | <0.001** | 0.22 | 0.16–0.31 | <0.001** |
| Age | ||||||
| ≤44 | Reference | |||||
| 45—64 | 0.95 | 0.82–1.09 | 0.438 | 0.82 | 0.68–1.01 | 0.057 |
| ≥65 | 0.99 | 0.84–1.17 | 0.915 | 0.91 | 0.71–1.16 | 0.456 |
| Female | 0.94 | 0.84–1.07 | 0.363 | 0.87 | 0.73–1.05 | 0.145 |
| Race | ||||||
| White | Reference | |||||
| Black | 1.60 | 1.25–2.06 | <0.001** | 1.27 | 0.89–1.80 | 0.184 |
| Other | 1.15 | 0.69–1.93 | 0.593 | 0.55 | 0.30–0.98 | 0.042 |
| Unknown | 1.18 | 0.83–1.68 | 0.351 | 1.32 | 0.78–2.23 | 0.294 |
| Tobacco Use | 1.10 | 0.96–1.26 | 0.152 | 0.88 | 0.73–1.06 | 0.176 |
| Alcohol Use | 0.99 | 0.71–1.39 | 0.952 | 1.30 | 0.77–2.19 | 0.324 |
| Cancer | 0.94 | 0.76–1.16 | 0.573 | 1.34 | 0.97–1.86 | 0.077 |
| Obese | 1.03 | 0.93–1.16 | 0.542 | 0.90 | 0.77–1.05 | 0.190 |
| Chronic Condition | 0.84 | 0.62–1.14 | 0.271 | 0.74 | 0.49–1.13 | 0.165 |
| Hypertension | 1.04 | 0.92–1.18 | 0.504 | 1.08 | 0.90–1.28 | 0.415 |
| Chronic Obstructive Pulmonary Disease | 0.94 | −.75–1.17 | 0.571 | 0.95 | 0.69–1.29 | 0.730 |
| Diabetes Class | ||||||
| Non-Diabetic | Reference | |||||
| Diet-Controlled | 0.89 | 0.64–1.26 | 0.522 | 1.25 | 0.73–2.14 | 0.417 |
| Oral Medication-Controlled | 0.90 | 0.74–1.09 | 0.271 | 1.00 | 0.76–1.33 | 0.977 |
| Insulin-Dependent | 1.22 | 0.92–1.61 | 0.164 | 0.86 | 0.59–1.25 | 0.432 |
| ASA Class | ||||||
| 1 | Reference | |||||
| 2 | 1.00 | 0.81–1.24 | 0.975 | 1.22 | 0.91–1.63 | 0.185 |
| 3 | 0.86 | 0.68–1.09 | 0.205 | 1.28 | 0.92–1.78 | 0.145 |
| 4 | 0.76 | 0.52–1.11 | 0.154 | 1.04 | 0.61–1.78 | 0.875 |
| Functional Status | ||||||
| Independent | Reference | |||||
| Non-Independent | 1.12 | 0.68–1.85 | 0.653 | 0.63 | 0.33–1.17 | 0.143 |
| Unknown | 2.09 | 0.59–7.40 | 0.251 | 2.98 | 0.38–23.57 | 0.300 |
| Elective/Emergent Status | ||||||
| Elective | Reference | |||||
| Urgent/Emergent | 1.07 | 0.90–1.28 | 0.461 | 1.65 | 1.27–2.16 | <0.001** |
| Inpatient Status | 0.80 | 0.68–0.94 | 0.007** | 0.88 | 0.70–1.10 | 0.258 |
| Procedure | ||||||
| Abdominal Hernia | Reference | |||||
| Carotid Endarterectomy | 1.01 | 0.50–2.03 | 0.977 | 2.74 | 0.62–12.05 | 0.182 |
| Creation, Re-siting, or Closure of Ileostomy | 0.89 | 0.60–1.33 | 0.581 | 0.75 | 0.44–1.28 | 0.291 |
| Laparoscopic Hysterectomy | 1.03 | 0.76–1.40 | 0.839 | 0.87 | 0.57–1.31 | 0.502 |
| Laparoscopic Anti-Reflux and Hiatal Hernia | 0.79 | 0.48–1.29 | 0.344 | 0.60 | 0.31–1.13 | 0.111 |
| Laparoscopic Appendectomy | 1.13 | 0.82–1.55 | 0.462 | 1.49 | 0.89–2.49 | 0.130 |
| Laparoscopic Cholecystectomy | 1.14 | 0.90–1.46 | 0.283 | 1.04 | 0.73–1.47 | 0.833 |
| Laparoscopic Colectomy | 1.48 | 1.06–2.07 | 0.021** | 1.13 | 0.71–1.81 | 0.607 |
| Minor Hernia | 1.05 | 0.82–1.34 | 0.724 | 0.92 | 0.65–1.30 | 0.635 |
| Open Appendectomy | 0.53 | 0.28–1.01 | 0.054 | 0.82 | 0.30–2.28 | 0.706 |
| Open Cholecystectomy | 0.44 | 0.25–0.76 | 0.003** | 0.45 | 0.21–0.945 | 0.035** |
| Open Colectomy | 0.96 | 0.71–1.31 | 0.814 | 0.90 | 0.58–1.40 | 0.641 |
| Open Small Bowel Resection or Enterolysis | 0.79 | 0.53–1.19 | 0.266 | 1.23 | 0.64–2.39 | 0.536 |
| Thyroidectomy | 1.24 | 0.81–1.91 | 0.321 | 0.77 | 0.43–1.37 | 0.371 |
| Total Abdominal Hysterectomy | 1.42 | 0.96–2.11 | 0.079 | 1.45 | 0.82–2.58 | 0.204 |
| Vaginal Hysterectomy | 0.99 | 0.71–1.39 | 0.969 | 1.16 | 0.71–1.88 | 0.555 |
P-values of <0.05 are considered significant
Postoperative pain score was also significantly associated with patient satisfaction after surgery. Specifically, patients had 20%, 61%, and 77% lower odds of being highly satisfied if they reported minimal, moderate, or severe pain, respectively (1-OR 0.80, 95% CI 0.64–0.99; 1-OR 0.39, 95% CI 0.32–0.49; and 1-OR 0.23, 95% CI 0.18–0.29, respectively).
Race, inpatient status, and particular procedures were also associated with high satisfaction. Specifically, those who identify as black were 1.60 times more likely to be highly satisfied than those who identify as white (OR: 1.60, 95% CI: 1.25–2.06). Patients who were admitted after their surgery (inpatient status) had 20% lower odds (1-OR: 0.80, 95% CI: 0.68–0.94) of being highly satisfied compared to patients who underwent outpatient surgery. Furthermore, compared to patients who underwent an abdominal hernia repair (reference procedure), those who had a laparoscopic colectomy were 1.48 times more likely to be highly satisfied (OR: 1.48, 95% CI: 1.06–2.07), and those who had an open cholecystectomy 56% lower odds (1-OR: 0.44, 95% CI: 0.25–0.76) of being highly satisfied.
Postoperative pain score was also significantly associated with regret to undergo surgery. Specifically, patients had 45% and 78% lower odds of having absolutely no regret if they reported moderate or severe pain, respectively (1-OR 0.55, 95% CI 0.40–0.76; 1-OR 0.23, 95% CI 0.16–0.31, respectively).
Surgery urgency status (elective versus urgent/emergent) and specific procedures are additionally associated with regret. Particularly, patients who underwent urgent or emergent surgery were 1.65 times more likely (OR: 1.67, 95% CI: 1.26–2.16) to have absolutely no regret compared to patients who underwent elective surgery. Finally, compared to abdominal hernia repair, patients who underwent open cholecystectomy had 56% lower odds (1-OR: 0.44, 95% CI: 0.21–0.95) of having absolutely no regret.
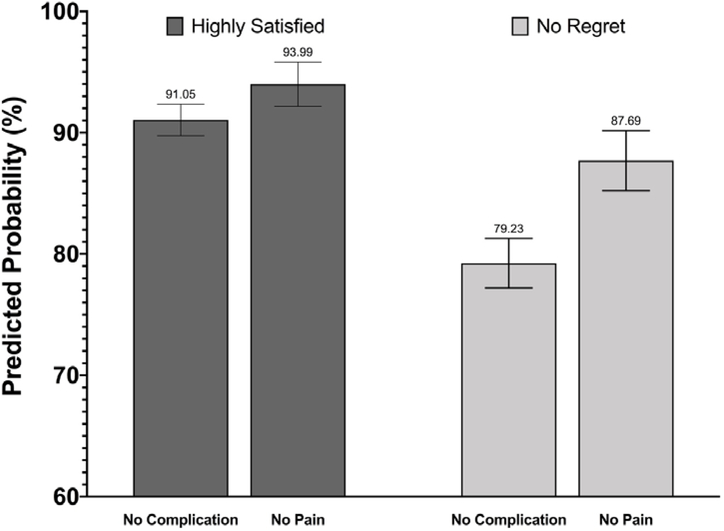
Predicted probabilities of being highly satisfied and having absolutely no regret by complication grade and pain score are shown in Figure 1.
Figure 1 –
Predicted probabilities of being highly satisfied and having no regret in patients who have no complications and no pain.
Discussion
After adjusting for a number of patient- and hospital-level factors, patients who experience grade 1–3 complications after surgery are less likely to be highly satisfied and more likely to regret undergoing surgery. These findings further clarify the relationship between a patient’s clinical outcomes – which are universally used as a marker of care quality – and the patient’s experience of their care. Additionally, worse postoperative pain, which affected many more patients than experienced complications, was also strongly associated with a lower likelihood of being satisfied after surgery. Our analysis revealed that a patient with severe pain was nearly twice as likely to be unsatisfied or regret surgery than a patient who experienced a complication.
This patient-level study adds to the growing evidence demonstrating an association between high quality surgical care and increased patient satisfaction. While a number of previous studies have failed to demonstrate an association between patient satisfaction and clinical outcomes, more recent studies have upheld this association.11,13,28 Tsai et. al. used a national inpatient claims dataset to demonstrate that hospitals with high satisfaction had better clinical outcomes, such as lower surgical mortality rates, lower readmission rates, and shorter lengths of stay.10 Similarly, Sacks et. al. conducted an analysis of hospitals participating in the American College of Surgeons National Surgical Quality Improvement Project (ACS-NSQIP) which found that hospitals in the highest quartile of satisfaction scores had lower mortality, failure to rescue, and minor complications.9 By analyzing this relationship at the patient level, our results further support a direct association between patient satisfaction and clinical outcomes.
Further, we found that post-surgical pain was one of the strongest predictors of satisfaction or regret compared to adverse clinical outcomes. What’s more, over 1000 patients experienced severe pain in the week following surgery, compared to less than 200 patients who experienced a serious complication. This demonstrates the profound role that pain plays in the patient experience. Specifically, a patient who experiences severe pain is less likely to be highly satisfied than a patient who experiences a complication. For example, our analysis suggests that a patient who experiences a myocardial infarction, stroke, or unplanned intubation had 56% lower odds of being highly satisfied, while a patient experiencing severe pain after surgery had 77% lower odds of being highly satisfied. This same effect is observed with patient regret after surgery as well – a patient with more pain after surgery is more likely to regret surgery than a patient with an adverse clinical outcome.
It is unsurprising that patients with worse pain after surgery report worsened measures of patient experience, and this has been previously demonstrated.29 To our knowledge, this is the first study to demonstrate the association between postoperative pain and patient experience for a wide variety of common surgical procedures, and to demonstrate the degree to which pain impacts patient experience even more so than clinical outcomes. This relationship has significant implications for surgical quality improvement. Currently, billions of dollars are spent on addressing patient satisfaction by improving traditional care pathways and surgical outcomes. These efforts focus on complications that affect a vast minority of patients. Much less attention, however, is paid to improving comprehensive pain management strategies. Our study demonstrates that moderate and severe pain after surgery affected ten-fold more patients than experienced a complication. While surgical outcomes have improved tremendously over the last two decades, less progress has been made regarding excellent pain control, suggesting that the patient experience may be significantly improved by focusing efforts in this area.30 For example, while enhanced recovery after surgery pathways have emphasized the role of multimodal analgesia in optimal pain management after surgery, improved patient counseling and expectation-setting may also be necessary to improve a patient’s pain experience after surgery, which our study suggests will in turn improve their overall experience significantly.31
This study also has implications for the way in which PROs are believed to reflect a hospital’s clinical performance and quality. A hospital that provides high-quality care and achieves low complication rates may have their HCAHPS scores negatively impacted if their patients experience uncontrolled pain after surgery. In fact, CMS revised the three HCAHPS questions about pain management in 2018 and will remove them entirely starting January 2022.32 Citing concerns about the opioid epidemic, CMS pursued these changes to avoid incentivizing hospitals to overprescribe opioids in an effort to boost HCAHPS scores. However, our findings suggest that pain management may still be reflected in measures of patient experience. Insofar as patient experience is now part of CMS’s Value-Based Purchasing program, this effect may lead to hospital reimbursement being disproportionally impacted by patient pain, an outcome that is not traditionally measured as part of hospital quality.33
This also raises the question of the impact of unmeasured patient experiences on patients’ perceived quality of care. For example, it is conceivable that a patient who has an uncomplicated post-surgical recovery will nevertheless be dissatisfied if they do not like the hospital food or have a frustrating experience in a crowded parking structure. While generalized concepts of patient-reported outcomes, patient-centered care, and care quality are often used interchangeably by hospitals, we have demonstrated that there is an unexplored deeper relationship between quality of care and patient satisfaction that requires a more nuanced look.
Given the role that patient experiences, such as pain, specifically play in the care pathway of a surgical patient, it may be necessary to narrow questions in standardized surveys like HCAHPS to accurately capture experiences. For example, surgery-specific measures of the patient experiences, such as S-CAHPS, may more accurately measure satisfaction as it relates to the care a patient receives.34 Of note, this finding should not be taken to suggest that increasing patient satisfaction as it relates to postoperative pain is as simple as prescribing more opioids: rather, a national study demonstrates that hospitals in the highest quintile of postoperative opioid prescribing had no difference in their HCAHPS scores compared to hospitals in the lowest quintile.35 Improving a patient’s pain experience after surgery requires a combination of appropriate expectation-setting, use of multimodal analgesia, and follow up.36
This study has several limitations. First, the observational nature of this study precludes any determination of causation with regard to the relationship between postoperative outcomes, pain, and PROs. Importantly, we are unable to characterize survey non-responders. It is possible that non-responders have different complication rates or clinical confounders (e.g., being unable to respond to the survey due to their outcome), or that a patient’s clinical experience motivates them to respond or not when contacted with a survey. This introduces the possibility of bias into the PROs under analysis, which may not be representative of the population at large. Responses may also be affected by recall bias on the part of patients, however a number of PRO surveys use a similar timeframe. Lastly, the satisfaction measure employed is relatively general, but again, mirrors the scoring and reporting methodology employed by CMS for HCAHPS scoring.
Conclusion
This population-based, patient-level study found a significant association between patients’ clinical outcome and their experience. Patients who experienced a postoperative complication or experienced moderate to severe pain were less likely to be highly satisfied or not regret undergoing surgery. Of these factors, postoperative pain had the greatest impact on satisfaction and regret. While these findings further support an association between clinical outcomes and patient satisfaction, policymakers should pay special attention to the degree to which postoperative pain may influence satisfaction compared to traditional markers of surgical quality. Hospital reimbursement may be disproportionally affected based on these findings despite providing quantifiably high-quality care, and improving pain care after surgery may be a critical opportunity to improve a patient’s overall experience.
Acknowledgments
Disclosures: Dr. Vu receives funding from the National Institute of Diabetes, Digestive, and Kidney Diseases (1F32 DK115340-01A1). Drs. Brummett, Waljee, and Englesbe receive funding for research from the National Institute on Drug Abuse (R01DA042859). Dr. Brummett consults for Heron Therapeutics. Dr. Englesbe receives partial salary support from Blue Cross and Blue Shield of Michigan through the Michigan Surgical Quality Collaborative. Dr. Howard receives funding from the Blue Cross Blue Shield of Michigan Foundation.
References
- 1.Centers for Medicare & Medicaid Services. Medicare Program: Hospital Inpatient Value-Based Purchasing Program. Fed Regist. 2011;76(9):2454–2491.To be codified at 42 CFR §422 and §480. [PubMed] [Google Scholar]
- 2.Services CfMM. HCAHPS Fact Sheet (CAHPS® Hospital Survey). [PDF]. 2017; https://www.hcahpsonline.org/globalassets/hcahps/facts/hcahps_fact_sheet_november_2017.pdf. Accessed June 4, 2019.
- 3.Donabedian A The Quality of Care: How Can It Be Assessed? JAMA. 1988;260(12):1743–1748. [DOI] [PubMed] [Google Scholar]
- 4.Tevis SE, Schmocker RK, Kennedy GD. Can patients reliably identify safe, high quality care? Journal of hospital administration. 2014;3(5):150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gurland BH, Merlino J, Sobol T, et al. Surgical complications impact patient perception of hospital care. Journal of the American College of Surgeons. 2013;217(5):843–849. [DOI] [PubMed] [Google Scholar]
- 6.Jha AK, Orav EJ, Zheng J, Epstein AM. Patients’ perception of hospital care in the United States. New England Journal of Medicine. 2008;359(18):1921–1931. [DOI] [PubMed] [Google Scholar]
- 7.Kennedy GD, Tevis SE, Kent KC. Is there a relationship between patient satisfaction and favorable outcomes? Annals of surgery. 2014;260(4):592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prabhu KL, Cleghorn MC, Elnahas A, et al. Is quality important to our patients? The relationship between surgical outcomes and patient satisfaction. BMJ Qual Saf. 2018;27(1):48–52. [DOI] [PubMed] [Google Scholar]
- 9.Sacks GD, Lawson EH, Dawes AJ, et al. Relationship between hospital performance on a patient satisfaction survey and surgical quality. JAMA surgery. 2015;150(9):858–864. [DOI] [PubMed] [Google Scholar]
- 10.Tsai TC, Orav EJ, Jha AK. Patient satisfaction and quality of surgical care in US hospitals. Annals of surgery. 2015;261(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lyu H, Wick EC, Housman M, Freischlag JA, Makary MA. Patient satisfaction as a possible indicator of quality surgical care. JAMA surgery. 2013;148(4):362–367. [DOI] [PubMed] [Google Scholar]
- 12.Schmocker RK, Stafford LMC, Winslow ER. Satisfaction with surgeon care as measured by the Surgery-CAHPS survey is not related to NSQIP outcomes. Surgery. 2019;165(3):510–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sheetz KH, Waits SA, Girotti ME, Campbell DA Jr, Englesbe MJ. Patients’ perspectives of care and surgical outcomes in Michigan: an analysis using the CAHPS hospital survey. Annals of surgery. 2014;260(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang JT, Hays RD, Shekelle PG, et al. Patients’ global ratings of their health care are not associated with the technical quality of their care. Annals of Internal Medicine. 2006;144(9):665–672. [DOI] [PubMed] [Google Scholar]
- 15.Howard R, Fry B, Gunaseelan V, et al. Association of opioid prescribing with opioid consumption after surgery in Michigan. JAMA surgery. 2019;154(1):e184234–e184234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kupfer JM, Bond EU. Patient satisfaction and patient-centered care: necessary but not equal. Jama. 2012;308(2):139–140. [DOI] [PubMed] [Google Scholar]
- 17.Rao M, Clarke A, Sanderson C, Hammersley R. Patients’ own assessments of quality of primary care compared with objective records based measures of technical quality of care: cross sectional study. Bmj. 2006;333(7557):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tevis SE, Kennedy GD. Patient satisfaction: does surgical volume matter? journal of surgical research. 2015;196(1):124–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vu JV, Collins SD, Seese E, et al. Evidence that a regional surgical collaborative can transform care: surgical site infection prevention practices for colectomy in Michigan. Journal of the American College of Surgeons. 2018;226(1):91–99. [DOI] [PubMed] [Google Scholar]
- 20.Campbell DA Jr., Kubus JJ, Henke PK, Hutton M, Englesbe MJ. The Michigan Surgical Quality Collaborative: a legacy of Shukri Khuri. American journal of surgery. 2009;198(5 Suppl):S49–55. [DOI] [PubMed] [Google Scholar]
- 21.Englesbe MJ, Dimick JB, Sonnenday CJ, Share DA, Campbell DA Jr. The Michigan surgical quality collaborative: will a statewide quality improvement initiative pay for itself? Annals of surgery. 2007;246(6):1100–1103. [DOI] [PubMed] [Google Scholar]
- 22.Healy MA, Regenbogen SE, Kanters AE, et al. Surgeon Variation in Complications With Minimally Invasive and Open Colectomy: Results From the Michigan Surgical Quality Collaborative. JAMA Surg. 2017;152(9):860–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brehaut JC, O’Connor AM, Wood TJ, et al. Validation of a decision regret scale. Med Decis Making. 2003;23(4):281–292. [DOI] [PubMed] [Google Scholar]
- 24.Holmes-Rovner M, Kroll J, Schmitt N, et al. Patient satisfaction with health care decisions: the satisfaction with decision scale. Med Decis Making. 1996;16(1):58–64. [DOI] [PubMed] [Google Scholar]
- 25.Elliott MN, Zaslavsky AM, Goldstein E, et al. Effects of survey mode, patient mix, and nonresponse on CAHPS hospital survey scores. Health Serv Res. 2009;44(2 Pt 1):501–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Regenbogen SE, Gawande AA, Lipsitz SR, Greenberg CC, Jha AK. Do differences in hospital and surgeon quality explain racial disparities in lower-extremity vascular amputations? Annals of surgery. 2009;250(3):424–431. [DOI] [PubMed] [Google Scholar]
- 27.Schmocker RK, Cherney Stafford LM, Winslow ER. Satisfaction with surgeon care as measured by the Surgery-CAHPS survey is not related to NSQIP outcomes. Surgery. 2019;165(3):510–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kennedy GD, Tevis SE, Kent KC. Is there a relationship between patient satisfaction and favorable outcomes? Ann Surg. 2014;260(4):592–598; discussion 598–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baker PN, van der Meulen JH, Lewsey J, Gregg PJ, National Joint Registry for E, Wales. The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J Bone Joint Surg Br. 2007;89(7):893–900. [DOI] [PubMed] [Google Scholar]
- 30.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364(22):2128–2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hallway A, Vu J, Lee J, et al. Patient Satisfaction and Pain Control Using an Opioid-Sparing Postoperative Pathway. J Am Coll Surg. 2019. Available at 10.1016/j.jamcollsurg.2019.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Proposed Changes to Hospital Outpatient Prospective Payment and Ambulatory Surgical Center Payment Systems and Quality Reporting Programs. CMS-1695–P. Center for Medicaire & Medicaid Services (CMS). 2019. [Google Scholar]
- 33.Centers for Medicare and Medicaid Services. Medicare program; hospital inpatient Value-Based Purchasing program: final rule. Fed Regist. 2011;76(88):26490–26547. [PubMed] [Google Scholar]
- 34.Sage J Using S-CAHPS. Bull Am Coll Surg. 2013;98(8):53–56. [PubMed] [Google Scholar]
- 35.Lee JS, Hu HM, Brummett CM, et al. Postoperative Opioid Prescribing and the Pain Scores on Hospital Consumer Assessment of Healthcare Providers and Systems Survey. Jama. 2017;317(19):2013–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gawande AA. It’s Time to Adopt Electronic Prescriptions for Opioids. Ann Surg. 2017;265(4):693–694. [DOI] [PubMed] [Google Scholar]